Abstract
Background
Infant colic, characterised by excessive crying/fussing for no apparent cause, affects up to 20% of infants under three months of age and is a great burden to families, health professionals and the health system. One promising approach to improving its management is the use of oral probiotics. The Baby Biotics trial aims to determine whether the probiotic Lactobacillus reuteri DSM 17938 is effective in reducing crying in infants less than three months old (<13.0 weeks) with infant colic when compared to placebo.
Methods/Design
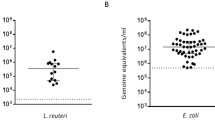
Design: Double-blind, placebo-controlled randomised trial in Melbourne, Australia. Participants: 160 breast and formula fed infants less than three months old who present either to clinical or community services and meet Wessel’s criteria of crying and/or fussing. Intervention: Oral once-daily Lactobacillus reuteri (1x108 cfu) versus placebo for one month. Primary outcome: Infant crying/fussing time per 24 hours at one month. Secondary outcomes: i) number of episodes of infant crying/fussing per 24 hours and ii) infant sleep duration per 24 hours (at 7, 14, 21, 28 days and 6 months); iii) maternal mental health scores, iv) family functioning scores, v) parent quality adjusted life years scores, and vi) intervention cost-effectiveness (at one and six months); and vii) infant faecal microbiota diversity, viii) infant faecal calprotectin levels and ix) Eschericia coli load (at one month only). Analysis: Primary and secondary outcomes for the intervention versus control groups will be compared with t tests and non-parametric tests for continuous data and chi squared tests for dichotomous data. Regression models will be used to adjust for potential confounding factors. Intention-to-treat analysis will be applied.
Discussion
An effective, practical and acceptable intervention for infant colic would represent a major clinical advance. Because our trial includes breast and formula-fed babies, our results should generalise to most babies with colic. If cost-effective, the intervention’s simplicity is such that it could be widely taken up as a new standard of care in the primary and secondary care sectors.
Trial Registration
Current Controlled Trials ISRCTN95287767
Similar content being viewed by others
Background
The burden of infant colic
Infant colic, characterised by excessive crying/fussing for no apparent cause, is common and distressing to families. Infant colic is defined clinically by Wessel’s criteria of crying and/or fussing ≥3 hours/day for ≥3 days/week for ≥3 weeks [1]. In research, the modified Wessel’s criteria of crying and/or fussing ≥3 hours/day for ≥3 days/week for one week is used for practicality and feasibility, due to the natural course of infant colic symptoms appearing by around three weeks, peaking at eight weeks, and remitting beyond 12 weeks of a term infant’s chronological age. Infant colic affects up to 20% of infants under three months [2, 3].
Infant colic poses a great burden to families, health professionals and the health system. Early infant sleeping and crying problems are the most common reason parents seek health professional help in the first three months of life, costing an estimated £65 million pounds per annum in the UK in 2001 [4]. Infant colic has significant adverse effects on maternal mental health and family quality of life [5, 6] and is a trigger for child abuse [7, 8]. Infants in whom crying persists beyond three months are at risk of adverse outcomes in the school years including anxiety, aggression, hyperactivity, allergy, and sleep disorders [9, 10], and at more than double the risk of poor mental health in later years [11]. Families of infants with colic are more dissatisfied with their daily family functioning in later years [12].
After 50 years of research into infant colic, its aetiology remains unclear and evidence-based management options limited. Finding an effective management strategy for infant colic could significantly reduce its associated morbidities and improve the quality of life of many families.
Proposed aetiological factors for infant colic
Debate continues around whether infant colic represents an extreme of the spectrum of normal crying, or a manifestation of underlying physiological or psychosocial factors. Perhaps, infant colic is best thought of as an exacerbation of infant crying with the aggravation brought about by either physiological factors within the infant, or psychosocial issues with the mother and infant [13]. Proposed psychosocial theories include difficult infant temperament, immaturity in the infant’s ability to modulate reactions to internal and external stimuli, inadequate maternal-infant interaction and maternal anxiety [13]. Physiological theories are based on gastrointestinal factors, including gut dysmotility, excessive intragastrointestinal air, and visceral pain [14, 15]. However, no study has been able to definitively prove whether these are causal factors of infant colic. Gastro-oesphageal reflux was traditionally assumed to be a cause of infant distress, but several recent clinical trials have demonstrated that it is an unlikely cause for persistent crying [16, 17]. Food allergy is perhaps the strongest factor identified so far in the causal pathway to crying [18–22], with gut inflammation resulting from allergy to cow’s milk protein assumed to be the underlying mechanism. Faecal calprotectin, a gut inflammatory marker, has been identified to be higher in infants with colic compared to those without in one study [23], although another study did not confirm this finding [24]. Another possible mechanism may be an alteration of gut microbiota in infants with cow’s milk protein allergy [25, 26].
Recent research has focussed on the pathophysiological role of gut microbiota in the exacerbation of infant crying. This promising new hypothesis is currently generating substantial research interest, with several studies confirming differences in gut microbiota between infants with and without colic. One study indicated increased concentrations of faecal Clostridium difficile in infants with colic compared to controls [27], while two studies reported increased Eschericia coli (E coli) concentrations and reduced Lactobacillus species concentrations in infants with colic compared to controls [28, 29]. Another study identified certain Lactobacillus strains to predominate in infants with colic compared to controls [30], while a more recent study suggested certain Bifidobacterium and Lactobacillus species to be protective against crying [31]. These findings suggest that while the microbiota are likely to be different in infants with colic, it remains uncertain whether these microbiota differences are the cause or result of the colic condition. Disturbances in gut microbiota may lead to mechanical changes in the gut, such as gas production and bloating and/or gut dysmotility [32, 33], which in turn lead to infant crying. The aetiology of infant colic is likely multifactorial.
Current treatment options for infant colic
Four systematic reviews have evaluated the effectiveness of interventions for infant colic [34–37]. The best evidence supports the use of hypoallergenic or extensively hydrolysed whey or casein-based formula in infants, and instigating maternal elimination diets in breastfeeding mothers, supporting the role of food allergy as a cause of persistent infant crying. However, elimination of cow’s milk from breastfeeding mothers is not always effective and it is unclear which babies respond to hypoallergenic diets and which do not. Other possible effective strategies include improved parental responsiveness, reduced stimulation and the use of sucrose. Ineffective strategies include focused parental counselling, increased carrying, use of car ride stimulators, soy milk and fibre enriched diets. Proton-pump inhibitors for presumed gastrooesophageal reflux disease are ineffective [17]. Simethicone, an anti-foaming agent used to reduce intragastrointestinal gas and bloating, is also ineffective [38, 39]. Anticholinergic drugs such as dicyclomine are effective but are associated with significant adverse effects in infants [2, 35]. Providing families with support is effective in reducing caregiver stress, but effects on crying are inconclusive [34]. There are therefore no effective and feasible strategies that can be easily implemented to help families with infants with colic.
Use of probiotics and the potential role of Lactobacillus reuteriin infant colic
One promising new approach to the management of infant colic is the use of probiotics. Probiotics are live microorganisms believed to confer health benefits and are used widely in food products, including infant formulae [40]. Probiotics colonise the bowel, competitively inhibit other bacterial adhesion, stimulate host immune responses to pathogens, suppress intestinal inflammation, increase mucus layers and strengthen mucosal barriers [41–43]. Probiotics can modulate infant gut microbiota and increase microbiota diversity [44–52]. A recent study demonstrated specific Lactobacillus strains were able to inhibit the growth of gas-producing coliforms isolated in infants with colic [32]. Probiotics and prebiotics have also been shown to alter gastrointestinal motility in newborns by stimulating gastric emptying [33]. Animal studies have shown probiotics to change pain perception mediated by the gut and inhibit gut contractile activity in rats [53–59]. Another explanation is that probiotics may reduce gut inflammation, from whatever cause, in turn reducing associated infant distress.
Four randomised controlled trials have examined the therapeutic effects of probiotics in treating infant colic. In 2007, Savino et al. reported a significant benefit in the use of Lactobacillus reuteri (L reuteri) strain ATCC 55730 in the treatment of infant colic when compared with simethicone (n = 83) [60]. This study was replicated in 2010 using L reuteri strain DSM17938 as the intervention and a placebo (n = 50), with similar promising results [61]. Both studies involved only exclusively breastfed infants whose mothers were all on cow’s milk-free diets. Two other trials using different mixtures of probiotics investigated their therapeutic effects on infant colic (n = 9, n = 62) [52, 62] and concluded there were no significant effects on crying time.
The mixed results in the above studies mean that the role of probiotics (including L reuteri) in the treatment of infant colic remains uncertain. Moreover, the findings may not necessarily be applicable to the general population since in both the Savino et al. trials, the study populations were restricted to breastfed infants whose mothers were on a cow’s milk-free diet (a select group that is not representative of the general population). Furthermore, there are methodological concerns regarding the previous studies that require further investigation. For example, the comparison group in the 2007 Savino et al. study was simethicone rather than a placebo, which meant that the interventions could not be blinded due to differences in dosage and time of administration. The other trials lacked sufficient power to detect differences and used combinations of probiotics, which can contribute to varying results since probiotic bacteria are known to have species specific effects [52, 62]. In summary, there is insufficient evidence to recommend the use of probiotics in infant colic.
Aims and hypotheses
This double-blind, placebo-controlled randomised trial aims to determine whether the probiotic L reuteri DSM 17938 benefits infants <3 months old (<13.0 weeks) with colic by reducing daily duration of infant crying/fussing. Secondary aims are whether there is reduced daily frequency of episodes of infant crying/fussing, and improved infant sleep, maternal mental health, and parent and family functioning. We also aim to investigate changes in gut microbiota, faecal calprotectin and E coli colonisation which are all possibly implicated in the mechanism of disease, and finally to determine whether probiotic use reduces healthcare costs in infant colic.
We hypothesise that, compared to the placebo (control) group, the L reuteri (intervention) group will have lower daily crying/fussing time per 24 hours at one month post randomisation. We further hypothesise that the L reuteri (intervention) group at 7, 14, 21, 28 days and 6 months post randomisation will have:
-
lower crying/fussing time per 24 hours,
-
fewer crying/fussing episodes per 24 hours,
-
longer sleep duration,
-
higher scores on a standardised measure of maternal mental health (one and six months),
-
higher scores on a standardised measure of family functioning (one and six months), and
-
higher scores on a standardised measure of parent quality adjusted life years (one and six months).
We also hypothesise that the intervention group compared to the control group will have (at one month):
-
more diverse gut microbiota,
-
lower faecal calprotectin levels, and
-
less E. coli colonisation, thereby suggesting a potential pathophysiological mechanism in infant colic.
Finally, we hypothesise that the intervention will be potentially cost-saving to the health care system by diverting families away from more expensive management such as overnight stays at mother-infant units.
Methods/Design
Study design, setting and participants
This is a phase III, double-blind, randomised placebo-controlled trial drawing on clinical and community based samples. The trial has been approved by the Royal Children’s Hospital Human Research Ethics Committee (HREC 30111).
Recruitment is from a range of services widely used by and readily accessible to parents seeking medical advice regarding their crying babies in Melbourne, Australia. These comprise: the Royal Children’s Hospital Emergency Department (RCH ED), the RCH Unsettled Babies clinic (a tertiary referral-based clinic for assessment and management of unsettled babies), Tweddle Child and Family Health Centre (a mother-infant parenting centre), two Maternal Child Health centres (universal nurse health checks in the Boroondara and Moonee Valley districts), and paediatricians at the RCH and in private practices. Interested families can also directly contact the study team to be involved.
A total sample of 160 infants less than three months (13.0 weeks) old with infant colic is being recruited between August 2011 and August 2012. The expected total duration of the study from the start of recruitment to the last subject finishing the six month follow-up is 18 months. The treatment period is one month, with a follow-up period of six months.
Inclusion criteria
Each infant must meet all of the following criteria to be enrolled in this study:
-
1.
Infant colic, i.e. crying or fussing ≥ 3 hours/day for ≥ 3 days over seven days (as defined by the modified Wessel’s criteria) by caregiver’s report at the time of study commencement;
-
2.
Less than three months (i.e. up to and excluding 13.0 weeks) old at the time of study commencement;
-
3.
Greater than 36 weeks gestation at birth; and
-
4.
Birth weight of more than 2500 g.
Exclusion criteria
Infants meeting any of the following criteria are excluded from the study:
-
1.
Failure to thrive (weight gain < 100 grams/week averaged from birth to the last recorded weight);
-
2.
Major medical problems (eg. ill, immunocompromised, major developmental or genetic abnormality);
-
3.
Taking solids, antibiotics or L reuteri and, if breastfeeding, has mother taking L reuteri at the time of study commencement;
-
4.
Cow’s milk protein allergy, defined as resolution of crying after a paediatrician-recommended two week trial of dairy-free diet in the infant, or in the mother if breast-feeding, at the time of study enrolment; and
-
5.
Caregiver has insufficient English to understand informed consent and complete questionnaires.
Randomisation
A block randomisation schedule to maintain balance between treatment arms has been prepared by an independent statistician, not directly involved in the analysis of the study results, from the Clinical Epidemiology and Biostatistics Unit (CEBU) at the RCH and supplied to Pharmacy who dispense the study product. Randomisation is stratified by method of infant feeding (breastfed versus formula-fed) and age at the time of study commencement (≤6 weeks versus >6 weeks, due to the natural crying peak occurring at around six weeks of age). Infants on a mixture of both breast- and formula-feeding are allocated to the formula-fed stratum. To minimise potential biases, the study is double-blind whereby treatment allocation is concealed from all study investigators and participants.
Treatment arms, dosage and route of administration
The intervention is L reuteri DSM 17938 (0.2x108 cfu per drop as five drops per day) in an oil suspension. Under refrigeration, it is stable for 21 months at 2°C to 8°C (as documented by the manufacturer, BioGaia AB, Stockholm, Sweden). The placebo is maltodextrose in the same oil suspension, identically packaged and stored, and has the same appearance, colour and taste as the intervention. Both intervention and placebo are labeled with only the randomisation number, batch number, expiry date, and the statement “For clinical trial use only”.
Carers administer five drops of study product orally to each infant once daily for 28 days. The dose does not need to be given at a fixed time each day, nor does it need to be given with feeds. However, for compliance and ease of administration, we recommend that families give the dose with the same feed each day.
Outcome measures
Table 1 shows the primary and secondary outcome measures at different time points of the study. Table 2 shows other information collected at different time points, including family demographics, potential confounders, physical assessments, and records of compliance and side effects.
Study procedure details
Figure 1 and Figure 2 show details of study procedures.
Recruitment
Eligible families who present through the RCH ED are identified in three ways: i) by the treating doctor, ii) by the ED social worker, or iii) through the ED electronic database. Eligible families who present through the RCH Unsettled Babies Clinic are identified by their treating doctors. Eligible families who present through the Boroondara and Moonee Valley Maternal and Child Health Nurses and Tweddle Child and Family Services are identified by their nurses or intake worker. Potentially eligible families are referred to study team members, who call families or approach them in the ED or clinic if appropriate.
The study team establishes eligibility criteria. Infants and breastfeeding mothers who are on a paediatrician-recommended dairy-free diet, infants who are taking L reuteri/solids/antibiotics, and breastfeeding mothers who are taking L reuteri at the time of study enrolment are reassessed for eligibility by telephone call after two weeks. Eligible families are approached for consent. Each family can choose to be visited at home or attend a visit at RCH for the first study visit. Study researchers call the families one day before the proposed study visit to confirm the home or RCH visit. During this call, study researchers reconfirm eligibility and consent, remind families who have not completed the consent form and baseline questionnaire to complete them, and instruct caregivers to collect a stool sample from their babies and store it in a freezer. Study researchers also record on the Clinical Record Form whether the babies are breast- or bottle-fed.
Visit one
During the visit, the researcher reconfirms eligibility, asks the mother to complete the baseline questionnaire, and reviews with the family in detail the study diary, anticipated phone calls, the procedure of administering the study product to the infant, and the anticipated procedures at the end of the study. The researcher weighs the baby, collects the stool sample and transports it back to the RCH on ice in a portable cooler, and then stores it in the laboratory −80°C freezer.
Study period Days 1 – 28
On days 1, 7, 14 and 21 the study team sends a mobile text (SMS) message to families to remind families to fill in the weekly diary. Study researchers call families on day 28 to remind families to a) stop administration of the study product; b) fill in the one month questionnaire; c) collect a stool sample; and d) make an appointment for the second (final) visit.
Visit two
During the second visit, the researcher weighs the infant, and collects a) the study diary; b) the one month questionnaire; c) the study product bottle and d) a stool sample which is transported back to the RCH on ice in a portable cooler, and then stored in the laboratory -80°C freezer.
Six month follow-up
At six months, the families are sent a letter together with a 24-hour study diary, a questionnaire and a reply-paid envelope. Caregivers are asked to complete the study diary and questionnaire, and return both in the enclosed reply-paid envelope.
Compliance with the study product
Compliance is assessed by weighing of study bottles pre- and post- dispensing, collection of faecal samples at the end of the intervention period to assess for presence of L reuteri in each infant’s stool, and weekly diary to record administering of the product.
Data analysis
Estimation of sample size
We have selected a sample size of 160 to provide 80% power to detect a minimum effect size of 0.5 standard deviations, difference in the mean daily crying time between treatment groups with a significance level of p < 0.05, allowing for a drop out rate of 20%. If the data are substantially skewed, 80% power would be maintained to detect a minimum effect size of 0.525 [63, 64]. In Savino’s trial [60], the percentage reduction in median daily crying time at day 28 compared to baseline was 70% for the probiotic and 26% for simethicone, suggesting substantive differences in this outcome are likely. With a much larger sample size (double that of Savino’s trial) in our study, we are confident we would also be able to detect a smaller difference in daily crying time reduction. Our sample size of 160 infants provides 80% power to detect a minimum effect size of 0.85 standard deviations, difference in the mean daily crying time between treatment groups within either the formula-fed or breastfed babies, assuming 40% of infants in the sample are exclusively breastfed.
We will be conducting an intention-to-treat analysis in which participants are compared according to the group to which they were randomly allocated regardless of participants' compliance, crossover to other treatments or withdrawal from the study. This approach preserves the prognostic balance in the study arms achieved by randomisation.
Baseline characteristics and study outcomes will be described for each treatment group using means and standard deviations for normally distributed continuous outcomes, while medians and inter-quartile ranges will be used for continuous outcomes that are skewed. Proportions for categorical data will be given. All primary and secondary outcomes for the intervention versus control groups will be compared with t tests and non-parametric tests for continuous data, and chi squared tests for dichotomous data. The primary outcome is the crying time/24 hours at day 28. We will additionally consider a dichotomised indicator of treatment response defined as a 50% reduction in crying time. Subgroup analyses are intended a priori to examine treatment differences amongst breastfed babies and those who are formula-fed, and amongst infants with a family history of atopy and those without.
Regression models will be used to estimate treatment effect sizes, odds ratios and 95% confidence interval, adjusting for potential confounding factors identified a priori and measured at baseline. These include infant age (≤6 weeks versus >6 weeks, taking into account the natural course of infant colic symptomatology with the peak of crying at six weeks), mode of birth delivery, maternal smoking, use of antibiotics or probiotics in infants and breastfeeding mothers, maternal diet if breastfeeding, maternal mental health scores, and known causes of crying (e.g. fever, eczema, vaccination, vomiting, and diarrhoea). Random effects regression models will be used for further longitudinal analysis examining trends in crying time within individual babies.
Discussion
Infant colic is common, distressing, impacts adversely on maternal mental health, and is a risk factor for shaken baby syndrome. An effective, practical and acceptable intervention for infant colic would represent a major clinical and public health advance. As our trial will include breast and formula-fed babies, regardless of maternal diet, our results can be generalised to most babies presenting with colic. If cost-effective, the simplicity of the intervention is such that it could be widely taken up as a new standard of care in the primary and secondary care sectors.
With the boom of probiotic products appearing on the market, the use of probiotics in the community is becoming more widespread. It is therefore important to provide sufficient sound scientific evidence for its effectiveness in infant colic before it becomes incorporated into regular use by the community, and avoid unnecessary consumption of costly products if the intervention is not found to be effective.
Authors’ information
VS is a paediatrician and is undertaking a PhD in the area of infant colic. HH and MW are her supervisors.
Abbreviations
- L reuteri :
-
Lactobacillus reuteri
- E coli :
-
Eschericia coli
- RCH:
-
Royal Children’s Hospital
- ED:
-
Emergency Department
- CEBU:
-
Clinical Epidemiology and Biostatistics Unit
- cfu:
-
Colony forming units
- SMS:
-
Short message service
- mins:
-
Minutes
- ml:
-
Milliliter
- kg:
-
Kilogram
- mg:
-
Milligram.
References
Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC: Paroxysmal fussing in infancy, sometimes called "colic". Pediatrics. 1954, 14: 421-434.
Lucassen PL, Assendelft WJ, van Eijk JT, Gubbels JW, Douwes AC, van Geldrop WJ: Systematic review of the occurrence of infantile colic in the community. Arch Dis Child. 2001, 84: 398-403. 10.1136/adc.84.5.398.
Wake M, Morton-Allen E, Poulakis Z, Hiscock H, Gallagher S, Oberklaid F: Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: prospective community-based study. Pediatrics. 2006, 117: 836-842. 10.1542/peds.2005-0775.
Morris S, James-Roberts IS, Sleep J, Gillham P: Economic evaluation of strategies for managing crying and sleeping problems. Arch Dis Child. 2001, 84: 15-19. 10.1136/adc.84.1.15.
McMahon C, Barnett B, Kowalenko N, Tennant C, Don N: Postnatal depression, anxiety and unsettled infant behaviour. Aust N Z J Psychiatry. 2001, 35: 581-588. 10.1080/0004867010060505.
Smart J, Hiscock H: Early infant crying and sleeping problems: a pilot study of impact on parental well-being and parent-endorsed strategies for management. J Paediatr Child Health. 2007, 43: 284-290. 10.1111/j.1440-1754.2007.01060.x.
Barr RG, Trent RB, Cross J: Age-related incidence curve of hospitalized Shaken Baby Syndrome cases: convergent evidence for crying as a trigger to shaking.[see comment]. Child Abuse Negl. 2006, 30: 7-16. 10.1016/j.chiabu.2005.06.009.
Lee C, Barr RG, Catherine N, Wicks A: Age-related incidence of publicly reported shaken baby syndrome cases: is crying a trigger for shaking?. J Dev Behav Pediatr. 2007, 28: 288-293. 10.1097/DBP.0b013e3180327b55.
Savino F, Castagno E, Bretto R, Brondello C, Palumeri E, Oggero R: A prospective 10-year study on children who had severe infantile colic. Acta Paediatr Suppl. 2005, 94: 129-132. 10.1080/08035320510043691.
Wolke D, Rizzo P, Woods S: Persistent infant crying and hyperactivity problems in middle childhood. Pediatrics. 2002, 109: 1054-1060. 10.1542/peds.109.6.1054.
Brown M, Heine RG, Jordan B: Health and well-being in school-age children following persistent crying in infancy. J Paediatr Child Health. 2009, 45: 254-262. 10.1111/j.1440-1754.2009.01487.x.
Rautava P, Lehtonen L, Helenius H: Infantile colic: child and family three years later. Pediatrics. 1995, 96: 43-47.
Hiscock H, Jordan B: Problem crying in infancy. Med J Aust. 2004, 181: 507-512.
Gupta SK: Is colic a gastrointestinal disorder?. Curr Opin Pediatr. 2002, 14: 588-592. 10.1097/00008480-200210000-00005.
Geertsma MA, Hyams JS: Colic–a pain syndrome of infancy?. Pediatr Clin North Am. 1989, 36: 905-919.
Jordan B, Heine RG, Meehan M, Catto-Smith AG, Lubitz L: Effect of antireflux medication, placebo and infant mental health intervention on persistent crying: a randomized clinical trial. J Paediatr Child Health. 2006, 42: 49-58. 10.1111/j.1440-1754.2006.00786.x.
Moore DJ, Tao BS, Lines DR, Hirte C, Heddle ML, Davidson GP: Double-blind placebo-controlled trial of omeprazole in irritable infants with gastroesophageal reflux. J Pediatr. 2003, 143: 219-223. 10.1067/S0022-3476(03)00207-5.
Hill DJ, Roy N, Heine RG, Hosking CS, Francis DE, Brown J, Speirs B, Sadowsky J, Carlin JB: Effect of a low-allergen maternal diet on colic among breastfed infants: a randomized, controlled trial. Pediatrics. 2005, 116: e709-e715. 10.1542/peds.2005-0147.
Lucassen PL, Assendelft WJ, Gubbels JW, van Eijk JT, Douwes AC: Infantile colic: crying time reduction with a whey hydrolysate: A double-blind, randomized, placebo-controlled trial. Pediatrics. 2000, 106: 1349-1354. 10.1542/peds.106.6.1349.
Jakobsson I, Lothe L, Ley D, Borschel MW: Effectiveness of casein hydrolysate feedings in infants with colic. Acta Paediatr. 2000, 89: 18-21. 10.1111/j.1651-2227.2000.tb01180.x.
Jakobsson I, Lindberg T: Cow's milk proteins cause infantile colic in breast-fed infants: a double-blind crossover study. Pediatrics. 1983, 71: 268-271.
Hill DJ, Hudson IL, Sheffield LJ, Shelton MJ, Menahem S, Hosking CS: A low allergen diet is a significant intervention in infantile colic: results of a community-based study. J Allergy Clin Immunol. 1995, 96: 886-892. 10.1016/S0091-6749(95)70224-5.
Rhoads JM, Fatheree NY, Norori J, Liu Y, Lucke JF, Tyson JE, Ferris MJ: Altered fecal microflora and increased fecal calprotectin in infants with colic. J Pediatr. 2009, 155: 823-828. 10.1016/j.jpeds.2009.05.012. e821
Olafsdottir E, Aksnes L, Fluge G, Berstad A: Faecal calprotectin levels in infants with infantile colic, healthy infants, children with inflammatory bowel disease, children with recurrent abdominal pain and healthy children. Acta Paediatr. 2002, 91: 45-50. 10.1111/j.1651-2227.2002.tb01638.x.
Thompson-Chagoyan OC, Vieites JM, Maldonado J, Edwards C, Gil A: Changes in faecal microbiota of infants with cow's milk protein allergy - A Spanish prospective case–control 6-month follow-up study. Pediatr Allergy Immunol. 2010, 21: e394-e400. 10.1111/j.1399-3038.2009.00961.x.
Thompson-Chagoyan OC, Fallani M, Maldonado J, Vieites JM, Khanna S, Edwards C, Dore J, Gil A: Faecal microbiota and short-chain fatty acid levels in faeces from infants with cow's milk protein allergy. Int Arch Allergy Immunol. 2011, 156: 325-332. 10.1159/000323893.
Lehtonen L, Korvenranta H, Eerola E: Intestinal microflora in colicky and noncolicky infants: bacterial cultures and gas–liquid chromatography. J Pediatr Gastroenterol Nutr. 1994, 19: 310-314. 10.1097/00005176-199410000-00009.
Savino F, Cordisco L, Tarasco V, Calabrese R, Palumeri E: Matteuzz iD: Molecular identification of coliform bacteria from colicky breastfed infants. Acta Paediatrica, International Journal of Paediatrics. 2009, 98: 1582-1588. 10.1111/j.1651-2227.2009.01419.x.
Savino F, Cresi F, Pautasso S, Palumeri E, Tullio V, Roana J, Silvestro L, Oggero R: Intestinal microflora in breastfed colicky and non-colicky infants. Acta Paediatr. 2004, 93: 825-829. 10.1111/j.1651-2227.2004.tb03025.x.
Savino F, Bailo E, Oggero R, Tullio V, Roana J, Carlone N, Cuffini AM, Silvestro L: Bacterial counts of intestinal Lactobacillus species in infants with colic. Pediatr Allergy Immunol. 2005, 16: 72-75. 10.1111/j.1399-3038.2005.00207.x.
Partty AKM, Endo A, Salminen S, Isolauri E: Compositional development of Bifidobacterium and Lactobacillus microbiota is linked with crying and fussing in early infancy. PLoS One. 2012, 7: e32495-10.1371/journal.pone.0032495. 1-5
Savino F, Cordisco L, Tarasco V, Locatelli E, Di Gioia D, Oggero R, Matteuzzi D: Antagonistic effect of Lactobacillus strains against gas-producing coliforms isolated from colicky infants. BMC Microbiol. 2011, 11: 157-10.1186/1471-2180-11-157.
Indrio F, Riezzo G, Raimondi F, Bisceglia M, Cavallo L, Francavilla R: Effects of probiotic and prebiotic on gastrointestinal motility in newborns. J Physiol Pharmacol. 2009, 60 (Suppl 6): 27-31.
Cohen-Silver J, Ratnapalan S: Management of infantile colic: a review. Clin Pediatr. 2009, 48: 14-17.
Garrison MM, Christakis DA: A systematic review of treatments for infant colic.[see comment]. Pediatrics. 2000, 106: 184-190.
Lucassen PL, Assendelft WJ: Systematic review of treatments for infant colic. Pediatrics. 2001, 108: 1047-1048. 10.1542/peds.108.4.1047.
Wade S, Kilgour T: Extracts from "clinical evidence": Infantile colic. BMJ. 2001, 323: 437-440. 10.1136/bmj.323.7310.437.
Metcalf TJ, Irons TG, Sher LD, Young PC: Simethicone in the treatment of infant colic: A randomized, placebo- controlled, multicenter trial. Pediatrics. 1994, 94: 29-34.
Danielsson B, Hwang CP: Treatment of infantile colic with surface active substance (simethicone). Acta Paediatr Scand. 1985, 74: 446-450. 10.1111/j.1651-2227.1985.tb11001.x.
Wallace B: Clinical use of probiotics in the pediatric population. Nutr Clin Pract. 2009, 24: 50-59. 10.1177/0884533608329298.
Cabana MD, Shane AL, Chao C, Oliva-Hemker M: Probiotics in primary care pediatrics. Clin Pediatr. 2006, 45: 405-410. 10.1177/0009922806289614.
Thomas DW, Greer FR: Probiotics and prebiotics in pediatrics. Pediatrics. 2010, 126: 1217-1231. 10.1542/peds.2010-2548.
Penna FJ, Peret LA, Vieira LQ, Nicoli JR: Probiotics and mucosal barrier in children. Curr Opin Clin Nutr Metab Care. 2008, 11: 640-644. 10.1097/MCO.0b013e32830a70ab.
Abrahamsson TR, Sinkiewicz G, Jakobsson T, Fredrikson M, Bjorksten B: Probiotic lactobacilli in breast milk and infant stool in relation to oral intake during the first year of life. J Pediatr Gastroenterol Nutr. 2009, 49: 349-354. 10.1097/MPG.0b013e31818f091b.
Lahtinen SJ, Boyle RJ, Kivivuori S, Oppedisano F, Smith KR, Robins-Browne R, Salminen SJ, Tang MLK: Prenatal probiotic administration can influence Bifidobacterium microbiota development in infants at high risk of allergy. J Allergy Clin Immunol. 2009, 123: 499-501. 10.1016/j.jaci.2008.11.034.
Spinelli M, Bastelli A, Capretti MG, Mariani E, Corvaglia L, Tripapalli E, Faldella G: Efficacy of oral supplementation with Lactobacillus reuteri in infants weighing less than 1500g in modifying the intestinal colonisation by Gram-negative bacteria. 28th National congress of antibiotic therapy in paediatrics. 2009, Milan, Italy
Ren YF, Wang LL: Effects of probiotics on intestinal bacterial colonization in premature infants. Chinese Journal of Contemporary Pediatrics. 2010, 12: 192-194.
Mah KW, Chin VI, Wong WS, Lay C, Tannock GW, Shek LP, Aw MM, Chua KY, Wong HB, Panchalingham A, Lee BW: Effect of a milk formula containing probiotics on the fecal microbiota of asian infants at risk of atopic diseases. Pediatr Res. 2007, 62: 674-679. 10.1203/PDR.0b013e31815991d5.
Lee SJ, Cho SJ, Park EA: Effects of probiotics on enteric flora and feeding tolerance in preterm infants. Neonatology. 2007, 91: 174-179. 10.1159/000097449.
Mohan R, Koebnick C, Schildt J, Schmidt S, Mueller M, Possner M, Radke M, Blaut M: Effects of Bifidobacterium lactis Bb12 supplementation on intestinal microbiota of preterm infants: A double-blind, placebo-controlled, randomized study. J Clin Microbiol. 2006, 44: 4025-4031. 10.1128/JCM.00767-06.
Akiyama K, Hosono S, Takahashi E, Ishizeki S, Takigawa I, Imura S, Yamauchi K, Yaeshima T, Hayasawa H, Shimamura S: Effects of oral administration of Bifidobacterium breve on development of intestinal microflora in extremely premature infants. Acta Neonatologica Japonica. 1994, 30: 130-137.
Mentula S, Tuure T, Koskenala R, Korpela R, Kononen E: Microbial composition and fecal fermentation end products from colicky infants - a probiotic supplementation pilot. Microbial Ecology in Health and Disease. 2008, 20: 37-47. 10.1080/08910600801933846.
Kamiya T, Wang L, Forsythe P, Goettsche G, Mao Y, Wang Y, Tougas G, Bienenstock J: Inhibitory effects of Lactobacillus reuteri on visceral pain induced by colorectal distension in Sprague–Dawley rats. Gut. 2006, 55: 191-196. 10.1136/gut.2005.070987.
Lutgendorff F, Akkermans LM, Soderholm JD: The role of microbiota and probiotics in stress-induced gastro-intestinal damage. Curr Mol Med. 2008, 8: 282-298. 10.2174/156652408784533779.
Ma X, Mao Y-K, Wang B, Huizinga JD, Bienenstock J, Kunze W: Lactobacillus reuteri ingestion prevents hyperexcitability of colonic DRG neurons induced by noxious stimuli. Am J Physiol Gastrointest Liver Physiol. 2009, 296: G868-G875. 10.1152/ajpgi.90511.2008.
Rousseaux C, Thuru X, Gelot A, Barnich N, Neut C, Dubuquoy L, Dubuquoy C, Merour E, Geboes K, Chamaillard M, et al: Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med. 2007, 13: 35-37. 10.1038/nm1521.
Wang B, Mao YK, Diorio C, Wang L, Huizinga JD, Bienenstock J, Kunze W: Lactobacillus reuteri ingestion and IK(Ca) channel blockade have similar effects on rat colon motility and myenteric neurones. Neurogastroenterol Motil. 2010, 22: 98-107.
Wang L, Ham H, Bienenstock J: Differential effects of two probiotic strains on pain perception of gastric and colonic distension in sprague dawley rats. Gastroenterology. 2009, 136: A771-Conference:Digestive Disease Week
Kunze WA, Mao YK, Wang B, Huizinga JD, Ma X, Forsythe P, Bienenstock J, Kunze WA, Mao Y-K, Wang B, et al: Lactobacillus reuteri enhances excitability of colonic AH neurons by inhibiting calcium-dependent potassium channel opening. J Cell Mol Med. 2009, 13: 2261-2270. 10.1111/j.1582-4934.2009.00686.x.
Savino F, Pelle E, Palumeri E, Oggero R, Miniero R: Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Pediatrics. 2007, 119: e124-e130. 10.1542/peds.2006-1222.
Savino F, Cordisco L, Tarasco V, Palumeri E, Calabrese R, Oggero R, Roos S, Matteuzzi D: Lactobacillus reuteri DSM 17 938 in Infantile Colic: A Randomized, Double-Blind, Placebo-Controlled Trial. Pediatrics. 2010, 126: e526-e533. 10.1542/peds.2010-0433.
Dupont C, Rivero M, Grillon C, Belaroussi N, Kalindjian A: Marin V: alpha-Lactalbumin-enriched and probiotic supplemented infant formula in infants with colic: growth and gastrointestinal tolerance. Eur J Clin Nutr. 2010, 64: 767-
GraphPad Statistics Guide: Sample size for nonparametric tests. http://www.graphpad.com/guides/prism/6/statistics/index.htm?stat_sample_size_for_nonparametric_.htmAccessed 13th August 2012
Lehmann E: Nonparametrics: Statistical Methods Based on Ranks, Revised. 1998
Barr RG, Kramer MS, Leduc DG, Boisjoly C, McVey-White L, Pless IB: Parental diary of infant cry and fuss behavior. Arch Dis Child. 1988, 63: 380-387. 10.1136/adc.63.4.380.
Barr RG, Kramer MS, Pless IB, Boisjoly C, Leduc D: Feeding and temperament as determinants of early infant crying/fussing behavior. Pediatrics. 1989, 84: 514-521.
Hunziker UA, Barr RG: Increased carrying reduces infant crying: a randomized controlled trial. Pediatrics. 1986, 77: 641-648.
Cox JL, Holden JM, Sagovski R: Detection of postnatal depression: development of a 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987, 150: 1172-1175.
Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P: The PedsQLTM Family Impact Module: Preliminary reliability and validity. Health Qual Life Outcomes. 2004, 2: 1-6. 10.1186/1477-7525-2-1.
Varni JW, Burwinkle TM, Seid M, Skarr D: The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003, 3: 329-341. 10.1367/1539-4409(2003)003<0329:TPAAPP>2.0.CO;2.
Hawthorne G, Richardson J: Atherton Day M: A comparison of the Assessment of Quality of LIfe (AQoL) with four other generic utility instruments. Ann Med. 2001, 33: 358-370. 10.3109/07853890109002090.
Osborne CA, Rees GN, Bernstein Y, Janssen PH: New threshold and confidence estimates for terminal restriction fragment length polymorphism analysis of complex bacterial communities. Appl Environ Microbiol. 2006, 72: 1270-1278. 10.1128/AEM.72.2.1270-1278.2006.
CALPRO: CalproLab ELISA kit. http://www.calpro.no/uploads/pdf/110831_CalproLab%20ALP%20ELISA.pdf Accessed 14th August 2012. 2012
Chern EC, Siefring S, Paar J, Doolittle M, Haugland RA: Comparison of quantitative PCR assays for Escherichia coli targeting ribosomal RNA and single copy genes. Lett Appl Microbiol. 2011, 52: 298-306. 10.1111/j.1472-765X.2010.03001.x.
Orenstein SR, Cohn JF, Shalaby TM, Kartan R: Reliability and validity of an infant gastroesophageal reflux questionnaire. Clin Pediatr. 1993, 32: 472-484. 10.1177/000992289303200806.
Kleinman L, Rothman M, Strauss R, Orenstein SR, Nelson S, Vandenplas Y, Cucchiara S, Revicki DA: The Infant Gastroesophageal Reflux Questionnaire Revised: development and validation as an evaluative instrument. Clin Gastroenterol Hepatol. 2006, 4: 588-596. 10.1016/j.cgh.2006.02.016.
Million MMM, Henry M, Armougom F, Richet H, Carrieri P, Valero R, Raccah D: Vialettes B, Raoult D: Obesity-associated gut microbiota is enriched in Lactobacillus reuteri and depleted in Bifidobacterium animalis and Methanobrevibacter smithii. Int J Obes (Lond). 2012, 36: 817-825. 10.1038/ijo.2011.153.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/12/135/prepub
Acknowledgements
The trial is funded by the Equitee Trustees Georgina Menzies Maconcachie Charitable Trust and Australian National Health and Medical Research Council (NHMRC) Postgraduate Scholarship 607447, and part-supported by the Centre for Community Child Health at the Royal Children’s Hospital. Murdoch Childrens Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. HH and MW are supported by NHMRC Population Health Career Development Awards (Grants 607351 and 546405). FM is supported by the NHMRC Population Health Capacity Building Grant 436914 and Early Career Fellowship 1037449. The investigational product and placebo are supplied and manufactured by BioGaia. Calpro AS supplied the CalproLab ELISA kits for the analysis of calprotectin levels. BioGaia, Calpro AS and Equitee Trustees are all independent of the study. BioGaia, Calpro AS and Equitee Trustees played no role in the trial’s design, in the collection, analysis, and interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication. We thank all families, maternal and child health nurses, doctors, paediatricians and research assistants (EY, Jane Sheehan, Saga Arthursson) who are taking part in the trial.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors declare that they and their spouses, partners or children have no financial and non-financial relationships or interests that may be relevant to the submitted work. The authors declare they have no competing interests.
Authors’ contributions
VS, HH and MW conceived the Baby Biotics trial with MT, RH and FM. VS is the Project Manager and takes overall responsibility for all aspects of the trial and this manuscript. EY is the Research Assistant. VS, HH and MW designed the intervention, with advice from MT, RH and RGB, who also advised on measures and their interpretation. FM advised on statistical issues. AS contributed to recruitment procedures. All authors contributed to, read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sung, V., Hiscock, H., Tang, M. et al. Probiotics to improve outcomes of colic in the community: Protocol for the Baby Biotics randomised controlled trial. BMC Pediatr 12, 135 (2012). https://doi.org/10.1186/1471-2431-12-135
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-12-135