Abstract
Background
Since the introduction of antipsychotics, especially the so called atypicals, the treatment of schizophrenia has shown important improvements. At the present time, it is preferred to label clozapine and other antipsychotics sharing similar profiles as second-generation antipsychotics (SGAs). These medications have been proposed by some experts as a first line treatment for schizophrenia.
It is critical to have reliable data about antipsychotic prescription in Mexico and to create management guidelines based on expert meetings and not only on studies carried out by the pharmaceutical industry. Only this approach will help to make the right decisions for the treatment of schizophrenia.
Methods
A translated version of Rabinowitz's survey was used to evaluate antipsychotic prescription preferences and patterns in Mexican psychiatrists.
The survey questionnaire was sent by mail to 200 psychiatrists from public institutions and private practice in Mexico City and Guadalajara, Mexico.
Results
Recommendations for antipsychotics daily doses at different stages of the treatment of schizophrenia varied widely.
Haloperidol was considered as the first choice for the treatment of positive symptoms. On the contrary, risperidone was the first option for negative symptoms. For a patient with a high susceptibility for developing extrapyramidal symptoms (EPS), risperidone was the first choice.
It was also considered that SGAs had advantages over typical antipsychotics in the management of negative symptoms, cognitive impairment and fewer EPS.
Besides, there was a clear tendency for prescribing typical antipsychotics at higher doses than recommended and inadequate doses for the atypical ones.
Conclusions
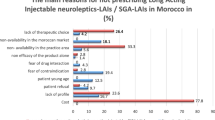
Some of the obstacles for the prescription of SGAs include their high cost, deficient knowledge about their indications and dosage, the perception of their being less efficient for the treatment of positive symptoms and the resistance of some Mexican physicians to change their prescription pattern. It is necessary to reach a consensus, in order to establish and standardize the treatment of schizophrenia, based on the information reported in clinical trials and prevailing economic conditions in Mexico.
Similar content being viewed by others
Background
Since the introduction of antipsychotics, especially the so- called atypicals, the treatment of schizophrenia has shown important improvements. Antipsychotic medications were initially called neuroleptics because of their effect on mobility; nowadays they are known as first-generation antipsychotics (FGAs) [1]. Later on, clozapine, a drug with good antipsychotic profiles but without extrapyramidal side effects, emerged and was called an atypical antipsychotic [2]. Clozapine and other antipsychotics with similar properties are now called second generation antipsychotics (SGAs).
In different treatment guidelines, SGAs have been considered as the first therapeutical option in schizophrenia [3–6], because they have been associated with a lower probability of EPS development, and possibly with a better efficacy over negative symptoms, depression and hostility [7]. These medications have also been found to be associated with less cognitive impairment, even producing improvement in some cases [8].
In Mexico, SGAs have been available for the treatment of psychosis since 1994, when risperidone and clozapine were introduced. Olanzapine and quetiapine were added in 1996 and 1997, respectively; and finally, ziprasidone was introduced in 2001. New SGAs have been added to actual treatment options, being amisulpride one of the most recently introduced. This medication is a dopamine D2/D3 receptor antagonist with similar properties to SGAs [9]. In 2003, the introduction of aripiprazole, a partial dopamine agonist, raised polemic due to its classification, since it has a different mechanism of action. Some clinicians consider it as a third-generation antipsychotic or a pioneer of the so called dopamine-serotonin system stabilizers [10]. Other drugs like amoxapine, which have a lower direct cost, are being evaluated for their use since they have shown similar profiles to SGAs [11].
Pharmaceutical industries spend around 23% to 30% of the actual cost of a drug on its promotion [12]. This is basically directed to advertisements for physicians, trying to convince them to prescribe a particular drug. This strategy has generated better results rather that promoting the drug directly with the patients or their families. On the other hand, psychiatrists (as well as other physicians) update their medical knowledge through information provided by the industry in medical courses, visits at their offices, and briefs of medical articles. Clinical trials sponsored by the pharmaceutical industry represent nowadays a good proportion of the medical literature [13]. It has been estimated that between 89% to 98% of published clinical trials comparing two different medications tend to show positive results (efficacy and safety) of the product from the pharmaceutical house sponsoring the study [14–16]. To counteract this tendency, CATIE, a long-term follow-up study in the US [17], is comparing the use of different SGAs with perfenazine. This study does not involve any pharmaceutical industry and may provide reliable information for a better treatment of schizophrenia.
The previous information underscores the importance of having reliable data regarding antipsychotic prescription in our country and the need to create management guidelines based on expert meetings and not only on studies carried out by the pharmaceutical industry. This will help physicians in making the right decisions for the treatment of schizophrenia.
The aim of this study was to determine the antipsychotic preferences and patterns of prescription for the treatment of schizophrenia among a group of Mexican psychiatrists.
Methods
A survey developed by Rabinowitz et al [18] was translated into Spanish, with permission of the author, and used to evaluate antipsychotic prescription preferences and patterns.
This survey assesses the knowledge regarding the prescription of antipsychotics by inquiring the following aspects: 1) Mean dosage of several antipsychotics at different stages of the treatment of schizophrenia, 2) perception of the advantages of typical and atypical antipsychotics, 3) preferences for the prescription of antipsychotics in different clinical conditions (e.g. predominantly negative symptoms), 4) patterns of prescription for concomitant therapy, and 5) treatment strategies in different clinical situations.
Only those antipsychotics available at the time of the study were included in the survey; drugs such as amisulpride, ziprasidone and aripiprazole were excluded. Only the most frequently used FGAs were included.
The sample comprised 200 psychiatrists from public institutions and private practice in Mexico City and Guadalajara, Mexico. The selected sample represented 10% of these specialized physicians in the country. They were randomly chosen from the Mexican Association of Psychiatry register. Psychiatrists were asked to answer the questionnaire and to return it closed and without identification to preserve confidentiality.
Analysis
Frequencies and percentages were used for descriptive analysis of categorical variables and means and standard deviations (+/-) for continuous variables.
Results
One hundred and forty eight questionnaires were returned, 74% of the total. Within the physicians who returned the questionnaires, mean age was 43.9 +/- 10.6 year old (range 25 to 73 years) and 113 (76.4%) were male. Seventy nine (53.4%) were certified by the Mexican Board of Psychiatry 60 (40.5%) were not, and 9 (6.1%) were residents. About 80% of those inquired worked at a public institution. There were no differences in response rates between psychiatrists from public and private institutions.
Prescription dosages for different stages of schizophrenia treatment given by surveyed psychiatrists are shown in Table 1. The initial and maintenance doses, as well as those prescribed for chronically ill patients were registered over a wide range on the survey. Perceptions about FGAs and SGAs advantages and disadvantages were divided in efficacy, safety and cost-benefit (Table 2). Haloperidol was considered the first choice for the treatment of positive symptoms followed by risperidone. On the other hand, risperidone was reported as a first line drug for the treatment of negative symptoms, while olanzapine was second.
For the treatment of first-psychotic episode, haloperidol was preferred as first choice and olanzapine as the second. For chronic schizophrenia, the most frequently prescribed drug was risperidone followed by olanzapine. For the treatment of psychosis in the elderly, the first choice was risperidone; haloperidol and olanzapine were considered second options. For patients prone to EPS, psychiatrists preferred risperidone as a first option followed by olanzapine. Risperidone was also the first and second choice for the treatment of resistant schizophrenia. Finally, for acute relapse episodes, the first choice was haloperidol and the second was risperidone.
It is a common practice to combine antipsychotic therapy with other drugs. Table 3 shows prescription patterns of these drugs.
The last section of the survey included information obtained by direct questions or clinical vignettes evaluating knowledge about treatment switching strategies, typical daily dosages for particular clinical conditions (e.g. early psychosis, refractory psychosis, etc.), the concept of resistant schizophrenia, recommended treatment duration and the most effective atypical antipsychotic for relapse prevention 'Questionnaire [see Additional file 1]'.
Discussion
Psychiatrists' perception about SGAs
The results of the survey showed that Mexican psychiatrists are aware of the higher efficacy of SGAs on negative symptoms as well as their lower incidence of EPSs, akathisia and tardive dyskinesia. However, they considered these antipsychotics less effective on positive symptoms than FGAs. Half of those surveyed answered that SGAs could reduce the cost of treatment but the main limitation for their use was their high cost. In fact, most psychiatrists would prescribe these drugs to patients if their cost per patient were lower (i.e. less than $50 USD a month).
Antipsychotic prescription patterns
According to the results of the survey, there is a wide knowledge about the indications and dose ranges recommended in the literature for risperidone and olanzapine [19–22]. On the other hand, less than half of the surveyed knew the recommended average doses of clozapine and quetiapine and the trend was to prescribe lower doses than those reported on international studies [23–30]. This may be explained by the fact that risperidone and olanzapine have been available for a longer time and physicians have more information about them. The use of clozapine was found to be limited due to its high direct cost and side effects profile [28].
Two possible explanations can be offered for the wide range of FGA doses reported for the different phases of treatment among particular clinical scenarios. First, the persistence of FGA prescription at higher doses than the recommended on international consensus [3–6] may be related to the belief on "rapid neuroleptization" or impregnation for the management of an aggressive and agitated psychotic patient; and second, the use of low doses of these drugs reflects the preference for prescribing threshold or minimum effective doses. Many studies on the effectiveness of this approach have been published [31–36]. This strategy is based on the finding that clinical response is reached with 65% dopamine D2 receptor occupancy. If this threshold is surpassed by 72% high prolactin levels are reached and if it surpasses 78% the risk of EPS increases [37–41]. In our country some studies support the use of minimum dosages of these medications as a first choice for the treatment of acute and chronic schizophrenia [42–44]. Not controlled, open trials comparing the efficacy of minimum effective doses of haloperidol with SGAs reported similar response rates [45–48].
Another important issue raised by the survey was the duration of the treatment with a given antipsychotic before considering it a treatment failure. A common mistake is to give the antipsychotic for a short time (e.g. two weeks). Current guidelines indicate that one must wait at least 6 weeks for assessing a clinical response; the results of our survey showed that 78% of the physicians do wait this time.
A good consensus on the strategies to change the prescribed antipsychotic due to a lack of response or severe side effects was observed in the survey. These strategies consisted in: a) to start the new antipsychotic and raise the dose to therapeutic levels, while gradually lowering the dose of previous antipsychotic, and b) to instate a washout period before starting the new antipsychotic [49]. Both strategies are recommended and the selection depends on the clinical condition of the patient, the presence of side effects, or the risk of appearance of new adverse events.
Regarding concomitant treatment, it was observed that many physicians had a tendency to prescribe serotonin reuptake inhibitors and benzodiazepines. The antidepressants are frequently prescribed for comorbid depression. Sertraline, a SSRI, has shown efficacy for the treatment of major depression in schizophrenic patients [50, 51]. On the other hand, benzodiazepines are first line drugs for the management of agitation or aggression in psychotic patients [5]. Although the indications for the use of these drugs have been clearly established, it is not possible from our results to infer the reasons the surveyed clinicians had for prescribing these drugs.
Regarding the maintenance phase, a clear and adequate estimation was found with regard to the duration of treatment for a multi-episode patient, but not in the case of a first-episode patient. In this case, the prevailing practice was to maintain the treatment for at least two years; if patients have gone into remission during this period, treatment suspension must be considered [52]. Nevertheless, only 15% to 25% of first-episode patients will not present a relapse during the first 5 years of treatment [53–56]. A 5-year relapse is around 86%, due mainly to treatment abandonment [57].
According to the information collected on refractory schizophrenia, the first treatment choice among surveyed psychiatrists was risperidone; the dosages of different antipsychotics for this type of patients varied widely. Until now, clozapine represents the first treatment choice for a refractory patient and can be administered to a maximum dose of 900 mg/day; this information is not commonly handled by the physicians. Another important issue found in our results was the association of a SGA with a typical one for the treatment of partial response or lack of response. There is no evidence that this strategy increases response. Addition of lithium or valproate has been recommended [3–6].
The limitations of this study were that the survey did not include all FGAs currently available in Mexico nor SGAs more recently introduced; therefore, prescription patterns of other drugs, probably frequently used, were missed. The survey made no difference between depot (long-acting injectable medication) and oral drugs. Also, it did not include differences in treatment between inpatients and outpatients, nor the reasons for prescribing concomitant drugs. Further studies are needed to include these variables and to increase the sample size.
Conclusions
From the results of this survey it can be concluded that Mexican psychiatrists are aware of the advantages of SGAs in the treatment of schizophrenia, although they perceive SGAs as being less efficacious for the treatment of positive symptoms than FGAs. In addition, the high direct cost of SGAs is a limitation for their prescription.
Surveyed psychiatrists exhibited different levels of knowledge on clinical concepts (e.g. refractory schizophrenia) and on prescription guidelines of some SGAs. In addition, it was also found that FGA prescription is still determined by old concepts, such as "rapid neuroleptization" and that there is resistance in some Mexican physicians for changing their pattern of prescription. Similar difficulties have been encountered in other cities of Europe and developing countries.
It is necessary to reach a consensus to establish and standardize the treatment of schizophrenia, based on the information reported in clinical trials and on the economic conditions of the country to avoid inadequate treatments as those observed in the present study.
References
Deniker P: Psychopharmacology and biologic psychiatry. Historical review. Soins Psychiatrie. 1983, 37: 5-6.
Hippius H: A historical perspective of clozapine. Journal of Clinical Psychiatry. 1999, 60: 22-23.
Treatment of schizophrenia. The Expert Consensus Panel for Schizophrenia. J Clin Psychiatry. 1996, 57 (Suppl 12B): 3-58.
Canadian clinical practice guidelines for the treatment of schizophrenia. The Canadian Psychiatric Association. Can J Psychiatry. 1998, 43 (Suppl 2): 25S-40S.
Treatment of Schizophrenia 1999. The Expert Consensus Guideline Series. J Clin Psychiatry. 1999, 60 (Suppl 11): 3-80.
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, Kreyenbuhl J: Practice guideline for the treatment of patients with schizophrenia, second edition. American Journal of Psychiatry. 2004, 161: 1-56. 10.1176/appi.ajp.161.1.1.
Stip E: Novel antipsychotics: issues and controversies. Typicality of atypical antipsychotics. Journal of Psychiatry & Neuroscience. 2000, 25: 137-153.
Keefe RS, Silva SG, Perkins DO, Lieberman JA: The effects of atypical antipsychotics drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophrenia Bulletin. 1999, 25: 201-222.
Schoemaker H, Claustre Y, Fage D, Rouquier L, Chergui K, Curet O, Oblin A, Gonon F, Carter C, Benavides J, Scatton B: Neurochemical characteristics of amisulpride, an atypical dopamine D2/D3 receptor antagonist with both presynaptic and limbic selectivity. The Journal of Pharmacology and Experimental Therapeutics. 1997, 280: 83-97.
Stahl SM: Dopamine system stabilizers, aripiprazole, and the next generation of antipsychotics, part 1, "Goldilocks" actions at dopamine receptors. Journal of Clinical Psychiatry. 2001, 62: 841-842.
Apiquian R, Ulloa RE, Fresán A, Loyzaga C, Nicolini H, Kapur S: Amoxapine shows atypical antipsychotic effects in patients with schizophrenia: results from a prospective open-label study. Schizophrenia Research. 2003, 59: 35-39. 10.1016/S0920-9964(01)00342-5.
Josefson D: Marketing of antipsychotic drugs attacked. BMJ. 1998, 316: 648-
Angell M: Is academic medicine for sale?. New England Journal of Medicine. 2000, 342: 1516-1518. 10.1056/NEJM200005183422009.
Cho MK, Bero LA: The quality of drug studies in symposium proceedings. Annals of Internal Medicine. 1996, 124: 485-489.
Mandelkern M: Manufacturer support and outcome. Journal of Clinical Psychiatry. 1999, 60: 122-
Safer DJ: Design and reporting modifications in industry-sponsored comparartive psychopharmacology trials. Journal of Nervous and Mental Disease. 2002, 190: 583-592. 10.1097/00005053-200209000-00002.
Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM, McGee MF, Simpson GM, Stevens MC, Lieberman JA: The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophrenia Bulletin. 2003, 29: 15-31.
Rabinowitz J, Lichtenberg P, Kaplan Z: Comparison of cost, dosage and clinical preference for risperidone and olanzapine. Schizophrenia Research. 2000, 46: 91-96. 10.1016/S0920-9964(00)00036-0.
Beasley C.M. Jr., Tollefson G, Tran P, Satterlee W, Sanger T, Hamilton S: Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology. 1996, 14: 111-123. 10.1016/0893-133X(95)00069-P.
Tran PV, Dellva MA, Tollefson GD, Wentley AL, Beasley C.M. Jr.: Oral olanzapine versus oral haloperidol in the maintenance treatment of schizophrenia and related psychoses. British Journal of Psychiatry. 1998, 172: 499-505.
Kopala LC: Clinical experience in developing treatment regimens with novel antipsychotic risperidone. International Clinical Psychopharmacology. 1997, 12: S11-S18.
Marder SR, Davis JM, Chouinard G: The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. Journal of Clinical Psychiatry. 1997, 58: 538-546.
Arvanitis LA, Miller BG, Group. Seroquel Trial 13 Study: Multiple fixed doses of "Seroquel" (Quetiapine) in patients with acute exacerbation of schizophrenia: A comparison with haloperidol and placebo. Biological Psychiatry. 1997, 42: 233-246. 10.1016/S0006-3223(97)00190-X.
Buchanan RW, Breier A, Kirkpatrick B, Ball P, Carpenter WT Jr.: Positive and negative symptom response to clozapine in schizophrenic patients with and without the deficit syndrome. American Journal of Psychiatry. 1998, 155: 751-760.
Copolov David L., Link CGG, Kowalcyk B: A multicentre, double-blind, randomized comparison of quetiapine (ICI 204,636, "Seroquel') and haloperidol in schizophrenia. Psychological Medicine. 2000, 30: 95-105. 10.1017/S0033291799001476.
Emsley RA, Raniwalla J, Bailey PJ, Jones AM: A comparison of the effects of quetiapine ('seroquel') and haloperidol in schizophrenic patients with a history of and a demonstrated, partial response to conventional antipsychotic treatment. PRIZE Study Group. International Clinical Psychopharmacology. 2000, 15: 121-131.
Fleischhacker WW: Clozapine: A comparison with other novel antipsychotics. Journal of Clinical Psychiatry. 1999, 60: 30-34.
Wahlbeck K, Cheine M, Essali A, Adams C: Evidence of clozapine's effectiveness in schizophrenia: A systematic review and meta-analysis of randomized trials. American Journal of Psychiatry. 1999, 156: 990-999.
Kane JM, Marder SR, Schooler NR, Wirshing WC, Umbricht D, Baker RW, Wirshing DA, Safferman A, Ganguli R, McMeniman M, Borenstein M: Clozapine and haloperidol in moderately refractory schizophrenia: a 6-month randomized and double-blind comparison. Archives of General Psychiatry. 2001, 58: 965-972. 10.1001/archpsyc.58.10.965.
Small JG, Hirsch SR,, Arvanitis LA, Miller BG, Link CGG: Quetiapine in patients with schizophrenia. A high- and low-dose double-blind comparison with placebo. Seroquel Study Group. Archives of General Psychiatry. 1997, 54: 549-557.
Baldessarini RJ, Cohen BM, Teicher M: Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Archives of General Psychiatry. 1988, 45: 79-91.
McEvoy JP, Hogarty GE, Steingard S: Optimal dose of neuroleptic in acute schizophrenia. A controlled study of the neuroleptic threshold and higher haloperidol dose. Archives of General Psychiatry. 1991, 48: 739-745.
Oosthuizen P, Emsley RA, Turner J, Keyter N: Determining the optimal dose of haloperidol in first-episode psychosis. Journal of Psychopharmacology. 2001, 15: 251-255.
Stone CK, Garver DL, Griffith J, Hirschowitz J, Bennett J: Further evidence of a dose-response threshold for haloperidol in psychosis. American Journal of Psychiatry. 1995, 152: 1210-1212.
Van Putten T, Marder SR, Mintz JA: A controlled dose comparison of haloperidol in newly admitted schizophrenic patients. Archives of General Psychiatry. 1990, 47: 754-758.
Zhang-Wong J, Zipursky RB, Beiser M, Bean G: Optimal haloperidol dosage in first-episode psychosis. Can J Psychiatry. 1999, 44: 164-167.
Daskalakis Z, Christensen B, Zipursky RB, Zhang-Wong J, Beiser M: Relationship between D2 occupancy and prolactin levels in first episode psychosis. Biological Psychiatry. 1998, 43: 113S-10.1016/S0006-3223(98)90824-1.
Farde L, Nordstrom AL, Wiesel FA, Pauli S, Haldin C, Sedval G: Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine:Relation to extrapyramidal side effects. Archives of General Psychiatry. 1992, 49: 538-544.
Kapur S, Zipursky RB, Jones C, Remington G, Houle S: Relationship between dopamine D2 occupancy, clinical response, and side effects: A double-blind PET study of first-episode schizophrenia. Amerian Journal of Psychiatry. 2000, 157: 514-520. 10.1176/appi.ajp.157.4.514.
Nordstrom AL, Farde L, Wiesel FA, Forslund K, Pauli S, Halldin C, Uppfeldt G: Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects: a double-blind PET study of schizophrenic patients. Biological Psychiatry. 1993, 33: 227-235. 10.1016/0006-3223(93)90288-O.
Schlegel S, Schlosser R, Hiemke C, Nickel O, Bockisch A, Hahn K: Prolactin plasma levels and D2 dopamine receptor occupancy measured with IBZM-SPECT. Psychopharmacology (Berl). 1996, 124: 285-287.
Ortega-Soto HA, Páez F,, Fernández A, Pinedo H, Hernández C: El efecto terapéutico de las dosis umbrales de haloperidol: resultados preliminares de un estudio piloto. Anales del Instituto Mexicano de Psiquiatría. 1991, 30-34.
Ortega-Soto HA, Brunner E, Apiquian R, De la Torre MP, Pinedo H, Chávez JL, Moreno J, Páez F: Efecto terapéutico de las dosis umbrales de antipsicóticos. VIII Reunión de Investigación IMP. 1993, Mexico City, Mexico, 4:
Ortega-Soto HA, Brunner E, Apiquian R, Ulloa RE, De la Torre MP: Typical antipsychotics: the threshold doses strategy. XXth CINP Congress Collegium Internationale Neuro-Psychopharmacologicum. 1996, Melbourne, Australia
Kopala Lili C., Good Kimberley P., Fredrikson Diane, Whitehorn David, Lazier Lorraine, Honer William G.: Risperidone in first-episode schizophrenia: Improvement in symptoms and pre-existing extrapyramidal signs. International Journal of Psychiatry in Clinical Practice. 1998, 2: S19-S26.
Keshavan MS, Schooler NR, Sweeney JA, Haas GL, Pettegrew JW: Research and treatment strategies in first-episode psychoses: The Pittsburgh experience. Br J Psychiatry. 1998, 172 (Suppl): 60-65.
Apiquian R, Fresán A, Herrera K, Loyzaga C, García-Anaya M, Ulloa RE, García-Marín J, Gutierrez D, Nicolini H: Estudio comparativo de dosis mínimas de haloperidol vs olanzapina en el primer episodio psicótico. Psiquiatría y Salud Integral. 2003, 3: 56-65.
Apiquian R, Fresán A, Herrera K, Ulloa RE, Loyzaga C, Gutiérrez D, Nicolini H: Minimum effective doses of haloperidol for the treatment of first psychotic episode: a comparative study with risperidone and olanzapine. International Journal of Neuropsychopharmacology. 2003, 6: 1-6. 10.1017/S1461145702003188.
Lee CT, Conde BJ, Mazlan M, Visanuyothin T, Wang A, Wong MM, Walker DJ, Roychowdhury SM, Wang H, Tran PV: Switching to olanzapine from previous antipsychotics: a regional collaborative multicenter trial assessing 2 switching techniques in Asia Pacific. Journal of Clinical Psychiatry. 2002, 63: 569-576.
Addington D, Addington J, Patten S, Remington G, Moamai J, Labelle A, Beauclair L: Double-blind, placebo-controlled comparison of the efficacy of sertraline as treatment for a major depressive episode in patients with remitted schizophrenia. Journal of Clinical Psychopharmacology. 2002, 22: 20-25. 10.1097/00004714-200202000-00004.
Mulholland C, Lynch G, King DJ, Cooper SJ: A double-blind, placebo-controlled trial of sertraline for depressive symptoms in patients with stable, chronic schizophrenia. Journal of Psychopharmacology. 2003, 17: 107-112. 10.1177/0269881103017001713.
Gitlin M, Nuechterlein K, Subotnik KL, Ventura J, Mintz J, Fogelson DL, Bartzokis G, Aravagiri M: Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia. American Journal of Psychiatry. 2001, 158: 1835-1842. 10.1176/appi.ajp.158.11.1835.
Johnstone EC, Crow TJ, Frith CD, Owens DGC, Done JD, Baldwin EJ, Charlette A: The Northwick Park functional psychosis study: diagnosis and outcome. Psychological Medicine. 1992, 22: 331-346.
Linszen D, Dingemans P, Lenior M: Early intervention and a five year follow up in young adults with short duration of untreated psychosis:ethical implications. Schizophrenia Research. 2001, 51: 55-61. 10.1016/S0920-9964(01)00239-0.
Vazquez-Barquero JL, Cuesta MJ, Herrera Castanedo S, Lastra I, Herran A, Dunn G: Cantabria First-Episode Schizophrenia Study: Three-year follow-up. Br J Psychiatry. 1999, 174: 141-149.
Fresán A, Apiquian R, Loyzaga C, García-Anaya M, Ulloa RE, Nicolini H: Functional recovery in first-episode psychosis. Psiquiatría y Salud Integral. 2002, 2: 40-44.
Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, Koreen A, Sheitman B, Chakos M, Mayerhoff D, Lieberman JA: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of General Psychiatry. 1999, 56: 241-247. 10.1001/archpsyc.56.3.241.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/4/12/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
RA, REU and CdlF drafted the manuscript. AF performed the statistical analysis. RA and HN participated in the study design and coordination. All authors read and approved the final manuscript.
Electronic supplementary material
12888_2003_51_MOESM1_ESM.doc
Additional File 1: Questionnaire for different clinical scenarios. The contents of Rabinowitz Survey regarding antipsychotic prescription patterns including the answers of the surveyed psychiatrist. (DOC 34 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Apiquian, R., Fresán, A., de la Fuente-Sandoval, C. et al. Survey on schizophrenia treatment in Mexico: perception and antipsychotic prescription patterns. BMC Psychiatry 4, 12 (2004). https://doi.org/10.1186/1471-244X-4-12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-4-12