Abstract
Background
Forces deployed to the first Gulf War report more ill health than veterans who did not serve there. Many studies of post-Gulf morbidity are based on relatively small sample sizes and selection bias is often a concern. In a setting where selection bias relating to the ill health of veterans may be reduced, we: i) examined self-reported adult ill health in a large sample of male UK Gulf War veterans and a demographically similar non-deployed comparison group; and ii) explored self-reported ill health among veterans who believed that they had Gulf War syndrome.
Methods
This study uses data from a retrospective cohort study of reproduction and child health in which a validated postal questionnaire was sent to all UK Gulf War veterans (GWV) and a comparison cohort of Armed Service personnel who were not deployed to the Gulf (NGWV). The cohort for analysis comprises 42,818 males who responded to the questionnaire.
Results
We confirmed that GWV report higher rates of general ill health. GWV were significantly more likely to have reported at least one new medical symptom or disease since 1990 than NGWV (61% versus 37%, OR 2.7, 95% CI 2.5–2.8). They were also more likely to report higher numbers of symptoms. The strongest associations were for mood swings (OR 20.9, 95%CI 16.2–27.0), memory loss/lack of concentration (OR 19.6, 95% CI 15.5–24.8), night sweats (OR 9.9, 95% CI 6.5–15.2), general fatigue (OR 9.6, 95% CI 8.3–11.1) and sexual dysfunction (OR 4.6, 95%CI 3.2–6.6). 6% of GWV believed they had Gulf War syndrome (GWS), and this was associated with the highest symptom reporting.
Conclusions
Increased levels of reported ill health among GWV were confirmed. This study was the first to use a questionnaire which did not focus specifically on the veterans' symptoms themselves. Nevertheless, the results are consistent with those of other studies of post-Gulf war illness and thus strengthen overall findings in this area of research. Further examination of the mechanisms underlying the reporting of ill health is required.
Similar content being viewed by others
Background
Following the 1990–91 Gulf War there have been a number of published reports highlighting the increased morbidity of military personnel who served in the conflict. Studies from all over the world show that forces deployed to the Gulf (GWV) report more ill health than veterans who did not serve there (NGWV) [1–7]. In terms of the types of reported symptoms, different studies have discovered a range of nonspecific chronic conditions. Many research groups have noted that GWV are more likely to suffer from substantial fatigue, symptoms of post-traumatic stress, and psychological distress [1, 2, 4]. Others have also described peripheral, respiratory, gastrointestinal, psychological and concentration problems [3].
Despite millions of dollars of funding and several independent investigations in a number of countries [8], the increased morbidity of GWV remains an unexplained phenomenon. Media interest and anecdotal reports have fuelled speculation concerning the existence of a Gulf War syndrome (GWS), linking reports of ill health to certain hazardous exposures experienced during the conflict. Most notably these include anti-chemical warfare nerve agent prophylaxis (NAPS), depleted uranium, multiple vaccinations, smoke from oil fires and pesticide use. It is hypothesised that exposure to these hazards has led to the development of a unique syndrome among some GWV, including symptoms of post-traumatic stress disorder [4], fibromyalgia [9], chronic fatigue [1, 10] and multiple chemical sensitivity [10, 11]. However, attempts to specify and measure the syndrome have led to contradictory findings and interpretations [12]. Current opinion does not support the existence of a unique syndrome affecting GWV, but findings support an excess of non-specific self-reported ill health in this group [13, 14].
This is the largest UK study of post-Gulf War morbidity to date, and the first to approach all veterans of the Gulf war (rather than a sample), including both serving and discharged personnel. The questionnaire focused on reproduction and child health, but a page was included which asked for information on the study participants' changes in health status since 1990. Since the focus of the study was on reproduction and child health, we reasoned that selection bias relating to the ill health of the veterans themselves might be reduced. Previous studies have included tick-boxes or grading scales with a list of possible symptoms for respondents to mark and GWV have tended to report increased frequencies of almost all symptoms included in questionnaires [1, 3, 4]. In contrast, we asked participants to respond to an open-ended question about 'any new medical problems or changes in general health since 1990'. By allowing veterans to report on a full and non-specific range of symptoms using free text it was hoped that they would report only those symptoms which they felt were most important to them.
The main objective of this analysis was to quantify and describe symptoms and diseases reported by UK GWV and a comparison group since 1990. We aimed to determine whether GWV still report more ill health, and/or a different profile of symptoms and diseases than NGWV when, i) their children's rather than their own health was the focus of the study; and ii) details of their own ill health were requested in a non-specific way using free-text. In addition, we aimed to estimate the number of GWV who believed that they had Gulf war syndrome (GWS), and to compare their reported disease/symptom profiles with GWV who did not believe they had the syndrome.
Methods
Full details of the study are reported elsewhere [15]. In brief, the Gulf War cohort (GWV) consisted of all UK armed forces personnel deployed to the Gulf area at any time between August 1990 and June 1991 (51,581 men and 1,230 women). Special forces were excluded for security reasons. The comparison cohort (NGWV) comprised demographically similar personnel who were in service on 1st January 1991 and were appropriately fit, but were not deployed to the Gulf (51,688 men and 1,236 women). The group was stratum-matched on sex, age (five-year groups), service (Army, Navy, Air Force), rank (officer, other ranks), serving status at the time of the Gulf War (regular, reservist) and on fitness to be deployed (Army and Air Force only). 42,818 men and 1,269 women responded to the survey, representing response rates of 48% and 66% respectively after adjusting for undelivered mail. For reasons of statistical power, the analyses reported in this paper were restricted to the 42,818 male responders.
Basic demographic details and last known address for all surviving cohort members were obtained from the Ministry of Defence (MoD). Information was collected using a validated postal questionnaire sent to both serving and discharged military personnel between August 1998 and March 2001. In addition to questions on reproduction and pregnancy outcome, information was collected on the study participant's current health, and on changes in health status since 1990. Questions on service history, smoking status, current alcohol consumption, and details of vaccinations and exposure to specific chemical and environmental factors during the Gulf war (1990–91 for NGWV) were included. GWV were also asked if they considered that they had 'Gulf War syndrome' (Yes /No/Not Sure). Missing information was checked by letter or telephone, and an Intensive Tracing Study (ITS) of non-responders was conducted.
The primary outcome measure was the reporting of one or more new medical problems or changes in general health since 1990. Reported symptoms/diseases were coded into one of 36 different categories (based loosely on ICD-10 classification), and the data were examined by these ill health categories. Subjects were counted only once in the analysis if they had more than one symptom in the same category.
Statistical analysis
All analyses were performed using Stata 7.0 statistical software [16]. All p-values quoted are two-sided and values less than 0.05 were taken to indicate statistical significance. t-tests were conducted on log transformed data to compare the average number of ill health categories reported per subject in different groups. The association between deployment and ill health was explored using logistic regression analysis, calculating odds ratios and 95%CIs (with NGWV as baseline) for each ill health category. We adjusted for age at survey, service, rank, serving status at time of survey, smoking status and current alcohol consumption in all models.
Results
Response
Data supplied by all male respondents are analysed here (24,379 GWV; 18,439 NGWV). Characteristics of these men and of those reporting one or more medical problems arising since 1990 are presented in Table 1. GWV responders were slightly younger than NGWV responders, and were more likely to have served in the Army, to not be an officer, to have left the Armed Services, to have ever smoked, and to have consumed larger amounts of alcohol. However, the differences in the distributions were not large. Among those reporting one or more medical symptom/disease, GWV were again younger, more likely to serve in the Army, to not be an Officer, and to have ever smoked.
Symptoms/diseases
61% of GWV reported at least one new medical symptom since 1990 compared with 37% of NGWV (adjusted OR 2.7, 95% CI 2.5–2.8). The data are presented by ill health category in Table 2 in order of frequency of reporting by GWV (highest to lowest). The most common symptoms/diseases reported by GWV were skeletal and other muscular symptoms (15.1%), 'other' symptoms (13.1%), general fatigue (10.8%), memory loss/lack of concentration (7.9%) and skin allergies (7.6%). Accidental injury (2.6%) was among one of the most common ill health categories reported by NGWV. Overall, GWV reported significantly more symptoms/diseases than NGWV. Among all those reporting one or more new symptom/disease since 1990, GWV reported a median of two different ill health categories per subject (range 1–23), while NGWV reported a median of one (range 1–17) (p < 0.001).
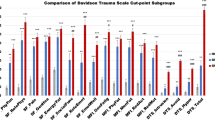
For over 85% of categories of ill health, symptom/disease prevalence was higher among GWV (Figure 1; Table 2). Strongest associations with Gulf war service included mood swings (OR 20.9, 95%CI 16.2–27.0), memory loss/lack of concentration (OR 19.6, 95% CI 15.5–24.8), night sweats (OR 9.9, 95% CI 6.5–15.2), general fatigue (OR 9.6, 95% CI 8.3–11.1) and sexual dysfunction (OR 4.6, 95%CI 3.2–6.6). Adjustment for potential confounding factors had little impact on these associations, none changing the ORs by more than about 3–4% on average.
Gulf War syndrome (GWS) among GWV
23,103 GWV answered the question "Do you consider that you have "Gulf War Syndrome"?". 5.6% believed that they had the syndrome (GWS) and 40.9% stated that they were 'unsure' (Table 1). Among all GWV reporting one or more new symptom/disease since 1990, veterans who believed that they had GWS reported the highest number of different symptoms/diseases (median = 3; range 1–23), with those who were unsure (unsure-GWS) reporting more symptoms/diseases (median = 2; range 1–15) than those who stated that they did not (non-GWS) (median = 1; range 1–10 categories per subject); (χ2 trend: p < 0.001). For all but one ill health category (accidental injury), those who believed that they had GWS reported the highest symptom/disease prevalence, with unsure-GWS reporting intermediate frequencies for all categories (Table 3; Figure 2).
Discussion
This is the largest study of male UK veterans of the first Gulf war and the only one to approach all those deployed. Unlike other Gulf war studies, information on ill health arising since the war was collected using free text. Our study confirmed that GWV were significantly more likely to report at least one new medical problem since 1990 than a non-deployed comparison group. It also confirmed that veterans were more likely to report higher numbers of symptoms/diseases. These typically included skeletal and other muscular symptoms, general fatigue, memory loss/lack of concentration, skin allergies, mood swings/aggression and headaches. This pattern of symptom reporting is similar to that found in other studies of UK GWV [1–3], which looked at the same populations using different methods. For example, Unwin et al [1] found that GWV reported all symptoms (in pre-defined categories) at higher frequencies than NGWV in their study of a sample of UK veterans with two matched comparison groups, while we found that GWV reported higher prevalence in 85% of ill health categories.
In terms of the nature of self-reported ill health, we found similar results to the range of symptoms that have been reported elsewhere. Gray et al's [17] study of GWV found that over 50 percent of diagnoses could be classified into four large categories: diseases of the musculoskeletal system and connective tissue (19.0%), mental disorders (14.7%), diseases of the respiratory system (10.5%) and diseases of the skin and subcutaneous tissue (9.4%). In our study the same four categories accounted for 50.3 percent of all reported symptoms/diseases and this figure rises to over 70 percent when the categories of fatigue and nervous system disorders are included. An additional point concerns the higher levels of accidental injury reported by NGWV veterans; accidents were only half as likely to occur among GWV compared to NGWV (1.3% versus 2.6%). This was surprising as mortality from accidents has repeatedly been found to be raised among GWV [18]. This difference is probably due to the inclusion of both major and minor injuries (including those resulting in bone fractures) in our study, and because GWV may be more inclined to report things they think are associated with their Gulf War service.
Our findings on Gulf War syndrome (GWS) approximate those from other studies [12–14, 19, 20]. A significant proportion of GWV believed that they had GWS (5.6%) and this belief was associated with increased symptom reporting. This figure was lower than that reported by other studies (Chalder et al [12] found that 17.3% of GWV believed that they had GWS), but we are the first group to report on a large proportion of GWV who were 'unsure' of their GWS-status (40.9%). 'Unsure' veterans generally reported intermediate frequencies of ill health between those veterans who believed that they had GWS and those that did not. In a sample of UK veterans, Chalder et al [12] found that those who believed they had GWS were more fatigued, more distressed, and more likely to have a post-traumatic stress reaction than veterans who did not believe they suffered from GWS. Our data showed that GWS veterans reported higher frequencies of all categories of ill health (except accidental injury), including skeletal and other muscular symptoms, general fatigue, mood swings, memory loss/lack of concentration and headaches. In common with results from other studies of GWV [13, 14, 19, 21], those who stated that they had Gulf War syndrome reported the same types of symptoms as all GWV, but reported them at higher frequencies, providing evidence against a unique syndrome.
Study limitations
In the absence of an official register or a mandatory health evaluation programme, obtaining accurate information from post-combat veterans is a difficult process and one which inevitably relies on self-reporting. This method of data collection introduces possible selection bias into a study. After adjusting for undelivered mail, response rates among men were 53% for GWV and 42% for NGWV [15]. Given the relatively low response rate, an intensive tracing study of non-responders was conducted to investigate possible selection bias. Data from the study indicated that the majority of reasons given for previous non-participation were entirely unrelated to reproduction or Gulf War service. Ninety percent of the reasons given by both GWV and NGWV for earlier non-response related to such things as not remembering receiving a questionnaire, thinking they had sent it back, or general 'mistrust' of the MoD [15]. It might therefore be concluded that response bias relating to adverse health outcomes was not large in this study.
In terms of suitable controls, an advantage of this study was the comparison of GWV with another military cohort. Comparisons with civilian populations may have been misleading as military recruitment involves medical and fitness screening. Furthermore, 'healthy warrior' bias (where veterans deployed to the Gulf might be healthier than those who were not deployed) [22–24] is unlikely to account for the findings in our study because the comparison group were broadly matched to the GWV on fitness to be deployed.
A potential problem with any retrospective study design is recall bias. The questionnaire asked veterans to consider any new medical problems or changes in general health they had experienced since the end of the Gulf War, and this involved them recalling events that might have happened up to seven or eight years in the past. During this time there has been much media speculation over Gulf War illness and this may have introduced recall bias and led to under- or over-reporting of certain symptoms. Gray et al have shown that participation in Gulf War health registries is greatly influenced by media attention and is likely to be influenced by compensation issues. This was illustrated by increased enrollment during periods of high media interest in Gulf War issues [17]. A further limitation of this study concerns the lack of clinical validation of self-reported ill health. However, conducting clinical examinations and psychiatric assessments of every veteran would have been time consuming and prohibitively expensive. Furthermore, studies looking at 'hard' clinical diagnoses or more objective outcomes, such as cancer [25] or hospitalisation rates [26], have shown no important differences between GWV and comparison groups. Researchers have concentrated instead on differences in 'softer' endpoints [1–3], which are similar to those reported here.
Conclusions
This study is consistent with other research showing a significant excess of morbidity among GWV. It also confirms the lack of specificity in post-Gulf war illness. These findings were replicated despite the fact that reproduction and child health were the focus of the study (rather than the veterans' general health), and questions relating to the veterans' own health were open-ended. Research groups have linked post-Gulf War ill health to a number of self-reported exposures but these analyses are limited by a lack of independent individual-level exposure data [1, 27, 28]. It has been suggested that changes in perception resulting from the disruption of war rather than specific exposures might be responsible [3], and there have been calls to move away from this narrow focus [29]. In the Gulf, disruption included change of climate, living conditions, diet, sleeping patterns, physical activity and separation from family, as well as the threat of chemical and biological weapons [27]. Despite such conjecture, explaining the increased ill health of GWV remains a controversial subject and there is no real consensus of opinion. In order for more rigorous aetiological studies of post-conflict illness to be undertaken in the future, there is a need to improve routine health surveillance and record-keeping both pre- and post- deployment [30]. This surveillance should also translate into more effective prevention and treatment programs in order to reduce the burden of post-war illness. Further research on the mechanisms underlying the reporting of ill health is required and this will entail a more qualitative approach to the problem of Gulf War illness. Continued quantitative documentation of the long-term health outcomes of Gulf War veterans remains essential.
Abbreviations
- GWS:
-
Gulf War syndrome
- GWV:
-
Gulf War veterans
- MoD:
-
Ministry of Defense (UK)
- NGWS:
-
non-Gulf War syndrome
- NGWV:
-
non-Gulf War veterans (comparison group)
- RAF:
-
Royal Air Force
- RN:
-
Royal Navy
References
Unwin C, Blatchley N, Coker W, Ferry S, Hotopf M, Hull L, Ismail K, Palmer I, David A, Wessely S: Health of UK servicemen who served in Persian Gulf War. Lancet. 1999, 353: 169-78. 10.1016/S0140-6736(98)11338-7.
Hotopf M, David AS, Hull L, Nikalaou V, Unwin C, Wessely S: Gulf war illness-better, worse, or just the same? A cohort study. BMJ. 2003, 327 (7428): 1370-10.1136/bmj.327.7428.1370.
Cherry N, Creed F, Silman A, Dunn G, Baxter D, Smedley J, Taylor S, Macfarlane GJ: Health and exposures of United Kingdom Gulf war veterans. Part I: The pattern and extent of ill health. Occup Environ Med. 2001, 58 (5): 291-8. 10.1136/oem.58.5.291.
The Iowa Persian Gulf Study Group: Self-reported illness and health status among Gulf War veterans. A population-based study. JAMA. 1997, 277 (3): 238-45.
Ishoy T, Suadicani P, Guldager B, Appleyard M, Hein HO, Gyntelberg F: State of health after deployment in the Persian Gulf. The Danish Gulf War Study. Dan Med Bull. 1999, 46 (5): 416-9.
Australian Gulf War Veterans' Health Study. Executive Study. 2003, Monash University
Health study of Canadian forces personnel involved in the 1991 conflict in the Persian Gulf. Ottawa: Goss Gilroy. 1998
Military and Veterans Health Coordinating Board: Annual Report to Congress: Federally Sponsored Research on Gulf War Veterans' Illnesses for 2001; Washington, DC. 2001
Erickson AR, Enzenauer RJ, Bray VJ, West SG: Musculoskeletal complaints in the Persian Gulf War veterans. J Clin Rheumato. 1998, 4: 181-5. 10.1097/00124743-199808000-00002.
Kipen HM, Hallman W, Kang H, Fiedler N, Natelson BH: Prevalence of chronic fatigue and chemical sensitivities in Gulf Registry Veterans. Arch Environ Health. 1999, 54 (5): 313-8.
Reid S, Hotopf M, Hull L, Ismail K, Unwin C, Wessely S: Reported chemical sensitivities in a health survey of United Kingdom military personnel. Occup Environ Med. 2002, 59 (3): 196-8. 10.1136/oem.59.3.196.
Chalder T, Hotopf M, Unwin C, Hull L, Ismail K, David A, Wessely S: Prevalence of Gulf war veterans who believe they have Gulf war syndrome: questionnaire study. BMJ. 2001, 323: 473-6. 10.1136/bmj.323.7311.473.
Ismail K, Everitt B, Blatchley N, Hull L, Unwin C, David A, Wessely S: Is there a Gulf War syndrome?. Lancet. 1999, 353: 179-82. 10.1016/S0140-6736(98)11339-9.
Knoke JD, Smith TC, Gray GC, Kaiser KS, Hawksworth AW: Factor analysis of self-reported symptoms: does it identify a Gulf War Syndrome?. Am J Epidemiol. 2000, 152 (4): 379-88. 10.1093/aje/152.4.379.
Maconochie N, Doyle P, Davies G, Lewis S, Pelerin M, Prior S, Sampson P: The study of reproductive outcome and the health of offspring of UK veterans of the Gulf war: methods and description of the study population. BMC Public Health. 2003, 3 (1): 4-10.1186/1471-2458-3-4.
StataCorp Stata statistical software: release 7.0. College Station, TX: Stata Corporation. 1999
Gray GC, Hawksworth AW, Smith TC, Kang HK, Knoke JD, Gackstetter GD: Gulf War Veterans' Health Registries. Who is most likely to seek evaluation?. Am J Epidemiol. 1998, 148 (4): 343-9.
Kang HK, Bullman TA, Macfarlane GJ, Gray GC: Mortality among US and UK veterans of the Persian Gulf War: a review. Occup Environ Med. 2002, 59 (12): 794-9. 10.1136/oem.59.12.794.
Doebbeling BN, Clarke WR, Watson D, Torner JC, Woolson RF, Voelker MD, Barrett DH, Schwartz DA: Is there a Persian Gulf War syndrome? Evidence from a large, population-based survey of veterans and nondeployed controls. Am J Med. 2000, 108 (9): 695-704. 10.1016/S0002-9343(00)00405-8.
Murphy FM: Gulf war syndrome. BMJ. 1999, 318: 274-5.
Fukuda K, Nisenbaum R, Stewart G, Thompson WW, Robin L, Washko RM, Noah DL, Barrett DH, Randall B, Herwaldt BL, Mawle AC, Reeves WC: Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA. 1998, 280 (11): 981-8. 10.1001/jama.280.11.981.
Haley RW: Point: bias from the "healthy warrior effect" and unequal follow-up in three government studies of health effects of the Gulf War. Am J Epidemiol. 1998, 148 (4): 315-23.
Kang HK, Bullman TA: Counterpoint: Negligible "healthy-warrior effect" on Gulf War Veterans' mortality. Am J Epidemiol. 1998, 148 (4): 324-5.
Gray GC, Knoke JD, Berg SW, Wignall FS, Barrett-Connor E: Counterpoint: Responding to suppositions and misunderstandings. Am J Epidemiol. 1998, 148 (4): 328-33.
Macfarlane GJ, Biggs A, Maconochie N, Hotopf M, Doyle P, Lunt M: Incidence of cancer among UK Gulf war veterans: cohort study. BMJ. 2003, 327 (7428): 1373-10.1136/bmj.327.7428.1373.
Gray GC, Coate BD, Anderson CM, Kang HK, Berg SW, Wignall FS, Knoke JD, Barrett-Connor E: The postwar hospitalization experience of U.S. veterans of the Persian Gulf War. N Engl J Med. 1996, 335: 1505-13. 10.1056/NEJM199611143352007.
Hotopf M, David A, Hull L, Ismail K, Unwin C, Wessly S: Role of vaccinations as risk factors for ill health in veterans of the Gulf war: cross sectional study. BMJ. 2000, 320: 1363-7. 10.1136/bmj.320.7246.1363.
Cherry N, Creed F, Silman A, Dunn G, Baxter D, Smedley J, Taylor S, Macfarlane GJ: Health and exposures of United Kingdom Gulf war veterans. Part II: The relation of health to exposure. Occup Environ Med. 2001, 58 (5): 299-306. 10.1136/oem.58.5.299.
Clauw D: The health consequences of the first Gulf war. BMJ. 2000, 327 (7428): 1357-8. 10.1136/bmj.327.7428.1357.
Joellenbeck LM, Russell PK, Cuze SB, eds: Strategies to protect the health of deployed US forces. 1999, Washington DC: National Academy Press
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/4/27/prepub
Acknowledgements
We would like to thank the many people who supported the conduct of this study: Representatives of the Armed Services, the British Legion, in particular Col Terry English, National Gulf Veterans and Families Association, Gulf Veterans Association, and, most importantly, the study members themselves for taking the time and effort to participate. We also acknowledge the skills and commitment of those who worked on the study, particularly Graham Davies, Sam Lewis, Margo Pelerin, Susan Prior, Patrick Sampson, Tommy Clarke, Haydon Hughes, Juliet Jain, Darren Reed and Janet Sullivan. For supplying cohort data and for invaluable help with queries, we thank all members of the Gulf Veterans Illness Unit at the Ministry of Defence, in particular Nick Blatchley, John Graham, Philip Bolton, Linda Walpole and Chris Baker. We appreciate the work of Steve McManus and colleagues at the British Forces Post Office for providing valuable serving status and address information on a regular basis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
RS performed the statistical analysis and drafted the manuscript. NM and PD designed the study and contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Simmons, R., Maconochie, N. & Doyle, P. Self-reported ill health in male UK Gulf War veterans: a retrospective cohort study. BMC Public Health 4, 27 (2004). https://doi.org/10.1186/1471-2458-4-27
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-4-27