Abstract
Background
Depression is a common and mostly undertreated problem in patients with chronic diseases. However, population-based studies on the association between chronic obstructive pulmonary disease (COPD) and subsequent depression are limited in Asian populations. This study evaluated the incidence and risk factors of depression for patients with COPD in Taiwan.
Methods
Using the claims data from the National Health Insurance of Taiwan, we identified 38,010 COPD patients newly diagnosed in 2000–2004 and 38,010 subjects without COPD frequency, matched by sex, age and index date. The incidence rate and hazard ratio for depression were estimated by the end of 2008.
Results
The incidence rate of depression was 1.88 folds higher in the COPD cohort than in the non-COPD cohort (12.2 versus 6.47 per 1,000 person-years, p < 0.0001). The depression risk was the greatest within the first year following COPD diagnosis and tended to decline with follow-up time. Among COPD patients, multivariate analysis showed that younger women and low-income patients were at higher risk of depression. Hospitalization and comorbidities such as hypertension, arthritis, cancer, and heart disease were also significant predictors for depression risk.
Conclusion
This population-based cohort study demonstrated a strong relationship between COPD and subsequent depression. These findings could assist healthcare providers to pinpoint individuals with a higher predisposition to having depression, which could then facilitate the provision of culturally appropriate rehabilitation within the first year after the diagnosis of COPD.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is characterized by airflow obstruction, which leads to the slow, progressive symptoms of persistent cough, exertional dyspnea, wheezing, and eventually functional impairment [1]. World Health Organization (WHO) has reported in the Global Burden of Disease Project that approximately 5 of 100 deaths worldwide are associated with COPD [2]. At this rate, COPD may rank as the third leading cause of death in the world by 2020 [3]. Given the complex symptoms and long duration of COPD, the medical expenses for curing the disease cannot be ignored. A study by Menzin et al. [4] found that the average medical expenses per COPD patient per year was estimated at US$27,656, which is nearly 4 times higher than the average cost for patients without COPD (US$7,126). In a review of the financial burden of COPD in USA, the authors estimated that the annual direct medical costs for COPD amounted to $21.8 billion, and the indirect costs for restricted days, lost workdays, and productivity were at $17 billion [5].
COPD does not only cause enormous economic burden, it also triggers subsequent illnesses. The risk of lung cancer for COPD patients is more than two folds higher than for those without the disease [6]. Curkendall et al. also confirmed that COPD patients have a 60%–80% higher risk of developing cardiovascular diseases compared with the general population [7]. Given the irreversible nature and unsatisfactory prognostic outcomes, COPD patients are frequently diagnosed with psychiatric disorders, particularly depression [8]. A systematic review of 64 studies on patients with chronic disease concluded that the prevalence of depression ranged from 37% to 71% in COPD patients, figures comparable to or higher than prevalence rate in patients with other chronic diseases, such as cancer, AIDS, heart disease, and renal disease [9]. Depression not only increases hospitalization and emergency visits by 48% and 77%, respectively, in COPD patients [10], but also doubles the likelihood of dying from the comorbidities of COPD-related depression [11]. Therefore, depression has become a matter of great healthcare concern for COPD patients and their families.
Studies on COPD-related depression have been conducted mainly on Western populations but rarely for people of Asian descent [12]. Chinese, in particular, often consider depression to be a taboo issue and they may suffer more in terms of emotional distress [13, 14]. Previous studies on Chinese COPD patients have focused on the effect of medical treatments [15], mortality [16], and the subsequent risk of skin disease following COPD [17]. In contrast, data related to the psychological issues, especially depression, among Asian patients with COPD are limited. Few studies investigating the influencing factor of depression among Chinese COPD patients have been conducted, but these studies were limited to a cross-sectional design and small sample sizes [18, 19]. We conducted a follow-up study to determine the association between depression risk and COPD using claims data from the National Health Insurance (NHI) of Taiwan to evaluate the risk of depression in Oriental patients with COPD. Apart from being a preliminary study of depression in COPD patients, its findings should be able to help healthcare providers identify potential cases of having depression and this will allow more efficient interventions to improve the quality of life for them.
Methods
Data source
In order to remove financial barriers to medical care for all residents, Taiwan Department of Health launched a single-payer NHI Program in 1995. At the end of 2008, over 99% of Taiwan’s population was enrolled in this program [20]. The National Health Research Institutes in Taiwan has been responsible to manage the insurance claims data and established several sets of Longitudinal Health Insurance Databases (LHID), providing to scientists in Taiwan for research purposes. This study used a subset of NHI database, which contained the utilization and enrollment information for a randomly selected of one million NHI beneficiaries, representing 5% of all enrollees in Taiwan in 2000. Because a multistage stratified systematic sampling method was applied, there were no statistically significantly differences in sex or age between the sample group and all enrollees [20]. All data files can be linked with scrambled identifications. Our study was thus exempted from full review by the Institutional Review Board (Research Ethnics Committee, Buddhist Dalin Tzu Chi Hospital).
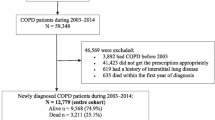
Study population
Diagnoses in the insurance claims data were coded with International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM). From records in LHID, we identified patients with COPD among adults newly diagnosed during 2000–2004 with the ICD codes of 491, 492, and 496 as the COPD cohort. To reduce the misclassification, we selected patients with at least two diagnosis of COPD in outpatient visits within 12 months or patients being admitted to hospital with a primary diagnosis of COPD during the 5-year period [17, 21].
A comparison cohort was randomly selected from the remaining insured population without COPD. For each COPD patient, one person free of COPD was selected frequency matched with sex, age, and the index date of COPD. After excluding subjects with a history of depression at the baseline, we identified 38,010 patients with COPD and 38,010 subjects in non-COPD cohort for data analysis. All subjects were followed up to the end of 2008 to measure the incidence of depression. We identified subjects as having depression if they had at least two treatment claims for depression in outpatient visits or hospitalization with depression for ICD-9-CM codes of 296.2, 296.3, 300.4, or 311 during the follow-up period. Follow-up person-years (PYs) were determined by calculating the time interval from the entry date to the earliest of one of the following: a diagnosis of depression, the date of withdrawal from the insurance, or the date of December 31, 2008.
Demographic variables and comorbidities
The demographic variables used in this study included age, gender, income for estimating insurance payment, and urbanization of the subject’s residential area. The monthly incomes were divided into three levels: ≤NT$17,880, NT$17,881–$43,900, and ≥NT$43,901. An income of NT$17,880 was the government-stipulated minimum for full-time employees in Taiwan. Urbanization levels were stratified into three strata, namely urban (levels 1–2), suburban (levels 3–4) and rural (levels 5–7) areas, based on population density. Level 1 refers to the “most urbanized” and level 7 refers to the “least urbanized” communities [22]. The baseline comorbidity was also identified for each subject, including hypertension (ICD9-CM 401–405), arthritis (ICD9-CM 715, 716.90), diabetes (ICD9-CM 250), heart disease (ICD9-CM 410–429), chronic kidney disease (ICD9-CM 585), and cancer (ICD9-CM 140–208).
Statistical analysis
We performed the χ2 test to examine the differences in demographic characteristics and comorbidities between the COPD and comparison cohorts. The incidence rate of depression for the two cohorts was presented with the number of cases per 1,000 PYs. COPD patients were further divided into two groups based on initial way of medical care seeking, and examined the incidence rate of depression among them. Cox proportional hazards regression analysis was applied to compute the hazard ratio (HR) and 95% confidence intervals (CI) of depression for COPD compared with the comparison cohort. We also used multivariate Cox proportional hazards model to determine the risk factors that might predict depression and their adjusted hazard ratio (aHR) within the COPD cohort. We further evaluated whether the relation between COPD and depression risk differed over time by sex. All analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA), and p < 0.05 was considered significant.
Results
Baseline and depression incidence between two cohorts
Table 1 shows the distributions of the demographic data and comorbid medical disorders for the COPD and comparison cohorts. Patients with COPD were more likely to have a lower monthly income (p < 0.0001), reside in rural areas (p < 0.0001), and suffer comorbidities, such as hypertension, arthritis, diabetes, heart disease, chronic kidney disease, and cancer (all p < 0.0001).
Of the total sample of 76,020 patients, 4,109 had incident depression during the follow-up period. The incidence of depression in the COPD cohort was nearly two folds higher than that in the comparisons (12.19 vs. 6.47 per 1,000 PYs) with an aHR of 1.88 (95% CI 1.74–1.98; Table 2). The depression risk was slightly greater for inpatients than for outpatients with COPD, with aHR of 2.29 (95% CI: 1.98–2.65) and 1.85 (95% CI: 1.74–1.98).
Relative risk of depression among COPD cohorts
The multivariate Cox proportional-hazard regression analysis estimated the aHR of depression in COPD patients by demographic status and comorbidity (Table 3). Age, gender, monthly income and hospitalization were significantly related to the risk of depression in COPD patients. Compared with the oldest group (≥70 years old), the risk of depression was 15% higher for those aged ≦ 50 years of age; those aged 51–70 also had an excess risk of 11%. Female sex was related to an aHR of 1.19 for depression, as compared to male. With regard to monthly income, aHR compared to the subjects with high monthly income was 1.09 for those with median monthly income, and 1.23 for those with low monthly income. Furthermore, the aHR was 1.16 times greater for COPD inpatients than COPD outpatients. Comorbidity increased the depression risk, with the highest risk for those with heart disease (aHR 1.47, 95% CI 1.35–1.61), followed by those with arthritis (aHR 1.32, 95% CI 1.21–1.44), cancer (aHR 1.24, 95% CI 1.06–1.45), and hypertension (aHR 1.12, 95% CI 1.03–1.23).
Additionally, we found the risk of depression across the period following COPD diagnosis was 2.01 (95% CI: 1.72–2.32) in year one. The aHR decreased with follow-up time to 1.40 (95% CI: 1.22–1.60) after year 5 (Table 4). The sex-specific patterns during the follow-up period were similar for males and females, but higher for females.
Discussion
Previous studies have shown that emotional impairments, depression in particular, are common among COPD patients, but mainly in Western populations. To the best of our knowledge, the present study is the first population-based cohort study addressing the association between COPD and the risk of subsequent depression in an Asian population. The results are consistent with findings in previous studies on Western populations [8, 23, 24]. The likely explanation for this finding was as follows. COPD patients may require more daily care due to gradually worsening physical conditions, which may lower self-esteem and self-efficacy, inducing a higher risk of depression [9]. Schane et al. found that COPD patients of lower education, living alone and female gender were more likely to have depression [8]. A cross-sectional study in China also found low income COPD patients are more likely depressive [25]. Our study revealed similar socioeconomic association, indicating the elderly and low income COPD patients are at higher risk of depression.
Additionally, the same debilitating and continuous physical symptoms may also trigger cognitions of “learned helplessness”, such that one’s inability to successfully cope with physical deterioration and life threatening situations result in increased levels of uncertainty, unpredictability and ultimately emotional distress and depression [26]. On the other hand, several inflammatory cytokines, such as tumor necrosis factor-α (TNF-α) or interleukin-6 (IL-6), have been considered pathogenic factors associated with the mechanism of developing depression [27]. A meta-analysis containing 24 studies indicated that the inflammatory cytokines may regulate adult neurogenesis to induce hippocampal neurogenesis atrophy, which has been implicated as a key contributing mechanism in the pathophysiology and treatment of depression [28].
The depression incidence among COPD patients in this study is somewhat lower than that in a previous report [24]. The difference may stem from the different composition of the two groups of participants. In addition, the stigma of mental illness is particularly entrenched in Asian patients and they may be unwilling to acknowledge or admit feelings of depression [13]. Depression, in many Asian countries, is an embarrassing issue for the general population to openly seek regular psychotherapy. Most importantly, less than 20% of patients with COPD have ever received appropriate psychiatric treatment since they were diagnosed with COPD [19]. Therefore, the implementation of a standardized care process, including some screening tools applicable to COPD patients, may be of utmost importance.
Our study indicated that women are at a 1.19-fold greater risk of depression than men in the COPD cohort, which supports the findings of previous studies [8, 24]. Two reasons may account for this phenomenon. First, women are more health consciousness than men and more likely to seek medical care during irregularities in their well-being [29]. Moreover, women are traditionally more obedient, passive, and emotional, which may insidiously elevate the risk of depression [30]. In contrast, our finding contradicts those reported by van Manen et al. [31]. A small sample size of 162 subjects used in their study may lead to a null association between the depression risk and gender.
We found a lower risk of depression in patients with higher monthly incomes than in those with lower monthly incomes, which is in line with previous studies [30, 32]. Patients with higher incomes may have better financial resources in dealing with the challenges engendered by COPD. This result, however, is inconsistent with that reported by Lin et al. [33], which may stem from the use of a different study design. Given that establishing a clear causality with the cross-sectional design is difficult, erroneously determining the effect of risk factors is possible [34].
Consistent with previous studies [8, 18, 31], we found that younger COPD patients were at a higher hazard for depression than the elderly. Most of the young COPD patients were employed; therefore their workload may have contributed to additional emotional distress. More importantly, our results demonstrated that the incidence of depression is higher in COPD inpatients than in outpatients. This finding indicates that severe COPD, which requires hospitalization, may trigger an increased risk of depression. Similar to previous report [35], we also noted that the risk of depression in COPD patients was higher within one year after diagnosis. The newly diagnosed patients may be highly fragile and overwhelmed by COPD symptoms. These findings suggest that healthcare providers need to pay closer attention to newly diagnosed patients with COPD, particularly inpatients. Interventions geared toward providing emotional support to enhance the psychological adjustment of patients may be of utmost importance.
COPD patients with other comorbidities, such as hypertension, arthritis, heart disease, or cancer had a significantly higher risk of depression, whereas those with diabetes mellitus and chronic kidney disease were at borderline significance. Our findings are partially paralleled with those of a previous study [8], indicating that comorbidities are associated with the predisposition for depression among COPD patients. The occurrence of comorbidities could play a role in weakening the perceptions of health status among COPD patients, thus leading to increased risk of depression. Additionally, a review article demonstrated that a depressive mood might be related to medication, such as antihypertensive agents, corticosteroids, or other biological agents [36]. So it was suggested that clinicians should actively assess existing medications prior to initiating depression-related treatments for COPD patients, which may reduce the risk of depression after COPD diagnosis.
Several limitations in this study should be mentioned. First, information on tobacco use, social network relationships, religious belief, and education level was unavailable from the claims data, which may be related to depression. Further study linking administrative data and the above mentioned information is warranted to examine the impact of these potential confounding variables on depression. Second, inaccurate diagnoses may occur. Therefore, we selected only those subjects with COPD or depression with at least two consistent outpatient visits or one inpatient admission to minimize this error. Furthermore, NHI has randomly sampled claims from hospitals and randomly interviewed patients, as well as reviewed medical charts to verify the accuracy of medical records. Finally, data regarding the severity of COPD, such as lung function data, were not available in the database. We were unable to estimate the dose–response relations between COPD severity and depression. Despite these methodological concerns, this population-based cohort study has been successful in examining the relationship between COPD and the subsequent risk of depression among Chinese patients. The retrospective cohort study design per se provided stronger evidence on the relationship between COPD and depression risk compared with previous studies.
Conclusions
Findings from this study reveal that the depression risk is nearly two folds higher for COPD patients than for general population. The risk of depression is related to being female and young, as well as with lower monthly income and comorbidity, such as hypertension, arthritis, cancer, and heart disease. Healthcare providers could be able to better understand the demographic and diseases characteristics that may contribute to the depression risk from this population-based study. The need to routinely screen COPD patients for depression and institute culturally appropriate interventions should be emphasized, especially within the first year since COPD diagnosis. Healthcare providers must be cognizant of the existence of depression among COPD patients and inform them by standard care process to avoid potential embarrassment when discussing psychiatric-related issues; this will help to achieve better therapeutic outcomes for them.
References
Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L: Definition, epidemiology and natural history of COPD. Eur Respir J. 2007, 30: 993-1013.
World Health Organization: The global burden of disease: 2004 update. 2012, http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf,
Murray CJ, Lopez AD: Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet. 1997, 349: 1498-1504.
Menzin J, Boulanger L, Marton J, Guadagno L, Dastani H, Dirani R, et al: The economic burden of chronic obstructive pulmonary disease (COPD) in a U.S. medicare population. Respir Med. 2008, 102: 1248-1256.
Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J: Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006, 3: 211-218.
Turner MC, Chen Y, Krewski D, Calle EE, Thun MJ: Chronic obstructive pulmonary disease is associated with lung cancer mortality in a prospective study of never smokers. Am J Respir Crit Care Med. 2007, 176: 285-290.
Curkendall SM, DeLuise C, Jones JK, Lanes S, Stang MR, Goehring E, et al: Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006, 16: 63-70.
Schane RE, Walter LC, Dinno A, Covinsky KE, Woodruff PG: Prevalence and risk factors for depressive symptoms in persons with chronic obstructive pulmonary disease. J Gen Intern Med. 2008, 23: 1757-1762.
Hynninen KM, Breitve MH, Wiborg AB, Pallesen S, Nordhus IH: Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res. 2005, 59: 429-443.
Dalal AA, Shah M, Lunacsek O, Hanania NA: Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD. 2011, 8: 293-299.
de Voogd JN, Wempe JB, Koëter GH, Postema K, van Sonderen E, Ranchor AV, et al: Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009, 135: 619-625.
Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, et al: Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008, 134: 43S-56S.
Yeh YH, Lin CH: A questionnaire study of depression related help-seeking behavior among the general public in Taiwan. Formos J Ment Health. 2005, 19: 125-148.
Karasz A: Cultural differences in conceptual models of depression. Soc Sci Med. 2005, 60: 1625-1635.
Lin PH, Chen PP, Lee JD: Outcome of in-patients with chronic obstructive pulmonary disease requiring non-invasive positive pressure ventilator. J Resp Ther. 2009, 8: 13-25.
Kuo LC, Yang PC, Kuo SH: Trends in the mortality of chronic obstructive pulmonary disease in Taiwan, 1981–2002. J Formos Med Assoc. 2005, 104: 89-93.
Yang YW, Chen YH, Wang KH, Wang CY, Lin HW: Risk of herpes zoster among patients with chronic obstructive pulmonary disease: a population-based study. CMAJ. 2011, 183: E275-E280.
Hayashi Y, Senjyu H, Iguchi A, Iwai S, Kanada R, Honda S, et al: Prevalence of depressive symptoms in Japanese male patients with chronic obstructive pulmonary disease. Psychiatry Clin Neurosci. 2011, 65: 82-88.
Chan HN, Yap HL, Kanagasuntheram N, Chan YH: Prevalence of depression and anxiety in hospitalized chronic obstructive pulmonary disease patients and their quality of life: a pilot study. Asia Pac Psychiatry. 2009, 1: 130-137.
National Health Insurance Database: LHID 2000. 2012, http://nhird.nhri.org.tw/date_cohort.htm#2,
Scherrer JF, Virgo KS, Zeringue A, Bucholz KK, Jacob T, Johnson RG, et al: Depression increases risk of incident myocardial infarction among veterans administration patients with rheumatoid arthritis. Gen Hosp Psychiatry. 2009, 31: 353-359.
Liu CY, Hung YT, Chuang YL, Chen YJ, Weng WS, Liu JS, et al: Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manage. 2006, 4: 1-22.
van den Bemt L, Schermer T, Bor H, Smink R, van Weel-Baumgarten E, Lucassen P, et al: The risk for depression comorbidity in patients with COPD. Chest. 2009, 135: 108-114.
Schneider C, Jick SS, Bothner U, Meier CR: COPD and the risk of depression. Chest. 2010, 137: 341-347.
Lou P, Zhu Y, Chen P, Zhang P, Yu J, Zhang N, et al: Prevalence and correlations with depression, anxiety, and other features in outpatients with chronic obstructive pulmonary disease in China: a cross-sectional case control study. BMC Pulm Med. 2012, 12: 53-doi:10.1186/1471-2466-12-53
Mishel MH: Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch. 1990, 22: 256-262.
Barnes PJ: Chronic obstructive pulmonary disease: effects beyond the lungs. PLoS Med. 2010, 7: e1000220-
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al: A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010, 67: 446-457.
Minh HV, Byass P, Chuc NT, Wall S: Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of Vietnam. J Hum Hypertens. 2006, 20: 109-115.
Jang SN, Kawachi I, Chang J, Boo K, Shin HG, Lee H, et al: Marital status, gender, and depression: analysis of the baseline survey of the Korean longitudinal study of ageing (KLoSA). Soc Sci Med. 2009, 69: 1608-1615.
van Manen JG, Bindels P, Dekker F, IJzermans C, van der Zee JS, Schade E, et al: Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002, 57: 412-416.
Akhtar-Danesh N, Landeen J: Relation between depression and sociodemographic factors. Int J Ment Health Syst. 2007, 1: 4-
Lin M, Chen Y, McDowell I: Increased risk of depression in COPD patients with higher education and income. Chron Respir Dis. 2005, 2: 13-19.
Hernberg S: Introduction to occupational epidemiology. 1991, Michigan: Lewis Press
Verdelho A, Hénon H, Lebert F, Pasquier F, Leys D: Depressive symptoms after stroke and relationship with dementia. Neurology. 2004, 62: 905-911.
Celano CM, Freudenreich O, Fernandez-Robles C, Stern TA, Caro MA, Huffman JC: Depressogenic effects of medications: a review. Dialogues Clin Neurosci. 2011, 13: 109-125.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/13/976/prepub
Acknowledgements
The present study was supported in part by the National Sciences Council, Executive Yuan (Grant Number NSC 100-2621-M-039-001), the Buddhist Dalin Tzu Chi Hospital (Grant Number DTCRD101-E-08), the China Medical University Hospital (Grant Number 1MS1), the Department of Health of Taiwan, the Clinical Trial and Research Center for Excellence (Grant Number DOH101-TD-B-111-004), and the Cancer Research Center of Excellence (DOH101-TD-C-111-005).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived and designed the experiments: TYT HL MCL FCS PCC. Performed the experiments: TYT FCS PCC. Analyzed the data: TYT PYT. Wrote the paper: TYT FCS PCC. All authors approved the final version of the manuscript. PCC is the co-corresponding author.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tsai, TY., Livneh, H., Lu, MC. et al. Increased risk and related factors of depression among patients with COPD: a population-based cohort study. BMC Public Health 13, 976 (2013). https://doi.org/10.1186/1471-2458-13-976
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-13-976