Abstract
Background
Multiple relapses characterise the course of illness in most patients with schizophrenia, yet the nature of these episodes has not been extensively researched and clinicians may not always be aware of important implications.
Methods
We critically review selected literature regarding the nature and underlying neurobiology of relapse.
Results
Relapse rates are very high when treatment is discontinued, even after a single psychotic episode; a longer treatment period prior to discontinuation does not reduce the risk of relapse; many patients relapse soon after treatment reduction and discontinuation; transition from remission to relapse may be abrupt and with few or no early warning signs; once illness recurrence occurs symptoms rapidly return to levels similar to the initial psychotic episode; while most patients respond promptly to re-introduction of antipsychotic treatment after relapse, the response time is variable and notably, treatment failure appears to emerge in about 1 in 6 patients. These observations are consistent with contemporary thinking on the dopamine hypothesis, including the aberrant salience hypothesis.
Conclusions
Given the difficulties in identifying those at risk of relapse, the ineffectiveness of rescue medications in preventing full-blown psychotic recurrence and the potentially serious consequences, adherence and other factors predisposing to relapse should be a major focus of attention in managing schizophrenia. The place of antipsychotic treatment discontinuation in clinical practice and in placebo-controlled clinical trials needs to be carefully reconsidered.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic and disabling illness, with the majority of patients experiencing multiple relapses during the course of the illness [1]. Relapse, characterised by acute psychotic exacerbation, may have serious implications. For example, there is a risk of patients harming themselves or others, of jeopardising personal relationships, education or employment status [2], and of further stigmatisation of the illness. Additionally, relapse may carry a biological risk. It has been proposed that active psychosis reflects a period of disease progression insofar as patients may not return to their previous level of function and treatment refractoriness may emerge [3, 4]. Multiple factors contribute to increasing the risk of relapse. In a systematic review and meta-analysis of longitudinal studies it was found that non-adherence with medication, persistent substance use, carers' criticism and poorer premorbid adjustment significantly increased the risk for relapse in first-episode psychosis [5]. In a prospective, 5 yr follow-up of first-episode psychosis patients it was found that the most common risk factor by far was antipsychotic medication discontinuation [1]. In clinical settings disengagement from treatment is common, even and perhaps particularly, in the early stages of illness [6–9]. In recognition of the associated risks, improving medication adherence and relapse prevention have been emphasised as key components of the management of schizophrenia [2]. However, there remain many unanswered questions regarding the nature of relapse making further study of this component of the illness imperative. During recent studies of relapse in schizophrenia that we conducted [10–12], we were struck by several observations:
-
1.
Relapse rates are very high after treatment discontinuation, even after a single episode of psychosis.
-
2.
A longer treatment period prior to discontinuation does not reduce the risk of relapse.
-
3.
Many patients relapse very soon after treatment discontinuation.
-
4.
The transition from remission to relapse may be abrupt, with few early warning signs.
-
5.
Once illness recurrence occurs symptom severity rapidly returns to levels similar to the initial psychotic episode.
-
6.
While most patients respond promptly to re-introduction of antipsychotic treatment after relapse, the response time is variable and frank treatment failure may emerge in a subset of patients.
In this article we critically examine each of these points and their clinical implications, and speculate on some underlying neurobiological mechanisms. We have not attempted to cover all of the important aspects such as risk-factors for, and predictors of relapse, and our focus is on relapse in the earlier phase of illness.
Review
Relapse rates after treatment discontinuation in first-episode schizophrenia
The rationale for clinicians to consider antipsychotic discontinuation after successful treatment of a first-episode of schizophrenia is based on three major considerations. First, there is a supposition that a substantial portion (perhaps 10–20%) of patients never experience a recurrence after a single psychotic episode [13], and will therefore not require ongoing maintenance treatment. Second, there is a considerable side-effect burden associated with antipsychotics. Prior to the availability of the second generation antipsychotics (SGAs) physicians were primarily concerned with the risk of motor disorders, particularly tardive dyskinesia (TD). In fact, it was recommended that antipsychotics should not be prescribed over a long period of time without adequate justification, for both clinical and medico-legal reasons [14]. Shortly after the introduction of the SGAs the hope was expressed that these agents, with their reduced propensity for motor side-effects, would carry a small enough risk to warrant indefinite maintenance treatment [15]. However, it is now recognized that these agents carry a significant side-effect burden of their own, including weight gain and its metabolic concomitants [16] and hyperprolactinaemia [17]. Also, it has been reported that rates of TD with SGAs, although lower than with conventional antipsychotics, are not as low as originally thought [18]. A third important reason for considering antipsychotic withdrawal is that clinicians may have difficulty in convincing patients that indefinite treatment is indicated after a single episode of psychosis, particularly those who have responded favourably to treatment. Treatment disengagement is common early in the illness, and the decision to discontinue medication is largely patient driven [19]. It could be argued that planned medication withdrawal with careful follow-up is preferable to treatment disengagement or covert non-adherence.
When determining the most appropriate maintenance treatment plan for an illness one aspect that needs to be considered is the risk of recurrence after discontinuation of treatment. While studies of treatment discontinuation consistently report higher relapse rates than with maintenance treatment, results differ widely. A comprehensive review of relapse after antipsychotic withdrawal in schizophrenia included 4365 patients from 66 studies published between 1958 and 1993 [20]. The authors found a mean cumulative relapse rate of 52% (ranging from 0% to 100%) over a mean follow-up period of 6.3 months (ranging from 0.5 to 24 months) for patients withdrawn from antipsychotics, versus 16% for those patients who continued to receive maintenance antipsychotic treatment. How-ever, these studies were conducted between 1958 and 1992, and interpretation of the results is hampered by inconsistencies in aspects such as diagnostic criteria, duration of treatment prior to antipsychotic discontinuation, degree of response at the time of discontinuation, criteria used to define relapse, and perhaps most significantly, the duration of follow-up periods. Furthermore, all but two of the 66 studies reported in the Gilbert et al. review [20] were conducted in chronic, multi-episode samples.
We performed a systematic review of the literature to identify studies that investigated relapse rates after treatment discontinuation after a first-episode of schizophrenia. We used the following key words: “first-episode schizophrenia or first-episode psychosis” combined with “discontinuation, intermittent treatment”. We also checked the reference lists of the relevant publications. We identified eight studies, details of which are summarised in Table 1. As with the multi-episode samples, these studies report varying rates of relapse, with four reporting symptom recurrence rates of close to 80% at 12 months after discontinuation [10, 21–23] and two reporting rates of about 95% at 24 months [10, 21]. Reasons for the lower reported recurrence rates in the other studies are not entirely apparent, although the Kane et al. study [24] had a high dropout rate (40%) and these patients were considered not to have relapsed; and in the Wunderink et al. study [25], of 65 patients randomized to the discontinuation arm 14 (21.5%) did not have symptom recurrence. Sixteen (24.6%) relapsed and 5 (7.7%) had mild symptom recurrence. However, in 30 subjects (46.2%) in the discontinuation arm antipsychotics were not discontinued due to physician concerns of worsening of psychosis. Taken together, these results suggest that even after a single episode of psychosis the vast majority of patients will experience symptom recurrence if followed up for a sufficient period of time.
It could be argued that a substantial proportion of patients remain relapse-free even 12 months after treatment discontinuation, and that these patients may not require continuous antipsychotic treatment. This may be an option if such patients could be identified prior to considering treatment discontinuation. However, while Chen et al. found pre-morbid schizoid and schizotypal traits, level of functioning, and a diagnosis of schizophrenia to significantly predict relapse after 12 months of treatment discontinuation, we were unable to identify any predictors of early relapse in our own study [10].
Duration of antipsychotic treatment and risk of relapse after discontinuation
A key clinical question is what the risk of relapse is after a single episode of psychosis, and whether the risk is reduced with a longer treatment period. Despite the fact that several studies have assessed the risk of relapse after discontinuation of antipsychotic medication, there is no consensus on the recommended duration of treatment. A recent systematic review of guidelines for maintenance treatment of schizophrenia found that, of 14 such guidelines, discontinuation of antipsychotic medication after a first-episode of schizophrenia was partially recommended after 1 to 2 years in six, not recommended in two, and not mentioned in six [28].
It can be seen from Table 1 that the duration of treatment periods before withdrawal varied. There was no indication of reduced risk with longer treatment periods - in fact, the study with the longest prior treatment period (2 years)[10] had the highest risk of symptom recurrence. This has implications for clinical practice, and suggests that lengthening the recommended treatment period after a first psychotic episode does not reduce the risk of recurrence. It could even be speculated that a longer treatment duration might increase risk of relapse, although the study with the shortest reported treatment period (3 months in remission) had an equally high symptom recurrence rate [21].
Time to relapse after treatment discontinuation
The interval between treatment discontinuation and symptom recurrence is highly variable. Three of the eight studies investigating relapse rates after treatment discontinuation (Table 1) reported mean times to relapse of 235 days [21], 323 days [27] and 207 days [10]. This could create the impression that patients remain well for a considerable period – perhaps months – before relapse. While this may be so for some, in many cases relapse occurs within days or weeks of discontinuation. In our own study all patients were treated with long-acting risperidone injection which is associated with the persistence of steady state blood levels for several weeks after the last injection [29]. Despite this several symptom recurrences occurred within a few weeks of the last injection, suggesting that relapse occurs with treatment reduction even in the presence of substantial antipsychotic occupancy of D2 receptors. Symptom recurrence shortly after treatment discontinuation is well recognized and has raised the question whether relapse may be a feature of drug withdrawal rather than the re-emergence of an underlying illness, at least in some patients [30]. The term “neuroleptic-induced supersensitivity psychosis” was originally proposed, and was linked to a hypothesised underlying mechanism of increased sensitivity of mesolimbic dopamine D2 receptors as a consequence of chronic D2 blockade with antipsychotic medication [31]. Moncrieff [30] suggested an alternative term of “rapid onset psychosis”, which does not imply underlying mechanisms. In a review article he pointed out that if the process of antipsychotic drug withdrawal is in itself psychotogenic, then the psychosis would be expected to have its own distinct symptom profile, different to that of the underlying illness. He underlined the need for further urgent research in this area. We were able to investigate this possibility by comparing the factor analysis derived symptom domains observed in the first psychotic episode with that of a recurrence episode. We found that symptom expression profiles were similar for the two episodes and, except for the positive domain, of similar severity [10]. While this counts against a role for a distinct antipsychotic withdrawal syndrome, we did not specifically examine the symptom profiles of those patients with rapid onset of relapse.
Onset of relapse may be abrupt
Reliable early warning signs of relapse would be of great value in clinical settings. They would offer the opportunity of early intervention and prevention of florid relapse. Indeed, success has been reported in identifying early signs of relapse [32]. However, whereas the onset of a first episode of psychosis may be gradual and is typically heralded by a prodromal period lasting months to even years [33], this does not appear to be the case in relapse episodes. For these reasons it has been recommended that the term “prodromal symptoms” be restricted to precursors of a first psychotic episode and "early warning signs" be used to describe antecedents of psychotic relapse [34]. Studies suggest that it may be difficult to identify many patients who are at risk of imminent relapse in clinical practice, and that early warning signs are relatively unreliable predictors of relapse [35–37]. Using a structured interview for early signs of relapse, Herz and Mellville [38] assessed 145 patients with chronic schizophrenia and 80 family members. Approximately half of the patients and 68% of the family members indicated that the interval between the onset of noticeable symptoms and relapse was at least 1 week. Between 8 and 15% of patients and families gave this interval as 1 to 3 days and 7 to 8% patients and 11% families indicated that it was less than 1 day. Birchwood et al. [32] reported that 75% of relatives of patients noticed changes from 2 to 4 weeks before relapse. Henmi [39] retrospectively investigated 61 schizophrenic outpatients in remission, of whom 33 had relapses in the past 20 months. Non-specific (non-psychotic) prodromal symptoms were identified 4 weeks prior to relapse in 64%, although no changes were detected in global assessment of function. Tarrier et al. [40] compared symptoms of 16 patients who relapsed within 9 months after discharge with 16 patients who had not, and found a significant increase in depressive symptoms and hallucinations in the preceding month in those who had relapsed. In a review of the pertinent literature Norman and Malla [35] concluded that prodromal symptoms have only modest power as predictors of relapse. In a study investigating the predictive validity of self-reported early warning signs of relapse in a cohort of 60 remitted first-episode patients, the Early Signs Scale (ESS) achieved adequate sensitivity but poor specificity and positive predictive validity in predicting relapse or symptom exacerbations [41].
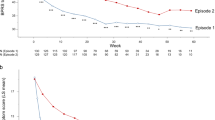
One difficulty in interpreting results of longitudinal studies assessing precursors of relapse is that the relapse events occur at different timepoints in different individuals. Therefore, group mean symptom scores at assessment visits do not give an accurate picture of symptom changes prior to relapse. To circumvent this problem we analysed precursors of relapse in a different way in two studies [10, 11]. With the relapse visit as starting point we grouped patients with the preceding visits arranged before that (i.e. visit −1, -2, -3). We did not find a gradual worsening of symptoms prior to relapse, but rather that patients remained in remission right up until and including the visit prior to relapse. Retrospective estimates of caregivers indicated a mean duration 16.3±10.9 days between the onset of the first recognisable symptoms and psychotic symptom recurrence, with several patients relapsing within a matter of days [10]. Our analyses were conducted retrospectively and it is possible that with more frequent assessments and with the use of more sensitive instruments designed specifically to detect prodromal symptoms more subtle symptoms could have been detected. Nevertheless, the results suggest that in everyday clinical practice relying on early warning signs to prevent full-blown relapse would not be feasible. Frequent and careful follow-up together with the use of instruments specifically designed to detect early warning signs would be necessary [42].
Once illness recurrence occurs symptom severity rapidly returns to levels similar to the initial psychotic episode
We observed a rapid return of symptoms in the relapse episode to severity levels similar to those in the acute phase of the first psychotic episode. This rapid return of symptoms occurred despite marked differences in estimated duration of untreated psychosis for the first-episode (129 ± 199 days) [43] and the second episode (16.3 ± 10.9 days) [12]. This finding is consistent with that of Chen et al. who found no significant correlation between symptom severity and time to receiving treatment [22].
Is relapse associated with disease progression?
In addition to its associated psychosocial risks, active psychosis may affect the brain in a more fundamental way. It has been suggested that psychosis may be neurotoxic and that acute psychotic exacerbations represent active periods of a morbid process that leads to disease progression and to impairment of treatment response [4, 44, 45]. Supportive evidence was initially provided by the well replicated finding that a longer duration of untreated psychosis is associated with a poorer long-term outcome [46]. Similarly, relapses also represent episodes of active psychosis and may also be associated with illness progression. However, to date there is limited empirical evidence to support the neurotoxic psychosis hypothesis, and specifically for illness progression after relapse. A search of the literature revealed the following: 1) Treatment response has been observed to be better in first-episode schizophrenia than in chronic multi-episode schizophrenia [45]. 2) A study utilizing the neuroleptic threshold principle found that first-episode patients required lower doses of haloperidol to achieve optimal clinical response than multi-episode patients [47], raising the possibility that tolerance to the effects of antipsychotics may develop. 3) Eighty % of patients with schizophrenia were judged to have deteriorated over time in a 7-yr follow-up study, and the degree of deterioration was significantly correlated with the number of relapses that patients experienced [48]. 4) In another long-term follow-up study of the natural course of schizophrenia, Wiersma et al. examined the course of patients over the first four psychotic episodes. They reported a remarkable observation, namely that, on average 1 in 6 patients failed to remit after each episode, irrespective of which episode it was. 5) More direct evidence was obtained in a preliminary study comparing treatment response times of first and subsequent episodes, where median (SE) times to remission were significantly longer for the second episode and third episode [4]. On the other hand, there is evidence to suggest that disease progression does not occur as a consequence of relapse: 1) It has been reported that patients’ symptoms rapidly return to baseline with resumption of antipsychotic medication shortly after recurrence of psychotic symptoms [49]; 2) In patients with relatively refractory schizophrenia who were exposed to placebo treatment for at least 6 weeks and experienced symptom worsening, it was found that, given a sufficiently lengthy recovery period, symptom levels returned to those of baseline [50]; 3) Response trajectory analyses in early psychosis suggest that, while some patients respond poorly initially, response is generally characterised by amelioration [51]; 4) The clinical and neurobiological evidence for neurotoxicity of psychosis has been reviewed and found wanting [52]; 5. Finally, a recent paper challenges the concept of schizophrenia as a progressive brain disease, arguing the following: a) While longitudinal studies report a poor outcome in approximately 25% of patients, few of them describe incremental deterioration that would characterize neurodegenerative disorders; b) while some neuro-imaging studies report brain tissue volumes decreasing over time, this could be attributed to the effects of antipsychotic medication, substance abuse, effects of lifestyle or elevated glucocorticoid levels associated with chronic stress; c) cognitive functioning does not appear to deteriorate over time; and d) the deterioration that occurs in some patients could reflect poor access, or adherence, to treatment, the effects of concomitant conditions, and social and financial impoverishment [53].
We were able to compare treatment response before and after relapse in both a first-episode [12] and a multi-episode [11] sample. We found that in both groups treatment response was highly variable, with some patients rapidly returning to pre-relapse symptom severity levels, and others having a more protracted recovery. Most notably, we found evidence of emergent treatment failure in a subset of 16% of the first episode and 14% of the multi-episode samples respectively. These results are consistent with the findings of Wiersma et al. [54] who reported that on average 1 in 6 patients failed to recover from each of their first four relapses, irrespective of which relapse it was.
Dopamine and the neurobiology of relapse in schizophrenia
In addition to the obvious clinical implications, our observations may shed light on the underlying pathogenesis of the illness. The very high relapse rates and abrupt re-emergence of psychotic symptoms suggest a reduced threshold for psychotic decompensation once a first episode has occurred [32], and are consistent with a direct relationship between dopamine and psychosis. The dopamine hypothesis of schizophrenia has been central to our understanding of neurobiological mechanisms underpinning the illness, and dopamine D2 receptor blockade remains a necessary and sufficient component for antipsychotic action [55]. In a recent elaboration of the dopamine hypothesis Howes and Kapur [56] incorporate multiple genetic and environmental factors that compromise the brain and manifest as dopamine dysregulation. They point out that elevated striatal dopamine function is likely linked to the dimension of psychosis rather than the full spectrum of symptom expression of the illness. Therefore relapse, characterised by acute psychotic exacerbation, would be associated with striatal dopamine hyperfunction, likely as elevation of presynaptic dopamine synthesis [57]. Linked to the dopamine hypothesis is the proposal that psychosis represents a state of aberrant salience due to a dysregulated hyperdopaminergic state [58]. A direct relationship is proposed between dopamine, psychosis and antipsychotic action, and supportive evidence is provided by the finding that the onset of antipsychotic effect is rapid rather than, as previously thought, delayed [59–61]. According to the aberrant salience hypothesis antipsychotics do not eradicate symptoms but dampen them. When they are discontinued there is a resurgence of a hyperdopaminergic state with symptoms being re-invested with salience [62], which would manifest as a rapid return of previous symptoms. This hypothesis is consistent with 1) the very high relapse rates reported after antipsychotic treatment discontinuation; 2) the failure of a longer treatment duration to reduce the risk of relapse when treatment is discontinued; 3) the onset of relapse soon after discontinuation in many patients; and 4) the abrupt onset of recurrence symptoms, with rapid return to levels of symptom severity that are similar to the previous episode.
The “glutamate” hypothesis of schizophrenia emerged from the observation that inhibition of glutamate N-methyl-D-aspartate (NMDA) receptors, with for example phencyclidine, induces an array of schizophrenia-likebehaviours in humans. Cortical and limbic striatal (nucleus accumbens) dopamine release is regulated by a glutamate-GABA-glutamate loop located on pyramidal cells of the frontal cortex [63]. Cortical hypoglutamatergia in turn compromises dopamine release in the ventral tegmentum leading to meso-limbic hyperdopaminergic and meso-cortical hypodopaminergia that we observe as positive or negative symptoms, respectively. Thus schizophrenia envelopes a combined state of glutamate and dopamine dysfunction [63]. However, altered glutamate may originate from various sources with activation of the NMDA receptor representing a distal event in the cascade, thereafter leading to the aforementioned dopamine changes. Schizophrenia is associated with a pro-inflammatory state [64], with altered blood/cerebrospinal fluid levels of interleukin-2 (IL-2), IL-6, IL-1, IL-10 and tumour necrosis factor (TNF)-α [65]. Mitochondrial dysfunction, altered pro-inflammatory cytokines and increased indoleamine 2,3 dioxygenase (IDO)-mediated conversion of tryptophan to quinolinic acid (an NMDA agonist) may directly or indirectly provoke glutamate hyperactivity leading to overt NMDA receptor activation, altered redox balance and oxidative stress. Importantly, each of the aforementioned either alone or in concert is capable of modifying dopamine release and function [66]. What is interesting is that increased CSF levels of IL-1 have been found to be a predictor of acute psychotic relapse in patients recently withdrawn from haloperidol [67]. Together this suggests that immune-inflammatory-glutamate dysfunction may play a critical role in the neurobiology of relapse. Indeed, the association between cytokine abnormalities and acute exacerbations of schizophrenia seems to be independent of antipsychotic medications [68]. In fact some cytokines (eg. IL-1β, IL-6, and TGF-β) as well as abnormal blood lymphocyte parameters (CD4/CD8) have been suggested to represent state markers for acute exacerbations of psychosis [69].
The pattern of treatment failure developing abruptly in a subset of patients suggests a threshold phenomenon, and is consistent with a sensitization, or “kindling” model. Such a model was initially proposed for TD where it was suggested that chronic antipsychotic exposure induces neostriatal dopaminergic receptor supersensitivity. Similarly, these same authors suggested that mesolimbic dopaminergic supersensitivity after chronic antipsychotic treatment could explain the emergence of antipsychotic treatment failure [31]. The kindling phenomenon has also been linked to increased excitatory glutamatergic activity combined with a relative loss of inhibitory GABA’ergic tone [70]. The vacuous chewing movement (VCM) model in rats has been proposed as a model for TD, and the involvement of dopamine receptor supersensitivity has been suggested [71]. Of note is that the VCM model is also associated with increased glutamate-nitric oxide signaling [72, 73] and striatal oxidative stress [74] that has also been linked to antipsychotic discontinuation [75]. Antipsychotic-induced striatal oxidative stress is abolished with N-acetyl cysteine (NAC), a glutathione replenisher and NMDA receptor modulator [74]. Thus, dopamine receptor supersensitivity, glutamate dysfunction and the release of reactive oxygen and nitrogen species together may play a role in the development of TD. Drawing on this analogy with TD may be useful in explaining post-relapse emergence of treatment non-responsiveness. Indeed, clinical [76] and animal [66] studies concur that adjunctive NAC is an effective antipsychotic augmentation strategy. It could be postulated that a relative imbalance in GABA-glutamate function, altered redox balance and its associated effects on cellular resilience lead to a self-perpetuating morbid process that eventually compromises long-term treatment response and disease outcome. It is not clear whether intermittent treatment or chronic, uninterrupted treatment is more likely to induce supersensitivity. While some evidence suggests that interrupted antipsychotic treatment may increase the risk of supersensitivity [77], sensitization of D2 receptors and ensuing treatment failure has been reported in animals not only during antipsychotic withdrawal, but also as a “breakthrough” phenomenon during chronic antipsychotic administration [78].
Conclusions
There is a need for further research on the phenomenology and neurobiology of relapse in schizophrenia. Particularly, the long-2222term outcome of patients with post-relapse treatment failure should be investigated to establish whether the emergent refractoriness persists. Given the difficulties in identifying those at risk of relapse, the ineffectiveness of rescue medications in preventing full-blown psychotic recurrence and the potentially serious consequences, every effort needs to be made to effectively address adherence and other factors predisposing to relapse. Antipsychotic treatment discontinuation should not be a part of routine clinical care and alternatives to the use of placebo in clinical trials need to be carefully reconsidered. However, despite the clearly demonstrated benefits of antipsychotic therapy in relapse prevention [79] it needs to be kept in mind that ongoing maintenance treatment carries its own burden, including substantial risk of relapse [11], significant side-effects and even the possibility of brain morphological changes [80].
References
Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, et al: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999, 56: 241-247. 10.1001/archpsyc.56.3.241.
Kane JM: Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007, 68 (Suppl 14): 27-30.
Wyatt RJ: Research in schizophrenia and the discontinuation of antipsychotic medications. Schizophr Bull. 1997, 23: 3-9. 10.1093/schbul/23.1.3.
Lieberman JA, Alvir JM, Koreen A, Geisler S, Chakos M, Sheitman B, et al: Psychobiologic correlates of treatment response in schizophrenia. Neuropsychopharmacology. 1996, 14: 13S-21S. 10.1016/0893-133X(95)00200-W.
Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al: Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012, 139: 116-128. 10.1016/j.schres.2012.05.007.
Coldham EL, Addington J, Addington D: Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand. 2002, 106: 286-290. 10.1034/j.1600-0447.2002.02437.x.
Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P: A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011, 168: 603-609. 10.1176/appi.ajp.2011.10081224.
Miller BJ: A review of second-generation antipsychotic discontinuation in first-episode psychosis. J Psychiatr Pract. 2008, 14: 289-300. 10.1097/01.pra.0000336756.65308.83.
Miller BJ, Bodenheimer C, Crittenden K: Second-Generation Antipsychotic Discontinuation in First Episode Psychosis: An Updated Review. Clin Psychopharmacol Neurosci. 2011, 9: 45-53.
Emsley R, Oosthuizen PP, Koen L, Niehaus DJ, Martinez L: Symptom Recurrence Following Intermittent Treatment in First Episode Schizophrenia Successfully Treated for Two Years. In J Clin Psychiatry. 2012, In press
Emsley R, Nuamah I, Hough D, Gopal S: Treatment response after relapse in a placebo controlled maintenance trial in schizophrenia. Schizophr Res. 2012, 138 (1): 29-34. 10.1016/j.schres.2012.02.030. Epub 2012 Mar 23
Emsley R, Oosthuizen PP, Koen L, Niehaus DJ, Martinez L: Comparison of Treatment Response in Second Episode Versus First Episode Schizophrenia. J Clin Psychopharmaco. 2013, 33 (1): 80-83. 10.1097/JCP.0b013e31827bfcc1.
Moller HJ, von Ziersen D, et al: Course and outcome of schizophrenia. Schizophrenia. 1995, Oxford: Blackwell, 127-
Kane JM, Jeste DV, Barnes TR: Tardive dyskinesia: A task force report of the American Psychiatric Association. 1992, Washington, D.C: American Psychiatric Association, Ref Type: Report
Meltzer HY: Neuroleptic withdrawal in schizophrenic patients. An idea whose time has come. Arch Gen Psychiatry. 1995, 52: 200-202.
Newcomer JW: Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007, 68 (Suppl 1): 20-27.
Bostwick JR, Guthrie SK, Ellingrod VL: Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009, 29: 64-73. 10.1592/phco.29.1.64.
Correll CU, Schenk EM: Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatry. 2008, 21: 151-156. 10.1097/YCO.0b013e3282f53132.
Perkins DO, Gu H, Weiden PJ, McEvoy JP, Hamer RM, Lieberman JA: Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry. 2008, 69: 106-113. 10.4088/JCP.v69n0114.
Gilbert PL, Harris MJ, McAdams LA, Jeste DV: Neuroleptic withdrawal in schizophrenic patients. A review of the literature. Arch Gen Psychiatry. 1995, 52: 173-188. 10.1001/archpsyc.1995.03950150005001.
Gitlin M, Nuechterlein K, Subotnik KL, Ventura J, Mintz J, Fogelson DL, et al: Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia. Am J Psychiatry. 2001, 158: 1835-1842. 10.1176/appi.ajp.158.11.1835.
Chen EY, Hui CL, Lam MM, Chiu CP, Law CW, Chung DW, et al: Maintenance treatment with quetiapine versus discontinuation after one year of treatment in patients with remitted first episode psychosis: randomised controlled trial. BMJ. 2010, 341: c4024-10.1136/bmj.c4024.
Boonstra G, Burger H, Grobbee DE, Kahn RS: Antipsychotic prophylaxis is needed after remission from a first psychotic episode in schizophrenia patients: results from an aborted randomised trial. Int J Psychiatry Clin Pract. 2011, 15: 128-134. 10.3109/13651501.2010.534801.
Kane JM, Rifkin A, Quitkin F, Nayak D, Ramos-Lorenzi J: Fluphenazine vs placebo in patients with remitted, acute first-episode schizophrenia. Arch Gen Psychiatry. 1982, 39: 70-73. 10.1001/archpsyc.1982.04290010048009.
Wunderink L, Nienhuis FJ, Sytema S, Slooff CJ, Knegtering R, Wiersma D: Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry. 2007, 68: 654-661. 10.4088/JCP.v68n0502.
Crow TJ, MacMillan JF, Johnson AL, Johnstone EC: A randomised controlled trial of prophylactic neuroleptic treatment. In Br J Psychiatry. 1986, 148: 120-127. 10.1192/bjp.148.2.120.
Gaebel W, Riesbeck M, Wolwer W, Klimke A, Eickhoff M, Von WM, et al: Relapse prevention in first-episode schizophrenia–maintenance vs intermittent drug treatment with prodrome-based early intervention: results of a randomized controlled trial within the German Research Network on Schizophrenia. J Clin Psychiatry. 2011, 72: 205-218. 10.4088/JCP.09m05459yel.
Takeuchi H, Suzuki T, Uchida H, Watanabe K, Mimura M: Antipsychotic treatment for schizophrenia in the maintenance phase: a systematic review of the guidelines and algorithms. Schizophr Res. 2012, 134: 219-225. 10.1016/j.schres.2011.11.021.
Gefvert O, Eriksson B, Persson P, Helldin L, Bjorner A, Mannaert E, et al: Pharmacokinetics and D2 receptor occupancy of long-acting injectable risperidone (Risperdal Consta) in patients with schizophrenia. Int J Neuropsychopharmacol. 2005, 8: 27-36. 10.1017/S1461145704004924.
Moncrieff J: Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr Scand. 2006, 114: 3-13.
Chouinard G, Jones BD: Neuroleptic-induced supersensitivity psychosis: clinical and pharmacologic characteristics. Am J Psychiatry. 1980, 137: 16-21.
Birchwood M, Smith J, MacMillan F, Hogg B, Prasad R, Harvey C, et al: Predicting relapse in schizophrenia: the development and implementation of an early signs monitoring system using patients and families as observers, a preliminary investigation. Psychol Med. 1989, 19: 649-656. 10.1017/S0033291700024247.
Yung AR, McGorry PD: The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996, 22: 353-370. 10.1093/schbul/22.2.353.
Bustillo J: Buchanan RW. Carpenter WT Jr: Prodromal symptoms vs. early warning signs and clinical action in schizophrenia. Schizophr Bull. 1995, 21: 553-559.
Norman RM, Malla AK: Prodromal symptoms of relapse in schizophrenia: a review. Schizophr Bull. 1995, 21: 527-539. 10.1093/schbul/21.4.527.
Gaebel W, Riesbeck M: Revisiting the relapse predictive validity of prodromal symptoms in schizophrenia. Schizophr Res. 2007, 95: 19-29. 10.1016/j.schres.2007.06.016.
Gaebel W, Frick U, Kopcke W, Linden M, Muller P, Muller-Spahn F, et al: Early neuroleptic intervention in schizophrenia: are prodromal symptoms valid predictors of relapse?. Br J Psychiatry Suppl. 1993, 21: 8-12.
Herz MI, Melville C: Relapse in schizophrenia. Am J Psychiatry. 1980, 137: 801-805.
Henmi Y: Prodromal symptoms of relapse in schizophrenic outpatients: retrospective and prospective study. Jpn J Psychiatry Neurol. 1993, 47: 753-775.
Tarrier N, Barrowclough C, Bamrah JS: Prodromal signs of relapse in schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 1991, 26: 157-161.
Gleeson JF, Rawlings D, Jackson HJ, McGorry PD: Early warning signs of relapse following a first episode of psychosis. Schizophr Res. 2005, 80: 107-111. 10.1016/j.schres.2005.07.019.
Birchwood M, Spencer E: Early intervention in psychotic relapse. Clin Psychol Rev. 2001, 21: 1211-1226. 10.1016/S0272-7358(01)00105-2.
Emsley R, Medori R, Koen L, Oosthuizen PP, Niehaus DJ, Rabinowitz J: Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol. 2008, 28: 210-213. 10.1097/JCP.0b013e318167269d.
Wyatt RJ: Neuroleptics and the natural course of schizophrenia. Schizophr Bull. 1991, 17: 325-351. 10.1093/schbul/17.2.325.
Lieberman JA, Jody D, Geisler S, Alvir J, Loebel A, Szymanski S, et al: Time course and biologic correlates of treatment response in first-episode schizophrenia. Arch Gen Psychiatry. 1993, 50: 369-376. 10.1001/archpsyc.1993.01820170047006.
Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T: Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005, 62: 975-983. 10.1001/archpsyc.62.9.975.
McEvoy JP, Hogarty GE, Steingard S: Optimal dose of neuroleptic in acute schizophrenia. A controlled study of the neuroleptic threshold and higher haloperidol dose. Arch Gen Psychiatry. 1991, 48: 739-745.
Curson DA, Barnes TR, Bamber RW, Platt SD, Hirsch SR, Duffy JC: Long-term depot maintenance of chronic schizophrenic out-patients: the seven year follow-up of the Medical Research Council fluphenazine/placebo trial. III. Relapse postponement or relapse prevention? The implications for long-term outcome. Br J Psychiatry. 1985, 146: 474-480. 10.1192/bjp.146.5.474.
Glovinsky D, Kirch DG, Wyatt RJ: Early antipsychotic response to resumption of neuroleptics in drug-free chronic schizophrenic patients. Biol Psychiatry. 1992, 31: 968-970. 10.1016/0006-3223(92)90124-I.
Wyatt RJ, Henter ID, Bartko JJ: The long-term effects of placebo in patients with chronic schizophrenia. Biol Psychiatry. 1999, 46: 1092-1105. 10.1016/S0006-3223(99)00227-9.
Levine SZ, Leucht S: Elaboration on the early-onset hypothesis of antipsychotic drug action: treatment response trajectories. Biol Psychiatry. 2010, 68: 86-92. 10.1016/j.biopsych.2010.01.012.
McGlashan TH: Is active psychosis neurotoxic?. Schizophr Bull. 2006, 32: 609-613.
Zipursky RB, Reilly JL, Murray RM: The myth of schizophrenia as a progressive brain disease. Schizophr Bull. 2012, Epub ahead of print
Wiersma D, Nienhuis FJ, Slooff CJ, Giel R: Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull. 1998, 24: 75-85. 10.1093/oxfordjournals.schbul.a033315.
Kapur S, Mamo D: Half a century of antipsychotics and still a central role for dopamine D2 receptors. Prog Neuropsychopharmacol Biol Psychiatry. 2003, 27: 1081-1090. 10.1016/j.pnpbp.2003.09.004.
Howes OD, Kapur S: The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull. 2009, 35: 549-562. 10.1093/schbul/sbp006.
Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, et al: The Nature of Dopamine Dysfunction in Schizophrenia and What This Means for Treatment: Meta-analysis of Imaging Studies. Arch Gen Psychiatry. 2012, 69 (8): 776-786. 10.1001/archgenpsychiatry.2012.169.
Kapur S: Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003, 160: 13-23. 10.1176/appi.ajp.160.1.13.
Agid O, Kapur S, Arenovich T, Zipursky RB: Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003, 60: 1228-1235. 10.1001/archpsyc.60.12.1228.
Leucht S, Busch R, Hamann J, Kissling W, Kane JM: Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry. 2005, 57: 1543-1549. 10.1016/j.biopsych.2005.02.023.
Emsley R, Rabinowitz J, Medori R: Time course for antipsychotic treatment response in first-episode schizophrenia. Am J Psychiatry. 2006, 163: 743-745. 10.1176/appi.ajp.163.4.743.
Kapur S, Agid O, Mizrahi R, Li M: How antipsychotics work-from receptors to reality. NeuroRx. 2006, 3: 10-21. 10.1016/j.nurx.2005.12.003.
Schwartz TL, Sachdeva S, Stahl SM: Glutamate neurocircuitry: theoretical underpinnings in schizophrenia. Front Pharmacol. 2012, 3: 195-
Leonard BE, Schwarz M, Myint AM: The metabolic syndrome in schizophrenia: is inflammation a contributing cause?. J Psychopharmacol. 2012, 26: 33-41. 10.1177/0269881111431622.
Drzyzga L, Obuchowicz E, Marcinowska A, Herman ZS: Cytokines in schizophrenia and the effects of antipsychotic drugs. Brain Behav Immun. 2006, 20: 532-545. 10.1016/j.bbi.2006.02.002.
Moller M, Du Preez JL, Viljoen FP, Berk M, Emsley R, Harvey BH: Social isolation rearing induces mitochondrial, immunological, neurochemical and behavioural deficits in rats, and is reversed by clozapine or N-acetyl cysteine. Brain Behavior and Immunity. 10.1016/j.bbi.2012.12.011. Epub ahead of print
McAllister CG, van Kammen DP, Rehn TJ, Miller AL, Gurklis J, Kelley ME, et al: Increases in CSF levels of interleukin-2 in schizophrenia: effects of recurrence of psychosis and medication status. Am J Psychiatry. 1995, 152: 1291-1297.
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B: Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011, 70: 663-671. 10.1016/j.biopsych.2011.04.013.
Miller BJ, Gassama B, Sebastian D, Buckley P, Mellor A: Meta-Analysis of Lymphocytes in Schizophrenia: Clinical Status and Antipsychotic Effects. Biol Psychiatry. 2012, doi:10.1016/j.biopsych.2012.09.007. doi:pii: S0006-3223(12):00779-2.
Harvey BH, McEwen BS, Stein DJ: Neurobiology of antidepressant withdrawal: implications for the longitudinal outcome of depression. Biol Psychiatry. 2003, 54: 1105-1117. 10.1016/S0006-3223(03)00528-6.
Andreassen OA, Jorgensen HA: Neurotoxicity associated with neuroleptic-induced oral dyskinesias in rats, implications for tardive dyskinesia. Prog Neurobiol. 2000, 61: 525-531. 10.1016/S0301-0082(99)00064-7.
Naidu PS, Kulkarni SK: Excitatory mechanisms in neuroleptic-induced vacuous chewing movements (VCMs): possible involvement of calcium and nitric oxide. Behav Pharmacol. 2001, 12: 209-216. 10.1097/00008877-200105000-00006.
Nel A, Harvey BH: Haloperidol-induced dyskinesia is associated with striatal NO synthase suppression: reversal with olanzapine. Behav Pharmacol. 2003, 14: 251-255. 10.1097/00008877-200305000-00010.
Harvey BH, Joubert C, du Preez JL, Berk M: Effect of chronic N-acetyl cysteine administration on oxidative status in the presence and absence of induced oxidative stress in rat striatum. Neurochem Res. 2008, 33: 508-517. 10.1007/s11064-007-9466-y.
Harvey BH, Bester A: Withdrawal-associated changes in peripheral nitrogen oxides and striatal cyclic GMP after chronic haloperidol treatment. Behav Brain Res. 2000, 111: 203-211. 10.1016/S0166-4328(00)00156-X.
Berk M, Copolov D, Dean O, Lu K, Jeavons S, Schapkaitz I, et al: N-acetyl cysteine as a glutathione precursor for schizophrenia–a double-blind, randomized, placebo-controlled trial. Biol Psychiatry. 2008, 64: 361-368. 10.1016/j.biopsych.2008.03.004.
van Harten PN, Hoek HW, Matroos GE, Koeter M, Kahn RS: Intermittent neuroleptic treatment and risk for tardive dyskinesia: Curacao Extrapyramidal Syndromes Study III. Am J Psychiatry. 1998, 155: 565-567.
Samaha AN, Seeman P, Stewart J, Rajabi H, Kapur S: "Breakthrough" dopamine supersensitivity during ongoing antipsychotic treatment leads to treatment failure over time. J Neurosci. 2007, 27: 2979-2986. 10.1523/JNEUROSCI.5416-06.2007.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al: Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012, 379: 2063-2071. 10.1016/S0140-6736(12)60239-6.
Konopaske GT, Dorph-Petersen KA, Sweet RA, Pierri JN, Zhang W, Sampson AR, et al: Effect of chronic antipsychotic exposure on astrocyte and oligodendrocyte numbers in macaque monkeys. Biol Psychiatry. 2008, 63: 759-765. 10.1016/j.biopsych.2007.08.018.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/13/50/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Robin Emsley has participated in speakers/advisory boards and received honoraria from AstraZeneca, Bristol-Myers Squibb, Janssen, Lilly, Lundbeck, Organon, Pfizer, Servier, Otsuka and Wyeth. He has received research funding from Janssen, Lundbeck and AstraZeneca. Bonginkosi Chiliza has participated in speakers/advisory boards and received honoraria from Janssen and Sandoz. Brian Harvey has participated in speakers/advisory boards and has received honoraria from Bristol-Myers Squibb, Organon (Merck), Pfizer and Servier, and has received research funding from Lundbeck. Laila Asmal has no conflict of interest to declare.
Authors’ contributions
RE conceived and drafted the manuscript; BH was responsible for neurobiological inputs. BC and LA contributed to the conceptualisation and interpretation of results and drafting of the manuscript, and all authors reviewed and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Emsley, R., Chiliza, B., Asmal, L. et al. The nature of relapse in schizophrenia. BMC Psychiatry 13, 50 (2013). https://doi.org/10.1186/1471-244X-13-50
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-13-50