Abstract
Background
Prefrontal repetitive transcranial magnetic stimulation (rTMS) has been used to induce side-specific mood changes in volunteers and patients. To clarify inconsistencies between reports that used different stimulation frequencies, we conducted a controlled study with a low (1 Hz) frequency, comparing left with right-sided stimulation
Methods
Nineteen healthy volunteers received randomised left or right prefrontal rTMS at a frequency of 1 Hz and 100% of motor threshold in two sessions two weeks apart.
Results
There were significant improvements with TMS for performance in the digit symbol substitution and verbal fluency tests, but no change of mood on a number of measures. There was also a reduction of pulse rate after TMS. The only side-specific TMS-effect was on mean arterial pressure, which decreased pressure after left, but not after right prefrontal TMS.
Conclusions
Apart from the unexpected and so far unreplicated effect on mean arterial pressure, there were no side-specific effects on mood in volunteers. It is unlikely that a simple laterality model of mood together with the assumed activating effect of higher and 'quenching' effect of lower stimulation frequency can account for the effects of TMS on mood.
Similar content being viewed by others
Background
Transcranial Magnetic Stimulation (TMS) has been used as an investigative tool since the early eighties to map motor and sensory cortical functions and to establish the integrity of cortico-spinal pathways and central nerve conduction times. During language localisation studies, researchers noted that subjects experienced mood changes during TMS over dominant frontal regions. In particular, stimulation of the left (dominant) frontal cortex resulted in subjects reporting feelings of frustration, sadness and even spontaneous weeping. The finding that TMS had an influence on affect in healthy volunteers has led to the notion that TMS may also be a useful clinical tool in the treatment of depressive illness. Stimulation at different frequencies may have differential effects on the brain, which may explain the reverse laterality observed in patient and volunteers studies. Previous studies of healthy volunteers at 5, 10 and 20 Hz have shown mood-lowering effect of left and mood-lifting effect of right prefrontal stimulation [1–3] while other studies at 10 and 20 Hz [4–6] have found no effect. In an attempt to further analyse the role of stimulation frequency and laterality in healthy controls we conducted a healthy volunteer study using stimulation at 1 Hz over left and right prefrontal cortex.
Methods
Subjects
We recruited twenty-five healthy volunteers to take part in this study; nineteen (10 female) completed the protocol. Subjects were students from Edinburgh and Napier Universities and staff from the Royal Edinburgh Hospital. They were aged between 19 and 38 years (mean ± SD = 24.6 ± 5.3 years). Mean NART-estimated IQ was 112.7 (SD = 6.2) [7]. All subjects met our local safety criteria for TMS in normal volunteers and were right handed. All female participants were required to have a negative pregnancy test on the study day. Subjects were asked before the study if they had any pre-conceived ideas about what type of mood might be induced when either the left or right side of the brain was stimulated. None reported any expectations, and the investigators were careful not to induce any. All volunteers received information sheets outlining the study at least twenty-four hours before giving written informed consent, and were paid £25 expenses for completing both test sessions. The study was approved by the local ethics of research subcommittee.
Experimental design
Subjects were studied in two sessions separated by seven days. Individual subjects were tested at the same time of day on both occasions. All participants received TMS between midday and 3 pm. On arrival at the laboratory, subjects were given the opportunity to discuss the protocol and ask any questions. At the start of each session, a psychiatrist interviewed participants to check for signs of a possible mood disorder. All but one (who scored 1) had Hamilton Depression Scores of 0 [8]. Subjects also completed the Beck Depression Inventory (BDI) [9], none scoring higher than 6. Mean scores were 0.5 and 0.3 on the left and right stimulation days, respectively. All subjects were right-handed on the Annett Handedness Scale (mean +/- sd = 20.7 +/- 2.3) [10].
Short-term changes in affect were measured with the Positive and Negative Affect Schedule (PANAS) [11] the Profile of Mood States (POMS) [12], the UWIST Adjective Checklist [13], the SAI (measure of stress and arousal) [14] and the Befindlichkeitsskala (BFS) adjective checklist [15]. To gauge any changes in cognitive performance, subjects were asked to complete the Digit Symbol Substitution (DSS) [16] and a Verbal Fluency Task (FAS) [17]. These same tasks were then repeated immediately after the TMS procedure. Parallel versions of the DSS, BFS and FAS were used and the order of presentation was counterbalanced between subjects.
Subjects were pseudo-randomly allocated to either receiving stimulation to their left dorsolateral prefrontal cortex (LDLPFC) on their first visit and right dorsolateral prefrontal cortex (RDLPFC) on their second or vice versa. In addition to the ECG recordings, blood pressure and pulse were recorded immediately before and after the TMS procedure.
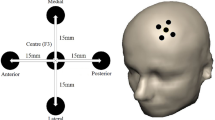
Transcranial magnetic stimulation procedure
Subjects were seated comfortably with both forearms supported horizontally by pillows. They were instructed to keep their hands still but as relaxed as possible. An appropriate sized Lycra cap was placed on the subjects' head to enable marking of the TMS coil position. For each individual, the site of prefrontal stimulation was determined from the location of the motor cortex. Motor evoked potentials (MEPs) were recorded from the abductor pollicis brevis (APB) muscle from the contra-lateral hand. Talairach atlas co-ordinates [18] were used to estimate the optimum stimulation site for this study, which for right or left prefrontal cortex is 5 cm anterior in the midline of the APB site. Electrodes located at the contra-lateral APB muscle detected MEP signals via a bioamplifier, which were recorded using the MacLab TM (AD Instruments Ltd, UK) 'Scope' software for Apple Macintosh. We used a 70 mm figure-of-eight coil connected to a Dantec stimulator (Dantec Electronics Limited, Bristol). The coil was systematically displaced (mapping) over the primary motor cortex, until the largest consistent MEP response from the APB was recorded. Motor threshold (Tm) was then determined. This was defined as the minimum stimulus intensity to produce a MEP response of at least 50 microvolts, from a minimum of five out often consecutive stimuli. Subjects then received a total of 1,000 stimuli at a frequency of 1 Hz at their own individual threshold Tm over the left or right DLPFC. The stimulation was administered in 60-second blocks with 15-second breaks in between. During this 'mood induction' stage the experimenters and subject remained silent to ensure the same conditions for each subject and for each visit. For a few subjects who had relatively high thresholds, the temperature of the coil exceeded 35 degrees and so there was a short (1–2 minute) interruption to the protocol while the coil was replaced.
Results
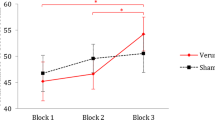
As subjects were balanced for order of starting with right (or left) sided stimulation, there was no significant "side"-effect for any of the measures. There were a number of "TMS"-effects that were independent of stimulation side: both digit symbol substitution and verbal fluency were performed better after TMS, pulse rate was reduced, and POMS depression and PANAS negative affect scores were marginally lower. Only one measure actually showed selective effects ("side-by-TMS" interaction). This was mean arterial pressure, which was reduced after left, but not after right-sided stimulation.
Discussion
Using 1 Hz prefrontal stimulation, we were the second group not able to induce either low or improved mood in a side-specific fashion [19]. A failure to demonstrate lateralised effects on mood has been described in three further healthy volunteer studies [4–6]. This is in direct contrast to the studies by George et al [2], Pascual-Leone et al [3] and Dearing et al [1], which showed left prefrontal rTMS to induce a transient decrease in self-rated happiness and an increase in sadness compared with the effects of right prefrontal cortical rTMS. The differences in design are considered below as possible explanations for the studies' contrary findings.
The sample size was small in each of the studies which found lateralised effects [1–3] with only 10, 10 and 9 subjects respectively, while the studies by our group (N = 19), Nedjat [5] (N = 50), and Mosimann [4] (N = 25) used larger numbers and failed to elicit such an effect.
The number or intensity of stimuli applied could have been too small. We used 1000 stimuli per session, which compares to 500 stimuli in George's [2] and Pascual-Leone's [3] studies, 800–1000 in Cohrs' [6], Dearing's [1] and Nedjat's [5] and 1600 in Mosimann's [4]. We stimulated at 100% motor threshold as did Mosimann et al [4], compared to 120% used by the George [2] and Cohrs [6] groups, 110% in the Pascual-Leone study [3], while Dearing [1] and Nedjat [5] stimulated at 80% Tm. Cortical stimulation studies have demonstrated that the after discharge threshold of the motor cortex is lower than that of the prefrontal cortex [20]. Therefore it may be that the intensity applied in several studies was insufficient to elicit threshold response. Although on the face of it, both number and intensity of TMS in our study was adequate [19], the dose response relationship at 1 Hz may be flatter and require a larger number of stimuli or increased intensity to achieve its effects.
Assessment of mood was slightly different in the various studies. All the other studies used visual analogue scales, and only George [2] also used the PANAS and the NIMH mood scales. We employed a larger battery of validated self-rating scales, previously employed in controls and patients. George found the visual analogue scales not sensitive to mood change, but he got positive results with the self-rating scales. We did not use visual analogue scales for this reason and because comparison data are mainly available for standardised scales. Pascual-Leone comments that his subjects did not experience a clinically detectable mood change, although their analogue scale ratings differed [3]. It is possible, in spite of George's results, that scales designed to detect mood change do not usually capture the discrete changes caused by rTMS.
Finally, the scheduling of stimulation sessions was different between the studies: Pascual-Leone [3] stimulated six times in 3.5 hours, George five times in the same number of days [2], whereas we stimulated on two different days, separated by a full week. The negative Mosimann study [4] was designed with a delay of 2–3 days between the 2 stimulation sessions. It is conceivable that the noise of baseline fluctuation across this longer period drowned out possible minor fluctuations due to rTMS. On the other hand, study designs that permit stimulating more than one site per day may attribute effects to a given site due to carry over effects [3]. The main difference between the studies, however, is in their stimulation frequency. The frequency of rTMS is thought to determine the brain response: high frequencies are said to enhance, low frequencies to quench brain excitability [21]. Stimulation near 1 Hz has been demonstrated to have an inhibiting effect on brain excitability [22]. This could explain some but not all of the contradictory results found between studies of healthy volunteers and depressed patients who show worse and improved mood, respectively, with left prefrontal stimulation. Based on the assumption that high stimulation frequencies stimulate, low frequencies quench brain activity, Klein et al. [23] predicted and found antidepressant activity after right prefrontal stimulation at 1 Hz in depressed patients, while both 20 and 10 Hz had been shown to be antidepressant after left prefrontal stimulation only [24, 25]. Presence of an antidepressant effect at this frequency with an absence of effects in healthy volunteers may suggest a specific antidepressant rather than a non-specific activating effect. Why rTMS at 10 Hz should be deactivating in controls [3], but in patients implicitly activating [25], as exemplified in the two Pascual-Leone studies, is unclear.
Differential responses in the two groups due either to the illness or its treatment, e.g. medication, may be responsible. It is further unclear why Dearing [1] should have found an effect in healthy volunteers identical to the lower frequency studies of George (5 Hz) [2] and Pascual-Leone (10 Hz) [3] with the significantly higher frequency of 20 Hz. George has argued that after an initial increase, there is a rebound decrease in excitability after these putatively excitatory frequencies in the healthy volunteers which explains the reduction in mood [26]. It is not immediately clear, however, why this should not be the case in depressed patients. There is, finally, an outside chance that, although aiming for a frequency with a net inhibitory effect, we may have selected a frequency where stimulating and inhibitory effects were at a balance. This would explain the absence of an effect on mood.
The divergence of experimental findings between the various studies suggests that further work is needed to confirm an effect on mood of rTMS over DLPFC in healthy controls. Future studies should employ larger sample sizes and validated measures of mood. Stimulation intensity must be adequate and studies using crossover design must exclude interaction effects by incorporating adequate intervals between stimulation sessions.
The outcome measures in the neuropsychology domain are reassuring, in that no deterioration of function after TMS was observed [27]. The autonomic measures, particularly the mean arterial pressure, are of interest, but the side-specific effect on arterial pressure requires replication. Effects on pulse rate and blood pressure have been reported after meditation, relaxation and bio-feedback. A possible association between lateralised brain (de-) activation and autonomic changes deserves further enquiry.
References
Dearing J, George MS, Greenberg BD, Wasserman EM, Schlaepfer TE, Murphy DL: Mood effects of prefrontal repetitive high frequency transcranial magnetic stimulation (rTMS) in healthy volunteers. CNS Spectrums. 1997, 2: 53-68.
George MS, Wassermann EM, Williams WA, Steppel J, Pascual-Leone A, Basser P, et al: Changes in mood and hormone levels after rapid-rate transcranial magnetic stimulation (rTMS) of the prefrontal cortex. Journal of Neuroscience. 1996, 8: 172-180.
Pascual-Leone A, Catalá MD, Pascual-Leone Pascual A: Lateralized effect of rapid-rate transcranial magnetic stimulation of the prefrontal cortex on mood. Neurology. 1996, 46: 499-502.
Mosimann UP, Rihs TA, Engeler J, Fisch H, Schlaepfer TE: Mood effects of repetitive transcranial magnetic stimulation of left prefrontal cortex in healthy volunteers. Psychiatry Research. 2000, 94: 251-256. 10.1016/S0165-1781(00)00146-3.
Nedjat N, Folkerts HW, Michael ND, Arolt V: Evaluation of the side effects after rapid-rate transcranial magnetic stimulation over the left prefrontal cortex in normal volunteers. Clinical Neurophysiology. 1998, 107: 96-
Cohrs S, Tergau F, Riech S, Kastner S, Paulus W, Ziemann U, et al: High-frequency repetitive transcranial magnetic stimulation delays rapid eye movement sleep. Neuroreport. 1998, 9: 3439-43.
Nelson HE, Willison JR: The revised National Adult Reading Test-Test Manual. NFER-Nelson;. 1991
Hamilton M: Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967, 6: 278-296.
Beck AT, Ward CH, Mendelson M, Mock JE, Erbaugh JK: An inventory for measuring depression. Archives of General Psychiatry. 1961, 4: 561-571.
Briggs GG, Nebes RD: Patterns of hand preference in a student population. Cortex. 1975, 11: 230-238.
Watson D, Clark LA, Tellegen A: Development and validation of brief measures of positive and negative affect: the PANAS Scales. Journal of Personality and Social Psychology. 1988, 54: 1063-1070. 10.1037//0022-3514.54.6.1063.
McNair DM, Lorr M, Droppleman LF: Edits Manual for the Profile of Mood States. San Diego: Edits Educational and Industrial Testing Service;. 1992
Mathews G, Jones DM, Chamberlain AG: Refining the measurement of mood: the UWIST Mood Adjective Checklist. British Journal of Psychology. 1990, 81: 17-42.
MacKay C, Cox T, Burrows G, Lazzerini T: An inventory for the measurement of self-reported stress and arousal. British Journal of Social and Clinical Psychology. 1978, 17: 283-284.
von Zerssen D, Strian F, Schwarz D: Evaluation of depressive states, especially in longitudinal studies. In Psychological Measurements in Psychological Measurements in Psychopharmacology. Edited by: Pichot P. 1974, Paris: Karger, 189-202.
Wechsler D: Wechsler Adult Intelligence Scale – Revised. New York: Psychological Corporation;. 1981
Borkowski JG, Benton AL, Spreen O: Word fluency and brain damage. Neuropsychologia. 1967, 5: 135-140. 10.1016/0028-3932(67)90015-2.
Talairach J, Tournoux P: A coplanar stereotaxic atlas of a human brain. Stuttgart: Thieme;. 1988
Grisaru N, Bruno R, Pridmore S: Effects on the emotions of healthy individuals of slow repetitive transcranial magnetic stimulation applied to the prefrontal cortex. Journal of ECT. 2001, 17: 184-189. 10.1097/00124509-200109000-00007.
Penfield W, Jasper H: Epilepsy and the functional anatomy of the human brain. Boston: Brown & Co;. 1954
Weiss SRB, Li X-L, Rosen JB, Li H, al e: Quenching: inhibition of development and expression of amygdala kindled seizures with low frequency stimulation. NeuroReport. 1995, 4: 2171-2176.
Chen R, Classen J, Gerloff C, Celnik P, Wassermann EM, Hallett M, et al: Depression of motor cortex excitability by low-frequency transcranial magnetic stimulation. Neurology. 1997, 48: 1398-403.
Klein E, Kreinin I, Chistyakov A, Koren D, Mecz L, Marmur S, et al: Therapeutic efficacy of right prefrontal slow repetitive transcranial magnetic stimulation in major depression: a double-blind controlled study. Archives Of General Psychiatry. 1999, 56: 315-20. 10.1001/archpsyc.56.4.315.
George MS, Wassermann EM, Kimbrell TA, Little JT, Williams WE, Danielson AL, et al: Mood improvement following daily left prefrontal repetitive transcranial magnetic stimulation in patients with depression: a placebo-controlled crossover trial. American Journal Of Psychiatry. 1997, 154: 1752-6.
Pascual-Leone A, Rubio B, Pallardó F, Catalá MD: Rapid-rate transcranial magnetic stimulation of left dorsolateral prefrontal cortex in drug-resistant depression [see comments]. Lancet. 1996, 348: 233-7. 10.1016/S0140-6736(96)01219-6.
George MS, Nahas Z, Speer AM, Kimbrell TA, Wassermann EM, Lawandales CC, et al: Transcranial Magnetic Stimulation (TMS) – A new method for investigating the neuroanatomy of depression. In Biological Psychiatry: New Models for Depression. Edited by: Ebert D, Ebmeier KP. 1998, Basel: Karger
Grafman J, Wassermann E: Transcranial magnetic stimulation can measure and modulate learning and memory. Neuropsychologia. 1999, 37: 159-167. 10.1016/S0028-3932(98)00090-6.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/2/1/prepub
Acknowledgements
The Medical Research Council for funding, Carol A. Swanson for technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interests
One year free loan of Dantec Stimulator (Dantec Electronics Limited, Bristol)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jenkins, J., Shajahan, P.M., Lappin, J.M. et al. Right and left prefrontal transcranial magnetic stimulation at 1 Hz does not affect mood in healthy volunteers. BMC Psychiatry 2, 1 (2002). https://doi.org/10.1186/1471-244X-2-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-2-1