Abstract
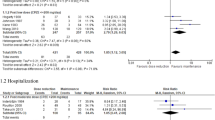
Background
The dogma of a delayed onset of antipsychotic treatment effects has been maintained over the past decades. However, recent studies have challenged this concept. We therefore performed an analysis of the onset of antipsychotic treatment effects in a sample of acutely decompensated patients with schizophrenia.
Methods
In this observational study, 48 inpatients with acutely decompensated schizophrenia were offered antipsychotic treatment with oral risperidone. PANSS-ratings were obtained on day 0, day 1, day 3, day 7 and day 14.
Results
Significant effects of treatment were already present on day 1 and continued throughout the study. The PANSS positive subscore and the PANSS total score improved significantly more than the PANSS negative subscore.
Conclusion
Our results are consistent with the growing number of studies suggesting an early onset of antipsychotic treatment effects. However, non-pharmacological effects of treatment also need to be taken into consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Since their introduction half a century ago, antipsychotics have constituted the backbone of pharmacological treatment of psychosis. In accordance with other groups of psychotropic agents (e.g. antidepressants), a substantial time-lag has been postulated between the initiation of antipsychotic treatment and the onset of the antipsychotic effect. However, this concept of a delayed onset of action has been challenged recently and an earlier onset of antipsychotic treatment effects has been proposed [1, 2].
Our group has recently shown that the atypical antipsychotic risperidone is effective in the treatment of acutely decompensated patients with schizophrenia [3]. In this manuscript we present an analysis of the time-course of treatment effects in acutely decompensated patients with schizophrenia, who remained in treatment.
Methods
A detailed description of the study-design was previously published [3]. In brief, acutely decompensated subjects with schizophrenia were offered treatment with oral risperidone (daily dose 4 – 8 mg given in two doses) upon admission to the secure unit of the Dept. of Psychiatry of the University Medical Center Hamburg-Eppendorf. This unit serves a catchment-area of approximately 250.000 inhabitants of the city of Hamburg, Germany. Benzodiazepines (diazepam 5 – 60 mg/d and lorazepam 0.5 – 10 mg/d) as well as anticholinergics (biperiden 2 – 8 mg/d) were added as clinically indicated. The demographic information of the treatment-group is listed in Table 1.
Subjects were rated with the PANSS and CGI on day 0 (baseline), day 1, day 3, day 7 and day 14. For the PANSS, we analysed the total score as well as the positive, negative and general psychopathology scales. Due to weekends and holidays, four subjects were not rated on day 1. All other ratings were performed as scheduled. For easier comparison, all ratings were expressed as percentage of the baseline-values (day 0 = 100%).
Statistical Analysis
We performed an observed cases analysis for the first two weeks of treatment. Wilcoxon's matched pairs test was used for comparison of symptom-ratings with baseline-ratings. Friedman's two-way analysis of variance was used to assess statistical differences between the different PANSS-subscores for each day.
Results
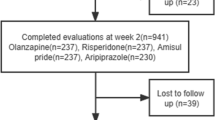
48 subjects participated in this open-label observational study. Subjects were diagnosed with schizophrenia (n = 40), schizoaffective disorder (n = 5) or schizophreniform disorder (n = 3) according to DSM-IV-TR.
Data are available for 43 patients on day 1 (89.6%), 37 patients on day 3 (77.1%), 32 patients on day 7 (66.7%) and 25 patients on day 14 (52.1%). The reasons for discontinuation of risperidone are shown in Table 2.
All PANSS ratings showed a significant improvement with antipsychotic treatment. Table 3 lists the PANSS total scores as well as the different PANSS subscores for each time-point.
On day 1, the PANSS total score as well as the PANSS negative subscale and the PANSS general psychopathology subscale decreased significantly compared to baseline (n = 43; all Z > 2.92; all p < 0.01). The positive symptoms subscale of the PANSS on day 1 showed no significant difference when compared to baseline (n = 43; Z = 1.46; p < 0.15).
On day 3, the positive symptom subscale of the PANSS was significantly lower than the baseline-rating. The PANSS total score as well the PANSS negative subscale and the PANSS general psychopathology subscale also decreased further. All scores were significantly lower than the baseline-scores on day 3 (n = 37; all Z > 3.61; all p < 0.001). On day 7 and day 14, a highly significant decrease in the ratings of total PANSS and all PANSS subscales was observed compared to baseline (all Z > 3.29; all p < 0.001).
Comparing the changes between the subscales of the PANSS, significant differences were found on day 7 (X2 = 23.7; p < 0.001) and day 14 (X2 = 15.1; p < 0.01). While all ratings improved, the decrease in symptom severity was most pronounced on the PANSS positive subscale. In contrast, the ratings on the PANSS negative subscale showed the smallest decrease over time. Further analysis revealed that the decrease in symptom rating was significantly higher on the positive subscale (Z = 3.80; p < 0.001) and the PANSS total score (Z = 2.59; p < 0.01) than on the PANSS negative subscale on day 7. Similar differences were found on day 14 with a significantly stronger improvement in the PANSS positive subscore (Z = 2.62; p < 0.01) and a trend towards significance for the PANSS total score (Z = 1.92; p = 0.05) compared to the PANSS negative subscale.
Discussion
Over the past decades, the concept of a delayed onset of antipsychotic effects on symptoms of acute schizophrenia has been generally accepted. This concept included the understanding that first effects after the initiation of antipsychotic treatment were not seen until after several weeks of treatment.
The dogma of a delayed onset of action has only recently been challenged for antipsychotic treatment [1, 2] as well as for antidepressant treatment [4, 5]. Our data provide additional support for the concept of an early onset of action of antipsychotic treatment in acutely decompensated patients with schizophrenia. Our results suggest that in severely ill subjects who remained in treatment, first effects of treatment can be demonstrated as early as after one day of treatment. Over the course of the next two weeks, symptom ratings for positive, negative and general symptoms of schizophrenia decreased further. While positive symptoms responded even better to antipsychotic treatment, we still saw a significant improvement in negative symptoms during the first two weeks of treatment.
The observational nature of this study without a placebo-group precludes definite statements on the time-course of antipsychotic treatment effects. Still, our data are consistent with previously published studies. Looking at the effects of intramuscular medications, both intramuscular haloperidol and olanzapine led to an improvement in symptoms of schizophrenia within the first 24 hours of treatment [6]. In a large meta-analysis of antipsychotic response, a decrease in psychotic symptom ratings (e.g. PANSS and BPRS) of 13.8% was seen during the first week of treatment. The second week of treatment led to an additional decrease in symptom-ratings of 8.1% [1]. Similar acute treatment effects were seen with the atypical antipsychotic amisulpride with the largest improvement in psychotic symptoms occurring within the first two weeks of treatment [2]. Both studies found a larger symptom reduction during the first two weeks of treatment than during consecutive weeks. An onset of action during the first week of treatment across a broad range of symptoms was also described for the second generation antipsychotic quetiapine [7]. The atypical antipsychotic risperidone has been associated with an earlier onset of action than haloperidol [8], clozapine [9] and zuclopenthixol [10] in the treatment of schizophrenia. While the rate of improvement of symptoms in our study exceeds some of these studies [e.g. [1, 2]], it should be kept in mind that subjects who discontinued treatment were excluded from further analysis.
Potential effects of non-pharmacological interventions should be taken into consideration when assessing the results of this study. We studied a group of patients with schizophrenia who were admitted to a secure unit with acute psychotic decompensation. All subjects were treated with oral risperidone in a daily dose between 4 and 8 mg as well as benzodiazepines as needed. In addition to the pharmacological intervention, all subjects received skilled nursing-care in the setting of an acute treatment ward. Non-pharmacological interventions included a safe, structured and quiet environment, the normalization of food- and fluid-intake as well as adequate opportunity to rest. Concomitant alcohol- and substance-use, which may have contributed to the exacerbation of psychosis, also came to an end with the admission. In addition, precipitating events were addressed during the in-patient treatment. These non-pharmacological factors need to be taken into consideration when assessing the effects of acute treatment. However, in clinical practice, a substantial number of patients with schizophrenia refuse antipsychotic treatment and fail to stabilize despite being placed in a quiet and safe environment. The lack of improvement in patients who refuse antipsychotic treatment points to a specific role of the pharmacological treatment in the stabilization of acutely decompensated patients with schizophrenia.
Conclusion
Our data add to the growing number of studies showing an early onset of antipsychotic effects in subjects with acutely exacerbated schizophrenia. While full benefits of antipsychotic treatment may take several weeks to months, first effects of antipsychotic treatment can be seen as early as after one day of treatment. However, non-pharmacological effects also need to be taken into consideration.
Abbreviations
- BPRS:
-
Brief Psychiatric Rating Scale
- CGI:
-
Clinical Global Impression scale
- PANSS:
-
Positive and Negative Syndrome Scale
References
Agid O, Kapur S, Arenovich T, Zipursky RB: Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003, 60: 1228-1235. 10.1001/archpsyc.60.12.1228.
Leucht S, Busch R, Hamann J, Kissling W, Kane JM: Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry. 2005, 57: 1543-1549. 10.1016/j.biopsych.2005.02.023.
Raedler TJ, Schreiner A, Naber D, Wiedemann K: Risperidone in the treatment of acute schizophrenia. J Clin Psychopharmacol. 2004, 24: 335-338. 10.1097/01.jcp.0000126660.50788.ef.
Rojo JE, Gibert K, Cobo J, Rodriguez-Cano E, Vallejo J: Onset of antidepressant action: a pharmacological question?. Hum Psychopharmacol. 2005, 20: 425-433. 10.1002/hup.708.
Mitchell AJ: Two-week delay in onset of action of antidepressants: new evidence. Br J Psychiatry. 2006, 188: 105-106. 10.1192/bjp.bp.105.011692.
Kapur S, Arenovich T, Agid O, Zipursky R, Lindborg S, Jones B: Evidence for onset of antipsychotic effects within the first 24 hours of treatment. Am J Psychiatry. 2005, 162: 939-946. 10.1176/appi.ajp.162.5.939.
Small JG, Kolar MC, Kellams JJ: Quetiapine in schizophrenia: onset of action within the first week of treatment. Curr Med Res Opin. 2004, 20: 1017-1023. 10.1185/030079904125004033.
Möller HJ, Bäuml J, Ferrero F, Fuger J, Geretsegger C, Kasper S, Kissling W, Schubert H: Risperidone in the treatment of schizophrenia: results of a study of patients from Germany, Austria, and Switzerland. Eur Arch Psychiatry Clin Neurosci. 1997, 247: 291-296.
Bondolfi G, Dufour H, Patris M, May JP, Billeter U, Eap CB, Baumann P: Risperidone versus clozapine in treatment-resistant chronic schizophrenia: a randomized double-blind study. The Risperidone Study Group. Am J Psychiatry. 1998, 155: 499-504.
Huttunen MO, Piepponen T, Rantanen H, Larmo I, Nyholm R, Raitasuo V: Risperidone versus zuclopenthixol in the treatment of acute schizophrenic episodes: a double-blind parallel-group trial. Acta Psychiatr Scand. 1995, 91: 271-277.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/7/4/prepub
Acknowledgements
This study was supported by an unrestricted grant from Janssen Pharmaceuticals.
We thank Dr. Alexander Reiprich, Medical Project Coordination, Janssen-Cilag Germany, for his assistance with the statistical analysis
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Dr. Raedler, Prof. Naber and Prof. Wiedemann have received honoraria, grant-support and/or travel funds from Janssen Pharmaceuticals. Dr. Schreiner is an employee of Janssen-Cilag Germany.
Authors' contributions
TJR conceived of the study, participated in the design and coordination and drafted the manuscript.
AS participated in the design and coordination, helped with the statistical analysis and drafted the manuscript
DN participated in the design and coordination of the study
KW conceived of the study and participated in the design and coordination.
All authors read and approved the final manuscript
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Raedler, T.J., Schreiner, A., Naber, D. et al. Early onset of treatment effects with oral risperidone. BMC Psychiatry 7, 4 (2007). https://doi.org/10.1186/1471-244X-7-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-7-4