Abstract
Background
The volume, extent and speed of travel have dramatically increased in the past decades, providing the potential for an infectious disease to spread through the transportation network. By collecting information on the suspected place of infection, existing surveillance systems in industrialized countries may provide timely information for areas of the world without adequate surveillance currently in place. We present the results of a case study using reported cases of Shigella dysenteriae serotype 1 (Sd1) in European travellers to detect "events" of Sd1, related to either epidemic cases or endemic cases in developing countries.
Methods
We identified papers from a Medline search for reported events of Sd1 from 1940 to 2002. We requested data on shigella infections reported to the responsible surveillance entities in 17 European countries. Reports of Sd1 from the published literature were then compared with Sd1 notified cases among European travellers from 1990 to 2002.
Results
Prior to a large epidemic in 1999–2000, no cases of Sd1 had been identified in West Africa. However, if travellers had been used as an early warning, Sd1 could have been identified in this region as earlier as 1992.
Conclusion
This project demonstrates that tracking diseases in European travellers could be used to detect emerging disease in developing countries. This approach should be further tested with a view to the continuous improvement of national health surveillance systems and existing European networks, and may play a significant role in aiding the international public health community to improve infectious disease control.
Similar content being viewed by others
Background
Emerging or re-emerging infections can be defined as infections that have newly appeared in a population or have existed but are rapidly increasing in incidence or geographic range [1]. The potentially devastating effects of an emerging or re-emerging disease are related to its capacity to spread rapidly and therefore to infect many people.
New diseases have often first emerged in resource poor countries: HIV infection in central Africa [2, 3]; Lassa fever in west Africa [4]; Ebola virus infection in the Democratic Republic of Congo (ex Zaire)[5]; Marburg haemorrhagic fever in Zimbabwe [6]; cholera due to Vibrio cholerae O139 on the Indian subcontinent [7, 8]; and meningococcal meningitis caused by the serogroup W135 in Sahelian countries [9, 10].
While the epidemiological characteristics of these diseases are very different, a common element of HIV [11], meningoccccal infections due to the serogroup W135 [12] and Marburg haemorrhagic fever [13] is that they were first detected in western countries. Diagnostic capabilities for certain pathogens are simply not available in many resource-poor countries, nor are networks for sharing epidemiological information. In those countries, therefore, the emergence or re-emergence of some pathogens is not likely to be detected.
Early detection and adequate response are key elements in controlling emerging diseases, which depend upon rapid clinical diagnosis and containment in populations and in the environment [3]. In recent years, many efforts have been made to reinforce laboratory capacities and epidemiological surveillance in countries with limited medical and laboratory infrastructures. Despite these measures, many countries still lack basic laboratory facilities, sufficient financial resources to run expensive laboratory techniques, and adequate means of communication for surveillance purposes.
It is well known that because people travel more often and to more places than ever before, the potential for infectious disease transmission has increased. But, from an epidemiologic perspective, the increase in travel can also help to provide insight into infectious disease circulation in other areas of the world, and perhaps make it possible to detect new events [14]. By collecting information on the probable place of infection, existing surveillance systems in industrialized countries can play an important role in sharing information. However, at national surveillance level, there is no systematic coordinated system to take advantage of this epidemiological information. Current mechanisms to share health information depend on the "good will" of each country to provide such information to the international health community. We explore the possibility of using European national reporting data to inform on the presence and changes in patterns of a specific disease in a region. The goal of this research is to quantify, using a case example, the effectiveness of this "travellers' alert" to detect emerging or re-emerging diseases in countries with limited laboratory facilities.
Methods
Choice of Shigella dysenteriaeserotype 1
Shigellosis is endemic in numerous developing countries and the most important cause of dysentery worldwide. It has been estimated that shigellosis accounts for at least 80 million cases (99% in developing countries) and 700,000 deaths each year, and causes 5 to 10% of diarrhoeal illness and 75% of diarrhoeal deaths [15, 16]. Among shigellosis infections, we choose Shigella dysenteriae serotype 1 (Sd1) infections as a case study because Sd1 presents a unique opportunity to examine the viability of using travellers as an early alert for several key reasons. First, man is the only natural host for s higella species, and therefore no other vectors or reservoirs need to be considered. Second, shigella infections in industrialized countries are primarily due to S. sonnei and less frequently to S. flexneri and not to Sd1 [17]. Therefore, cases of Sd1 in industrialised countries will have been infected during travel and not in their country of residence. Third, unlike laboratories in industrialized countries, laboratories in developing countries often do not have the capacity to identify Sd1. The causative pathogen is more likely to be identified in western travellers when they come home, and have access to comprehensive laboratory facilities. Because of the short incubation period (average 1 to 3 days [18]) and severe clinical symptoms, travellers are likely both to seek medical attention (or follow up care) in their home country and to recall the probable place of infection during the course of their trip. In addition, chronic carriage of shigella is very uncommon. Finally, Sd1 while reported in many developing countries, seemed to emerge in West Africa in 1999. We wanted to test how an early alert based on travellers could have helped in detecting the emergence of Sd1 in that particular region of the world at that time.
Data sources
We present a comprehensive spatial and temporal review of notified Sd1 cases. Assuming that the most common channel of communication in the scientific community for sharing information about an emerging or re-emerging diseases is publication in scientific journals, we performed a comprehensive literature review. We identified papers from a Medline search for reported events of Sd1 from 1940 to 2002. Both English and French articles were included in the review (keywords: shigella, shigellosis, dysentery, shigella and dysentery, shigella dysenteriae). We also search PROMED using the same keywords. We included reports of laboratory confirmed Sd1 and probable Sd1 for both endemic and epidemic events.
Next, we submitted a protocol of the study and data form to the responsible surveillance entities in 17 European countries (Austria, Belgium, Denmark, France, Finland, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the United Kingdom). We used the European list of contacts from the International Surveillance Network for the Enteric Infections Salmonella and VTEC O157 (EnterNet). Though this existing network for human gastrointestinal infections did not specifically aim to collect data on Sd1, in most cases epidemiologists and microbiologists were also responsible in their country for surveying shigella infections. We requested data on the date of diagnosis, the probable place of infection (PPI) (at the country level), gender, age (less than 1 year, 1– 5 years, 6–14 years, 15–64 years, and 65 years and over), and antibiogrammes for Sd1 cases reported between 1990 and 2002.
Then we compared the temporal and geographic distribution of cases reported in the literature review to data provided by national surveillance entities. We compiled a yearly timeline of Sd1 from 1940 to 2002 by country for the literature review (we collected the date of the events, and date of publication) and from 1990 to 2002 for the travellers comparison.
Results
Sd1 infections reported in the literature
The first confirmed and published Sd1 outbreak occurred in Somalia in 1963–64 [19], followed by a long reporting gap in Africa until 1979 (Table 1). During this gap, large outbreaks occurred in Central America: Guatemala in 1968–69 [20, 21]; El Salvador [22], Honduras [22], Mexico in 1969 [23]; and Costa Rica in 1970 [22]. A 1972 manuscript mentioned a large outbreak in Bangladesh, although Sd1 is reported to be endemic in this region [24]. The following year (1973), a significant outbreak occurred in Coral Island in the Bay of Bengal, Bangladesh [25].
Next, we observed in the literature a new wave of reported cases in Central Africa starting in 1979 in northeast Democratic Republic of Congo (DRC, ex-Zaire) [24, 26] and Rwanda [27], followed by Burundi in 1980 [28], DRC [24, 29, 30] and Tanzania in 1981 [31], and Tanzania and Burundi in 1982 [31, 32]. Subsequent events in central-east Africa were not published until the early 1990s. However, epidemics were observed in India and Burma in 1984 [33–36], in Thailand in 1986 [37] and in Iran in 1988 [38].
From 1990 to 1995, outbreaks of Sd1 were reported in the literature in central and eastern Africa. A large wave started in Zambia in 1990–1991 [39–41] and then spread to central, eastern and southern Africa in the following years: in 1992, Zimbabwe [42], Swaziland [43], and Burundi [44]; in 1993, Zimbabwe [45], Mozambique [46], Rwanda [47], Sudan [48], Sao Tome [49], Uganda [49] and Burundi [44]; in 1994, South Africa [50–52], Mozambique [46], Kenya [53], Rwanda [54], Zimbabwe [55] and DRC [56–59]; in 1995, Kenya [60, 61], South Africa [62], Zimbabwe, Mozambique, and Malawi [55]. In 1997, the last epidemics in that region were reported in South Africa [63], Kenya [55], Zimbabwe [64] and Somalia [55].
According to the published literature, no outbreaks of Sd1 strains were reported in West Africa until 1999. Dialo et al first mentioned Sd1 in Senegal in 1999 [65], though for a limited number of cases. The first large outbreak reported in West Africa occurred in Sierra Leone at the end of 1999 [66, 67]. Endemic cases and outbreaks have been reported almost every year in India and Bangladesh from 1990 to 2002 [68–71].
Promed reported "dysentery outbreak" mostly in Russia and North America. The causal germ of the dysentery (shigella, ETEC or E. histolitica) was most of the time not identified, or was not shigella dysenteriae.
Sd1 surveillance of European travellers
Of the 17 countries where the protocol was submitted, we obtained responses from all but one country (Luxembourg). Seven countries reported either no case of Sd1 or reported cases but without PPI. A total of 263 cases were reported for the study period. The PPI was available for 178 (68%) of the cases. In five of these, the PPI was reported as Africa (unspecified country). The most frequent PPI was Senegal where 37 cases were reported over the study period (5 family-related outbreaks) and India (n = 21 cases) where cases were reported in all but 3 years of the study period. Cases were also frequently reported from Mali (n = 13), Egypt (n = 12), Djibouti (n = 10), Pakistan (n = 9), Kenya (n = 8), Cape Verde (n = 9), Bangladesh (n = 6) Ivory Coast (n = 5) and Democratic Republic of Congo (n = 5). Other countries of probable place of infection include: Angola (n = 2), Burkina Faso (n = 2), Lebanon (n = 2), Mauritania (n = 4), Nepal (n = 2), Nigeria (n = 3), Rwanda (n = 3), Tanzania (n = 3), the United Kingdom (n = 2), Uganda (n = 2), Uzbekistan (n = 3) and Zambia (n = 3). There were also multiple countries where the probable place of infection was reported only once during the study period: Afghanistan, Brazil, Eritrea, Ghana, Israel, Madagascar, Mozambique, Sudan, Sweden, Thailand, Tunisia, Turkey and Uganda.
Evaluation of the travellers early alert (Sd1 surveillance of European travellers) versus the literature notification
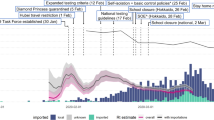
We explore timeliness between notification of an "Sd1 event" using the travellers alert and the literature. For Asia, the literature review points out the continuous endemicity of the diseases other the past 4 decades. For South America, no new Sd1 events were reported in the literature or through the travellers surveillance since the early 70s. Here, therefore, we only present data from African countries, in four regions: West Africa region (figure 1), North East Africa region (figure 2), Central and East Africa region (figure 3) and South Africa region, including Madagascar (figure 4). The median delay between the occurrence of an event and its publication in a journal was 2 years (range 6 months to 6 years).
The travellers alert detected Sd1 infections in several countries of West Africa: Mauritania (1992), Mali (1993), Tunisia (1994), Burkina Faso (1995), Ivory Coast (1999), Cape Verde (2000), Ghana (2001) and Nigeria (2001). We did not find Sd1 mentioned in the literature in any of these countries. Only one article mentioned Sd1 outbreaks in Senegal 7 years after the first case would have been detected through the early alert tested here.
In North East Africa, the travellers alert detected Sd1 in Eritrea, Sudan, Egypt, and Djibouti from 1991 to 2000, while this information had not yet appeared in the literature.
In Central, East and South African countries, the travellers alert reported Sd1 in DRC, Angola and Madagascar while no published data are available. In Kenya, we picked up an SD1 event 3 years before a large outbreak was mentioned in a publication.
The early alert would have identified the presence of Sd1 in West Africa 7 years (1992) before it was reported during an epidemic (1999). West African countries were not prepared for the magnitude of the Sd1 outbreaks in 1999 or for the identification of Sd1 in national laboratories.
Travellers' surveillance coincided with the literature review when cases were reported in Kenya (1994–1996) and in 1994 where cases were reported in Rwanda, DRC, and Mozambique.
Discussion
Using Sd1 as an example, our case study suggests that using existing surveillance systems of European travellers made it possible to detect an emerging disease in regions of the world apparently previously unaffected. Travellers can therefore serve as valuable sentinels in identifying new or changing infectious disease problems in areas of the world where resources may be insufficient to provide full laboratory identification and characterization of pathogens.
Using travellers as an early warning aims to create an alert, rather than function as a surveillance system used to follow trends. By using this information as an alert, even partial data proved to be effective in detecting an usual event, e.g. diagnosis of Sd1 in West Africa through a travellers alert, 7 years (1992) before an "official" report. The information collected by the early alert would be shared with the Ministry of Health (MoH) concerned. The WHO should be a natural channel of communication and could plan a response strategy with the MoH and other partners such as NGOs. The WHO is normally in a position to assess the public health relevance of the findings and therefore to emphasize to the MoH the need for certain measures. Training of national reference laboratories, equipment procurement (i.e. medium transport, laboratory equipment), training of clinicians to recognise the disease and adaptation of the surveillance system could have been implemented in order to improve the capacity to detect this particular disease in the region.
Several limitations to this analysis require discussion. Because of the short incubation period (1–3 days), many travellers with shigellosis are likely to become ill during travel. Empiric treatment of traveller's diarrhoea with antimicrobial agents is common; looking at returned travellers would be likely to miss many shigella infections in travellers. Because Sd1 is not necessarily a reportable disease or because the information concerning the probable place of infection was not communicated, many cases were not recorded at national surveillance levels. Thus, the total number of SD1 cases reported and used in this analysis is limited (e.g. 178 cases over a period of 13 years). In addition, travel patterns, i.e. numbers of travellers to a specific region in a definite time period, may affect the capacity of travellers surveillance to create an alert.
Events of Sd1 reported in the literature may contain temporal and spatial inaccuracies, although on a larger temporal and spatial scale they can be considered sufficiently robust. Reporting bias in the literature may be due to several reasons: the lack of diagnosis capacity of a country may induce decreased reporting. A highly active research team being collocated in a particular country, on the other hand, may stimulate publications that would not exist in another country. Other geopolitical factors might increase the likelihood of identification and reporting of such endemic disease (civil war, humanitarian emergencies, the presence of NGOs). The absence of Sd1 in a particular country through the travellers surveillance should not be assumed to be due to its true absence from the country. Differences in travel patterns may also affect the sensibility of the alert. The "model" proposed here should be considered as an additional tool to improve detection of emerging or re-emerging diseases. Nevertheless, the comparison between literature reporting and travellers surveillance is intended to test the efficacy of using European travellers for detecting emerging or re-emerging events of public health importance, i.e. large numbers of cases usually reported in the literature. A clear direction for future research is to examine other forms of surveillance data rather than the published literature.
Laboratory methods to confirm isolates as Sd1 reported here were not standardised in Europe, but were considered valid by each national reference laboratory.
One strength of using a travellers alert is that an isolated case report is sufficient to suggest circulation of Sd1 in the PPI and is independent of the magnitude of the events. A single event of a new pathogen (emerging or re-emerging) in a region would be sufficient to create the alert. Another strength of using travellers as an early alert is that denominator information (i.e. total number of travellers to a particular country or region), which is often difficult to collect, is not required. This factor is essential compared to surveillance systems, as in the "model" developed here; in principle, a single event is sufficient to create the alert.
In this study, only 4 countries had reported resistance patterns of Sd1 identified in travellers (data not shown). National surveillance systems were not systematically collecting these data, but from 2000, several countries started to record this information. In the future, recording resistance patterns of Sd1 in travellers could be a useful tool. However, information of resistance pattern evolution given by this early alert would remain occasional, and would not provide a representative sample of the infected population.
Through improved data collection (by standardising data collected and adding information on the probable place of infection) and international collaboration, the model used here could be applied to other diseases with short incubation periods and which are not prevalent in the travellers' country of origin. Because case counts of such events are expected to be low, coordination among national surveillance systems is crucial and probably feasible within the context of institutions covering large populations such as the new European Centre for Disease Prevention and Control (ECDC), the US Centres for Disease Control (CDC Atlanta) and of course the World Health Organisation. Travel medical clinic surveillance systems, such as TropNetEurop [72] or Geosentinel [73] are used to detect morbidity in travelers and to facilitate their accurate diagnoses and treatment. They have also attempted to use their data with the same objective and should be associated with this network.
Linking databases across countries increases the probability of picking up uncommon events. Communication channels should be developed to relay routinely captured information to countries and institutions that can use it.
Conclusion
Sentinel surveillance information may be most useful for infections that can be prevented (e.g., vaccine or other public health intervention) or treated with effective drugs (in this instance, information about resistance patterns may be valuable). Information about resistance patterns can have potential practical implications both for the residents in the country of origin (of the pathogen) and for travellers.
This approach should be further tested with a view to the continuous improvement of national health surveillance systems and existing European networks, and may play a significant role in aiding the international public health community to improve infectious disease control. The WHO or other international partners could provide the necessary information to the ministries of health concerned in order to improve laboratory capacity, and train laboratory personnel and clinicians to diagnose emerging or re-emerging diseases.
Abbreviations
- DRC:
-
Democratic Republic of Congo (ex-Zaire)
- PPI:
-
Probable place of infection
- Sd1:
-
shigella dysenteriae serotype 1
References
Morse SS: Factors in the emergence of infectious diseases. Emerg Infect Dis. 1995, 1: 7-15.
Sharp PM, Bailes E, Chaudhuri RR, Rodenburg CM, Santiago MO, Hahn BH: The origins of acquired immune deficiency syndrome viruses: where and when?. Philos Trans R Soc Lond B Biol Sci. 2001, 356: 867-876. 10.1098/rstb.2001.0863.
Morens DM, Folkers GK, Fauci AS: The challenge of emerging and re-emerging infectious diseases. Nature. 2004, 430: 242-249. 10.1038/nature02759.
Frame JD, Baldwin JM, Gocke DJ, Troup JM: Lassa fever, a new virus disease of man from West Africa. I. Clinical description and pathological findings. Am J Trop Med Hyg. 1970, 19: 670-676.
Johnson KM, Lange JV, Webb PA, Murphy FA: Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet. 1977, 1: 569-571. 10.1016/S0140-6736(77)92000-1.
Gear JS, Cassel GA, Gear AJ, Trappler B, Clausen L, Meyers AM, Kew MC, Bothwell TH, Sher R, Miller GB, et al: Outbreak of Marburg virus disease in Johannesburg. Br Med J. 1975, 4: 489-493.
Epidemic diarrhoea due to Vibrio cholerae non-O1. Wkly Epidemiol Rec. 1993, 68: 141-142.
Ramamurthy T, Garg S, Sharma R, Bhattacharya SK, Nair GB, Shimada T, Takeda T, Karasawa T, Kurazano H, Pal A, et al: Emergence of novel strain of Vibrio cholerae with epidemic potential in southern and eastern India. Lancet. 1993, 341: 703-704. 10.1016/0140-6736(93)90480-5.
Taha MK, Parent dC I, Schlumberger M, Sanou I, Djibo S, de Chabalier F, Alonso JM: Neisseria meningitidis serogroups W135 and A were equally prevalent among meningitis cases occurring at the end of the 2001 epidemics in Burkina Faso and Niger. J Clin Microbiol. 2002, 40: 1083-1084. 10.1128/JCM.40.3.1083-1084.2002.
Meningococcal disease, serogroup W135, Burkina Faso. Wkly Epidemiol Rec. 2002, 77: 152-155.
Gottlieb MS, Schroff R, Schanker HM, Weisman JD, Fan PT, Wolf RA, Saxon A: Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N Engl J Med. 1981, 305: 1425-1431.
Aguilera JF, Perrocheau A, Meffre C, Hahne S: Outbreak of serogroup W135 meningococcal disease after the Hajj pilgrimage, Europe, 2000. Emerg Infect Dis. 2002, 8: 761-767.
Martini GA, Knauff HG, Schmidt HA, Mayer G, Baltzer G: A hitherto unknown infectious disease contracted from monkeys. "Marburg-virus" disease. Ger Med Mon. 1968, 13: 457-470.
Wilson ME: The traveller and emerging infections: sentinel, courier, transmitter. J Appl Microbiol. 2003, 94 Suppl: 1S-11S. 10.1046/j.1365-2672.94.s1.1.x.
Shigellosis disease burden, epidemiology and case management. Wkly Epidemiol Rec. 2005, 80 (11): 94-99.
World Health Organization: Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1. 2005, [http://whqlibdoc.who.int/publications/2005/9241592330.pdf]
Keusch GT, Bennish ML: Shigellosis. Bacterial infections of humans. Epidemiology and control. 1998, New York and London: Plenum Medical Book Company, 631-656. 3
Heymann D: Control of Communicable Diseases Manual. Washington, 2004. Official report of the American Public Health Association, 18
Cahill KM, Davies JA, Johnson R: Report on an epidemic due to Shigella dysenteriae, type 1, in the Somali interior. Am J Trop Med Hyg. 1966, 15: 52-56.
Gangarosa EJ, Perera DR, Mata LJ, Mendizabal-Morris C, Guzman G, Reller LB: Epidemic Shiga bacillus dysentery in Central America. II. Epidemiologic studies in 1969. J Infect Dis. 1970, 122: 181-190.
Mata LJ, Gangarosa EJ, Caceres A, Perera DR, Mejicanos ML: Epidemic Shiga bacillus dysentery in Central America. I. Etiologic investigations in Guatemala, 1969. J Infect Dis. 1970, 122: 170-180.
Levine MM, DuPont HL, Formal SB, Gangarosa EJ: Epidemic Shiga dysentery in Central America. Lancet. 1970, 2: 607-608. 10.1016/S0140-6736(70)90184-4.
Weissman JB, Marton KI, Lewis JN, Friedmann CT, Gangarosa EJ: Impact in the United States of the Shiga dysentery pandemic of Central America and Mexico: a review of surveillance data through 1972. J Infect Dis. 1974, 129: 218-223.
Frost JA, Rowe B, Vandepitte J, Threlfall EJ: Plasmid characterisation in the investigation of an epidemic caused by multiply resistant Shigella dysenteriae type 1 in Central Africa. Lancet. 1981, 2: 1074-1076. 10.1016/S0140-6736(81)91277-0.
Rahaman MM, Khan MM, Aziz KM, Islam MS, Kibriya AK: An outbreak of dysentery caused by Shigella dysenteriae type 1 on a coral island in the Bay of Bengal. J Infect Dis. 1975, 132: 15-19.
Rogerie F, Ott D, Vandepitte J, Verbist L, Lemmens P, Habiyaremye I: Comparison of norfloxacin and nalidixic acid for treatment of dysentery caused by Shigella dysenteriae type 1 in adults. Antimicrob Agents Chemother. 1986, 29: 883-886.
Bogaerts J, Bosmans E, Vandenbulcke L, Lemmens P, Lepage P, Vandepitte J, Ghysels G: Shigella and Salmonella species from Kigali (Rwanda) (1976–1982). Ann Soc Belg Med Trop. 1985, 65: 281-292.
Shigellosis surveillance – Burundi. Wkly Epidemiol Rec. 1984, 59: 295-
Malengreau M, Molima K, Gillieaux M, de Feyter M, Kyele D, Mukolo N: Outbreak of Shigella dysentery in Eastern Zaire, 1980–1982. Ann Soc Belg Med Trop. 1983, 63: 59-67.
Ebright JR, Moore EC, Sanborn WR, Schaberg D, Kyle J, Ishida K: Epidemic Shiga bacillus dysentery in Central Africa. Am J Trop Med Hyg. 1984, 33: 1192-1197.
Mhalu FS, Moshi WK, Mbaga I: A bacillary dysentery epidemic in Dar es Salaam, Tanzania. J Diarrhoeal Dis Res. 1984, 2: 217-222.
Ries AA, Wells JG, Olivola D, Ntakibirora M, Nyandwi S, Ntibakivayo M, Ivey CB, Greene KD, Tenover FC, Wahlquist SP, et al: Epidemic Shigella dysenteriae type 1 in Burundi: panresistance and implications for prevention. J Infect Dis. 1994, 169: 1035-1041.
Pal SC: Epidemic bacillary dysentery in West Bengal, India, 1984. Lancet. 1984, 1: 1462-10.1016/S0140-6736(84)91948-2.
Albert MJ: Multiresistant Shigella dysenteriae type 1. Lancet. 1985, 2: 948-949. 10.1016/S0140-6736(85)90879-7.
Sen D, Dutta P, Deb BC, Pal SC: Nalidixic-acid resistant Shigella dysenteriae type 1 in eastern India. Lancet. 1988, 2: 911-10.1016/S0140-6736(88)92515-9.
Tin A, Aung MH, Khin MU: Epidemic shiga bacillary dysentery in Rangoon, Burma, 1984/85. Lancet. 1985, 1: 1442-10.1016/S0140-6736(85)91861-6.
Taylor DN, Bodhidatta L, Brown JE, Echeverria P, Kunanusont C, Naigowit P, Hanchalay S, Chatkaeomorakot A, Lindberg AA: Introduction and spread of multi-resistant Shigella dysenteriae I in Thailand. Am J Trop Med Hyg. 1989, 40: 77-85.
Katouli M, Shokouhi F, Motevallian M, Javanshir ET, Bairamian M, Jirsarayi R: Dysentery due to multiresistant Shiga bacillus in rural Iran. Lancet. 1988, 2: 911-10.1016/S0140-6736(88)92516-0.
Tuttle J, Ries AA, Chimba RM, Perera CU, Bean NH, Griffin PM: Antimicrobial-resistant epidemic Shigella dysenteriae type 1 in Zambia: modes of transmission. J Infect Dis. 1995, 171: 371-375.
van der Hoek W, van Oosterhout JJ, Ngoma M: An outbreak of dysentery in Zambia. S Afr Med J. 1996, 86: 93-94.
Karas JA, Pillay DG: Nalidixic acid-resistant Shigella dysenteriae type I in KwaZulu-Natal. S Afr Med J. 1996, 86: 93-
Nathoo KJ, Porteous JE, Siziya S, Wellington M, Mason E: Predictors of mortality in children hospitalized with dysentery in Harare, Zimbabwe. Cent Afr J Med. 1998, 44: 272-276.
Isaacson M, Canter PH, Effler P, Arntzen L, Bomans P, Heenan R: Haemorrhagic colitis epidemic in Africa. Lancet. 1993, 341: 961-10.1016/0140-6736(93)91253-I.
Engels D, Madaras T, Nyandwi S, Murray J: Epidemic dysentery caused by Shigella dysenteriae type 1: a sentinel site surveillance of antimicrobial resistance patterns in Burundi. Bull World Health Organ. 1995, 73: 787-791.
Mason PR, Nathoo KJ, Wellington M, Mason E: Antimicrobial susceptibilities of Shigella dysenteriae type 1 isolated in Zimbabwe–implications for the management of dysentery. Cent Afr J Med. 1995, 41: 132-137.
Aragon M, Barreto A, Chambule J, Noya A, Tallarico M: Shigellosis in Mozambique: the 1993 outbreak rehabilitation–a follow- up study. Trop Doct. 1995, 25: 159-162.
Paquet C, Leborgne P, Sasse A, Varaine F: [An outbreak of Shigella dysenteriae type 1 dysentery in a refugee camp in Rwanda]. Sante. 1995, 5: 181-184.
Musa HA, Hassan HS, Shears P: Occurrence in Sudan of Shigella dysenteriae type 1 with transferable antimicrobial resistance. Annals of Tropical Medicine & Parasitology. 1997, 91: 669-671. 10.1080/00034989760789.
World Health Organisation: Intercountry meeting on epidemic dysentery. 1995
Bloom PD, MacPhail AP, Klugman K, Louw M, Raubenheimer C, Fischer C: Haemolytic-uraemic syndrome in adults with resistant Shigella dysenteriae type I. Lancet. 1994, 344: 206-10.1016/S0140-6736(94)92815-0.
Rollins NC, Wittenberg DF, Coovadia HM, Pillay DG, Karas AJ, Sturm AW: Epidemic Shigella dysenteriae type 1 in Natal. J Trop Pediatr. 1995, 41: 281-284.
Klugman KP, MacPhail AP: Epidemic Shigella dysentery in South Africa. S Afr Med J. 1997, 87: 1145-1146.
Iijima Y, Oundo JO, Taga K, Saidi SM, Honda T: Simultaneous outbreak due to Vibrio cholerae and Shigella dysenteriae in Kenya. Lancet. 1995, 345: 69-70. 10.1016/S0140-6736(95)91197-9.
Milleliri JM, Soares JL, Signoret J, Bechen R, Lamarque D, Boutin JP, Coue JC, Niel L, Merouze F, Rey JL: [Epidemic of bacillary dysentery in the Rwanda refugee camps of the Goma region (Zaire, North Kivu) in August 1994]. Ann Soc Belg Med Trop. 1995, 75: 201-210.
Wittenberg DF: The spread of Shigella dysenteriae type I in Africa. Jpn J Med Sci Biol. 1998, 51 (Suppl): S36-S42.
Public health impact of Rwandan refugee crisis: what happened in Goma, Zaire, in July, 1994? Goma Epidemiology Group. Lancet. 1995, 345: 339-344. 10.1016/S0140-6736(95)90338-0.
Heyman SN, Ginosar Y, Niel L, Amir J, Marx N, Shapiro M, Maayan S: Meningococcal meningitis among Rwandan refugees: diagnosis, management, and outcome in a field hospital. Int J Infect Dis. 1998, 2: 137-142. 10.1016/S1201-9712(98)90115-1.
Legros D, Paquet C, Dorlencourt F, Saoult E: Risk factors for death in hospitalized dysentery patients in Rwanda. Trop Med Int Health. 1999, 4: 428-432. 10.1046/j.1365-3156.1999.00413.x.
Laureillard D, Paquet C, Malvy D: [Ciprofloxacin in the treatment of dysentery caused by type 1 Shigella dysenteriae during an epidemic in Rwandan refugees in Goma in 1994]. Sante. 1998, 8: 303-305.
Malakooti MA, Alaii J, Shanks GD, Phillips-Howard PA: Epidemic dysentery in western Kenya. Trans R Soc Trop Med Hyg. 1997, 91: 541-543. 10.1016/S0035-9203(97)90018-3.
Iversen ER, Colding H, Petersen L, Ngetich R, Shanks GD: Epidemic Shigella dysenteriae in Mumias, western Kenya. Trans R Soc Trop Med Hyg. 1998, 92: 30-31. 10.1016/S0035-9203(98)90942-7.
Chopra M, Wilkinson D, Stirling S: Epidemic shigella dysentery in children in northern KwaZulu-Natal. S Afr Med J. 1997, 87: 48-51.
Pillay DG, Karas AJ, Sturm AW: An outbreak of Shiga bacillus dysentery in KwaZulu/Natal, South Africa. J Infect. 1997, 34: 107-111. 10.1016/S0163-4453(97)92376-8.
Midzi SM, Tshimanga M, Siziya S, Marufu T, Mabiza ET: An outbreak of dysentery in a rural district of Zimbabwe: the role of personal hygiene at public gatherings. Cent Afr J Med. 2000, 46: 150-153.
Diallo A, Diop MB, Gueye MM, Etard JF: [Investigation of a shigellosis outbreak in a rural zone of Senegal]. Sante. 2001, 11: 217-219.
Guerin PJ, Brasher C, Baron E, Mic D, Grimont F, Ryan M, Aavitsland P, Legros D: Shigella dysenteriae serotype 1 in west Africa: intervention strategy for an outbreak in Sierra Leone. Lancet. 2003, 362: 705-706. 10.1016/S0140-6736(03)14227-4.
Guerin PJ, Brasher C, Baron E, Mic D, Grimont F, Ryan M, Aavitsland P, Legros D: Case management of a multidrug-resistant Shigella dysenteriae serotype 1 outbreak in a crisis context in Sierra Leone, 1999–2000. Trans R Soc Trop Med Hyg. 2004, 98: 635-643.
Sonawala M, Saraswathi K, Deodhar LP: Serogroup prevalence of Shigellae in Bombay. J Postgrad Med. 1995, 41: 104-106.
Dutta S, Rajendran K, Roy S, Chatterjee A, Dutta P, Nair GB, Bhattacharya SK, Yoshida SI: Shifting serotypes, plasmid profile analysis and antimicrobial resistance pattern of shigellae strains isolated from Kolkata, India during 1995–2000. Epidemiol Infect. 2002, 129: 235-243. 10.1017/S0950268802007240.
Talukder KA, Islam MA, Khajanchi BK, Dutta DK, Islam Z, Safa A, Alam K, Hossain A, Nair GB, Sack DA: Temporal shifts in the dominance of serotypes of Shigella dysenteriae from 1999 to 2002 in Dhaka, Bangladesh. J Clin Microbiol. 2003, 41: 5053-5058. 10.1128/JCM.41.11.5053-5058.2003.
Sarkar K, Ghosh S, Niyogi SK, Bhattacharya SK: Shigella dysenteriae type 1 with reduced susceptibility to fluoroquinolones. Lancet. 2003, 361: 785-10.1016/S0140-6736(03)12644-X.
TropNetEurop. [http://www.tropnet.net]
Geosentinel. [http://www.istm.org/geosentinel/main.html]
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/7/8/prepub
Acknowledgements
We thank our colleagues Leisa Weld (CDC, Atlanta, USA) and the GeoSentinel surveillance program for providing their insight. Special thanks to Dr Preben Aavitsland, Norwegian Institute of Public Health and to the European Programme for Field Epidemiolgy Training (EPIET), which created (among other things), a network of public health professionals allowing such a European project. We acknowledge the partial support of the 6th framework programme of the EU (grant SARSTRANS, project number: 511066).
List of Shigella Study Group participants:
Ingeborg Lederer, Franz Allerberger (National Reference Laboratory for Shigella, Austria); Jean-Marc Collard, Sophie Bertrand (National Reference Center for Shigella, Scientific Institute of Public Health, Brussels, Belgium); Steen Ethelberg (Dept. of Bacteriology, Mycology and Parasitology, Statens Serum Institut, Copenhagen, Denmark); Anja Siitonen, (National Public Health Institute (KTL), Helsinki, Finland); Francine Grimont (Centre National de Référence des Escherichia coli et Shigella, Institut Pasteur, Paris, France); Wolfgang Rabsch, Katharina Alpers (National Reference Centre for Salmonellae and other Enteric Bacteria & Department for Infectious Disease Epidemiology, Robert Koch Institute, Germany); Alkiviadis Vatopoulos, Athina Kansouzidou (Department of Microbiology, National School of Public Health, Greece); Paul McKeown, Patricia Garvey (Health Protection Surveillance Centre (HPSC), Dublin, Ireland), Biagio Pedalino, Marta Ciofi degli Atti (Istituto Superiore di Sanità, Rome, Italy); Yvonne van Duynhoven, Wilfrid van Pelt (Centre for Infectious Disease Epidemiology, National Institute of Public Health and the Environment, Bilthoven, The Netherlands); Karin Nygard, Jorgen Lassen (Division of Infectious Disease Control, Norwegian Institute of Public Health); Jorge Machado, Theresa Fernandes (Unidade de Enterobactérias, Centro de Bacteriologia, Instituto Nacional de Saúde, Lisboa, Portugal); Susan Brownlie, John Cowden (Gastrointestinal Infection and Zoonoses, Health Protection Scotland); Karen H Keddy (Enteric Diseases Unit, National Institute for Communicable Diseases, NHLS, Republic of South Africa); Gloria Hernández Pezzi, Ulrike Durr (Instituto de Salud Carlos III, Madrid, Spain); Herbert Haechler (National Centre for Enteropathogenic Bacteria, Switzerland); Birgitta de Jong, Yvonne Andersson (Dept. of Epidemiology, Swedish Institute for Infectious Disease Control, Sweden); Tom Cheasty (Public Health Laboratory Agency, London, United Kingdom); Audrey Lynch, Ruth Fox, (Communicable Disease Surveillance Centre, Northern Ireland, United Kingdom).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The author(s) declare they have no competing interests.
Authors' contributions
PJG participated in the conception and design of the study; analysis and interpretation of data; drafting the paper and revising it critically for substantial intellectual content. RFG, JAR and AJV participated in drafting the paper and revising it for substantial intellectual content.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Guerin, P.J., Grais, R.F., Rottingen, J.A. et al. Using European travellers as an early alert to detect emerging pathogens in countries with limited laboratory resources. BMC Public Health 7, 8 (2007). https://doi.org/10.1186/1471-2458-7-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-7-8