Abstract
Background
There are at least 51 adenovirus serotypes (AdV) known to cause human infections. The prevalence of the different human AdV (HAdV) serotypes varies among different regions. Presently, there are no reports of the prevalent HAdV types found in Malaysia. The present study was undertaken to identify the HAdV types associated primarily with respiratory tract infections (RTI) of young children in Malaysia.
Methods
Archived HAdV isolates from pediatric patients with RTI seen at the University of Malaya Medical Center (UMMC), Kuala Lumpur, Malaysia from 1999 to 2005 were used. Virus isolates were inoculated into cell culture and DNA was extracted when cells showed significant cytopathic effects. AdV partial hexon gene was amplified and the sequences together with other known HAdV hexon gene sequences were used to build phylogenetic trees. Identification of HAdV types found among young children in Malaysia was inferred from the phylograms.
Results
At least 2,583 pediatric patients with RTI sought consultation and treatment at the UMMC from 1999 to 2005. Among these patients, 48 (< 2%) were positive for HAdV infections. Twenty-seven isolates were recovered and used for the present study. Nineteen of the 27 (~70%) isolates belonged to HAdV species C (HAdV-C) and six (~22%) were of HAdV species B (HAdV-B). Among the HAdV-C species, 14 (~74%) of them were identified as HAdV type 1 (HAdV-1) and HAdV type 2 (HAdV-2), and among the HAdV-B species, HAdV type 3 (HAdV-3) was the most common serotype identified. HAdV-C species also was isolated from throat and rectal swabs of children with hand, foot, and mouth disease (HFMD). Two isolates were identified as corresponding to HAdV-F species from a child with HFMD and a patient with intestinal obstruction.
Conclusions
HAdV-1 and HAdV-2 were the most common HAdV isolated from pediatric patients who sought treatment for RTI at the UMMC from 1999 to 2005. HAdV-B, mainly HAdV-3, was recovered from ~22% of the patients. These findings provide a benchmark for future studies on the prevalence and epidemiology of HAdV types in Malaysia and in the region.
Similar content being viewed by others
Background
Respiratory tract infections (RTI) are common in adults and children worldwide. The disease varies in severity, presenting as uncomplicated, subacute, acute and chronic infection. RTIs can be life threatening depending on the causative agent and host condition. In children, a high incidence of RTI is caused either by: 1) heightened exposure of young children to RTI infectious agents from siblings, friends, and child care; 2) environmental factors; and 3) inherited disorders of the immune system [1]. In industrialized and developed countries, nearly 50% of pediatric consultations are RTI related [2, 3], and at least 1.9 million children died from acute RTI with 70% of them in Africa and Asia in 2000 [4].
There are a number of infectious agents that cause RTI. Bacteria, such as Haemophilus influenzae, Streptococcus pneumoniae, Escherichia coli, Klebsiella pneumoniae, Mycoplasma pneumonia, and Chlamydia trachomatis are among the most common. However, 80%-90% RTI are caused by viruses, such as respiratory syncytial virus (RSV), influenza virus, parainfluenza virus, and adenovirus (AdV) [1, 5]. RSV is one of the most common agents of RTI in infants and young children in many countries. It is estimated to cause ~39% of all pneumonia cases and up to 6% of pneumonia-associated deaths [6]. Parainfluenza virus and influenza virus also are commonly isolated viruses from children with viral RTI.
HAdV-associated RTI is reportedly low. It accounts for 4%-10% cases of pneumonia, 2%-10% cases of bronchiolitis, and 3%-9% cases of croup [7]. Severity of infection associated with HAdV varies with the different HAdV serotypes [7–9]. There are at least 51 immunologically distinct HAdV types classified into six species, designated A to F [10]. Viruses causing RTI are usually isolated in the laboratory from patients' nasal secretions and serotyped by immunological typing methods [11–13]. In recent years, molecular identification of the virus has become more common, where distinction of the virus types can be made through specific genomic sequence amplification by polymerase chain reaction (PCR) and determination of the partial hexon gene sequence [14, 15]. Presently, there is no report of the prevalent HAdV types causing infections among Malaysians. This could be due to the low infection and fatality rates of the infection resulting in limited interest in typing the virus. The present study was undertaken to type HAdV of pediatric patients younger than 5 years seen at the University of Malaya Medical Center (UMMC), Kuala Lumpur, Malaysia.
Methods
Virus
Twenty-seven archived HAdV isolates were recovered from the UMMC virology repository and used for the study. The isolates were derived mainly from the nasopharyngeal secretions (NPS) of children younger than 5 years diagnosed with RTI (Table 1). Virus isolation and propagation were performed using African green monkey kidney cells (Vero), human lung carcinoma cells (A549), and dog kidney cells (MDCK). The presence of HAdV was detected by immunofluorescence staining using specific antibodies (Cat. No. 5000; Light Diagnostics Inc., Salt Lake City, UT, USA) following manifestation of cytopathic effects. Virus inoculum was prepared and kept at -70°C until needed for genomic typing. Further maintenance and propagation of the HAdV isolates were performed in A549 cells.
PCR amplification and genome sequencing
Viral genomic DNA was extracted using Tri Reagent® (Molecular Research Center Inc., Cincinnati, OH, USA) following the manufacturer's protocol. The partial hexon gene was amplified using the primer pair, AdTU7 (5'-GCCACCTTCTTCCCCATGGC-3') and AdTU4 (5'-GTAGCGTTGCCGGCCGAGAA-3') to amplify a 1,001 bp fragment of the partial hexon gene (position 20,733 - 21,734; Accession # NC_001405). A nested polymerase chain reaction (PCR) also was performed on the amplified fragment using the primers, AdU-S (5'-TTCCCCATGGCNCACAACAC-3') and AdU-A (5'-GCCTCGATGACGCCGCGGTG-3') which resulted in a 956 bp fragment. Amplification was performed for 36 cycles consisting of a denaturation step at 94°C for 1 min, an annealing step at 50°C for 1 min, and an extension step at 72°C for 2 min. The extension was continued at 72°C for 7 min. The amplified DNA fragment was separated in 1.5% agarose gel (Promega, Madison, WI, USA), and purified using QIA Quick gel extraction system (Qiagen GmbH, Hilden, Germany) according to the manufacturer's protocol. The DNA fragments were sequenced at Macrogen Inc. (Seoul, Korea).
Sequence and phylogenetic analysis
The partial hexon gene sequences were aligned and phylogenetic trees were drawn as previously described [16]. Briefly, the HAdV partial hexon gene sequences were analyzed using Sequencher 4.6 (Gene Codes Corporation, Ann Arbor, MI) and aligned against other available AdV sequences using ClustalX [17]. Phylogenetic trees were drawn using the maximum-likelihood method as implemented in PHYLIP 3.67 [18] and the maximum-parsimony method using MEGA4 [19]. Bootstrap values were obtained from a random sampling of 100 replicates. Reference HAdV sequences used to build the phylogenetic trees were obtained from the GenBank. Details on the reference sequences are shown in Table 2.
The study was approved by the University Malaya Medical Centre Ethics Committee (Approval #794.6).
Results
A total of 2,583 pediatric patients with RTI were treated at the UMMC from 1999 to 2005. Of these patients, 48 (<2%) were positive for HAdV by either direct immunofluorescence staining of the patient's NPS, PCR amplification, or virus isolation. HAdV also was isolated from the throats of patients with HFMD. These HFMD patients usually did not present with RTI symptoms, but throat swabs were routinely collected in addition to rectal swabs.
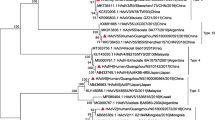
In the present study, the partial hexon gene sequences (nucleotide 20,734-21,737) of 27 HAdV isolates from UMMC were determined. The sequences were aligned and phylogenetic trees were drawn using the maximum-likelihood and maximum-parsimony methods. Only results from the maximum-likelihood method were presented, as trees drawn from both the methods were similar. The nucleotide sequence alignment clustered the UMMC isolates into HAdV-C species (n = 19), HAdV-B species (n = 6), and HAdV-F species (n = 2) with high bootstrap values. Within the HAdV-C species, eight isolates were HAdV-2 (42%); six isolates, HAdV-1 (32%); four isolates, HAdV-5 (21%);, and one isolate, HAdV-6 (5%; Figure 1a). When compared with other HAdV from the GenBank, most of the UMMC HAdV-5 and HAdV-2 isolates formed a separate subcluster of their own (Figure 1a). Within HAdV-B species, five isolates grouped into HAdV-3, and one was HAdV-7 (Figure 1b). HAdV-3 isolates from the study formed a separate subcluster together with an isolate from Guangzhou, China (Accession # AY878716) distinct from other known HAdV-3. This raised the possibility that the viruses may share a common ancestral lineage with the Malaysian isolate that was isolated in 1999. The HAdV-7 clustered together with isolates from the East Asian countries suggesting a possible widespread presence of the virus in the East Asian region. Four of the HAdV isolates sequenced in the study were from HFMD patients, and three of them clustered together with the HAdV-C species. One isolate clustered with known HAdV-40, whereas an isolate from the rectal swab of a patient diagnosed with intestinal obstruction clustered with known HAdV-41. No HAdV-B genotype previously associated with fatal cases of HFMD [20, 21] was detected in any of the HFMD patient samples. Isolates from HFMD patients were included in the study initially because no effort was made to discriminate the samples from those strictly with RTI. Patients with HFMD normally would not present with RTI symptoms.
Molecular typing of human adenoviruses (HAdV) isolated at the University of Malaya Medical Center (UMMC) from 1999 to 2005. HAdV-1 and HAdV-2 comprised most of the HAdV-C species isolated at the UMMC (a). HAdV-B species consisted of HAdV-3 and HAdV-7. HAdV-3 formed its own distinct cluster separate from the rest of the group (b). Two isolates from the study were grouped as HAdV-F serotype 40 and 41 (c), commonly implicated in gastroenteritis.
Discussion
Human adenovirus is most commonly associated with respiratory illnesses. However, depending on the infecting serotype, the virus also causes various other illnesses, including gastroenteritis, conjunctivitis, cystitis, and non- specific exanthemas [13, 22]. Symptoms of the respiratory illness associated with HAdV range from mild infection to severe pneumonia [8, 23]. Young children and immunocompromised patients are especially vulnerable to severe complications of HAdV infection [24, 25]. The findings that less that 2% of UMMC pediatric RTI is associated with HAdV respiratory infection is consistent with other reports that HAdV-associated respiratory infection is usually low in comparison to other viruses, such as RSV and parainfluenza virus. The infection also is generally milder and rarely leads to severe complications and deaths [8, 26]. The low number of HAdV isolation among pediatric patients seen at the UMMC also suggests that the virus is not associated with any major RTI outbreaks during the period from 1999 to 2005. This is perhaps among the reasons why there have not been many efforts to identify the HAdV species and types in children with RTI in many countries, including Malaysia. In addition, the low incidence of RTI caused by HAdV in the community hampered the effort to get enough representative isolates.
In our study, HAdV partial hexon gene sequences were used to type the different HAdV isolates. This gene region contains the hypervariable region that confers HAdV serotype specificity. Using this molecular typing method, HAdV-C species, specifically type 1 and 2, were the most common HAdV isolated from the pediatric patients seen at UMMC from 1999 to 2005. In contrast, studies done in the United States of America, United Kingdom, Korea, and China, showed HAdV-B species as the most commonly isolated HAdV [27–30]. The reasons for the marked differences are not known. It could be that HAdV-C is more common in the region in comparison to the more developed countries. However, the prevalence of HAdV-C species in the neighboring countries could not be compared because information from these countries are lacking.
Overrepresentation of HAdV-C in UMMC pediatric patients could suggest a high prevalence of the virus in the community. There are reports that the virus could persist and cause asymptomatic latent infection in rabbits for as long as one year [31]. HAdV-C serotypes 1, 2, and 5 are the most common serotype of HAdV associated in latent infection of tonsils and adenoids of humans, which at times cause RTI in young children [32]. The prolonged presence of the virus in infected children increases its transmissibility, and this could contribute to the persistence of the virus of young children in Malaysia. The ubiquitous presence of the virus also could help explain isolation of the virus from patients with HFMD and nonspecific viral fever. On the other hand, the results also could reflect the higher tendency of children with HAdV-C species infection to seek medical attention, hence suggesting that the virus could cause more severe manifestations of RTI. Further studies, however, will be needed to verify this.
Conclusions
The present study is the first to report the prevalent and circulating HAdV types in Malaysia. It showed that HAdV-C species especially HAdV-1 and HAdV-2 were the most commonly isolated HAdV among pediatric patients seen at UMMC from 1999 to 2005, followed by HAdV-B species type 3. These viruses are common serotypes of HAdV causing acute RTI in pediatric patients. Because no such study has ever been reported in Malaysia, the present study provides a benchmark for future studies of HAdV infection in the country.
Abbreviations
- HAdV:
-
human adenovirus
- HFMD:
-
hand, foot and mouth disease
- NPS:
-
nasopharyngeal secretion
- RTI:
-
respiratory tract infection
- UMMC:
-
University of Malaya Medical Center.
References
Schaad UB: Prevention of paediatric respiratory tract infections: emphasis on the role of OM-85. Eur Respir Rev. 2005, 14: 74-77. 10.1183/09059180.05.00009506.
Eggenberger K: Respiratory tract infections most frequently seen in pediatric outpatient care. Ars Medici. 1993, 83: 24-40.
Kvaerner KJ, Nafstad P, Jaakkola JJ: Upper respiratory morbidity in preschool children: a cross sectional study. Arch Otolaryngol Head Neck Surg. 2000, 126: 1201-1206.
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C: Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002, 2: 25-32. 10.1016/S1473-3099(01)00170-0.
Bakir TMF, Halawani M, Ramia S: Viral aetiology and epidemiology of acute respiratory infections in hospitalized Saudi children. J Trop Pediatrics. 1988, 44: 100-103. 10.1093/tropej/44.2.100.
Weber MW, Mulholland EK, Greenwood BM: Respiratory syncytial virus infection in tropical and developing countries. Trop Med International Health. 1998, 3: 268-280. 10.1046/j.1365-3156.1998.00213.x.
Cherry JD: Adenoviruses. Textbook of Pediatric Infectious Diseases. Edited by: Feigin RD, Cherry JD. 1998, Philadelphia: WB Saunders, 1666-1684. 4
Schmitz H, Wigand R, Heinrich W: Worldwide epidemiology of human adenovirus infections. Am J Epidemiol. 1983, 117: 455-466.
Larranaga C, Kajon A, Villagra E, Avendano LF: Adenovirus surveillance on children hospitalized for acute lower respiratory infections in Chile (1988-1996). J Med Virol. 2000, 60: 342-346. 10.1002/(SICI)1096-9071(200003)60:3<342::AID-JMV14>3.0.CO;2-0.
Shenk T, Horwitz MS: Adenoviridae: the viruses and their replication. Fields Virology. Edited by: Fields BN, Knipe DM, Howley PM. 2001, Philadelphia: Lippincott-Raven Publishers, 2265-2326. 4
Hierholzer JC: Adenoviruses. Diagnostic Procedures for Viral, Rickettsial and Chlamydial Infections. Edited by: Lennette EH, Lennette DA, Lennette ET. 1995, Washington DC: American Public Health Association, 169-188. 7
Hierholzer JC: Further subgrouping of the human adenoviruses by differential agglutination. J Infect Dis. 1973, 128: 541-550.
Wadell G: Molecular epidemiology of human adenoviruses. Curr Trop Microbiol Immunol. 1984, 110: 191-220.
Elnifro EM, Cooper RJ, Klapper PE, Bailey AS: PCR and restriction endonuclease analysis for rapid identification of human adenovirus subgenera. J Clin Microbiol. 2000, 38: 2055-2061.
Casas I, Avellon A, Mosquera M, Jabado O, Echevarria JE, Campos RH, Rewers M, Perez-Brena P, Lipkin WI, Palacios G: Molecular identification of adenoviruses in clinical samples by analyzing a partial hexon genomic region. J Clin Microbiol. 2005, 43: 6176-6182. 10.1128/JCM.43.12.6176-6182.2005.
AbuBakar S, Wong PF, Chan YF: Emergence of dengue virus type 4 genotype IIA in Malaysia. J Gen Virol. 2002, 83: 2437-2442.
Thompson JD, Higgins GD, Gibson TJ: CLUSTAL W: improving the sensitivity of progressive multiple sequence alignments through sequence weighting, position specific gap penalties and weight matrix choice. Nucl Acids Res. 1994, 22: 4673-4680. 10.1093/nar/22.22.4673.
Felsenstein J: PHYLIP (Phylogeny Inference Package) version 3.67. Distributed by the author. Department of Genetics, University of Washington, Seattle
Tamura K, Dudley J, Nei M, Kumar S: MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol Biol Evol. 2007, 24: 1596-1599. 10.1093/molbev/msm092.
Cardosa MJ, Krishnan S, Tio PH, Perera D, Wong SC: Isolation of subgenus B adenovirus during a fatal outbreak of enterovirus 71-associated hand, foot and mouth disease in Sibu, Sarawak. Lancet. 1999, 354: 987-991. 10.1016/S0140-6736(98)11032-2.
AbuBakar S, Chee HY, Shafee N: Adenovirus in EV71-associated hand, foot and mouth disease. Lancet. 2000, 355: 416-10.1016/S0140-6736(05)72060-2.
Wadell G, Allard A, Hierholzer JC: Adenoviruses. Manual of Clinical Microbiology. Edited by: Murray PR, Baron EJ, Pfaller MA, Tenover F, Yolken RN. 1999, Washington DC: American Society for Microbiology, 970-982. 7
Horwitz MS: Adenoviruses. Fields Virology. Edited by: Fields BN, Knipe DM, Howley PM, Griffin DE. 2001, Philadelphia: Lippincott Williams & Wilkins, 2301-2326. 4
Kojaoghlanian T, Flomenberg P, Horwitz MS: The impact of adenovirus infection on the immunocompromised host. Rev Med Virol. 2003, 13: 155-171. 10.1002/rmv.386.
Walls T, Shankar AG, Shingadia D: Adenovirus: an increasingly important pathogen in paediatric bone marrow transplant patients. Lancet Infect Dis. 2003, 3: 79-86. 10.1016/S1473-3099(03)00515-2.
Zamberi S, Zulkifli I, Ilina : Respiratory viruses detected in hospitalised paediatric patients with respiratory infections. Med J Malaysia. 2003, 58: 681-687.
Fox JP, Hall CE, Cooney MK: The Seattle virus watch. IV. Observations of adenovirus infections. Am J Epidemiol. 1977, 105: 362-386.
Cooper RJ, Hallett R, Tullo AB, Klapper PE: The epidemiology of adenovirus infections in Greater Manchester, UK 1982-96. Epidemiol Infect. 2000, 125: 333-345. 10.1017/S0950268899004550.
Hong JY, Lee HJ, Piedra PA, Choi EH, Park KH, Koh YY, Kim WS: Lower respiratory tract infections due to adenovirus in hospitalized Korean children: epidemiology, clinical features, and prognosis. Clin Infect Dis. 2001, 32: 1423-1429. 10.1086/320146.
Li QG, Zheng QJ, Liu YH, Wadell G: Molecular epidemiology of adenovirus types 3 and 7 isolated from children with pneumonia in Beijing. J Med Virol. 1996, 49: 170-177. 10.1002/(SICI)1096-9071(199607)49:3<170::AID-JMV3>3.0.CO;2-1.
Reddick RA, Lefkowitz SS: In vitro immune responses of rabbits with persistent adenovirus type 5 infection. J Immunol. 1969, 103: 687-694.
Pereira HG: Persistent infection by adenoviruses. J Clin Pathol Suppl. 1972, 6: 39-42. 10.1136/jcp.s3-6.1.39.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/10/46/prepub
Acknowledgements
We thank the Department of Medical Microbiology, University of Malaya for allowing the study to be undertaken using virus isolates from the UMMC Virology repository. None of the authors received specific funding for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SAB is the principal investigator of the study. SAB and JAJ designed the study and drafted and wrote the manuscript. NR and EHH propagated and maintained the virus isolates and performed the initial genomic sequence amplification. BTT performed the sequence alignment, sequence analysis, and tree-drawing. All authors have read and approved the final manuscript.
Juraina Abd-Jamil, Boon-Teong Teoh, Eddy H Hassan, Nuruliza Roslan and Sazaly AbuBakar contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Abd-Jamil, J., Teoh, BT., Hassan, E.H. et al. Molecular identification of adenovirus causing respiratory tract infection in pediatric patients at the University of Malaya Medical Center. BMC Pediatr 10, 46 (2010). https://doi.org/10.1186/1471-2431-10-46
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-10-46