Abstract
Background
Idiopathic pulmonary fibrosis (IPF) is a distinct form of interstitial pneumonia with unknown origin and poor prognosis. Current pharmacologic treatments are limited and lung transplantation is a viable option for appropriate patients. The aim of this review was to summarize lung transplantation survival in IPF patients overall, between single (SLT) vs. bilateral lung transplantation (BLT), pre- and post Lung Allocation Score (LAS), and summarize wait-list survival.
Methods
A systematic review of English-language studies published in Medline or Embase between 1990 and 2013 was performed. Eligible studies were those of observational design reporting survival post-lung transplantation or while on the wait list among IPF patients.
Results
Median survival post-transplantation among IPF patients is estimated at 4.5 years. From ISHLT and OPTN data, one year survival ranged from 75% - 81%; 3-year: 59% - 64%; and 5-year: 47% - 53%. Post-transplant survival is lower for IPF vs. other underlying pre-transplant diagnoses. The proportion of IPF patients receiving BLT has steadily increased over the last decade and a half. Unadjusted analyses suggest improved long-term survival for BLT vs. SLT; after adjustment for patient characteristics, the differences tend to disappear. IPF patients account for the largest proportion of patients on the wait list and while wait list time has decreased, the number of transplants for IPF patients has increased over time. OPTN data show that wait list mortality is higher for IPF patients vs. other diagnoses. The proportion of IPF patients who died while awaiting transplantation ranged from 14% to 67%. While later transplant year was associated with increased survival, no significant differences were noted pre vs. post LAS implementation; however a high LAS vs low LAS was associated with decreased one-year survival.
Conclusions
IPF accounts for the largest proportion of patients awaiting lung transplants, and IPF is associated with higher wait-list and post-transplant mortality vs. other diagnoses. Improved BLT vs. SLT survival may be the result of selection bias. Survival pre- vs. post LAS appears to be similar except for IPF patients with high LAS, who have lower survival compared to pre-LAS. Data on post-transplant morbidity outcomes are sparse.
Similar content being viewed by others
Background
Idiopathic pulmonary fibrosis (IPF), characterized histopathologically and/or radiologically with a usual interstitial pneumonia (UIP) pattern, is the most common adult form of interstitial pneumonia of unknown origin [1]. Progressive deterioration of lung function in patients with IPF is associated with poor prognosis. Natural histories for patients with IPF vary. In most patients, the disease progresses slowly and gradually over many years. Some patients remain stable, while others have accelerated decline often associated with episodes of acute respiratory worsening or exacerbations [2–4]. The median survival time for patients with IPF is 2 to 3 years from diagnosis and the 5-year survival rate ranges between 30% and 50% [1, 5–7].
There is no cure for IPF and treatment options are limited. Historically, available pharmacological therapies had limited efficacy and potential serious side effects; therefore, international guidelines concluded that there is no therapy with proven benefit to date [1]. However, just recently both nintedanib and pirfenidone have been shown to slow disease progression in separate Phase III clinical trials and for the first time, two treatment alternatives might become available for IPF patients [8, 9]. Lung transplantation is so far the only treatment with proven benefit, conferring a better survival for some carefully selected patients. However, the number of lung transplantations performed is limited primarily by the supply of donor organs [10], and survival is poor for IPF patients relative to most other disease categories [11, 12].
In May 2005 the United Network for Organ Sharing (UNOS) implemented the Lung Allocation Score (LAS) in the United States (US). The LAS has been utilized in Germany since December 2011, and the international exchange of donor lungs between all Eurotransplant countries is now based upon LAS. The LAS is an effort to identify the best candidates for transplant. The score is calculated using various measures of a patient’s health that estimate survival probability and projected duration of survival with or without a lung transplant. LAS scores range from 0–100 and patients with higher scores, reflecting greater predicted survival benefit, get priority. Implementation of the LAS resulted in an increased number of IPF patients receiving a lung transplant, and IPF became the most common diagnosis group to receive a lung transplant in the US in 2007 [13]. Since the implementation of the LAS system in the US, the percentage of patients on the wait list with restrictive lung disease (i.e., IPF or re-transplants) has increased from 33.8% to 46.1% [11].
Both single and bilateral lung transplantations are performed in patients with IPF, and debate remains as to whether single lung transplantation (SLT) or bilateral lung transplantation (BLT) is the better choice in this particular indication [14].
To our knowledge this is the first systematic review undertaken to summarize the published evidence on lung transplantation in IPF patients. The specific goals of this review were to summarize the published evidence on survival following lung transplantation in IPF patients, survival for SLT vs. BLT, survival post-transplant vs. wait-list survival, and survival pre- and post- LAS implementation. Data on peri-transplant complications and hospital length of stay following transplantation were summarized to the extent that data were available.
Methods
Literature search
A protocol detailing the methodology of this systematic review was developed. The methods used to perform this review involved both electronic and manual components, and followed established best methods used in the science of systematic review research [15–17]. A literature search was performed in MEDLINE and EMBASE to identify all English-language observational studies, published from 1990 to March 2013, reporting on lung transplantation in patients with an underlying diagnosis of IPF. Additional file 1 details the specific search strategy used. The electronic searches were supplemented by a manual search of the reference lists of all accepted studies, as well as the reference lists of recent relevant reviews. Data reported on the Organ Procurement and Transplantation Network (OPTN) and the International Society for Heart and Lung Transplantation (ISHLT) websites were also used in this review.
Study identification
In the initial screening, abstracts were reviewed for obvious exclusion criteria, which included, guidelines, animal and in vitro studies, case reports, meta-analyses, clinical trials, and studies with no IPF patients or no lung transplantation. The full-text publications of accepted abstracts were reviewed to satisfy all of the pre-specified inclusion criteria. Eligible studies were those of observational design reporting on at least 10 patients with IPF who underwent lung transplantation, and reporting survival outcomes in IPF patients after lung transplantation or while on the waiting list for transplantation. Studies that only reported outcomes for a population with mixed diagnoses, such as all pulmonary fibrosis patients, without reporting IPF data separately were excluded. The most recent published reports from the ISHLT (2012 report) and the OPTN (2011 report) were included. The agreement of two investigators was required to accept or reject any articles during the review process.
Data extraction and synthesis
Data elements of interest from each accepted study were extracted to a data extraction form. Extracted information included study-level characteristics, patient-level characteristics, and outcomes of interest. One investigator extracted the data from each study, and a second investigator independently reviewed the extracted data for completeness and accuracy.
Results
Study selection
After removing duplicates from the various sources, the entire literature search, including manual bibliography checks, identified 1,375 citations. The majority of these citations were rejected during abstract screening, and 385 full-text articles were retrieved and screened against the protocol-specified inclusion criteria. Of these, 331 were rejected after full-text review, leaving 54 publications included in this systematic review. A flow diagram of the study attrition is presented in Figure 1.
Study characteristics
A summary of the 56 sources (54 papers and the ISHLT and OPTN websites) is displayed in Additional file 2. The number of IPF patients in the studies ranged from 11 to 8,904. Thirteen of the 54 papers (24%) reported analyses of the OPTN data; two were analyses of the ISHLT data; six were reports of analyses from other registries or large databases; 18 papers reported data from single centers from North America; 12 papers reported data from single centers from Europe; two were from single centers from Brazil and one was a report from a single center from Australia. The mean age of the IPF patients included in the analyses was reported in 27 papers and ranged from 45.2 to 65.4 years; gender of the IPF patients was reported in 26 papers – the proportion of female patients ranged from 18.8% to 56.3%.
Post-transplant survival
Table 1 displays a summary of post-transplant survival among IPF patients from the ISHLT and OPTN data and from the papers included in this review.
From the 8,528 IPF patients transplanted from 1990 to 2011 and reported to the ISHLT, the median survival was 4.5 years [12]. Survival one year post-transplantation was 75%, which decreased to 59%, 47%, and 24% at three, five, and ten years post-transplantation, respectively [12]. Post-transplant survival for IPF patients (median 4.5 years) was significantly (P ≤ 0.001) lower compared to patients with pre-transplant diagnoses of cystic fibrosis (CF; 7.8 years), chronic obstructive pulmonary disease (COPD; 5.4 years), or Alpha-1 - antitrypsin deficiency (6.3 years) [12]. From the 2011 OPTN Annual Report, among all US lung transplants performed in IPF patients from 2005 to 2006, survival at one year post-transplantation was 81%, which decreased to 64% at three years’ post-transplantation and 53% at five years’ post-transplantation [11]. Data available via the OPTN web site demonstrated that long-term post-transplant survival among US IPF lung transplant recipients transplanted between 1997 – 2004 was lower (3-year: 57%; 5-year: 41%) [19]. Several papers reported post-transplant survival among IPF patients from analyses of the OPTN data [20–26]; one year survival ranged from ~68% to 80%, 3-year survival ranged from 50% to 61%, and 5-year from 32% to 49%. Analyses that included earlier transplant dates tended to have lower survival than those with more recent transplant dates.
Two papers reported results from analyses of large databases other than the OPTN or ISHLT. An analysis of transplants among IPF patients from 2006 – 2010 included in the Spanish Lung Transplant Registry reported 3-month post-transplant survival of ~80% and 1-year survival of ~63% [27]. An analysis of the US Nationwide Inpatient Sample from 1988 to 2006 found that in-hospital survival among IPF patients who received lung transplants was 91% [28].
Several papers reported post-transplant survival among IPF patients from single centers across Europe and North America; one paper each reported outcomes from single centers in Brazil and Australia [29–50]. The studies included transplants performed from 1983 – 2010 and had small sample sizes (11 – 89 IPF patients). Survival at one year post-transplantation ranged from 25% to 87%; at 3 years from 40% to 67%; and at five years from 33% to 63%.
Single vs. bilateral lung transplantation
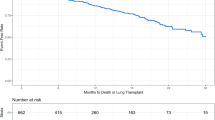
The proportion of BLT vs. SLT procedures among IPF patients included in the ISHLT database has steadily increased since 1997 (Figure 2). In 2011, 53.5% of lung transplants among IPF patients reported to the ISHLT database were BLT and 46.5% were SLT [12, 18]. In 2011, BLT accounted for 70.1% of the total number of US lung transplants (proportion of transplants among IPF patients that were BLT vs. SLT was not reported) [11]. Unadjusted analyses suggested improved long-term survival for BLT vs. SLT; (Table 2) after adjustment for patient characteristics, the differences tended to disappear.
For lung transplants received by IPF patients from 1990 to June 2011 and reported to the ISHLT, survival was significantly (P < 0.001) better for BLT vs. SLT [12]. At one year post-transplant, the proportion of IPF patients alive was similar between BLT (73.9%) and SLT (74.8%); long-term follow-up showed that a greater proportion of IPF patients who received BLT vs. SLT were alive (3-year post-transplant, BLT: 63.0%; SLT: 56.7%; 5-year: BLT: 49.4%; SLT: 43.3%; 10-year: BLT: 34.9%; SLT: 20.0%) [12].
Data from the OPTN also suggest improved survival for BLT vs. SLT. Among 3,830 IPF patients included in an analysis of the OPTN data who received transplants between 1997 and 2008, patients who received a BLT had significantly (P < 0.001) longer mean survival (8.34 years) compared to patients who received a SLT (7.37 years), (HR for mortality: 0.798 [95% CI 0.716 to 0.889]) [51]. Long-term survival, conditional to surviving one-year, was also significantly (P < 0.0006) better for patients who received a BLT vs. SLT (12.08 years versus 6.8 years) [51]. At five years’ post-transplantation, approximately 60% and 53% of patients who received BLT and SLT transplants, respectively, were alive [51]. At ten years’ post-transplantation, approximately 48% and 30% of patients who received BLT and SLT transplants, respectively, were alive [51]. An analysis of the OPTN data that included 92 (27 BLT) adults with IPF transplanted from 1987 to 1997 who survived ≥10 years after their first lung transplant and 205 (30 BLT) adults with IPF who received an allograft within the same era (1987–1997) and died between 1 and 5 years after lung transplantation, found that longer post-transplant survival among IPF patients was associated with BLT – 29.4% of 10-year survivors underwent BLT compared to only 14.6% of 1–5-year survivors (P = 0.003) [54]. Another analysis of the OPTN data that included 3,327 IPF patients transplanted between 1997 and 2009 also found significantly (P < 0.001) longer median survival after BLT (5.2 years [95% CI, 4.3 to 6.7 years]) vs. SLT (3.8 years [95% CI, 3.6 to 4.1 years]) [21]. However, the difference was not evident in an analysis restricted to 1,218 patients who had lung transplantation from 2002 onward (BLT: 5.0 years vs SLT: 4.6 years, P = 0.29). An unadjusted analysis suggested lower mortality with BLT vs. SLT (HR: 0.80 [95% CI, 0.71 to 0.89]), but the effect was no longer statistically significant after adjustment for recipient, donor, and procedure-related variables (HR: 0.92 [95% CI, 0.81 to 1.06]) [21]. The authors conducted further analyses and concluded that there was possibly an increased relative risk for death with BLT in the early postoperative period, followed by a decreased relative risk for death long-term [21]. A single center study from the US of 82 IPF patients who received a lung transplant found that one and five year survival was significantly greater following BLT vs. SLT [48]. However, when BLT vs. SLT survival was assessed using IPF patients matched on potential risk factors, there was no significant difference between transplantation types (P = 0.3). The matched analysis was limited by a very small sample of 10 BLT and 10 SLT patients. The authors suggested that SLT was a marker for a high-risk subgroup of older patients with IPF, rather than being a true risk factor for increased mortality [48].
Other analyses, including 1994 – 2004 data from the ISHLT [55], OPTN data [52], a single center study from the US [50], and a single center study from Australia [37], found no statistically significant difference in the survival between IPF patients receiving BLT and receiving SLT. However, survival tended to be numerically greater for BLT vs. SLT.
In contrast, an analysis of the Eurotransplant data which includes data from Austria, Belgium, Germany, The Netherlands, Luxembourg and Slovenia, found that 3-year survival among 104 transplants received between 1997 – 1999, was significantly (P = 0.04) better for SLT (63%) compared to BLT (47%) in IPF patients [53].
Two papers reported data on post-transplant in-patient mortality. From an analysis of the US National Inpatient Sample database, in-hospital death was significantly (P = 0.006) greater following SLT (16%) vs. BLT (5%) [28]. From a small single center study from the US that included 45 IPF patients, there was no significant difference in in-hospital mortality between BLT (9.4%) and SLT (9.4%) [41].
Post-transplant survival vs. wait list survival
In 2011, patients with IPF accounted for the largest proportion (46.1%) of patients on the lung transplant wait-list in the US [19]. The median time on wait list to transplant for IPF patients in the US has decreased from 4.1 months in 2005 to 2.1 months in 2011 [19]. Correspondingly, the percent of adults with IPF on the wait list who received a lung transplant within a year increased from 27% in 1998 to 71.2% in 2010 [19]. Despite the fact that the median wait-list time to transplant was lower for IPF vs. other diagnosis categories and that the transplant rate was highest among IPF patients (165.9/100 person-years of waiting time vs. 119.5, 46.9, and 66.3 for patients with obstructive lung disease, pulmonary vascular disease, and CF, respectively), OPTN data show that the pre-transplant mortality rate among adult IPF patients wait-listed for a lung transplant (26.9 / 100 patient years of waiting time) was higher for IPF vs. other underlying causes of disease (Table 3) [19]. An analysis of 61 IPF patients awaiting lung transplantation in five institutions and listed in The Korean Network for Organ Sharing (KONOS) from May 1996 to May 2011, found that mean survival time for IPF patients who died on the waiting list was 7.9 ± 15.5 months [56]. An analysis of 24 IPF patients referred for lung transplantation and lung-and-heart transplantation at a single center in Poland between September 1999 and December 2004 found that the mean time to death was 11.6 ± 10.5 months [57].
From the 13 papers that reported data on wait list mortality in IPF patients, the proportion of IPF patients who died while awaiting transplantation ranged from 14% to 67% (Table 4). An analysis of 53 IPF patients enrolled at a lung transplant program in Italy and assessed over a 100 month study period, found that mortality rate before lung transplantation for IPF was higher than after lung transplantation (44% vs 16%) [58]. An analysis that included 134 patients in the UK and Ireland found that, of those who died while awaiting lung transplantation, IPF was the leading cause of death. Among all lung transplant recipients and wait-list patients (regardless of underlying diagnosis), survival was significantly (P < 0.001) better among those who received a transplant [59]. From a single center study in France that included 46 IPF patients on the waiting list from 1988 to July 2001, lung transplantation in patients with IPF was associated with a 75% reduction in the risk of death (HR: 0.25 [95% CI: 0.08-0.86] P = 0.03) [33].
Cause of death among IPF patients
Among IPF patients who received a lung transplant in the US from 1987 to 2009, the leading cause of death was infection (24% of deaths) [21]; papers from single center studies and one dual center study, also reported that infection or sepsis was a leading cause of death [33, 34, 39, 41, 42, 45, 48, 69], along with bronchiolitis obliterans syndrome (BOS), chronic rejection [33, 34, 41, 42, 45, 47], or unspecified graft failure [70], (Additional file 3).
Burden post-transplantation
Few papers reported information on post-transplant burden. The papers that did report post-transplant hospital length of stay and adjunct interventions suggest that lung transplantation in IPF patients is associated with substantial resource use (Additional file 4).
Transplant era and LAS score
From the ISHLT data, a multivariable analysis of 4,463 IPF patients who received lung transplants from 1999 – 2011 found that patients transplanted from 2010 to 2011 had a significantly decreased 1-year mortality risk compared to patients transplanted between 2005 – 2006 (2005/2006 vs. 2010/2011: HR: 1.46 [95% CI: 1.2 – 1.8] P = 0.0013); 2003 – 2004 (HR: 1.70 [95% CI: 1.3 – 2.2] P < 0.001); 2001 – 2002 (HR: 1.99 [95% CI: 1.5 – 2.7] P < 0.001); and 1999 – 2000 (HR: 2.98 [95% CI: 2.2 – 4.0] P < 0.0001) [12]. Patients transplanted from 2007 – 2008 had a borderline increased 1-year mortality risk compared to patients transplanted from 2010 – 2011 (HR: 1.24 [95% CI 1.0 – 1.5] P = 0.0525) [12].
An analysis of the OPTN data which compared patients transplanted post-LAS (May 1, 2005 until April 30, 2008) to those transplanted pre-LAS (i.e., from May 1, 2002 through April 30, 2005) found that, among all lung transplant patients regardless of underlying diagnosis, survival at one year post-transplantation was similar between the pre- and post-LAS periods [71]. A single center study from the US found no significant (P = 0.98) difference in long-term survival for IPF patients transplanted pre-LAS (n = 33) vs. post-LAS (n = 46) [49]. For the pre-LAS group, actuarial survival at 1 and 3 years were 78.8% and 63.6%, respectively. For the post-LAS group, actuarial survival at 1 and 3 years were 85.8% and 62.8%, respectively.
From an analysis of the OPTN data, IPF patients with high LAS (>46) had significantly (P = 0.01) decreased one year survival (76.4%) compared to IPF patients with a low LAS (≤46) (82.6%) [71]. Compared to IPF patients in the pre-LAS group, IPF patients with LAS ≤46 did not have elevated risk of death (HR: 0.98 [95% CI 0.79–1.22]), though IPF patients with LAS >46 did (HR: 1.39 [95% CI: 1.07–1.81]) [71]. A single center study from the US also found that IPF patients with a high LAS (≥50) had significantly (P = 0.013) poorer one year survival (65.1%) compared to IPF patients with a low-LAS (<50) (79.9%) [72].
Discussion
Lung transplantation is now a well-accepted treatment option for the management of a wide range of chronic end-stage lung disorders, including IPF. The primary goal of lung transplantation is to provide a survival benefit for patients who are failing medical therapy or for whom there is no effective medical treatment. However, there are far fewer available donor organs than patients that would potentially benefit from the lung transplantation procedure. In 2011, approximately 886 IPF patients in the US underwent lung transplantation [19]. Using a prevalence of 14–43 per 100,000 [73] and a US adult population of approximately 311 million in 2011 [74], less than 1% of the estimated 42,000–130,000 US IPF patients had received a lung transplant during 2011. Not all IPF patients would be eligible for or willing to undergo transplantation, thus this probably overestimates the proportion not receiving a transplant. Nonetheless, there remains a large gap between those eligible and those receiving a transplant. Therefore, it is important that the available resources are optimally used, so that the patients selected for transplantation have the best chances for favorable long-term outcomes. There is no cure for IPF and current guidelines for the selection of lung transplant candidates recommend that appropriate IPF patients should be referred for transplantation as early as possible [75].
In this review we summarized lung transplantation outcomes in IPF patients using recent evidence. The published data and publically available data from the OPTN and ISHLT demonstrate that approximately 50% of IPF patients are alive at five years’ post-transplantation. IPF patients continue to have poorer survival compared to lung transplant patients with other underlying diagnoses. IPF patients also have a higher wait-list mortality compared to other diagnoses. The high proportion of IPF patients dying prior to receipt of a lung transplant and the low survival time among those who do die, support the benefits of lung transplantation as a treatment for IPF patients as well as the high unmet need in this patient population. However, there is the potential for a survivor treatment selection bias in the comparison of wait list vs. post-transplant survival — IPF patients who receive lung transplants have to live long enough to receive a donor lung, so if they are compared to the non-transplant group they may appear to have better survival. There has been a significant increase in the proportion of IPF patients receiving BLT vs. SLT. Data tend to suggest that BLT is associated with improved long-term survival compared to SLT. However, the apparent improved long-term survival may be due to the SLT patients being at higher risk for poor survival rather than effects of the BLT per se. Given the shortage of donor lungs available, it is important to understand whether there is a subgroup of IPF patients for whom BLT does offer a true survival advantage and whether it would be beneficial to reserve bilateral transplants for those patients. Data specifically comparing survival among IPF patients who received a lung transplant pre- vs. post-LAS are limited. However, implementation of the LAS has resulted in an increase in lung transplants due to IPF, and has resulted in shorter wait times when compared to patients in the pre-LAS period (due to patients being listed later since wait time is no longer a primary factor in determining allocation, and due to the fact that IPF patients are selected for transplants based on their LAS). The ISHLT data show that longer 1 year survival is associated with more recent transplant year; this could be an effect of the LAS system but may also be due to other factors such as improvements in medical care and immunosuppression drug regimens. Other than mortality data, there are few reported data on post- or peri-transplant outcomes among IPF patients. The data reported in the papers included in this review suggest that transplantation for IPF is associated with considerable resource allocation beyond the actual transplantation procedure; this includes substantial ICU length of stay as well as necessity for adjunct interventions such as tracheostomy and use of inhaled nitric oxide and prolonged mechanical ventilation.
To our knowledge, this is the first systematic and most extensive review of the available evidence on lung transplantation outcomes in IPF patients, evaluating the published literature over more than two decades. The systematic methodology employed for this effort and the extensive nature of the outcomes assessed (i.e., wait list and post-transplant survival; pre- vs. post-LAS survival; BLT vs. SLT survival; post-transplant morbidity) are strengths of this review. A substantial amount of the reviewed evidence was derived from OPTN or ISHLT data. While the availability if the OPTN and ISHLT data contributes extensively to the understanding of post-transplant survival, detailed post-transplant outcomes are not collected. A limitation of the data summarized in this review is the lack of actual confirmation of IPF in most of the studies.
Conclusions
This review highlights that data on post-transplant morbidity and resource use outcomes among IPF patients compared to other lung transplant patients are lacking. In addition, a greater understanding of which IPF patients should receive BLT is needed. While lung transplant appears to offer a survival advantage when compared to wait list IPF patients, IPF patients still have the lowest survival of all lung transplant patients; this coupled with the lack of available donor lungs, suggests a high need for effective medical therapy.
Authors’ information
Note: Luba Nalysnyk was employed by United BioSource Corporation at the time of the review.
Abbreviations
- BLT:
-
Bilateral lung transplantation
- BOS:
-
Bronchiolitis obliterans syndrome
- CF:
-
Cystic fibrosis
- COPD:
-
Chronic obstructive pulmonary disease
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IPF:
-
Idiopathic pulmonary fibrosis
- ISHLT:
-
International Society for Heart and Lung Transplantation
- KONOS:
-
Korean Network for Organ Sharing
- LAS:
-
Lung Allocation Score
- OPTN:
-
Organ Procurement and Transplantation Network
- SLT:
-
Single lung transplantation
- UIP:
-
Usual interstitial pneumonia
- UK:
-
United Kingdom
- UNOS:
-
United Network for Organ Sharing
- US:
-
United States.
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ, ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis: An Official ATS/ERS/JRS/ALAT Statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011, 183 (6): 788-824. 10.1164/rccm.2009-040GL.
Selman M, Carrillo G, Estrada A, Mejia M, Becerril C, Cisneros J, Gaxiola M, Pérez-Padilla R, Navarro C, Richards T, Dauber J, King TE, Pardo A, Kaminski N: Accelerated variant of idiopathic pulmonary fibrosis: clinical behavior and gene expression pattern. PLoS One. 2007, 2: e482-10.1371/journal.pone.0000482.
Song JW, Hong S-B, Lim C-M, Koh Y, Kim DS: Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J. 2011, 37 (2): 356-363. 10.1183/09031936.00159709.
Collard HR, Moore BB, Flaherty KR, Brown KK, Kaner RJ, King TE, Lasky JA, Loyd JE, Noth I, Olman MA, Lasky JA, Loyd JE, Noth I, Olman MA, Raghu G, Roman J, Ryu JH, Zisman DA, Hunninghake GW, Colby TV, Egan JJ, Hansell DM, Johkoh T, Kaminski N, Kim DS, Kondoh Y, Lynch DA, Müller-Quernheim J, Myers JL, Nicholson AG, Selman M, Toews GB, Wells AU, Martinez FJ, Idiopathic Pulmonary Fibrosis Clinical Research Network Investigators: Acute Exacerbations of Idiopathic Pulmonary Fibrosis. Am J Respir Crit Care Med. 2007, 176 (7): 636-643. 10.1164/rccm.200703-463PP.
Rudd RM, Prescott RJ, Chalmers JC, Johnston IDA: British Thoracic Society Study on cryptogenic fibrosing alveolitis: response to treatment and survival. Thorax. 2007, 62 (1): 62-66. 10.1136/thx.2005.045591.
Mapel DW, Hunt WC, Utton R, Baumgartner KB, Samet JM, Coultas DB: Idiopathic pulmonary fibrosis: survival in population based and hospital based cohorts. Thorax. 1998, 53 (6): 469-476. 10.1136/thx.53.6.469.
Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, Offord KP: Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998, 157 (1): 199-203. 10.1164/ajrccm.157.1.9704130.
King TE, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, Gorina E, Hopkins PM, Kardatzke D, Lancaster L, Lederer DJ, Nathan SD, Pereira CA, Sahn SA, Sussman R, Swigris JJ, Noble PW, ASCEND Study Group: A Phase 3 Trial of Pirfenidone in Patients with Idiopathic Pulmonary Fibrosis. N Engl J Med. 2014, 370 (22): 2083-2092. 10.1056/NEJMoa1402582.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, Cottin V, Flaherty KR, Hansell DM, Inoue Y, Kim DS, Kolb M, Nicholson AG, Noble PW, Selman M, Taniguchi H, Brun M, Le Maulf F, Girard M, Stowasser S, Schlenker-Herceg R, Disse B, Collard HR, INPULSIS Trial Investigators: Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis. N Engl J Med. 2014, 370 (22): 2071-2082. 10.1056/NEJMoa1402584.
Glanville AR, Estenne M: Indications, patient selection and timing of referral for lung transplantation. Eur Respir J. 2003, 22 (5): 845-852. 10.1183/09031936.03.00039003.
Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR): OPTN/SRTR 2011 Annual Data Report. 2012, Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation
Adult Lung Transplantation Statistics. [https://www.ishlt.org/registries/slides.asp?slides=heartLungRegistry]
Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, Coke MA, Garrity ER, Sweet SC, Heiney DA, Grover FL: Development of the New Lung Allocation System in the United States. Am J Transplant. 2006, 6 (5p2): 1212-1227. 10.1111/j.1600-6143.2006.01276.x.
Rinaldi M, Sansone F, Boffini M, El Qarra S, Solidoro P, Cavallo N, Ruffini E, Baldi S: Single versus double lung transplantation in pulmonary fibrosis: a debated topic. Transplant Proc. 2008, 40 (6): 2010-2012. 10.1016/j.transproceed.2008.05.052.
Higgins JPT, Green S: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. 2011, The Cochrane Collaboration, Available from http://www.cochrane-handbook.org
Cook DA, West CP: Conducting systematic reviews in medical education: a stepwise approach. Med Educ. 2012, 46 (10): 943-945. 10.1111/j.1365-2923.2012.04328.x.
Cook DJ, Mulrow CD, Haynes RB: Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997, 126 (5): 376-380. 10.7326/0003-4819-126-5-199703010-00006.
Christie JD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, Kirk R, Rahmel AO, Stehlik J, Hertz MI: The Registry of the International Society for Heart and Lung Transplantation: 29th Adult Lung and Heart-Lung Transplant Report—2012. J Heart Lung Transplant. 2012, 31 (10): 1073-1086. 10.1016/j.healun.2012.08.004.
OPTN data. [http://optn.transplant.hrsa.gov/latestData/rptData.asp]
Meyer KC: Lung transplant for interstitial lung disease. Clin Pulm Med. 2000, 7 (4): 178-186. 10.1097/00045413-200007040-00003.
Thabut G, Christie JD, Ravaud P, Castier Y, Dauriat G, Jebrak G, Fournier M, Leseche G, Porcher R, Mal H: Survival after bilateral versus single-lung transplantation for idiopathic pulmonary fibrosis. Ann Intern Med. 2009, 151 (11): 767-774. 10.7326/0003-4819-151-11-200912010-00004.
Edwards LB, Keck BM: Thoracic organ transplantation in the US. Clin Transpl. 2002, 29-40.
McCurry KR, Shearon TH, Edwards LB, Chan KM, Sweet SC, Valapour M, Yusen R, Murray S: Lung transplantation in the United States, 1998-2007. Am J Transplant. 2009, 9 (4 Pt 2): 942-958.
Chen H, Shiboski SC, Golden JA, Gould MK, Hays SR, Hoopes CW, De Marco T: Impact of the lung allocation score on lung transplantation for pulmonary arterial hypertension. Am J Respir Crit Care Med. 2009, 180 (5): 468-474. 10.1164/rccm.200810-1603OC.
Freitas MC: Trend in lung transplantation in the U.S.: an analysis of the UNOS registry. Clin Transpl. 2010, 17-33.
Takagishi T, Ostrowski R, Alex C, Rychlik K, Pelletiere K, Tehrani R: Survival and extrapulmonary course of connective tissue disease after lung transplantation. J Clin Rheumatol. 2012, 18 (6): 283-289. 10.1097/RHU.0b013e3182676089.
Coll E, Santos F, Ussetti P, Canela M, Borro JM, De La Torre M, Varela A, Zurbano F, Mons R, Morales P, Pastor J, Salvatierra A, de Pablo A, Gámez P, Moreno A, Solé J, Román A: The Spanish Lung Transplant Registry: first report of results (2006-2010). Arch Bronconeumol. 2013, 49 (2): 70-78. 10.1016/j.arbres.2012.06.001.
Teo AT, Pietrobon R, Atashili J, Rajgor D, Shah J, Martins H: Short-term outcomes of lung transplant in idiopathic pulmonary fibrosis. Eur Surg - Acta Chir Austriaca. 2011, 43 (5): 284-294. 10.1007/s10353-011-0618-6.
Burton CM, Carlsen J, Mortensen J, Andersen CB, Milman N, Iversen M: Long-term Survival After Lung Transplantation Depends on Development and Severity of Bronchiolitis Obliterans Syndrome. J Heart Lung Transplant. 2007, 26 (7): 681-686. 10.1016/j.healun.2007.04.004.
Nathan SD, Shlobin OA, Weir N, Ahmad S, Kaldjob JM, Battle E, Sheridan MJ, du Bois RM: Long-term course and prognosis of idiopathic pulmonary fibrosis in the new millennium. Chest. 2011, 140 (1): 221-229. 10.1378/chest.10-2572.
Nathan SD, Barnett SD, Urban BA, Nowalk C, Moran BR, Burton N: Pulmonary embolism in idiopathic pulmonary fibrosis transplant recipients. Chest. 2003, 123 (5): 1758-1763. 10.1378/chest.123.5.1758.
McNeil K, Higenbottam T: The long-term outcome of lung transplantation in interstitial lung disease. Clin Pulm Med. 1996, 3 (3): 137-141. 10.1097/00045413-199605000-00003.
Thabut G, Mal H, Castier Y, Groussard O, Brugiere O, Marrash-Chahla R, Leseche G, Fournier M: Survival benefit of lung transplantation for patients with idiopathic pulmonary fibrosis. J Thorac Cardiovasc Surg. 2003, 126 (2): 469-475. 10.1016/S0022-5223(03)00600-7.
Neurohr C, Huppmann P, Thum D, Leuschner W, von Wulffen W, Meis T, Leuchte H, Baumgartner R, Zimmermann G, Hatz R, Czerner S, Frey L, Ueberfuhr P, Bittmann I, Behr J, Munich Lung Transplant Group: Potential functional and survival benefit of double over single lung transplantation for selected patients with idiopathic pulmonary fibrosis. Transpl Int. 2010, 23 (9): 887-896.
Algar FJ, Espinosa D, Moreno P, Illana J, Cerezo F, Alvarez A, Baamonde C, Redel J, Vaquero JM, Santos F, Salvatierra A: Results of lung transplantation in idiopathic pulmonary fibrosis patients. Transplant Proc. 2010, 42 (8): 3211-3213. 10.1016/j.transproceed.2010.05.046.
Machuca TN, Schio SM, Camargo SM, Lobato V, Costa CD, Felicetti JC, Moreira JS, Camargo JJ: Prognostic factors in lung transplantation: the Santa Casa de Porto Alegre experience. Transplantation. 2011, 91 (11): 1297-1303. 10.1097/TP.0b013e31821ab8e5.
Keating D, Levvey B, Kotsimbos T, Whitford H, Westall G, Williams T, Snell G: Lung transplantation in pulmonary fibrosis: challenging early outcomes counterbalanced by surprisingly good outcomes beyond 15 years. Transplant Proc. 2009, 41 (1): 289-291. 10.1016/j.transproceed.2008.10.042.
Di Giuseppe M, Gambelli F, Hoyle GW, Lungarella G, Studer SM, Richards T, Yousem S, McCurry K, Dauber J, Kaminski N, Leikauf G, Ortiz LA: Systemic inhibition of NF-kappaB activation protects from silicosis. PLoS One. 2009, 4 (5): e5689-10.1371/journal.pone.0005689.
Schachna L, Medsger TA, Dauber JH, Wigley FM, Braunstein NA, White B, Steen VD, Conte JV, Yang SC, McCurry KR, Borja MC, Plaskon DE, Orens JB, Gelber AC: Lung transplantation in scleroderma compared with idiopathic pulmonary fibrosis and idiopathic pulmonary arterial hypertension. Arthritis Rheum. 2006, 54 (12): 3954-3961. 10.1002/art.22264.
Rivera-Lebron BN, Forfia PR, Kreider M, Lee J, Holmes JH, Kawut SM: Echocardiographic and Hemodynamic Predictors of Mortality in Idiopathic Pulmonary Fibrosis. Chest. 2013, 144 (2): 564-570. 10.1378/chest.12-2298.
Meyers BF, Lynch JP, Trulock EP, Guthrie T, Cooper JD, Patterson GA: Single versus bilateral lung transplantation for idiopathic pulmonary fibrosis: a ten-year institutional experience. J Thorac Cardiovasc Surg. 2000, 120 (1): 99-107. 10.1067/mtc.2000.106322.
Saggar R, Khanna D, Furst DE, Belperio JA, Park GS, Weigt SS, Kubak B, Ardehali A, Derhovanessian A, Clements PJ, Shapiro S, Hunter C, Gregson A, Fishbein MC, Lynch Iii JP, Ross DJ, Saggar R: Systemic sclerosis and bilateral lung transplantation: a single centre experience. Eur Respir J. 2010, 36 (4): 893-900. 10.1183/09031936.00139809.
Milstone AP, Brumble LM, Loyd JE, Ely EW, Roberts JR, Pierson RN, Dummer JS: Active CMV infection before lung transplantation: risk factors and clinical implications. J Heart Lung Transplant. 2000, 19 (8): 744-750. 10.1016/S1053-2498(00)00134-0.
Smith PW, Wang H, Parini V, Zolak JS, Shen KR, Daniel TM, Robbins MK, Tribble CG, Kron IL, Jones DR: Lung transplantation in patients 60 years and older: results, complications, and outcomes. Ann Thorac Surg. 2006, 82 (5): 1835-1841. 10.1016/j.athoracsur.2006.05.036. discussion 1841
Wille KM, Gaggar A, Hajari AS, Leon KJ, Barney JB, Smith KH, Pajaro O, Wang W, Oster RA, McGiffin DC, Young KR: Bronchiolitis obliterans syndrome and survival following lung transplantation for patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2008, 25 (2): 117-124.
Davis RD, Trulock EP, Manley J, Pasque MK, Sundaresan S, Cooper JD, Patterson GA: Differences in early results after single-lung transplantation. Washington University Lung Transplant Group. Ann Thorac Surg. 1994, 58 (5): 1327-1334. 10.1016/0003-4975(94)91907-0. discussion 1334-1325
Grossman RF, Frost A, Zamel N, Patterson GA, Cooper JD, Myron PR, Dear CL, Maurer J: Results of single-lung transplantation for bilateral pulmonary fibrosis. The Toronto Lung Transplant Group. N Engl J Med. 1990, 322 (11): 727-733. 10.1056/NEJM199003153221104.
Mason DP, Brizzio ME, Alster JM, McNeill AM, Murthy SC, Budev MM, Mehta AC, Minai OA, Pettersson GB, Blackstone EH: Lung transplantation for idiopathic pulmonary fibrosis. Ann Thorac Surg. 2007, 84 (4): 1121-1128. 10.1016/j.athoracsur.2007.04.096.
De Oliveira NC, Osaki S, Maloney J, Cornwell RD, Meyer KC: Lung transplant for interstitial lung disease: outcomes before and after implementation of the united network for organ sharing lung allocation scoring system. Eur J Cardiothorac Surg. 2012, 41 (3): 680-685. 10.1093/ejcts/ezr079.
De Oliveira NC, Osaki S, Maloney J, Cornwell RD, Meyer KC: Lung transplant for interstitial lung disease: outcomes for single versus bilateral lung transplantation. Interact Cardiovasc Thorac Surg. 2012, 14 (3): 263-267. 10.1093/icvts/ivr085.
Force SD, Kilgo P, Neujahr DC, Pelaez A, Pickens A, Fernandez FG, Miller DL, Lawrence C: Bilateral lung transplantation offers better long-term survival, compared with single-lung transplantation, for younger patients with idiopathic pulmonary fibrosis. Ann Thorac Surg. 2011, 91 (1): 244-249. 10.1016/j.athoracsur.2010.08.055.
Nwakanma LU, Simpkins CE, Williams JA, Chang DC, Borja MC, Conte JV, Shah AS: Impact of bilateral versus single lung transplantation on survival in recipients 60 years of age and older: analysis of United Network for Organ Sharing database. J Thorac Cardiovasc Surg. 2007, 133 (2): 541-547. 10.1016/j.jtcvs.2006.09.062.
Smits JM, Vanhaecke J, Haverich A, de Vries E, Smith M, Rutgrink E, Ramsoebhag A, Hop A, Persijn G, Laufer G: Three-year survival rates for all consecutive heart-only and lung-only transplants performed in Eurotransplant, 1997–1999. Clin Transpl. 2003, 89-100.
Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS: Factors indicative of long-term survival after lung transplantation: a review of 836 10-year survivors. J Heart Lung Transplant. 2010, 29 (3): 240-246. 10.1016/j.healun.2009.06.027.
Trulock EP, Edwards LB, Taylor DO, Boucek MM, Keck BM, Hertz MI: Registry of the International Society for Heart and Lung Transplantation: Twenty-third Official Adult Lung and Heart-Lung Transplantation Report-2006. J Heart Lung Transplant. 2006, 25 (8): 880-892. 10.1016/j.healun.2006.06.001.
Paik HC, Haam SJ, Lee DY, Yi GJ, Song SW, Kim YT, Kang CH, Kim KM, Park SI, Jheon SH: The fate of patients on the waiting list for lung transplantation in Korea. Transplant Proc. 2012, 44 (4): 865-869. 10.1016/j.transproceed.2011.12.059.
Jastrzebski D, Kozielski J, Nowak J, Zielinska-Les I, Ziora D, Szulik B, Wojarski J, Zakliczynski M, Zembala M: Prognostic risk factors in patients with interstitial lung disease referred for lung transplantation. J Physiol Pharmacol. 2005, 56 (Suppl 4): 107-113.
Callegari G, D'Armini AM, Vigano M, Fracchia C: Lung transplantation: the new point of view of an Italian centre. Monaldi Arch Chest Dis. 2000, 55 (4): 283-286.
Adamali HI, Judge EP, Healy D, Nolke L, Redmond KC, Bartosik W, McCarthy J, Egan JJ: International collaboration: a retrospective study examining the survival of Irish citizens following lung transplantation in both the UK and Ireland. BMJ Open. 2012, 2 (2): e000605-
Shorr AF, Davies DB, Nathan SD: Outcomes for patients with sarcoidosis awaiting lung transplantation. Chest. 2002, 122 (1): 233-238. 10.1378/chest.122.1.233.
Lederer DJ, Arcasoy SM, Wilt JS, D'Ovidio F, Sonett JR, Kawut SM: Six-minute-walk distance predicts waiting list survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006, 174 (6): 659-664. 10.1164/rccm.200604-520OC.
Timmer SJ, Karamzadeh AM, Yung GL, Kriett J, Jamieson SW, Smith CM: Predicting survival of lung transplantation candidates with idiopathic interstitial pneumonia: does PaO(2) predict survival?. Chest. 2002, 122 (3): 779-784. 10.1378/chest.122.3.779.
Mackay LS, Anderson RL, Parry G, Lordan J, Corris PA, Fisher AJ: Pulmonary fibrosis: rate of disease progression as a trigger for referral for lung transplantation. Thorax. 2007, 62 (12): 1069-1073. 10.1136/thx.2006.068494.
Nathan SD, Shlobin OA, Ahmad S, Koch J, Barnett SD, Ad N, Burton N, Leslie K: Serial development of pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Respiration. 2008, 76 (3): 288-294. 10.1159/000114246.
Kadikar A, Maurer J, Kesten S: The six-minute walk test: a guide to assessment for lung transplantation. J Heart Lung Transplant. 1997, 16 (3): 313-319.
Costa da Silva F, Afonso JE, Pego-Fernandes PM, Caramori ML, Jatene FB: Sao Paulo Lung Transplantation Waiting List: Patient Characteristics and Predictors of Death. Transplant Proc. 2009, 41 (3): 927-931. 10.1016/j.transproceed.2009.01.048.
Shitrit D, Gershman Y, Peled N, Medalion B, Saute M, Amital A, Kramer MR: Risk factors for death while awaiting lung transplantation in Israeli patients: 1997-2006. Eur J Cardiothorac Surg. 2008, 34 (2): 444-448. 10.1016/j.ejcts.2008.03.068.
Shitrit D, Rusanov V, Peled N, Amital A, Fuks L, Kramer MR: The 15-step oximetry test: a reliable tool to identify candidates for lung transplantation among patients with idiopathic pulmonary fibrosis. J Heart Lung Transplant. 2009, 28 (4): 328-333. 10.1016/j.healun.2008.12.019.
Rusanov V, Kramer MR, Raviv Y, Medalion B, Guber A, Shitrit D: The significance of elevated tumor markers among patients with idiopathic pulmonary fibrosis before and after lung transplantation. Chest. 2012, 141 (4): 1047-1054. 10.1378/chest.11-0284.
Erasmus DB, Keller CA, Alvarez FB: Large airway complications in 150 consecutive lung transplant recipients. Journal of Bronchology. 2008, 15 (3): 152-157. 10.1097/LBR.0b013e31817f8d2b.
Merlo CA, Weiss ES, Orens JB, Borja MC, Diener-West M, Conte JV, Shah AS: Impact of U.S. Lung Allocation Score on survival after lung transplantation. J Heart Lung Transplant. 2009, 28 (8): 769-775. 10.1016/j.healun.2009.04.024.
Horai T, Shigemura N, Gries C, Pilewski J, Bhama JK, Bermudez CA, Zaldonis D, Toyoda Y: Lung transplantation for patients with high lung allocation score: single-center experience. Ann Thorac Surg. 2012, 93 (5): 1592-1597. 10.1016/j.athoracsur.2011.09.045. discussion 1597
Raghu G, Weycker D, Edelsberg J, Bradford WZ, Oster G: Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006, 174 (7): 810-816. 10.1164/rccm.200602-163OC.
State Totals: Vintage 2011. Annual Population Estimates. [http://www.census.gov/popest/data/state/totals/2011]
Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, Egan T, Keshavjee S, Knoop C, Kotloff R, Martinez FJ, Nathan S, Palmer S, Patterson A, Singer L, Snell G, Studer S, Vachiery JL, Glanville AR, Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation: International guidelines for the selection of lung transplant candidates: 2006 update–a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006, 25 (7): 745-755. 10.1016/j.healun.2006.03.011.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2466/14/139/prepub
Acknowledgements
The authors are grateful to Dr. Susanne Stowasser from Boehringer Ingelheim for expert medical input and review.
This study was sponsored by Boehringer Ingelheim GmbH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
D.E. is an employee of Boehringer Ingelheim GmbH, funding for this study was provided to Evidera by Boehringer Ingelheim GmbH.
P.R. and K.K. are employees of Evidera, funding for this study was provided to Evidera by Boehringer Ingelheim GmbH.
L.N. was an employee of Evidera (formerly United Biosource) at the time of the study.
Authors’ contributions
LN, PR, DE, made substantial contributions to conception and design; PR and KK carried out the literature review; all authors contributed to the interpretation of data; LN, PR, and KK were involved in drafting the manuscript; DE and KK were involved in revising the manuscript critically for important intellectual content; all authors read and approved the final manuscript.
Electronic supplementary material
12890_2014_580_MOESM1_ESM.doc
Additional File 1: Search Strategy to Identify Papers Indexed in MEDLINE and EMBASE and Reporting Data on Post-Transplantation Survival Among Patients with IPF.(DOC 29 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kistler, K.D., Nalysnyk, L., Rotella, P. et al. Lung transplantation in idiopathic pulmonary fibrosis: a systematic review of the literature. BMC Pulm Med 14, 139 (2014). https://doi.org/10.1186/1471-2466-14-139
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2466-14-139