Abstract
Background
Gastric cancer is the second leading cause of oncologic death worldwide. One of the most noteworthy characteristics of this tumor's epidemiology is the marked decline reported in its incidence and mortality in almost every part of the globe in recent decades. This study sought to describe gastric cancer mortality time trends in Spain's regions for both sexes.
Methods
Mortality data for the period 1976 through 2005 were obtained from the Spanish National Statistics Institute. Cases were identified using the International Classification of Diseases 9th and 10th revision (codes 151 and C16, respectively). Crude and standardized mortality rates were calculated by geographic area, sex, and five-year period. Joinpoint regression analyses were performed to ascertain whether changes in gastric cancer mortality trends had occurred, and to estimate the annual percent change by sex and geographic area.
Results
Gastric cancer mortality decreased across the study period, with the downward trend being most pronounced in women and in certain regions situated in the interior and north of mainland Spain. Across the study period, there was an overall decrease of 2.90% per annum among men and 3.65% per annum among women. Generally, regions in which the rate of decline was sharpest were those that had initially registered the highest rates. However, the rate of decline was not constant throughout the study period: joinpoint analysis detected a shift in trend for both sexes in the early 1980s.
Conclusion
Gastric cancer mortality displayed in both sexes a downward trend during the study period, both nationally and regionally. The different trend in rates in the respective geographic areas translated as greater regional homogeneity in gastric cancer mortality by the end of the study period. In contrast, rates in women fell more than did those in men. The increasing differences between the sexes could indicate that some risk factors may be modifying the sex-specific pattern of this tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Gastric cancer (GC) is the second leading cause of oncologic death worldwide [1, 2], due to its elevated incidence and lethality; in many countries survival at five years of diagnosis is under 20% [3]. This cancer, with higher rates in males and sex ratios generally close to 2, displays wide geographic variability. In Japan, China and some regions of Eastern Europe and Latin America (Chile, Ecuador), rates are almost 20 times higher than those registered in India, the Philippines, USA or some areas in North and East Africa [1, 2].
One of the most noteworthy characteristics of this tumor's epidemiology is the marked decrease seen in its incidence and mortality since the second half of the 20th century: whereas stomach cancer was the second leading cause of death due to malignant tumors in the European Community in the 1990s [4], it currently ranks fourth after tumors of lung, breast and colon [2]. In Europe, gastric cancer incidence and mortality have registered a downward trend since the 1960s [5, 6].
Generally, this downward turn in gastric cancer is attributed to changes in some risk factors traditionally implicated in its etiology, namely: improvements in the way in which food is preserved, including the use of refrigeration, changes in the dietary habits of the population, and the decline in the prevalence of Helicobacter pylori infection [7–9]. Yet, as is the case with most tumors, the etiology of gastric cancer has not been entirely elucidated, in that there are other risk factors referred to in the literature, such as socio-economic level [10], presence of contaminants in drinking water [11, 12], and certain occupational exposures [13, 14].
In Spain, the trend in GC mortality rates in recent years has been similar to that of other countries in Western Europe. This tumor is currently the 5th leading cause of cancer-related death in both sexes, with rates of 12.94 and 5.65 in men and women, respectively [15]. However, as has also been reported in other European countries, such as Greece and Italy [16], there are important geographic differences within Spain. In this sense, some Spanish regions present mortality rates that are much higher than the European mean, while others show rates that are among the lowest in the continent [17, 18]. This study sought to describe GC mortality time trends in Spain and its constituent regions, for the period 1976 through 2005.
Methods
Mortality data were drawn from individual death entries furnished by the National Statistics Institute (NSI). We included all deaths certified as stomach cancer (codes 151 and C16 of the International Classifications of Diseases, 9th and 10th revisions (ICD-9 and ICD-10), respectively) in the period 1976-2005. As denominators, we used populations estimated at July 1 of each year, also provided by the NSI.
Crude and standardized mortality rates were calculated by the direct method (standard European population) for each Autonomous Region (AR), sex and five-year period (1976-1980,...; 2000-2005).
Trends in mortality rates (national and regional) were calculated by estimating the annual percent change (APC) and studying possible joinpoints (points at which a change in trend during the period is observed) in the trend. For this purpose, crude and standardized rates were then calculated for each calendar year, again broken down by AR, sex, and broadly categorized age group (35-64 and over 64 years).
Joinpoint analysis is known as multiple-phase regression analysis and is based on a Poisson model that fits the observed mortality rates [19]. Starting with the model having the minimum number of joinpoints the program adds new joinpoints (up to a maximum of three), and ascertains whether these should or should not be included in the initial model on the basis of their significance. To this end it performs hypothesis tests among the different models, based on a Monte Carlo method [20, 21]. The final model estimates the joinpoints and the APC for each temporal segment displaying constant trend. Each joinpoint indicates a significant change in trend during the study period.
Results
Table 1 shows the standardized five-yearly mortality rates for Spain as a whole and for each of the ARs, grouped by trend pattern registered over the study period and geographic location. Higher mortality rates were registered at the beginning of the period, with these being particularly high in some regions in inland and Northern Spain, with Castile & León at the head. Across the period analyzed, mortality decreased in all regions of Spain. This decline was more pronounced in those areas which initially had the highest rates, something that translated as greater regional homogeneity in GC mortality by the end of the study period. Hence, in the first five-year period, the observed rates ratio among the regions with highest and lowest mortality (Castile & León and the Balearic Islands, respectively) was 2.53 for men and 3.54 for women, while in the last five-year period these ratios were 1.99 and 2.10, respectively. Despite the declining trends, central and Northern Spain continued to be the regions with the highest rates in 2005, with Castile & León again at the head. In terms of gender, mortality was always higher in males, both nationally and regionally.
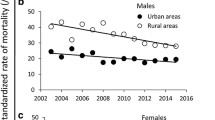
Figure 1 depicts the trend of standardized and truncated rates (ages 35-64 years and 65 years or more). Note should be taken of the steeper downward trend among women aged over 65 years. [see Additional file 1] shows the APC for the entire period and for the last 10 years, together with the rates for the first and last quinquennia. Also shown are the inflection points detected and the trend for each time segment. Across the study period, there was an overall decrease in the rates of 2.90% per annum in men and 3.65% per annum in women. Joinpoint analysis detected a change in trend in both sexes in the early 1980s. During the first period, rates fell by 4.58% per annum in men and 5.24% per annum in women, with the rate of decline leveling off thereafter.
When the trend was analyzed in the individual ARs (excluding the autonomous city enclaves of Ceuta and Melilla), two mortality patterns were discerned (Figure 2). The first of these included the ARs situated in the interior and in Northern Spain (Castile & León, Castile-La Mancha, Extremadura, La Rioja, and Aragon), with the highest rates at the beginning of the period and the greatest overall rate of decline during the initial years studied (APC of 2.7% to 3.6% in males, and 3.4% to 4.4% in women). The second group included the ARs in Eastern Spain, Andalusia and the Canary and Balearic Islands, with the lowest rates and, in general, lower rates of decline. The Madrid Region registered a pattern unlike that of the other ARs in the center of the country, with its trend being more like that of Eastern Spain. As reference, figure 3 shows the situation of Spain's Autonomous Communities.
Finally, it should be noted that the decline in the rates was greater among females, a phenomenon observed throughout the period. This larger rate of decline in women (who started from lower rates) explains the fact that sex-related differences have become more pronounced in recent years. Indeed, in some areas this has been compounded by the slowdown observed in the decrease in male mortality during the last ten years (e.g. Extremadura, Andalusia and Catalonia).
Discussion
Our results highlight a decrease in GC mortality in Spain across the entire study period. This fall proved greatest in areas which initially had the highest rates (inland areas lying near the Cantabrian mountains and the central plateau), a phenomenon that has made for greater uniformity among the different regional rates over time. Castile & León maintain the highest rates, with an especially high degree of excess mortality in men. Despite having started from lower rates, women nonetheless registered a greater decline in mortality rates due to this tumor.
When it comes to interpreting these results, the limitations of mortality data must be borne in mind. To study cause-specific trends, the best approach would be to combine incidence and mortality data. As there is no information on GC incidence countrywide, mortality continues to be the sole comprehensive source of information in Spain. In the case of GC, the fact that relative survival at 5 years is low, i.e., 24.9% in Europe and 31.8% in Spain [22], means that mortality data are a relatively reliable approximation of incidence rates. However, some authors suggest that in some countries the decline in mortality might have been swifter than that of incidence, in some countries at least [23]. Available incidence data from regional cancer population registries also suggest that this might be the case in Spain [24].
A further possible limitation of the data used is linked to the quality of death registry entries. In Spain, a recent review indicated that, for GC, mortality statistics are a valid and useful tool for estimating this tumor's impact [25]. Nevertheless, there are discontinuities in the coding which could be responsible for some of the changes observed in trends. The change in coding from ICD-8 to ICD-9 was introduced around 1980, and could be related with the change in trend observed for the country in the early 80s. In addition, the decentralization in the coding of mortality statistics in this decade led to an increase in the quality of these data [25], which might be responsible for some of the shifts in trends, as could be the case of Madrid. The improvement in the coding of some gynecological neoplasms (of ovarian or uterine origin), which have sometimes been erroneously registered as tumors of other organs of the abdominal cavity such as stomach, could have had some degree of influence on the sharper decline in trends among women [25].
To delimit the true causes that have led to the observed differences in GC trends among ARs is complex. Some factors, such as the role of H. pylori as a carcinogenic promoter [26], or diet [27, 28], which contribute to the etiopathogeny of GC are widely accepted. In Spain, studies published on the prevalence of H. pylori infection report interregional differences ranging from 43% [29] to 69% [30], but the scarcity of data do not enable their implication in the trend in rates to be assessed. Insofar as diet is concerned, some risk factors, e.g., intake of nitrates through consumption of cured and pickled foods [31, 32] or drinking water [33, 34], and prevention factors, e.g., consumption of fruit and vegetables in particular, have been recognized. Along with these factors, others have been described, such as socio-economic differences, a variable that may in turn indicate differences in exposure to various factors including prevalence of H. pylori infection, diet, tobacco use, alcohol, or access to the health system, among others [23].
During the study period, Spain's society underwent major transformations. Vigorous economic development was accompanied by important changes in social structure, with the urban middle classes becoming predominant, and increases in per capita income and the percentage allocated to public health expenditure [35, 36]. All these changes, taken together with a notable improvement in lifestyles, took place in parallel with the trend plotted by gastric cancer mortality.
In terms of socio-economic level, uniformity in rates has been accompanied by a convergence in socioeconomic levels among the different ARs [37, 38]. Even so, if one examines the economic level of each AR, it will be noted that among the ARs which had a lower socioeconomic level in the mid-20th century, some are still registering the highest GC mortality rates 25-30 years afterwards (Extremadura, Castile & León, Castile-La Mancha, and Galicia), whereas in others (Murcia, Andalusia) the opposite has occurred. Similarly, areas in which GDP per capita was higher than the national mean in the 1970s, such as Navarre or La Rioja, register elevated mortality rates.
In general terms, one of the reasons that may account for the decrease in mortality rates is the change in diet, with a progressive globalization in food consumption patterns and greater accessibility to perishable foods [39]. Whereas Spaniards' food intake was very unequal at the beginning of the century, being characterized by protein, mineral and vitamin deficiency [40], the nutritional transition, initiated with the industrialization process, entailed a change in the consumption of basic foods and an increase in foods of animal origin, fruit, and sugars. Homemade food production thus fell and industrial production rose. An important element in this change was the introduction of the first refrigerators in Spain in the early 1950s, though these were to take some years in finding their way into all Spanish homes. Little by little, habits tend to become more uniform, and differences in terms of consumption of certain foods, such as fruit and vegetables, viewed as protective against GC by providing compounds with antioxidant properties, tend to disappear [39, 41, 42].
With respect to H. pylori's role as a carcinogenic promoter, it has not been possible to measure the impact of H. pylori eradication treatment on the decrease in GC incidence [43], yet there is strong evidence to show that administration of such treatment in certain subgroups of patients prevents the progression of precursor lesions [44]. Sight should therefore not be lost of the favorable effect that the introduction and progressive improvement in H. pylori treatment guidelines, coupled with the generalized use of antibiotics which took place in the latter half of the 20th century, may have had on the observed trends.
Along these same lines, the role of probiotics in the prevention and eradication of H. pylori has recently been proposed [45–49]. The population's growing concern with health has made the so-called "functional foods" fashionable (i.e., foods enriched with biologically activated components); probiotics constituting up to 65% of the European functional food market [50]. Specifically, in Eastern Spain a reduction in the consumption of liquid milk in favor of enriched dairy products has been observed [51, 52], fundamentally among the higher-level social classes [53]. This also occurs in the Canary Islands [54] and Andalusia, where these products have traditionally been less expensive and the habit of consuming such foods is better established. In contrast, in the North and North-west regions and in Castile-La Mancha, the consumption of liquid milk still takes precedence.
Another factor that could be implicated in the decline in mortality is the improvement in drinking-water quality, linked to the country's economic development. Thus, in the study period, the population supplied by surface waters increased, in detriment to the use of subterranean waters which have a lower power of recovery vis-à-vis the presence of contaminants [55]. Besides, quality criteria set by international bodies became more stringent [56], thereby contributing to the decrease in exposure to physical or biological chemical contaminants in the Spanish population [57].
Lastly, stress must again be laid on the differences between the two sexes observed in the trend. To explain some of the sex-related differences in GC distribution, the protective role of estrogenic hormones has been proposed. These differences would not, however, account for the different behavior observed in the rates of decline, bearing in mind that when these rates were truncated, these differences were seen to become even more pronounced in women aged over 65 years. The role that improvements in coding may have had on this finding, has already been discussed above. Nevertheless, in view of the dominant role of environmental factors in the appearance of GC, consideration should be given to the possible coexistence of other factors of unequal sex-related distribution which might be influencing the two groups differently. Some authors propose greater self-care among women, or cite the different effect that physical exercise may have in both sexes, e.g., a recently published paper proposes the beneficial role of an increase in physical activity on reduction in GC risk among women, with no such effect being found for gastric cancer among males [58].
Conclusion
In conclusion, gastric cancer displayed a downward trend throughout the study period, both for Spain overall and for all the country's constituent regions, across the sexes. The different trend registered in the Spanish ARs has, however, translated as greater regional homogeneity in mortality due to this tumor because the fall was steeper in areas which initially had the highest rates. It is essential that efforts continue to be directed at ascertaining which factors are determining the greater rate of decline among women. Their identification could amount to an important advance in the prevention of this tumor.
Abbreviations
- GC:
-
Gastric cancer
- APC:
-
Annual percent change
- AR:
-
Autonomous region.
References
Ferlay J, Bray F, Pisani P, Parkin DM: GLOBOCAN 2002: Cancer Incidence, Mortality and Prevalence Worldwide. IARC CancerBase No.5. version 2.0. 2004, Lyon, IARC Press
Parkin DM, Bray F, Ferlay J, Pisani P: Global cancer statistics, 2002. CA Cancer J Clin. 2005, 55: 74-108. 10.3322/canjclin.55.2.74.
Verdecchia A, Mariotto A, Gatta G, Bustamante-Teixeira MT, Ajiki W: Comparison of stomach cancer incidence and survival in four continents. Eur J Cancer. 2003, 39: 1603-1609. 10.1016/S0959-8049(03)00360-5.
Parkin DM, Pisani P, Ferlay J: Global cancer statistics. CA Cancer J Clin. 1999, 49: 33-64. 10.3322/canjclin.49.1.33. 1.
Aragones N, Pollan M, Rodero I, Lopez-Abente G: Gastric cancer in the European Union (1968-1992): mortality trends and cohort effect. Ann Epidemiol. 1997, 7: 294-303. 10.1016/S1047-2797(97)00002-1.
Levi F, Lucchini F, Negri E, La Vecchia C: Trends in mortality from major cancers in the European Union, including acceding countries, in 2004. Cancer. 2004, 101: 2843-2850. 10.1002/cncr.20666.
Amiri M, Kunst AE, Janssen F, Mackenbach JP: Trends in stomach cancer mortality in relation to living conditions in childhood. A study among cohorts born between 1860 and 1939 in seven European countries. Eur J Cancer. 2006, 42: 3212-3218. 10.1016/j.ejca.2006.04.020.
Riboli E, Norat T: Epidemiologic evidence of the protective effect of fruit and vegetables on cancer risk. Am J Clin Nutr. 2003, 78: 559S-569S.
Roder DM: The epidemiology of gastric cancer. Gastric Cancer. 2002, 5 (Suppl 1): 5-11. 10.1007/s10120-002-0203-6.
Nagel G, Linseisen J, Boshuizen HC, Pera G, Del Giudice G, Westert GP, Bueno-de-Mesquita HB, Allen NE, Key TJ, Numans ME, et al: Socioeconomic position and the risk of gastric and oesophageal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Epidemiol. 2007, 36: 66-76. 10.1093/ije/dyl275.
Barrett JH, Parslow RC, McKinney PA, Law GR, Forman D: Nitrate in drinking water and the incidence of gastric, esophageal, and brain cancer in Yorkshire, England. Cancer Causes Control. 1998, 9: 153-159. 10.1023/A:1008878126535.
Morales-Suarez-Varela MM, Llopis-Gonzalez A, Tejerizo-Perez ML: Impact of nitrates in drinking water on cancer mortality in Valencia, Spain. Eur J Epidemiol. 1995, 11: 15-21. 10.1007/BF01719941.
Aragones N, Pollan M, Gustavsson P: Stomach cancer and occupation in Sweden: 1971-89. Occup Environ Med. 2002, 59: 329-337. 10.1136/oem.59.5.329.
Cocco P, Palli D, Buiatti E, Cipriani F, DeCarli A, Manca P, Ward MH, Blot WJ, Fraumeni JF: Occupational exposures as risk factors for gastric cancer in Italy. Cancer Causes Control. 1994, 5: 241-248. 10.1007/BF01830243.
Centro Nacional de Epidemiología: Mortalidad por cáncer en España (2006). [http://www.isciii.es/htdocs/centros/epidemiologia/epi_cancer.jsp]
Health Statistics: Atlas on mortality in the European Union. Luxembourg. 2002
Lopez-Abente G, Ramis R, Pollan M, Aragones N, Perez-Gomez B, Gomez-Barroso D, et al: Atlas municipal de mortalidad por cáncer en España 1989-1998. Madrid. 2006
López-Abente G, Pollán M, Escolar A, Errezola M, Abraira V: Atlas de mortalidad por cáncer y otras causas en España 1978-1992. Madrid. 1996, 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z.
National Cancer Institute: Joinpoint Regression Program. 2009, [http://srab.cancer.gov/joinpoint/]
Kim HJ, Fay MP, Feuer EJ, Midthune DN: Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000, 19: 335-351. 10.1016/S0959-8049(01)00279-9.
Fernandez E, Gonzalez JR, Borras JM, Moreno V, Sanchez V, Peris M: Recent decline in cancer mortality in Catalonia (Spain). A joinpoint regression analysis. Eur J Cancer. 2001, 37: 2222-2228. 10.1016/S1470-2045(07)70246-2.
Verdecchia A, Francisci S, Brenner H, Gatta G, Micheli A, Mangone L, Kunkler I: Recent cancer survival in Europe: a 2000-02 period analysis of EUROCARE-4 data. Lancet Oncol. 2007, 8: 784-796. 10.1016/j.bpg.2006.04.008.
Forman D, Burley VJ: Gastric cancer: global pattern of the disease and an overview of environmental risk factors. Best Pract Res Clin Gastroenterol. 2006, 20: 633-649. 10.1157/13101089.
IARC: Cancer Mondial. [http://www-dep.iarc.fr/]
Perez-Gomez B, Aragones N, Pollan M, Suarez B, Lope V, Llacer A, Lopez-Abente G: Accuracy of cancer death certificates in Spain: a summary of available information. Gac Sanit. 2006, 20 (Suppl 3): 42-51. 10.1007/s10120-007-0420-0.
Iarc.Monographs on the Evaluation of the Carcinogenic Risks to Humans: Schistosomes, liver flukes and Helicobacter pylori. 1994, Lyon: International Agency for Research on Cancer
Tsugane S, Sasazuki S: Diet and the risk of gastric cancer: review of epidemiological evidence. Gastric Cancer. 2007, 10: 75-83. 10.1007/s10120-007-0420-0.
Gonzalez CA, Jakszyn P, Pera G, Agudo A, Bingham S, Palli D, Ferrari P, Boeing H, Del Giudice G, Plebani M, et al: Meat intake and risk of stomach and esophageal adenocarcinoma within the European Prospective Investigation Into Cancer and Nutrition (EPIC). J Natl Cancer Inst. 2006, 98: 345-354. 10.1023/A:1007485815609.
Senra-Varela A, Lopez-Saez JB, Gomez-Biondi V: Prevalence of Helicobacter pylori infection in two Spanish regions with different incidence of gastric cancer. Eur J Epidemiol. 1998, 14: 491-494. 10.1023/A:1007485815609.
Macenlle GR, Gayoso DP, Sueiro Benavides RA, Fernandez SJ: Prevalence of Helicobacter pylori infection in the general adult population of the province of Ourense. Rev Esp Enferm Dig. 2006, 98: 241-248.
Llopis A, Morales M, Rodriguez R: Digestive cancer in relation to diet in Spain. J Environ Pathol Toxicol Oncol. 1992, 11: 169-175. 10.1093/ije/25.3.494.
Joossens JV, Hill MJ, Elliott P, Stamler R, Lesaffre E, Dyer A, Nichols R, Kesteloot H: Dietary salt, nitrate and stomach cancer mortality in 24 countries. European Cancer Prevention (ECP) and the INTERSALT Cooperative Research Group. Int J Epidemiol. 1996, 25: 494-504. 10.1093/ije/25.3.494.
Iarc.Monographs on the Evaluation of the Carcinogenic Risks to Humans: Ingested Nitrates and Nitrites, and Cyanobacterial Peptide Toxins. 2006, Lyon: International Agency for Research on Cancer
Sanz Anquela JM, Munoz Gonzalez ML, Ruiz Liso JM, Rodriguez ML, Alfaro TJ: [Correlation of the risk of gastric cancer in the province of Soria and the nitrate content of drinking water]. Rev Esp Enferm Apar Dig. 1989, 75: 561-565.
Alcaide Inchausti J: Evolución económica de las regiones y provincias españolas en el siglo XX. 2003
Robles GE, Garcia BF, Bernabeu MJ: [Health transition in Spain from 1900 to 1990]. Rev Esp Salud Publica. 1996, 70: 221-233.
Paradella M, Álvarez M: La distribución de la renta en España. Tendencias recientes y situación actual. Circunstancia: revista de ciencias sociales del Instituto Universitario de Investigación Ortega y Gasset. 2006
Navarro Espigares JL, Hernández Torres E: Distribución y redistribución de la renta en la literatura española reciente. Estudios de economía aplicada. 2004, 22 (1): 29-65.
Rodriguez AF, Graciani MA, Banegas JR, Martin-Moreno JM, Sabate J, Rey CJ: [Food and nutrient consumption in Spain in 1940-1988 (and II). Comparative study of the main sources of information on food consumption]. Med Clin (Barc). 1996, 107: 446-452. 10.1590/S1135-57272007000500003.
Bernabeu-Mestre J, Esplugues Pellicer JX, Galiana Sanchez ME: [Historical background data of Spanish community nutrition: the works of the National School of Health between 1930-36]. Rev Esp Salud Publica. 2007, 81: 451-459. 10.1038/sj.ejcn.1601414.
Moreno LA, Sarria A, Popkin BM: The nutrition transition in Spain: a European Mediterranean country. Eur J Clin Nutr. 2002, 56: 992-1003. 10.1038/sj.ejcn.1601414.
Gonzalez CA, Argilaga S, Agudo A, Amiano P, Barricarte A, Beguiristain JM, Chirlaque MD, Dorronsoro M, Martinez C, Navarro C, et al: [Sociodemographic differences in adherence to the Mediterranean dietary pattern in Spanish populations]. Gac Sanit. 2002, 16: 214-221.
Fuccio L, Zagari RM, Minardi ME, Bazzoli F: Systematic review: Helicobacter pylori eradication for the prevention of gastric cancer. Aliment Pharmacol Ther. 2007, 25: 133-141. 10.1136/gut.2006.101634.
Malfertheiner P, Megraud F, O'Morain C, Bazzoli F, El Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ: Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007, 56: 772-781. 10.1097/MOG.0b013e3282f0cffc.
Boirivant M, Strober W: The mechanism of action of probiotics. Curr Opin Gastroenterol. 2007, 23: 679-692. 10.1111/j.1523-5378.2007.00565.x.
Franceschi F, Cazzato A, Nista EC, Scarpellini E, Roccarina D, Gigante G, Gasbarrini G, Gasbarrini A: Role of probiotics in patients with Helicobacter pylori infection. Helicobacter. 2007, 12 (Suppl 2): 59-63. 10.1016/j.nut.2008.01.007.
Gotteland M, Andrews M, Toledo M, Munoz L, Caceres P, Anziani A, Wittig E, Speisky H, Salazar G: Modulation of Helicobacter pylori colonization with cranberry juice and Lactobacillus johnsonii La1 in children. Nutrition. 2008, 24: 421-426. 10.1016/j.nut.2008.01.007.
Jonkers D, Stockbrugger R: Review article: Probiotics in gastrointestinal and liver diseases. Aliment Pharmacol Ther. 2007, 26 (Suppl 2): 133-148. 10.1111/j.1523-5378.2008.00595.x.
Zhang L, Su P, Henriksson A, O'Rourke J, Mitchell H: Investigation of the immunomodulatory effects of Lactobacillus casei and Bifidobacterium lactis on Helicobacter pylori infection. Helicobacter. 2008, 13: 183-190. 10.1111/j.1523-5378.2008.00595.x.
Stanton C, Gardiner G, Meehan H, Collins K, Fitzgerald G, Lynch PB, Ross RP: Market potential for probiotics. Am J Clin Nutr. 2001, 73: 476S-483S.
Serra ML, Ribas BL, Salvador CG, Roman VB, Castell AC, Cabezas PC, Pastor Ferrer MC, Raido QB, Ngo dlC, Garcia AA, et al: [Trends in the nutritional status of the Spanish population: results from the Catalan nutrition monitoring system (1992-2003)]. Rev Esp Salud Publica. 2007, 81: 559-570. 10.1079/PHN2002443.
Ministerio de Medio Ambiente y Medio Rural y Marino: La alimentación en España. Años. 2003, [http://www.mapa.es/es/alimentacion/pags/consumo/consumo.htm] -2006
Capdevila F, Marti-Henneberg C, Closa R, Subias JE, Fernandez-Ballart J: Yoghurt in the Spanish diet: nutritional implications and socio-cultural aspects of its consumption. Public Health Nutr. 2003, 6: 333-340. 10.1157/13062255.
Serra ML, Armas NA, Ribas BL: [Food consumption and food sources of energy and nutrients in Canary Islands (1997-98)]. Arch Latinoam Nutr. 2000, 50: 23-33. 10.1093/aje/kwn146.
Barea J, de Armas H, Caballero MJ, Carrasco JF, Colmenarejo P, García L, et al: Agua. La calidad de las aguas en España. Un estudio por cuencas. Greenpeace 2005. [http://www.greenpeace.org/espana/reports/agua-la-calidad-de-las-aguas]
European Council: Directive 98/83/EC of 3 November 1998 on the quality of water intended for human consumption. [http://eur-lex.europa.eu]
Gonzalez B, Urbanos RM, Ortega P: [Public and private supply of health services by autonomous communities in Spain]. Gac Sanit. 2004, 18 (Suppl 1): 82-89. 10.1157/13062255.
Inoue M, Yamamoto S, Kurahashi N, Iwasaki M, Sasazuki S, Tsugane S: Daily total physical activity level and total cancer risk in men and women: results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2008, 168: 391-403. 10.1093/aje/kwn146.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/9/346/prepub
Acknowledgements
The authors would like to thank Michael Benedict for his help with the English and Diana Gómez-Barroso for her assistance with the graphic material.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NA, BPG, MP and GLA were all involved in designing the study. EGE, NA and BPG performed the statistical analysis and wrote the first draft of the manuscript to which all authors subsequently contributed. All authors read and approved the final manuscript.
Electronic supplementary material
12885_2009_1680_MOESM1_ESM.DOC
Additional file 1: Table S1. Age-standardized cancer mortality rates per 100,000 person-years (1976-1980 and 2001-2005) and joinpoint analysis (1976-2005) in Spain, by sex and Autonomous Region. (DOC 122 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
García-Esquinas, E., Pérez-Gómez, B., Pollán, M. et al. Gastric cancer mortality trends in Spain, 1976-2005, differences by autonomous region and sex. BMC Cancer 9, 346 (2009). https://doi.org/10.1186/1471-2407-9-346
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-9-346