Abstract
Background
Cervical pillar hyperplasia (CPH) is a recently described phenomenon of unknown aetiology. Its clinical importance is poorly understood at the present time; therefore, the objective of this study was to determine (1) the inter-examiner reliability of detecting CPH and (2) if there is a clinically important correlation (r > 0.4) between the number of cervical spine levels showing signs of degenerative joint disease (DJD) and CPH.
Methods
The sample consisted of 320 radiographs of human male and female subjects who ranged from 40 to 79 years of age. The inter-examiner reliability of assessing the presence/absence of pillar hyperplasia was evaluated on 50 neutral lateral radiographs by two examiners using line drawings and it was quantified using the kappa coefficient of concordance. To determine the presence/absence of hyperplastic pillars as well as the presence/absence of DJD at each intervertebral disc and zygapophysial joint, 320 AP open mouth, AP lower cervical and neutral lateral radiographs were then examined. The unpaired t-test at the 5% level of significance was performed to test for a statistically significant difference between the number of levels affected by DJD in patients with and without hyperplasia. The Spearman's rho at the 5% level of significance was performed to quantify the correlation between DJD and age.
Results
The inter-examiner reliability of detecting cervical pillar hyperplasia was moderate with a kappa coefficient of 0.51. The unpaired t-test indicated that there was no statistically significant difference (p > 0.05) between the presence/absence of cervical pillar hyperplasia and the number of levels affected by DJD in an age-matched population, regardless of whether all elements were considered together, or the discs and facets were analyzed separately. A Spearman correlation rank of 0.67 (p < 0.05) suggested a moderately strong correlation between the number of elements (i.e. discs/facets) affected, and the age of the individual.
Conclusion
Cervical pillar hyperplasia is a reasonable concept that requires further research. Its evaluation is easy to learn and acceptably reliable. Previous research has suggested that CPH may affect the cervical lordosis, and therefore, alter biomechanics which may result in premature DJD. This current study, however, indicates that, globally, CPH does not appear to be related to the development of DJD.
Similar content being viewed by others
Background
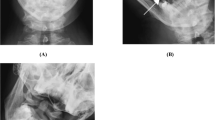
Several authors recently proposed the concept of cervical pillar hyperplasia [1–4]. Hyperplasia is identified on the neutral lateral cervical radiograph as parallel or posterior divergent lines drawn along the superior and inferior articular pillars (Figure 1b). The "usual" lordotic cervical curve requires these lines to converge posteriorly (Figure 1a) [2, 3]. The straightening effect of hyperplastic articular pillars on the cervical lordosis was suggested by Peterson and Wei [2] in 1987 and confirmed in 1999 [3]. These two studies were criticized by Harrison et al [5, 6] regarding the way pillar hyperplasia was determined, cervical lordosis was measured, and on a few other issues that were based on a misinterpretation of Peterson et al's article. In contrast to those critiques, Haas et al [7] reported that the measurement of each segment to determine the cervical lordosis, as suggested by Harrison et al would increase measurement errors. Furthermore, Peterson et al used Chamberlain's line to eliminate the effect of anterior head carriage in both the hyperplastic and the non-hyperplastic pillar populations. Flexion/extension studies were not necessary to define cervical pillar hyperplasia since it was detectable on the radiographic films most commonly used by primary physicians, the neutral lateral radiographs [3]. Therefore, to this point, both the concept of cervical pillar hyperplasia and its effect on the cervical lordosis seem reasonable [8]. This condition is of unknown aetiology and it may have clinical consequences that need to be determined.
Degenerative joint disease is a common, age-related [9–12], multi-factorial condition with several theorized aetiologies including metabolic, mechanical, inflammatory, and genetic components [11, 13–16]. It affects all joints, particularly those that experience chronic biomechanical stresses such as frequent repetitive use and strain, and constant weight-bearing.
The cervical/neck region is the human spine's most actively mobile part [17]. It has to support the permanent load of the head; therefore, progressive degenerative processes frequently affect it. This means that the intervertebral disc can become narrowed, develop osteophytes and have surrounding subchondral sclerosis in the condition called "degenerative disc disease" [12, 18]. It has been shown that there is a higher incidence of the development of disc space narrowing with the presence of anterior osteophytes on initial films, while posterior osteophytes are more commonly associated with the presence of an already narrowed disc space [19].
Both facet and uncovertebral joints can hypertrophy, sclerose and develop osteophytic spurs, in conditions described as facet arthrosis and uncovertebral arthrosis, respectively [12, 18]. Several grading systems have been developed to determine the degree of degeneration radiographically, using signs of subchondral sclerosis, joint space irregularity, decreased joint space and anterior and/or posterior osteophyte formation [9, 11, 12, 20–22]. The degenerative condition that involves degenerative disc disease, facet arthrosis and/or uncovertebral arthrosis is defined as "degenerative joint disease (DJD)," osteoarthrosis, or cervical spondylosis (Figure 2 and 3). Such degenerative processes may have various clinical implications: they may cause limitation of head and neck mobility, with or without pain; occasionally, they can cause intervertebral foramen encroachment and central canal stenosis, which can result in nerve root or spinal cord compression (radiculopathy and myelopathy respectively) [11, 23–26], and less commonly, extensive anterior osteophytosis can lead to dysphagia or even vocal fold paralysis [27].
The presence of osteoarthrosis is often confirmed using plain film radiographic findings, with the lateral view being the most informative [11]. Magnetic resonance imaging (MRI) and computed tomography (CT) are also useful diagnostic tools and can be used to determine the extent of soft tissue and bony involvement respectively. Although CT is the gold standard for detecting degenerative changes, plain film radiography is less expensive and more commonly used in primary contact clinical settings [11, 28].
There is some controversy in the literature over whether radiological findings are related, to a clinically important degree, to the patient's symptoms. In a recent long-term follow-up study, Gore [10] found that there might be a correlation between the patient's symptoms and radiographic findings. The subjects of his study who showed earlier degenerative changes at a particular level (C6-C7) were 4 times more likely to experience pain 10 years later compared to those without degenerative changes [10]. Most other authors, however, tend to dispute this finding [11, 29–31]. A recent cross-sectional study of United Kingdom patients found that there is no statistically significant difference in pain or disability levels, between patients with and without radiographic evidence of degeneration in the cervical spine [32].
It is currently not known whether the architecture of the articular pillars has any effect on regional biomechanics and subsequent degeneration. The hypothesis that was tested with our study was whether pillar hyperplasia accelerates the development of DJD, particularly in the intervertebral disc (IVD). The orientation of the facet joint in relation to the horizontal plane principally influences the axis around which flexion/extension occurs [33–35]. A more horizontal facet compared to the plane of the superior endplate of the vertebral body will shift the instantaneous center of rotation anteriorly, resulting in an increased load on the IVD [36–38]. It has also been shown that a flattened superior facet increases the risk of anterolisthesis (i.e. stress on the disc) [39]. Studies have shown that cervical pillar hyperplasia has an effect on the cervical curve [2, 3]. A straightening of the cervical curve results in a redistribution of the loads, favouring the facet joints, and therefore increasing the load on the IVD. An increase of the stress-load on the disc locally may enhance the degenerative process in the intervertebral compartment [40]. The presence of cervical pillar hyperplasia should consequently theoretically accelerate the degenerative processes of the IVD. We assumed that the degenerative processes would be a result of the cervical pillar hyperplasia and not the opposite, since cervical pillar hyperplasia has been observed at all ages.
No one has yet studied the prevalence of DJD in individuals with hyperplasia in comparison to those without. The purpose of this paper, therefore, was:
(1) to determine the inter-examiner reliability of detecting hyperplasia of the cervical articular pillars; and (2) to determine if there is a difference in the number of cervical spine levels showing signs of degenerative joint disease (DJD) in an age-matched sample with and without hyperplasia of the articular pillars at one or more levels, and hence, what the relationship is between cervical pillar hyperplasia and spinal DJD.
Methods
Radiograph Case Selection
Ethics approval to access the radiographs which were selected from the H.K. Lee radiology facility files at the Canadian Memorial Chiropractic College in Toronto was obtained from the CMCC Institutional Research Board. The inclusion criteria for the radiographs were:
a) the radiograph had to be of good radiological quality (collimation, penetration, absence of artifacts);
b) the radiograph had to be of a patient whose age ranged from 40 to 79 yrs;
c) the radiograph could not show evidence of a pathologic condition or abnormality other than signs of osteoarthrosis;
d) the file had to consist of at least three views: an anteroposterior open mouth (APOM), AP lower cervical and a neutral lateral.
The investigators selecting the cases were blinded with regard to the clinical status of the cases.
Inter-examiner Reliability Study
Sample Size Justification
A sample size estimate was performed according to the method of Donner and Eliasziw [41], and revealed that at an anticipated moderate agreement of kappa = 0.4 – 0.6 [42], and using the 5% level of significance, a power level of 80%, and 2 measurements per spinal level, a minimum of 50 radiographs would be required.
Assessment Protocol
The methodology was the same as that used by Peterson [2, 3]. Two previously trained 4th year chiropractic students independently evaluated the articular pillars of C3 through C6 (typical cervical facets) by drawing lines along the superior and inferior articular surfaces of each pillar. Lines converging posteriorly designated 'normal' pillar architecture. Parallel or posteriorly diverging lines designated what has been defined as 'pillar hyperplasia'. The data were categorical (binary) because each pillar set was assigned a label of either 'normal' or 'hyperplastic'. The articular pillars of C7 were not evaluated because of their normally 'notched' appearance [43].
Data Analysis
For each cervical segment, inter-examiner reliability was assessed via the kappa coefficient of concordance (k) [44].
Relationship Between CPH and Spinal DJD Study
Assessment Protocol
For the second part of the study, radiographs were evaluated until a total of 320 sets of films, 160 sets with pillar hyperplasia and 160 sets without pillar hyperplasia, were age and gender matched. Presence of hyperplasia at a single level was sufficient to categorize the cervical spine as 'hyperplastic'. Age was recorded as eight 5-yr categories. Radiographs were read until each age and gender sub-category contained 10 sets of films. Therefore, two options for the presence/absence of cervical pillar hyperplasia multiplied by two options for gender and eight age categories created 32 final subgroups each containing 10 radiograph sets. The same 320 radiographs were then read a second time to assess for degenerative changes. Eleven elements were assessed (namely C1-C2 facets, C2-C7 discs and facets).
APOM and AP lower cervical views were used to assess the zygapophysial joints. Signs of DJD affecting the zygapophysial joint included joint sclerosis, thinning of the joint space or bony hypertrophy [12], which results in a disruption of the normally smooth lateral sine curve formed by the external aspect of the articular pillars [45].
Neutral lateral cervical films were used to assess the disc spaces and the presence or absence of anterior or posterior osteophytes. The uncinate processes were not taken into consideration, given that their degenerative changes parallel those of the intervertebral disc [12]. Each radiograph was evaluated at six levels (from the C1-C2 level to the C6-C7 level) by one of the trained 4th year chiropractic students. All radiographs were then re-evaluated by a chiropractic radiologist to assure accuracy of the diagnosis.
The reliability of this method of assessing the presence of DJD in the cervical spine has been shown to be substantial [46]. These data were categorical (binary), because each articulation was labelled as either 'normal' or 'showing signs of DJD'.
Data Analysis
First, we determined whether a clinically and statistically significant difference existed for the average number of levels affected by DJD between patients with and without pillar hyperplasia. For the latter (statistical significance testing), we used the unpaired t-test and Mann-Whitney U test (depending on whether the data were normally distributed or not) at the 5% level of significance. It was planned to perform a logistic regression analysis to quantify the relationship between DJD and CPH, if the difference was clinically important and statistically significant. The data were also stratified by age and gender. The Spearman's rho at the 5% level of significance was performed to quantify the correlation between DJD and age.
Results
Inter-examiner Reliability Study
Both examiners assessed the first set of 50 films independently. The results are summarized in Table 1. The kappa value quantifying the overall inter-examiner reliability/agreement was 0.51, which is considered moderately strong, and was judged to be sufficiently acceptable to enable engaging in the next study assessing the relationship between CPH and spinal DJD, using only one examiner to assess each set of radiographs for the presence/absence of hyperplasia.
Relationship Between CPH and Spinal DJD Study
Radiographs were read until each age and gender sub-category contained 10 sets of films. Some radiographs had to be discarded in the process of achieving these numbers, most commonly due to the concomitant presence of diffuse idiopathic skeletal hyperostosis or fusion, as well as poor film quality. The Mann-Whitney U test showed no statistically significant difference between genders in the number of elements affected by DJD, not taking into account the age or the presence or absence of cervical pillar hyperplasia (with 160 sets of radiographs in each subgroup). A Spearman's correlation coefficient of 0.67 (p < 0.05) suggested a fairly strong and clinically important linear correlation between the number of elements (i.e. discs/facets) affected and the age of the individual.
Because gender did not appear to affect the development of DJD, we analyzed the possible effect of cervical pillar hyperplasia on the development of DJD, stratifying only by age category. The unpaired t-test was used for this purpose because the data were normally distributed. Table 2 shows that no statistically or clinically significant differences were found between the presence versus absence for cervical pillar hyperplasia groups and the number of levels affected by DJD in an age-matched population, regardless of whether all elements were considered together (n = 11), or the discs (n = 5) and facets (n = 6) were analyzed separately. Since no difference was found between the presence/absence of cervical pillar hyperplasia and the number of levels affected by DJD, logistic regression analysis was not performed.
Discussion
Cervical pillar hyperplasia is a recently described phenomenon of unknown aetiology. To date, the only promising data on the clinical relevance of hyperplasia is its possible effect on cervical spine lordosis [2, 3]. Having little information on cervical pillar hyperplasia allows for much speculation on the effect it may potentially have on cervical spine biomechanics; furthermore, it is important to determine whether this effect may or may not be of clinical significance. Theoretically, altered biomechanics of the spine could lead to degenerative changes and possible clinical consequences. It is currently not known to what degree, if any, cervical pillar hyperplasia contributes to the development of degenerative joint disease.
Our study found moderately strong agreement between two examiners in assessing cervical pillar hyperplasia. The moderate inter-examiner reliability achieved by the novices in this study coincided with the acceptable-to-good reliability (0.4–0.61) attained previously by Peterson [3]. It shows that the assessment of hyperplasia is an uncomplicated evaluation method, and therefore does not require expert skills. It should be noted, however, that in the study by Peterson, cervical pillar hyperplasia was assessed segmentally, and not globally; nevertheless, the fact that novice examiners performed the assessments of cervical pillar hyperplasia, and acceptable agreement was achieved, lends further credibility to the acceptability of the reliability of this diagnostic test.
Our study suggests that there is no clinically important difference between those with or without cervical pillar hyperplasia with respect to the prevalence of degenerative joint disease. This study also suggests that DJD is affected by age but not by gender, which concurs with previous studies [9–12, 47]. Other known contributors to the development of DJD that were not tested in this study include trauma, genetic, metabolic, and inflammatory processes [11, 13–16]. These results imply that cervical pillar hyperplasia is congenital, and allows the body to compensate for changes resulting from slightly aberrant biomechanics.
It should be noted that this study only looked at the presence/absence of DJD, and not its severity; thus there may indeed be a difference in the two groups if severity had been considered, but this has yet to be determined.
In our study, due to feasibility constraints, pillar hyperplasia was assessed globally in the cervical spine and considered to be present if even one cervical segment from C3 to C6 had a hyperplastic pillar. This definition may have resulted in more positive inter-examiner reliability than if segment-specific pillar hyperplasia had been assessed. Cervical pillar hyperplasia, as defined here, may possibly affect the biomechanics of the whole cervical spine; therefore, DJD was also assessed globally from C1 to C7.
Follow-up research should evaluate the segment-specific contribution of pillar hyperplasia to the development of DJD. Severity of DJD should perhaps also be considered. One of the limitations encountered when assessing films for cervical pillar hyperplasia was that the evaluation of C2-3 was not always adequate due to poor visualization. The same problem occurred at C1-2 while assessing for DJD. Another limitation of the study is using amateur examiners to detect cervical pillar hyperplasia and DJD; however, having a radiology expert re-evaluate each set of films likely minimized these problems.
Conclusions
Cervical pillar hyperplasia has shown evidence of being a credible phenomenon that requires further research. Its diagnosis appears to be easy to learn and reliable. This study indicated that, globally, cervical pillar hyperplasia does not appear to have an effect on the development of degenerative joint disease; however, because previous research suggests that cervical pillar hyperplasia affects the cervical lordosis, it is recommended that further research explore any segment-specific contribution of pillar hyperplasia to the development and severity of DJD.
Author contributions
Conception and design: CK Peterson, M Stupar, D Mauron
Generating and interpretation of data: D Mauron, M Stupar, CK Peterson
Statistical analysis and interpretation: D Mauron, M Stupar, CK Peterson
Drafting of the article: M Stupar, D Mauron
Critical revision of the article for important intellectual content: CK Peterson
Administrative, technical and logistic support: M Stupar, D Mauron
References
McRae J: Roentgenometrics in chiropractic. 1977, Toronto: Canadian Memorial Chiropractic College
Peterson CK, Wei T: Vertical hyperplasia of the cervical articular pillars. Another look at the straight cervical spine. J Chiropractic. 1987, 21: 78-9.
Peterson CK, Kirk RJ, Isdahl M, Humphrey BK: Prevalence of hyperplastic articular pillars in the cervical spine and relationship with cervical lordosis. J Manipulative Physiol Ther. 1999, 22: 390-4.
Pyrrha JL, Peterson CK: Flexicurve of the cervical spine of patients with and without hyperplastic pillars [abstract]. In Proceedings of the 2002 International Conference on Spinal Manipulation: October 4–5 2002; Toronto. 2002, The Foundation for Chiropractic Education and Research, Des Moines (IA), 99-100.
Harrison DE, Harrison DD, Troyanovich DC: Reliability of spinal displacement analysis on plain x-rays: a review of commonly accepted facts and fallacies with implications for chiropractic education and technique. J Manipulative Physiol Ther. 1998, 21: 252-66.
Harrison DD, Harrison DE, Troyanovich SJ, Harrison SO: Letter to the editor. Prevalence of hyperplastic articular pillars in the cervical spine and relationship with cervical lordosis. J Manipulative Physiol Ther. 2000, 23 (5): 366-8. 10.1067/mmt.2000.106862d.
Haas M, Taylor JAM, Gillette RG: The routine use of radiographic spinal displacement analysis: a dissent. J Manipulative Physiol Ther. 1999, 22: 254-9.
Peterson CK: In response. J Manipulative Physiol Ther. 2000, 23 (5): 368-9. 10.1067/mmt.2000.106862e.
Gore DR: Roentgenographic findings of cervical spine in asymptomatic people. Spine. 1986, 11: 521-4.
Gore DR: Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine. 2001, 26: 2463-6. 10.1097/00007632-200111150-00013.
McClure P: The degenerative cervical spine: pathogenesis and rehabilitation concepts. Journal of Hand Therapy. 2000, 163-74.
Yochum TR, Rowe LJ: Essentials of Skeletal Radiology. 1996, Baltimore: William & Wilkins
Attur MG, Dave M, Akamatsu M, Katoh M, Amin AR: Osteoarthritis or osteoarthrosis: the definition of inflammation becomes a semantic in the genomic era of molecular medicine. Journal of the OsteoArthritis Research Society International. 2002, 10: 1-4. 10.1053/joca.2001.0488.
Doss MG: Degenerative joint disease of the cervical spine. Journal of Chiropractic. 1982, 16: 41-2.
Ingvarsson T, Lohmander S: Icelandic genealogical registry sheds light on the significance of heredity in osteoarthritis. Lakartidningen. 2002, 99 (47): 4724-8.
Yoo K, Origaitano TC: Familial cervical spondylosis. Case report. Journal of Neurosurgery. 1998, 89 (1): 139-41.
Gay RE: The curve of the cervical spine: variations and significance. J Manipulative Physiol Ther. 1993, 16: 591-4.
Prescher A: Anatomy and pathology of the aging spine. European Journal of Radiology. 1998, 27 (3): 181-95. 10.1016/S0720-048X(97)00165-4.
Gore DR, Sepic SB, Gardner GM, Murray MP: Neck pain: a long term follow up of 205 patients. Spine. 1987, 12: 148-61.
Côté P, Cassidy JD, Yong-Hing K, Sibley J, Loewy J: Apophysial joint degeneration, disc degeneration and sagittal curve of the spine. Spine. 1997, 22: 859-64. 10.1097/00007632-199704150-00007.
Lane NF, Kremer LB: Radiographic indices for osteoarthritis. Rheum Dis Clin North Am. 1995, 379-94.
Taitz C: Osteophytosis of the cervical spine in South African Blacks and Whites. Clinical Anatomy. 1999, 12: 103-9. 10.1002/(SICI)1098-2353(1999)12:2<103::AID-CA4>3.0.CO;2-6.
Contley T, Schoenman K, Pudik T: Cervical spondylotic myelopathy. Topics in Clinical Chiropractic. 1995, 2 (3): 48-53.
Harding JG: Complications of cervical arthritis. Postgraduate Medicine. 1992, 91 (4): 309-18.
Lestini WF, Wiesel SW: The pathogenesis of cervical spondylosis. Clinical Orthopedics and Related Research. 1989, 239: 69-93.
Sanguinetti C, De Santis E: The role of apophysial osteoarthritis in cervical radicular syndromes. Journal of Neurosurgery Sciences. 1981, 25 (3–4): 159-61.
Yoskovitch A, Kantor S: Cervical osteophytes presenting as unilateral vocal fold paralysis and dysphagia. Journal of Laryngology and Otology. 2001, 115: 422-24. 10.1258/0022215011907820.
Rahim KA, Stambough JL: Radiographic evaluation of the degenerative cervical spine. Orthopedic Clinics of North America. 1992, 23 (3): 395-403.
Bassano JM: Radiological review of the arthritides. Topics of Clinical Chiropractic. 2000, 7 (2): 17-38.
Guyer RD, Mason SL, Ohnmeiss DD: The relation between cervical discographic pain responses and radiographic images. Clinical Journal of Pain. 2000, 16 (1): 1-5. 10.1097/00002508-200003000-00001.
Marchiori DM, Handerson CMR: A cross sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine. 1996, 21: 2747-51. 10.1097/00007632-199612010-00007.
Peterson CK, Bolton J, Wood A, Humphreys BK: A cross-sectional study correlating degeneration of the cervical spine with disability and pain in United Kingdom patients. Spine. 2003, 28 (2): 129-33. 10.1097/00007632-200301150-00007.
Harrison DD, Troyanovich SR, Harrison DE, Janik TJ, Murphy DJ: A normal sagittal spinal configuration: desirable clinical outcome. J Manipulative Physiol Ther. 1996, 19: 398-405.
Maurel N, Lavaste F, Skalli W: A three-dimensional parameterized finite element model of the lower cervical spine. Study of the influence of the posterior articular facets. J Biomechanics. 1997, 30 (9): 921-31. 10.1016/S0021-9290(97)00056-0.
Pal GP, Routal RV, Saggu SK: The orientation of the articular facets of the zygapophysial joints at the cervical and upper thoracic region. Journal of Anatomy. 2001, 198: 431-41. 10.1046/j.1469-7580.2001.19840431.x.
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GBJ, Haughton VM: The effect of disc degeneration and facet joint osteoarthrits on the segmental flexibility of the lumbar spine. Spine. 2000, 25 (23): 3036-44. 10.1097/00007632-200012010-00011.
Kumaresan S, Yoganandan N, Pintar FA, Maiman DJ, Goel VK: Contribution of disc degeneration to osteophyte formation in the cervical spine: a biomechanical investigation. J of Orthopaedic Research. 2001, 19: 977-984. 10.1016/S0736-0266(01)00010-9.
Pal GP, Shrek HH: The vertical stability of the cervical spine. Spine. 1988, 5: 447-9.
Pellengahr C, Pfahler M, Kuhr M, Hohmann D: Influence of facet joint angle and asymmetric disc collapse on degenerative olisthesis of the cervical spine. Orthopedics. 2000, 23: 697-701.
Yoganandan N, Kumaresan S, Pintar FA: Biomechanics of the cervical spine part 2. Cervical spine soft tissue response and biomechanical modeling. Clinical Biomechanics. 2001, 16: 1-27. 10.1016/S0268-0033(00)00074-7.
Donner A, Eliasziw M: Sample size requirement for reliability studies. Statistics in Medicine. 1987, 6: 441-8.
Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics. 1977, 33 (1): 159-74.
Keats TE: Atlas of Normal Roentgen Variants that may Simulate Disease. 1991, St. Louis (MO): Mosby Year Book, Inc
Haas M: Statistical methodology for reliability studies. J Manipulative Physiol Ther. 1991, 14 (2): 119-32.
Resnick D, Niwayama G: Diagnosins of bone and joint disorder. 2002, Philadelphia (PA): W.B. Saunders Company, 2:
Cook J, Peterson CK: Intervertebral disc, apophysial and uncovertebral joint degeneration in the cervical spine: reliability of radiological diagnosis [abstract]. European Journal of Chiropractic. 2003, 48 (2): 63-
Bolton PS, Ware AE: Degenerative joint disease in the cervical spine of chiropractic patients. J Aust Chiropractors' Assoc. 1988, 18: 51-4.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/4/28/prepub
Acknowledgements
We would like to thank Dr. Cam McDermaid and Ms. Carol Hagino for their input. As well, we would like to thank the CMCC HK Lee Clinic for permitting us access to the necessary radiology files. The authors were unable to locate the patients featured in the radiographs (Figures 1, 2, 3), so consent was not obtained from the patients or their relatives for publication of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Stupar, M., Mauron, D. & Peterson, C.K. Inter-examiner reliability of the diagnosis of cervical pillar hyperplasia (CPH) and the correlation between CPH and spinal degenerative joint disease (DJD). BMC Musculoskelet Disord 4, 28 (2003). https://doi.org/10.1186/1471-2474-4-28
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-4-28