Abstract
Background
Recent reports indicate that Campylobacter species are becoming one of the leading causes of bacterial diarrhoeal disease worldwide and most of the isolates are resistant to different antibiotics. This study aimed at determining the prevalence, associated risk factors and susceptibility pattern of Campylobacter species in under-five diarrheic children.
Methods
A cross-sectional study was conducted from October 2011 to March 2012. Samples were collected from under five diarrhoeic children who visited University of Gondar Teaching Hospital and seeking medical services during the study period. Stool specimens were aseptically inoculated using selective media and species isolation was further processed following standard procedures. Antimicrobial susceptibility test for Campylobacter species was performed using the standard agar disc diffusion method. The data was entered and analyzed using SPSS version 16 packages. Odd ratio was used to see their association between variables and then logistic regression was used to measure strengths of association. P-values less than 0.05 were taken as statistically significant.
Result
A total of 285 under five children with diarrhoea were included in this study. Of these144 (50.5%) were males and 141(49.5%) were females with the age range of one month to five years and mean age of 2.26 years (25months). Among 285 stool specimens cultured, 44(15.4%) of them were positive for Campylobacter species. Culture positivity for Campylobacter was higher in children below 12 months of age. Latrine usage, water source, boiling drinking water, bottle feeding, nutritional status and exposure to domestic animals had statistically significant association. Highest drug resistance rate were found in ampicillin (68.2%), tetracycline (56.8%) and trimethoprim- sulfamethoxazole (54.5%).
Conclusion
Isolation rate of Campylobacter species were frequent among under five children. The frequency was higher in those children who were malnourished, drinking of unprotected water and direct contact with infected animals (especially cats, dogs, pigeons, hens and their products). The antimicrobial resistance patterns for some of the commonly prescribed antibiotics were high. Therefore, awareness of hand washing and proper boiling of drinking water are probably important in preventing infection with Campylobacter species and childhood diarrhea should not be underestimated and effectiveness of the drugs should be continuously monitored by doing antimicrobial susceptibility test.
Similar content being viewed by others
Background
Campylobacter species (Campylobacter spp.) are small gram-negative, non-spore-forming, helical bacteria with a distinctive ‘darting’ motility, and are catalase and oxidase positive. Campylobacter spp. can be found in the reproductive organs, intestinal tracts, and oral cavity of animals and humans [1]. Diarrhoeal diseases are common in children aged less than five years, consumption of contaminated water and food is the major source of infection. Among Campylobacter spp., most commonly isolated species from cases of gastroenteritis was Campylobacter jejuni (C. jejuni) followed by Campylobacter coli. More recently, other Campylobacter species have been recognized as gastrointestinal pathogens in both industrialized and developing countries [2]. Campylobacter spp. are leading cause of bacterial diarrhoeal disease worldwide resulting mainly from contamination of poultry, or other meats, raw milk and milk products and surface or raw water [3].
The increasing rate of human infections caused by anti-microbial resistance strains of Campylobacter makes clinical management of cases of campylobacteriosis more difficult. Anti-microbial resistance can prolong the illness and compromise treatment of patients with bacteraemia. The rate of anti-microbial resistant enteric infections was highest in the developing world, where the use of anti-microbial drugs in humans and animals are largely unrestricted [4].
In Africa, a few studies have indicated that campylobacteriosis is most common among children of young age. In Ile-Ife, Nigeria, C. jejuni was found to be an important agent of diarrhoea in children [5]. In Durban, South Africa, Campylobacter were found in 21% of diarrhoeal cases among children aged less than five years [6]. Again in Venda, South Africa, Campylobacter spp. were also isolated from 20% of stool samples tested from HIV-positive individuals [7].
In Ethiopia, studies have revealed that diarrhoeal diseases are major causes of infant and child mortality and morbidity. About 39,000,000 episodes of diarrhoea per year were estimated to occur in Ethiopia; out of which 230,000 deaths occur in children below five years of age [8]. The pediatric admission review at Jimma hospital showed that diarrhoea was the second leading cause of admission and hospital deaths and Campylobacter is one cause of diarrhoea in the area [9]. There is no recent report on Campylobacter spp. and their drug susceptibility patterns in the North western Ethiopia. Therefore, this study aimed at determining the prevalence, associated risk factors and antimicrobial susceptibility pattern of Campylobacter spp. causing enteritis in under five diarrheic children at Gondar University Hospital, Northwest Ethiopia.
Methods
Study design and period
A cross-sectional study was conducted in Microbiology Laboratory at University of Gondar Teaching Hospital between October, 2011 and March, 2012. It is referral hospital that provides services to over 5 million inhabitants in the Northwest, Ethiopia. All the under five diarrhoeic children coming to the pediatric ward of the Gondar hospital seeking for treatment during the study period were the source population.
Sample size determination and Sampling technique
A total of 285 samples were collected from under five diarrhoeic children who visited University of Gondar Teaching Hospital and seeking medical services during the study period. Convenient sampling technique was used.
Inclusion criteria
All the under five diarrhoeic children coming to the pediatric ward of the Gondar hospital seeking for treatment during the study period.
Exclusion criteria
Those diarrheoic children under five years who had treatment with antibiotics in the last 5 days were excluded.
Data collection procedure
After obtaining written consent from the guardian, data about the socio-demographic characteristics, associated risk factors and relevant clinical information were taken using pre-structured questionnaire by pediatrician. To assess the validity of the questionnaire pre-test was conducted at the polyclinic: one of the health centers found in Gondar town. Two laboratory technologists were responsible to process the stool specimen for isolation of Campylobacter spp. To ensure the reliability of the information, the guardian’s were interviewed in their local language. All the questionnaires were checked for its completeness and consistency every day.
Specimen collection and processing
Fresh stool specimen was collected aseptically from each study subject using sterile screw-capped containers and transported immediately to the Microbiology Laboratory, University of Gondar. Specimens were inoculated on Campylobacter Agar Base (Karmali) (Oxoid, Ltd,England) supplemented with sodium pyruvate, cefoprazone, vancomycin and cyclohexamide then, kept in a 2.5 liter anaerobic jar and Campy-Gen gas generating kit (5% O2 and 10% CO2) (Oxoid CN0025A) was inserted to maintain the microarophilic condition. The jars were incubated at a temperature of 42°C for 48 hrs. The identification of Campylobacter spp was performed by characteristic appearance on culture medium (moist, creamy-grey and flat-spreading), gram stain, oxidase test, catalase reaction and dry spot Campylobacter test (Oxoid, Basingstoke, Hampshire, England). The type strains C. jejuni (LMG 13646) was inoculated as positive control.
Antimicrobial susceptibility test
Antimicrobial susceptibility test for Campylobacter spp was performed using the standard agar disc diffusion method as recommended by Clinical and Laboratory Standards Institutions (CLSI). The commonly prescribed antimicrobials were obtained from Oxoid at the concentration of ampicillin (30 μg), amoxicillin with clavulanic acid (30 μg) gentamicin (10 μg), tetracycline (30 μg), doxycycline (30 μg), chloramphenicol (30 μg), ciprofloxacin (5 μg), norfloxacin (5 μg), ceftriaxone (5 μg) erythromycin (15 μg) clindamycin (15 μg) and trimethoprim-sulphamethoxazole (25 μg). In brief, 3–4 morphologically identical colonies of bacteria from culture were picked and suspended in sterile normal saline. Turbidity of the broth culture was compared with that of 0.5 McFarland turbidity standards (10). A loop full of the bacterial suspension was placed at the center of Muller Hinton agar media (Oxoid, LTD) supplemented with 5% sheep blood and evenly spread using sterile cotton tipped applicator. After drying, antibiotic discs were placed and incubated at 42°C for 48 hours in anaerobic jar using CO2 generating kits. Finally, the diameter of growth inhibition around the discs was measured and interpreted as sensitive (S), and resistant (R) as per the guidelines of the manufacturer. Control strains of E. coli (ATCC 25922) sensitive to all antibiotic being tested was inoculated to evaluate the performance of culture media and antibiotic discs.
Susceptibility tests to naldixic acid (30 μg) (Oxoid, UK) and Cephlotin (30 μg) (Oxoid UK) were performed for all isolates of Campylobacter spp. in accordance with the criteria set by the National CLSI using the disk diffusion method [10]. The isolates were classified as sensitive and/or resistant according to the standardized tables supplied by the CLSIs. Campylobacter strains that were sensitive to naldixic acid but which are resistant to Cephlotin were considered C. jejuni and C. coli, while strains that were resistant to both drugs were considered other species [11].
Data processing and analysis
The data was entered and analyzed using SPSS version 16 packages. Odd ratio was used to compare association between Campylobacter spp and other variables of the study. Logistic regression was also used to assess associations with dependent and independent possible risk factor. P-values less than 0.05 were taken as statistically significant.
Ethical consideration
The study was conducted after obtaining institutional ethical clearance from Research and Publication office of University of Gondar. Permission was taken from Gondar University Hospital administrators and written consent also obtained from the guardians of study subjects. Positive study subjects to Campylobacter spp. were referred to the physician with their result for treatment.
Results
Socio-demographic characteristics
A total of 285 under five children with diarrhoea were included in this study. Of these144 (50.5%) were males and 141 (49.5%) were females with the age range of one month to five years and mean age of 2.26 years (25months). Seventy three (25.6%) of them were younger than one year and 212 (74.4%) were in the age range of 1 to 5 years. Majority of them were urban dwellers 230(80.7%) while 55 (19.3%) were rural dwellers [Table 1].
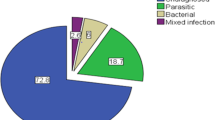
Prevalence of Campylobacterspecies
Among 285 stool specimens cultured, Campylobacter species were isolated from 44 (15.4%), from which 40/44 (90.9%) were C. jejuni and C. coli and 4/44 (9.1%) were other species. Twenty one (14.6%) of the male and 23(16.3%) of the female children were positive for Campylobacter species. Although, the variation was not statistically significant, the culture positivity for Campylobacter was relatively higher for children below 12 months of age compared to other age groups (P = 0.16). Even though, most study subjects live in urban, culture positivity rate is relatively higher in rural with the percentage of 14.8% and 18.2%, respectively [Table 1].
Possible risk factors and their association with Campylobacterinfections
Among the risk factors caretaker relation to child, education level of caretaker, family size, washing hands before feeding and preparing foods, cleaning utensils with soap and hypochlorite, washing the child with soap and water after defecation showed no statistically significant association with Campylobacter culture positivity; whereas usage of latrine, source of water, boiling drinking water, bottle feeding, nutritional status and exposure to domestic animals had statistically significant association [Table 2]. Of the 58 family who do not use latrine always 15(25.9%) of their children were found to be positive for Campylobacter species. Family who used latrine always were less likely to be positive for Campylobacter infection than those who do not use (AOR = 0.42; CI = 0.2, 0.90; P = 0.01).
The culture positive rate of Campylobacter species among study subjects who use pipe, well, river, and spring as a source of drinking water were 35 (14.1%), 3(75.0%), 3 (12.0%) and 3 (42.9%), respectively (Table 2). Children who used well and river as a source of drinking water had 4.6 and 2 times (AOR =2.0; CI = 2.0, 20.0; p = 0.001and AOR = 4.59; CI = 1.2, 21; P = 0.001) likely to be positive for Campylobacter infection, respectively. Children who drank boiled water were more protected from Campylobacter infection compared to non-boiled water users (AOR = 10.6; CI = 2.5, 45; P = 0.001). Of the one hundred children who use bottle feeding, 24 (24.0%) were positive for Campylobacter species compared to non bottle feeders 20/185 (10.8%). This indicate that children who used bottle feeding were 2.6 times (AOR = 2.6; CI = 1.36, 5.0; P = 0.008) more affected by Campylobacter infections. Malnourished children 14 (31.8%), were three times infected than well nourished 30 (12.4%) (AOR = 3.2; CI = 1.58, 6.8; P = 0.002). High culture positive rate of Campylobacter species had been observed in children who were exposed to domestic animals compared to non exposed. Children who were exposed to pet animals, hens and pigeons were found 2.9 times (AOR = 2.87; CI = 1.05, 7.88; P = 0.001) affected than non-exposed individuals. While children, who were exposed to cats and dogs were 5.1 times (AOR = 5.12; CI = 2.25, 11.65; P = 0.001) affected than non exposed children [Table 2].
The main significant clinical presentations for the Campylobacter culture positive children were abdominal pain (P = 0.002), but other symptoms like, fever, vomiting, duration of diarrhea, stool frequencies per 24 hours and stool consistency were not statistical significant in culture positive and negative patients [Table 3].
Antimicrobial susceptibility patters of the isolates
The results of antimicrobial susceptibility testing for Campylobacter species isolated from under five children with diarrhoea against 14 chosen antimicrobial agents are presented in Table 4. Lower resistance rate was observed in naldixic acid (9.1%), followed by chloramphenicol (11.4%) and norfloxacin (11.6%). However, higher drug resistances were observed in ampicillin (68.2%), tetracycline (56.8%) and trimethoprim sulfamethoxazole (54.5%).
Among the 44 Campylobacter culture positives, multidrug resistance (an isolate being resistant to two or more drugs) were detected in 30 (68.2%) of the strains. Among these 16 (36.4%) were resistant to four drugs (Table 5).
Discussion
This study showed that the prevalence of Campylobacter species in under five children with diarrhoea was 15.4%, which is slightly higher than other findings in Gondar [12], Dembia [13], Bahir Dar [14] and Jimma [15] with isolation rates of 13.8%, 10.5%, 8% and 11.6%, respectively. Lower incidence of Campylobacteriosis has been reported in Cameroon (7.7%) [16], Zimbabwe (9.3%) [17] and Egypt (9%) [18]. On the other hand slightly higher prevalence had been reported from Algeria (17.7%) [19], Nigeria (16.5%) [20], Tanzania (18%) [21], and South Africa (21%) [22] and higher prevalence reported from Bangladesh (26%) and Thailand (41%) [23, 24]. This could be due to differences in geographical location, study population, study period and method employed for each study. Our finding is consistent with reports from Iran (14.7%) [25] Peru (15%) [26] and Addis Ababa (15.3%) [13].
The distribution of Campylobacter species between females and males was not statistically significant, which agrees with the study results reported in different parts of Ethiopia [12, 13, 15, 27]. Although the finding was not statistically significant, higher rates were observed in rural (18.2%) than urban (14.8%), resident children, which is in line with the findings in Yemen and Mexico [28, 29]. This may be due to unprotected water source and presence of domestic animals in almost all rural house hold.
In this study, high infection rates were seen in under five children whose family didn’t use the latrine regularly and those whose family had no latrine in their home. Drinking water from unprotected source like river and well had statistical significant association with Campylobacter species culture positivity rate; so boiling drinking water had protective effect against Campylobacter infection, which is consistent with the study conducted in Yemen and Colorado [28, 30]. Our study also revealed that bottle feeding had also showed significant risk factors to Campylobacter infection in under five children. This can be explained by low level sterilization of the bottles, use of unpasteurized milk and storage of cooked food for later use.
High infection rates were seen in children who have close contact with pet animals (cats, dogs), pigeons and hens, which indicate the direct association between Campylobacter species infection and pets, as it is already pointed out that direct contact with these animals is a frequent mode of transmission to humans [30]. The rate of culture positivity was more likely higher among malnourished children than well nourished. This is consistent with the previous report in Chile [2], Gondar [12], Jimma [15] and Addis Ababa [27]. This may be due to low immune status of malnourished children.
In this study, abdominal pain was the most common symptom (92.2%) and had statistically significant association with isolation of Campylobacter species among under five children. This is consistent with the previous studies conducted in Thailand [18], Yemen [28], Jimma [15] and Addis Ababa [27]. Other symptoms such as fever, vomiting, duration of diarrhea, stool frequency per day and stool consistency were not important symptoms in the present study, which is similar with the study at Dembia [13] but different from previous studies in Thailand and Gondar, Jimma in which watery diarrhoea and the duration of diarrhoea had significant association, respectively [12, 15, 18].
Even though most gastroenteritis caused by Campylobacter species is often a mild and self-limiting disease, it causes mild to severe dehydration and occasionally spreads to the bloodstream and causes life-threatening infections in children; in this case it requires antibiotic treatment. In this study, fourteen antibiotics were tested against 44 isolates of Campylobacter species. Most tested isolates were sensitive to naldixic acid (90.9%) chloramphenicol (88.6%), nurfloxacin (86.4%), doxycicline (84.1%) ciprofloxacin (84%) and gentamicin (81.8%). Among these, norfloxacine ciprofloxacin and doxycicline are not prescribed to children due to their contradictions. A study from Jimma reported that all isolates of Campylobacter were sensitive to chloramphenicol and gentamicin [15]. This is different from our result that 11.4% and 18.2% resistance were detected in chloramphenicol and Gentamicin, respectively.
Campylobacter species were equally resistant to erythromycin and ceftriaxone in this study (22.7%), this is alarming because erythromycin is the drug of choice for Campylobacter species, and ceftriaxone it the 3rd generation cephalosporin, which is recently available in the market. Erythromycin resistance was higher than the previous study in Jimma (10%) [15] and Addis Ababa (2%) [13]. This might be due to the fact that erythromycin may act as a selective pressure and favor the proliferation of resistant strains.
A high percentage of amoxicillin with clavulanic acid resistance (36.4%) was also observed. This high rate may be due to indiscriminate use of amoxicillin in the area that leads to increased resistance. The majority of the isolates were resistant to ampicillin and trimethoprim-sulfamethoxazole (68.2%, 54.5%) respectively. This is almost similar to other studies conducted in Jimma and Addis Ababa [15, 27]. As it was indicated in another study, this higher resistance could be either because they are commonly prescribed and sold on the open market without prescription [15]. The rate of resistance to tetracycline against Campylobacter species (56.8%) in our study was higher than other results like Jimma (14%) [15], Addis Ababa (10%) [27] and Bahir Dar (22.2%) [14]. This might be due to the reason that tetracycline is frequently prescribed and sold in open market without prescriptions.
Compared with other similar research findings conducted in Addis Ababa and Jimma, this study showed increased resistance to most antibiotics. The frequency of multidrug resistant strains (resistant to two or more drugs) (68.2%) in this study was higher than the previous finding in Ethiopia (20%) [15].
Conclusions
The present study indicates that infection caused by Campylobacter species was very frequent among the under five children. The frequency were higher in malnourished than well nourished children. The possible risks of infection to children were through drinking of unprotected water or by direct contact with infected animals (especially cats, dogs, pigeons, hens and their products). Therefore, awareness of hand washing and proper boiling of drinking water are probably important in preventing infection with Campylobacter species. Our result showed that the resistance rate of Campylobacter species increased through time. This high rate of resistance reflects either frequently prescribing drugs without drug susceptibility testing results or inappropriate usage of the commonly available drugs in the local market. Therefore, providing treatments for children should be based on updated information on susceptibility pattern of Campylobacter species rather than clinical symptoms. Therefore, the clinicians and laboratory personnel should consider that diagnosing infection with Campylobacter species is as important as other infection with enteric pathogens. Further studies to investigate the role of domestic animals in the transmition of the disease, species differentiations and serotyping of Campylobacter spp are recommended.
References
Kassa T, Gebre-selassie S, Asrat D: The prevalence of thermo tolerant Campylobacter species in food animals in Jimma Zone, southwest Ethiopia. Ethiop J Health Dev. 2005, 19 (3): 225-229.
Fernández H, Vera F, Villanueva PM, García A: Occurrence of campylobacter species in health well-nourished and mal-nourished children. Brazilian Journal of Microbiology. 2008, 39: 56-58. 10.1590/S1517-83822008000100013.
Solomon EB, Hoover DG: Campylobacter jejuni: a bacterial paradox. J Food Safety. 1999, 19: 121-136. 10.1111/j.1745-4565.1999.tb00239.x.
Sean FA, Norman JS, Patricia IF, David LS: Centers for Disease Control and Prevention, Atlanta, Georgia USA. Emerg Infect Dis. 1999, 5 (1): 27-30.
Aboderin AO, Smith SI, Oyelese AO, Onipede AO, Zailani SB, Coker AO: Role of Campylobacter jejuni/coli in diarrhoea in Ill-Use, Nigeria. East Afr Med J. 2002, 79: 423-426.
Mackenjee MK, Coovadia YM, Coovadia HM, Hewitt J, Robins-Browne RM: Etiology of diarrhoea in adequately nourished young African children in Durban, South Africa. Ann Trop Paediatr. 1984, 4: 183-187.
Obi CL, Bessong PO: Diarrheagenic bacterial pathogens in HIV-positive patients with diarrhoea in rural communities of Limpopo province, South Africa. J Health Popul Nutr. 2002, 20: 230-234.
Kaba M, Ayele F: Ethnographic study of diarrhoeal diseases among under-five children in Mana district, Jimma Zone, Southwest Ethiopia. Ethiop J Health Dev. 2000, 14 (1): 77-83.
Meseret E: Analysis of pediatric admission to Jimma Hospital pediatric ward: A three year retrospective study. Bull JIHS:. 1994, 4: 1-11.
National Committee for Clinical Laboratory Standards: Performance standards for Antimicrobial Disk and Dilution Susceptibility Tests for bacterial isolated from animals. 1999, Wayne, PA: Approved standard M31-A-19, 11
National Committee for Clinical Laboratory Standards: Performance Standards for Antimicrobial Disk Susceptibility Tests. 2000, Wayne, PA USA: Approved standard M2–A7. National Committee for Clinical Laboratory Standards, 7
Gedlu E, Assefa A: Campylobacter enteritis among children in Northwest Ethiopia: a one-year prospective study. Ann Trop Paediat. 1996, 16: 207-212.
Mitike G, Kassu A, Genetu A, Nigussie D: Campylobacter enteritis among children in Dembia district Northwest Ethiopia. East Afr Med J. 2000, 77 (12): 654-657.
Ewunetu D, Mihert A: Prevalence and antimicrobial resistance of Campylobacter isolates from humans and chickens in Bahir Dar, Ethiopia. Foodborne Pathog Dis. 2010, 7 (6): 667-670. 10.1089/fpd.2009.0433.
Beyene G, Haile-Amlak A: Antimicrobial sensitivity pattern of Campylobacter species among children in Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop J Health Dev. 2004, 18 (3): 185-189.
Koulla-Shiro S, Loe C, Ekoe T: Prevalence of Campylobacter enteritis in children from Yaounde (Cameroon). Cent Afr J Med. 1995, 41: 91-94.
Simango C, Nyahanana M: Campylobacter enteritis in children in an urban community. Cent Afr Med J. 1997, 43: 172-175.
Rao MR, Naficy AB, Savarino SJ, Abu-Elyazeed R, Wierzba TF, Peruski LF: Pathogenicity and convalescent excretion of Campylobacter in rural Egyptian children. Am J Epidemiol. 2001, 154: 166-173. 10.1093/aje/154.2.166.
Wren BW, Linton D, Dorrell N, Karlyshev AV: Post genome analysis of Campylobacter jejuni. J Appl Microbiol. 2001, 90: 36-44. 10.1046/j.1365-2672.2001.01352.x.
Coker AO, Adefeso AO: The changing patterns of Campylobacter jejuni/ coli in Lagos, Nigeria after ten years. East Afr Med J. 1994, 71: 437-440.
Lindblom GB, Ahren C, Changalucha J, Gabone R, Kaijser B, Nilsson LA: Campylobacter jejuni/coli and enterotoxigenic Escherichia coli (ETEC) in faeces from children and adults in Tanzania. Scand J Infect Dis. 1995, 27: 589-593. 10.3109/00365549509047073.
Akitoye OC, Raphael D, Isokpehi , Bolaji N, Akitoye OC, Raphael D, Isokpehi WW, Thomas BN, Amisu KO, Larry Obi C: Human Campylobacteriosis in Developing Countries. Emerg Infect Dis. 2000, 8 (3)): 237-241.
Ashraful H, Rahman KM: Campylobacter jejuni as a cause of acute diarrhoea in children: a study of an urban hospital in Bangladesh. J Trop Med Hyg. 1991, 94: 50-54.
David NT, Martin JB, Peter EP, Bodhidatta L, Wang WLL: Erythromycin- Resistant Campylobacter Infections in Thailand. Antimicrob Agents Chemother. 1987, 31: 438-442. 10.1128/AAC.31.3.438.
Mehdi M, Dallal S: Diarrhea Caused by Enteropathogenic Bacteria in Children. Arch Iran Med. 2001, 4: 201-206.
Grados O, Bravo N, Black RE, Butzler JP: Pediatric Campylobacter diarrhea from household exposure to live chickens in Peru Lima. Bulletin of WHO. 1998, 66 (3): 369-374.
Asrat D, Hathaway A, Ekwall E: Studies on enteric Campylobacteriosis in Tikur Anbessa and Ethio-Swedish children's hospital, Addis Ababa, Ethiopia. Ethiop Med J. 1999, 37: 71-84.
Hassan A, Abdualbaki A, Khald A: Epidemiology, clinical features and antibiotic susceptibility of Campylobacter infections in Sanaa, Yemen. Journal of Chinese Clinical Medicine. 2007, 2 (8): 445-463.
Calva J, Palacios GM, Lopez-Vidal A: Cohort study of intestinal infection with Campylobacter in Mexican children. Lancet. 1988, 1: 503-506.
Richard S, Hopkins MD, Olmsted BS, Gregory R, Istre MD: Endemic Campylobacter jejuni Infection in Colorado: Identified Risk Factors. Am J Public Health. 1984, 74: 249-250. 10.2105/AJPH.74.3.249.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/13/82/prepub
Acknowledgement
We would like to thank and appreciate the contribution of Dr. Pascal and Dr. Abebe Beyene who sent us the necessary media and supplements from England and Belgium. We thank Dr. Zemene Tigabu, Pediatrician and Prof. Moges Tiruneh, Microbiologist for their support in accomplishing this work. We are also thankful to Getnet Ayalew, Amare Kifle for their assistance, and families’ of the children participated in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors declare that they have no competing interest.
Authors’ contributions
AL conceived the study, participated in sample collection, performed laboratory diagnosis, conducted data analysis and drafted the initial and final draft manuscript, FM, Prepared the initial and final drafts of the manuscript, CU, reviewed the initial and final drafts of the manuscript, BA, reviewed the initial and final drafts of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lengerh, A., Moges, F., Unakal, C. et al. Prevalence, associated risk factors and antimicrobial susceptibility pattern of Campylobacter species among under five diarrheic children at Gondar University Hospital, Northwest Ethiopia. BMC Pediatr 13, 82 (2013). https://doi.org/10.1186/1471-2431-13-82
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-13-82