Abstract
Background
Both violence and depression during pregnancy have been linked to adverse neonatal outcomes, particularly low birth weight. The aim of this study was to investigate the independent and interactive effects of these maternal exposures upon neonatal outcomes among pregnant adolescents in a disadvantaged population from Sao Paulo, Brazil.
Methods
930 consecutive pregnant teenagers, admitted for delivery were recruited. Violence was assessed using the Californian Perinatal Assessment. Mental illness was measured using the Composite International Diagnostic Interview (CIDI). Apgar scores of newborns were estimated and their weight measured.
Results
21.9% of mothers reported lifetime violence (2% during pregnancy) and 24.3% had a common mental disorder in the past 12 months. The exposures were correlated and each was associated with low education. Lifetime violence was strongly associated with Common Mental Disorders. Violence during pregnancy (PR = 2.59(1.05–6.40) and threat of physical violence (PR = 1.86(1.03–3.35) and any common mental disorders (PR = 2.09 (1.21–3.63) (as well as depression, anxiety and PTSD separately) were independently associated with low birth weight.
Conclusion
Efforts to improve neonatal outcomes in low income countries may be neglecting two important independent, but correlated risk factors: maternal experience of violence and common mental disorder.
Similar content being viewed by others
Background
Both the experience of violence and antenatal depression may be risk factors for adverse neonatal outcomes, particularly low birth weight. A review of studies conducted in the USA and Europe[1] showed a weak, but significant, association between abuse during pregnancy (physical, sexual or emotional) and low birth weight (pooled OR = 1.4, 95%CI = 1.1–1.8) Developing country studies are rarer, but with results in the same direction [2–4]. For antenatal mental disorder, the pattern of findings suggests that socio-economic status may be an effect modifier, with associations with low birth weight only being apparent in more deprived communities [5–9]. Although previous studies have looked at the effect of these exposures separately, they are, in fact, closely related. In a meta analysis the weighted odds ratios for the association of different mental disorders with violence among women varied from 3.5 to 5.6 [10]. The aim of this study is to describe, among disadvantaged adolescent Brazilian mothers, the association between these two exposures and their independent and interactive effects on newborn outcomes: low birth weight, small for gestational age, preterm birth, still-birth, and Apgar scores.
Methods
Sample and setting
The study was carried out in the Hospital Maternidade Mario de Moraes Altenfelder, the only public hospital providing obstetric care to people living in a poor neighbourhood in the north of São Paulo. Consecutive adolescents (11 to 19 years old) admitted to the hospital for obstetric care between 24/7/2001 and 27/11/2002 were invited to participate.
Measurements
Data were collected through interviews in hospital after the women had recovered from labor and the effects of anaesthesia. This period varied between 4 to 48 hours after delivery.
Experience of violence
Violence was assessed using the relevant section from the Californian Perinatal Assessment[11, 12]. The questions, which were translated to Portuguese and back-translated to English to ensure semantic and content validity, are:
1. Sometimes women (girls) are physically attacked by another person. Have you ever been attacked with a gun, knife or other weapon, either by a family member or a lover or friend, or by a stranger? (Subsequent questions also included a reminder to consider each of these potential perpetrators)
2. Have you ever been attacked by anyone without a weapon but with the intent to seriously injure you?
3. Have you ever been threatened with the intent to seriously harm or injure you?
4. Has anyone ever made you have any kind of sex by using physical force or by threatening to harm you?
5. Did any of these incidents occur during your pregnancy?
6. Did you ever ask for police help or for a restraining order due to domestic violence?
The first two questions were combined to generate the variable 'any physical violence' and questions one to four were combined to generate the variable "any lifetime violence". Item 4 was used to define "any sexual violence". Item 5 was used to define the exposure of any type of violence experienced during pregnancy.
Mental health
Mental disorders were assessed using the Composite International Diagnostic Interview (CIDI 2.1 version). The interview has been validated for use in Brazil[13, 14] and all interviewers attended the accredited CIDI training centre. The primary outcome was Common Mental Disorders (CMD) in the previous 12 months; defined as all those who had a diagnosis of depression, anxiety, post-traumatic stress disorder (PTSD), somatoform or dissociative disorders at any time in the past 12 months according to the Diagnostic and Statistical Manual of Mental Disorders – 4th version (DSM-IV).
Newborn outcomes
Five outcomes were considered: still-birth; pre term birth, Small for gestagional age (SGA), low birth weight and low Apgar scores. Babies were weighed immediately after delivery by a pediatrician using a digital scale with a precision level of 10 grams. Low birth weight was defined as < 2500 grams. A low Apgar score was defined as below 7 at 5 minutes [15]. Gestational age was calculated using the date of last menstrual period reported by participants using the New Ballard method[16]. A cutoff point of less than 37 weeks of completed gestation was used to define prematurtity[17]. Small-for-gestational-age birth was defined as birth weight below the 10th percentile for expected weight according to gestational age[17], using, in the absence of any Brazilian reference data, a Canadian [18] population based gender-specific reference for birth weight.
Potential confounders, mediators and covariates
We also asked about the participants' age, education, socio-economic status and living arrangements. A Brazilian classification of social-economic class [19] was used, which takes into account the head of the household's education and the number of domestic electric tools in the household. It classifies individuals into five different categories (A to E) recoded to three categories: high (A and B), middle (C) and low (D and E). Obstetric history included number of pregnancies, alcohol and tobacco intake during pregnancy, pre-existing diseases (hypertension, diabetes and any 'lung, heart or kidney' diseases), and pregnancy complications (pregnancy induced hypertension, early labour, placenta praevia, placental abruption).
Ethics
Written informed consent was sought after explanations about the aims, potential risks and benefits of the research. Interviewers offered referral to the social and mental health team of the hospital or other agencies, as appropriate. The study was approved by the ethical committee of the hospital (Hospital Maternidade Mario de Moraes Altenfelder) and the ethical committee of Federal University of Sao Paulo.
Statistical analysis
Prevalence ratios (PR) and 95% confidence intervals were calculated for associations of violence exposures with maternal and newborn health outcomes. Poisson regression with robust variance[20] was used to estimate Prevalence Ratios and to adjust for the effect of other variables; associations of maternal mental health with violence were adjusted for age and education, while associations of maternal mental health and violence with low birth weight were initially adjusted for potential confounders (age, education, baby gender, parity, pre-existing conditions and maternal mental disorders/maternal exposure to lifetime violence), and incrementally for potential mediator factors (complications during pregnancy, alcohol intake and smoking during pregnancy and number of ante-natal consultations). An interaction between violence during pregnancy and CMD in the last 12 months was tested in the final model using a likelihood-ratio test.
Results
One thousand and two pregnant adolescents were admitted to the hospital during the study period, representing 24.4% of the 4108 women admitted for obstetric care. One thousand adolescents agreed to participate, of whom 70, admitted for miscarriage were excluded entirely from this study (n = 930). There were eight twin pregnancies, and ten still births; Apgar scores, pre term births and small-for-gestational-age births were studied only in singleton live births leaving 912 mother/child dyads for these analyses. Low birth weight was restricted to singleton live births with 37 weeks of gestational age or above leaving 795 mother/child dyads for these analyses.
A third of the mothers were 16 or younger (Table 1). Two-thirds had completed fewer than eight years of schooling and almost half had a family income less than 400 Reais (US$120). Most cohabited with a partner. The majority had not planned their pregnancy, and were having their first baby (Table 2). One in five mothers had complications during pregnancy. Drinking and smoking were relatively uncommon. Only 4.5% (n = 42) of the participants did not present antenatally, but 30% had had fewer than the recommended six antenatal consultations. One hundred and thirty one adolescents (14.2%) had pre-term babies. 40.1 percent (n = 370) had a normal vaginal delivery while 32.2% (n = 297) had a forceps delivery and 27.7% (n = 256) had a caesarean section.
Experience of violence
203 participants (21.8%) had experienced one or more types of violence at some time in their lives. The most common category was actual physical violence, experienced by 14% (n = 130) (evenly distributed between with and without a weapon), with threats of physical violence reported by 10% (n = 95) and 5% (n = 48) reporting sexual violence. Most of the violence went unreported; only 4% of those who suffered violence with a weapon and 17% of those reporting sexual violence had sought police help. Only 2% of mothers (n = 19) experienced violence during pregnancy; 26% of these had asked for police help.
Mental health during pregnancy
Two hundred and twenty six participants (24.3%) were diagnosed with a Common Mental Disorder in the previous 12 months. The most common diagnosis was depression (13.0%) followed by PTSD (9.8%), anxiety disorders (5.7%), somatoform disorder (1.8%) and dissociative disorder (0.3%). There was much comorbidity between depression, anxiety and PTSD: 32.0% of those with PTSD and 39.6% of those with anxiety also had depression.
Associations of violence and CMD with potential confounders and mediators
Low education and higher alcohol intake in pregnancy were associated with lifetime violence and CMD (tables 1 and 2). Higher parity was associated with lifetime violence (table 2), and pre-existing physical conditions and smoking with CMD. There was a non-significant trend for an association between CMD and premature birth.
The association between violence and common mental disorder
After adjusting for age and years of education, violence was strongly associated with CMD: lifetime physical violence, PR 2.17 (95%CI 1.72–2.73); lifetime threats of physical violence, PR 2.39 (95%CI 1.89–3.02); lifetime sexual violence, PR 2.60 (95%CI 2.00–3.41); and any violence during pregnancy, PR 2.29 (95%CI 1.50–3.50). We examined the association between violence and specific types of CMD. The risk for depressive disorder was higher for mothers who had experienced lifetime physical violence (PR = 1.94, 95%CI 1.33–2.81), but associations with threats of physical violence (PR = 1.43, 95%CI 0.90–2.29), sexual violence (PR = 1.45, 95%CI 0.78–2.71) and violence during pregnancy (PR = 1.99, 95%CI 0.90–4.40) were not statistically significant. Post-traumatic stress disorder (PTSD) was more strongly associated with all of the categories of violence; actual physical violence (PR = 3.71, 95%CI 2.53–5.45), threats of violence (PR = 5.09, 95%CI 3.53–7.37), sexual violence (PR = 4.82, 95%CI 3.20–7.26) and violence during pregnancy (PR = 4.31, 95% CI 2.36–7.85). Anxiety disorders were strongly associated with actual physical violence (PR = 3.01, 95%CI 1.75–5.19); threats (PR = 3.22, 95%CI 1.80–5.77) and sexual violence (PR = 2.86, 95%CI 1.37–6.04).
Association of maternal experiences of violence and common mental disorders with newborn outcomes
Ten babies (1.1%) were still born. Only one of these mothers had experienced lifetime violence (not during the pregnancy). There was no association between CMD and still birth, crude PR = 1.33 (95%CI 0.35–5.12). Apgar scores at five minutes were low (below 7) in 146 babies (16%). Neither lifetime violence (crude PR 1.01, 95% CI 0.70–1.44, adjusted PR (*Adjusted for age, education, baby gender, parity, pre-existing conditions, gestational age, complications during pregnancy, alcohol intake and smoking during pregnancy, ante-natal consultations and CMD/lifetime violence) = 1.11, 95%CI 0.77–1.60), nor violence during pregnancy (crude PR = 1.49, 95%CI 0.62–3.56, adjusted PR* = 1.59, 95%CI 0.73–3.44), nor CMD (Crude PR = 1.06, 95%CI 0.75–1.48; adjusted PR* = 1.00, 95%CI 0.70–1.43) was associated with low Apgar scores. 14.2% (131) were born with less than 37 weeks of gestational age. After adjustment for all potential confounders and mediators (*), pre term birth was found to be associated with common mental disorders (PR = 1.45 95% CI 1.00–2.09) but not with experience of violence. 239 babies (22.6%) were small for gestational age (SGA). After controlling for all potential confounders and mediators (*) only violence during pregnancy was associated with SGA (PR = 1.81, 95% CI 1.04–3.13).
One hundred and forty one babies (15.5%) had low birth-weight (LBW). Among those over 37 weeks of gestational age (n = 795) there were 62 babies with LBW (7.8%). There was a statistically significant trend for the risk of LBW to decrease with the number of ante-natal consultations (p-value, test for trend = 0.03). LBW was also strongly associated with pregnancy complications (crude PR = 1.85, 95% CI 1.10–3.10).
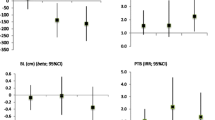
Table 3 summarizes the associations of violence and CMD with low birth-weight. There was a statistically significant crude association of all types of violence with low birth weight. However, after adjustment for potential confounders, only threat of physical violence and violence during pregnancy remained associated. After adjusting also for potential mediators (gestational age, complications during pregnancy, alcohol intake and smoking during pregnancy and ante-natal consultations) both any violence during pregnancy (PR = 2.59, 95%CI 1.05–6.40) and threat of physical violence (PR = 1.86, 95% CI 1.03–3.35) were associated with low birth weight. The association between CMD and LBW (crude PR = 2.19, 95% CI = 1.36 – 3.55) remaining significant after adjustment for potential confounders (PR = 1.93, 95% CI 1.07–3.47) and potential mediators (PR = 2.09, 95%CI 1.21–3.63). When looking at specific disorders depression PR = 2.52 (95%CI 1.43–4.44), anxiety disorders PR = 2.59 (95%CI 1.30–4.81) and PTSD PR = 1.91(95%CI 1.01–3.63) were each associated with low birth weight, after adjusting for confounders and mediators.
The effects of violence during pregnancy and CMD in the last 12 months on birth weight were additive rather than multiplicative; with no statistical interaction in the final model (p = 0.31) (interaction term PR = 0.35 (95%CI 0.11–2.00). One hundred and seventy seven adolescents had a CMD and did not suffer violence during pregnancy (adjusted PR* for association with LBW = 2.35, 95%CI 1.36–4.05), seven had only been exposed to violence during pregnancy (PR* = 1.67, 95% CI 1.40–21.16) and 10 had suffered both exposures (PR* = 4.50, 95% CI 1.56–12.92).
Discussion
Brazilian adolescents (10–19 years old) comprise 21% of the population[21]. Adolescent pregnancies are associated with poorer perinatal outcomes including low birth weight[22]. We found that violence and common mental disorders were common and correlated exposures among adolescent mothers attending a public obstetric hospital. Violence before pregnancy was not associated with low birth weight, unless there was a sexual element. Violence during pregnancy was less common, but was robustly associated with low birth-weight. Despite the strong associations between experience of violence and common mental disorders, the effects of each upon low birth weight were largely independent. Violence in pregnancy was associated with small-for-gestational-age but not with pre-term birth, whereas CMD was associated with pre-term birth but not SGA. Neither common mental disorder, nor experience of violence seemed to be associated with other adverse neonatal and pregnancy outcomes including pregnancy complications, still birth and Apgar scores.
The main limitation of our study is the timing of the interviews with mothers. The measurement of mental health shortly after childbirth may be confounded by emotional experiences common after childbirth. Also, recall bias is a possibility when exposures are ascertained after the outcomes have occurred. Arguably, this is more likely for still birth than for the less striking outcomes of low Apgar scores and low birth weight. However, we used a structured mental health diagnostic interview, delivered by trained interviewers who ensured that interviews were only carried out after the mother had fully recovered from childbirth. This method has been used in other studies[3, 23]. Antenatal interviews would have been logistically difficult because of the patchy nature of antenatal care. Furthermore, episodes of violence and mental disorder following the interview and prior to childbirth may be missed. Maternal CMD may also have biased recall of violent events in the past. This may have led to an overestimation of the association between these two exposures. However, this should not affect our main findings and makes the finding of an independent association of both exposures with LBW even more striking. Although we adjusted for most recognized correlates of poor maternal mental health, violence and low birth-weight, the possibility of residual confounding cannot be excluded. Maternal Body Mass Index (BMI), which is associated with neonatal adverse outcomes [24] might have been a mediator in our study, linking both exposures to low birth weight. Maternal BMI was not assessed, so unfortunately we could not explore this possibility. We have used a population based Canadian reference for calculating SGA [18]. Although this is not optimal, a Brazilian reference does not exist. Gestational age was calculated using the date of last menstrual period reported by participants. Again this method is not ideal, but it is widely used in developing countries as the most reliable measure of gestational age, when, as was the case in our study, ultrasound estimates are not available. On the other hand, our study had a high proportion responding, a large sample (compared to most other studies in this field), and used standardized and validated measures of the exposures and outcomes.
The 22% prevalence of lifetime physical violence in our study is consistent with other estimates; 25% in India[25], 18% in China[26], and 13.1% [3] and 33.5%[2] in two Latin American studies of pregnant women. However, the prevalence of physical or sexual violence during pregnancy in our study (2%) is amongst the lowest reported, with other studies reporting prevalences ranging from 3.5% to 20% [3, 26–28]. One explanation may be that a significant proportion of our young mothers were still in the parental home, rather than on their own with a potentially violent partner. The 24% prevalence of CMD among pregnant adolescents is similar to that typically found among pregnant adults in developed countries[29] and in the one previous study from Brazil [30]. Violence and CMD were highly correlated with each other in this population. Studies from developed countries clearly demonstrated that violence during pregnancy was associated with an increased risk for maternal mental disorders[31]. Women who experienced violence were more likely also to experience a range of other gendered disadvantages and this may act to create on oppressive atmosphere which results in poor mental health [32].
Very few studies have examined the impact of violence on newborn outcomes in developing countries. Nasir et al's review[33] reported three studies, and we were able to identify three more [2–4] (Jejeebhoy, 1998; Menezes, 2005; Valdez-Santiago & Sanin-Aguirre, 1996). None focused on adolescent mothers or measured maternal mental health. A study from Mexico[2] (Valdez-Santiago & Sanin-Aguirre, 1996) of 110 mothers showed a significant association of violence during pregnancy with low birth weight after adjusting for age and parity (4.0, 95% CI 1.3–1.2). Parker et al (1994)[28] found a greater risk of LBW among abused adult women compared to adolescents in a disadvantaged community in America. There is a negative report from China[26], but only violent threats were considered. A retrospective study from India, in which women recalled their last pregnancy, showed that victims of violence were significantly more likely to have experienced still birth or infant death [4], and Menezes et al [3] also reported an association with neonatal mortality. Recent studies of the association between antenatal common mental disorder and low birth weight are somewhat inconsistent in their findings. Reports of positive associations have tended to come from those living in conditions of absolute or relative socio-economic disadvantage. For example, Hoffman & Hatch[7] found a positive association, but only among women from a low social economic status in the USA. Two studies from South Asia[8, 9] and now our current study, of a disadvantaged population in Brazil, have also reported an independent association between CMD and LBW.
What are the possible mechanisms linking violence and mental disorder with adverse obstetric outcomes? The association between violence and low birth weight has been attributed to factors such as prematurity (caused by trauma), substance abuse (such as smoking), low socioeconomic status (leading to hunger), maternal medical problems and maternal mental illness [1, 31]. The same mediators might plausibly apply to the association with mental disorder. However, the associations we report were evident after adjustment for all these factors. It is possible that the associations were mediated by poor nutrition and self-care in mothers; for example, abusers limiting access to food and antenatal care[31]. There may also be more direct biological pathways; there is accumulating evidence in humans that the hypothalamopituitary axis is in overdrive in pregnant women subjected to psychosocial stress[34]. Cortisol crosses the placenta and high levels inhibit intrauterine growth[35, 36]. The fact that violence in pregnancy was associated with SGA but not with preterm babies, whereas CMD was associated with preterm birth but not SGA suggests different mechanisms for the two exposures on the pathway to low birth weight.
Conclusion
The effect of violence on young mothers who have limited personal and social resources can be devastating. Appropriate interventions are urgently required to avoid or minimize the effects of violence on the health of the mothers and the babies. The implication for clinical practice is that all adolescent mothers should be routinely screened for the experience of violence, both lifetime and during pregnancy, as well as for mental disorder. Identification of the one should alert clinical teams to the possibility of the other, given the strong correlations that we and others have reported. Exposed mothers should be treated as 'at risk', supported intensively during the pregnancy and monitored for fetal growth. Antenatal mental disorder seems particularly likely to be associated with adverse obstetric factors (drinking and smoking, poor physical health and premature birth). At the social policy level, concerted efforts are need to combat gender-based violence not only as a human rights issue but as a major risk factor for poor maternal and newborn health; health professionals must actively engage in this advocacy.
Further research, preferably utilizing longitudinal designs, is needed to tease out the causal mechanisms linking violence with maternal and newborn outcomes. Such studies should examine not only the role of physical violence but also the influence of behaviors that cause harm without the use of physical force including neglect, humiliation and non-violent coerced sexual acts. The role of protective factors, such as social support, also merits investigation.
References
Murphy CC, Schei B, Myhr TL, Du MJ: Abuse: a risk factor for low birth weight? A systematic review and meta-analysis.[see comment]. CMAJ Canadian Medical Association Journal 164(11):1567-72,. 2001, 164 (11): 1567-1572.
Valdez-Santiago R, Sanin-Aguirre LH: Domestic violence during pregnancy and its relationship with birth weight. [Spanish]. Salud Publica de Mexico 38(5):352-62,. 1996, Oct.
T.C. M, M.M.R. A, LC S, A F: Domestic Physical Violence and Pregnancy: Results of a Survey in the Postpartum Period. Revista Brasileira de Ginecologia & Obstetricia. 2005, 25: 309-316.
Jejeebhoy SJ: Associations between wife-beating and fetal and infant death: impressions from a survey in rural India. Studies in Family Planning 29(3):300-8,. 1998
Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M: Neonatal outcome following maternal antenatal depression and anxiety: a population-based study. American Journal of Epidemiology 159(9):872-81,. 2004
Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT: Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosomatic Medicine 63(5):830-4,. 2001, 63 (5): 830-834.
Hoffman S, Hatch MC: Depressive symptomatology during pregnancy: evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychology. 1919, 19 (6): 535-543. 10.1037/0278-6133.19.6.535.
V P, Prince M: Maternal psychological morbidity and the risk of low birth weight in poor countries. British Journal of Psychiatry (in press). 2006, 188: 284-285.
Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R: Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry. 2004, 61 (9): 946-952. 10.1001/archpsyc.61.9.946.
Golding JM: Intimate partner violence as a risk factor for mental disorders: A meta-analysis. 1999
Klein D, Zahnd E, Holtby S, Barth R: Perinatal Needs Assessment. St Study Final Report. 1994, Dacramento, CA: California Department of Alcohol and Drugs Programs
Zahnd E, Klein D: Substance Use and issues among low income pregnant women: the California Perinatal Needs Assessment. J Drugs Issues. 2005, 27: 563-583.
Quintana MI: Validity of the Brazilian version of the Composite International Diagnostic Interview (CIDI 2.1). 2005, PhD Thesis. Federal University of Sao Paulo, Department of Psychiatry.
Quintana MI, Andreoli SB, Jorge MR: The reliability of the Brazilian version of the Composite International Diagnostic Interview (CIDI 2.1). Braz J Med Bio Res. 2004, 37: 1739-1745.
Sykes GS, Molloy PM, Johnson P, Gu W, Ashworth F, Stirrat GM, Turnbull AC: Do Apgar scores indicate asphyxia?. Lancet. 1982, 1 (8270): 494-496. 10.1016/S0140-6736(82)91462-3.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R: New Ballard Score, expanded to include extremely premature infants. Journal of Pediatrics. 1991, 119 (3): 417-423. 10.1016/S0022-3476(05)82056-6.
WHO Expert Committee on Physical Status: The use and interpretation of anthropometrics Physical Status: The newborn infant. 2006
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, Blondel B, Breart G, Fetal/Infant Health Study Group of the Canadian Perinatal Surveillance System: A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001, 108 (2): E35-10.1542/peds.108.2.e35.
ANEP - Associcao Nacional de Empresas de Pesquisa (National Association of Research Companies).: Criteria of Economic Classification. [http://www.abep.org/]
Barros AJ, Hirakata VN: Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Medical Research Methodology. 2003, 3 (1): 21-10.1186/1471-2288-3-21.
IBGE Data from the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estattistica).: Brasil em sintese: population per age group. [http://www.ibge.gov.br]
Fraser AM, Brockert JE, Ward RH: Association of young maternal age with adverse reproductive outcomes.[see comment]. New England Journal of Medicine 332(17):1113-7,. 1995, 332 (17): 1113-1117. 10.1056/NEJM199504273321701.
Moraes CL, Reichenheim ME: Domestic violence during pregnancy in Rio de Janeiro, Brazil. International Journal of Gynaecology & Obstetrics. 2002, 79 (3): 269-277. 10.1016/S0020-7292(02)00250-3.
Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, Regan L, Robinson S: Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 2001, 25: 1175-1182. 10.1038/sj.ijo.0801670.
Purwar MB, Jeyaseelan L, Varhadpande U, Motghare V, Pimplakute S: Survey of physical abuse during pregnancy, GMCH, Nagpur, India. 2005, 25 (3): 165-171.
Leung WC, Wong YY, Leung TW, Ho PC: Pregnancy outcome following domestic violence in a Chinese community. International Journal of Gynaecology & Obstetrics 72(1):79-80,. 2001, 72 (1): 79-80. 10.1016/S0020-7292(00)00335-0.
Castro R, Ruiz A: [Prevalence and severity of domestic violence among pregnant women, Mexico]. [Spanish]. Revista de Saude Publica. 2004, 38 (1): 62-70.
Parker B, McFarlane J, Soeken K: Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstetrics & Gynecology. 1994, 84: 323-328.
Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR: Prevalence of depression during pregnancy: systematic review.[erratum appears in Obstet Gynecol. 2004 Jun;103(6):1344]. [Review] [78 refs]. Obstetrics & Gynecology. 2004, 103 (4): 698-709.
GM L, JRRA L, ESF C, V P: Poverty, violence and depression during pregnancy: a survey of mothers attending a public hospital in Brazil. 2005, 35 (10): 1485-1492.
Campbell JC: Health consequences of intimate partner violence.[see comment]. [Review] [83 refs]. Lancet. 2002, 359 (9314): 1331-1336. 10.1016/S0140-6736(02)08336-8.
Patel V, Kirkwood BR, Pednekar S, Pereira B, Barros P, Fernandes J, Datta J, Pai R, Weiss H, Mabey D: Gender disadvantage and reproductive health risk factors for common mental disorders in women: a community survey in India. Archives of General Psychiatry. 2006, 63 (4): 404-413. 10.1001/archpsyc.63.4.404.
Nasir K, Hyder AA: Violence against pregnant women in developing countries: review of evidence. [Review] [16 refs]. European Journal of Public Health. 2003, 13 (2): 105-107. 10.1093/eurpub/13.2.105.
O'Keane V, Scott J: From 'obstetric complications' to a maternal-foetal origin hypothesis of mood disorder. British Journal of Psychiatry. 2005, 186: 367-368. 10.1192/bjp.186.5.367.
Gitau R, Cameron A, Fisk NM, Glover V: Fetal exposure to maternal cortisol. Lancet. 1998, 352 (9129): 707-708. 10.1016/S0140-6736(05)60824-0.
French NP, Hagan R, Evans SF, Godfrey M, Newnham JP: Repeated antenatal corticosteroids: size at birth and subsequent development. American Journal of Obstetrics & Gynecology. 1999, 180 (1 Pt 1): 114-121. 10.1016/S0002-9378(99)70160-2.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/7/209/prepub
Acknowledgements
Support for this study was given by FAPESP (Fundacao de Amparo a Pesquisa do Estado de Sao Paulo – grant number 00/10293-5) which is a governmental Brazilian Institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
CPF, VP and MP participated in the study concept and design, analysis and interpretation of data, drafting the manuscript and reviewing the manuscript for important intellectual content. MB, EC, RG, RL and SM participated in the study concept and design, acquisition of data, obtaining funding and critically reviewed the paper for important intellectual content. All authors approved the version submitted.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ferri, C.P., Mitsuhiro, S.S., Barros, M.C. et al. The impact of maternal experience of violence and common mental disorders on neonatal outcomes: a survey of adolescent mothers in Sao Paulo, Brazil. BMC Public Health 7, 209 (2007). https://doi.org/10.1186/1471-2458-7-209
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-7-209