Abstract
Background
The development of novel chemotherapeutic agents in colorectal cancer has improved survival. Following initial response to chemotherapeutic strategies many patients develop refractory disease. This poses a significant challenge common to many cancer subtypes. Newer agents such as Bevacizumab have successfully targeted the tyrosine kinase receptor epidermal growth factor receptor in metastatic colorectal cancer. Human epidermal growth factor receptor-2 is another member of the tyrosine kinase receptor family which has been successfully targeted in breast cancer. This may play a role in colorectal cancer. We conducted a clinicopathological study to determine if overexpression of human epidermal growth factor receptor-2 is a predictor of outcome in a cohort of patients with colorectal cancer.
Methods
Clinicopathological data and paraffin-embedded specimens were collected on 132 consecutive patients who underwent colorectal resections over a 24-month period at Mayo General Hospital. Twenty-six contained non-malignant disease. Her-2/neu protein overexpression was detected using immunohistochemistry (IHC). The HER-2 4B5 Ventana monoclonal antibody was used. Fluorescent insitu hybridisation (FISH) was performed using INFORM HER-2/Neu Plus. Results were correlated with established clinical and pathological predictors of outcome including TNM stage. Statistical analysis was performed using SPSS version 11.5.
Results
114 were HER-2/Neu negative using IHC, 7 showed barely perceptible positivity (1+), 9 showed moderate staining (2+) and 2 were strongly positive (3+). There was no correlation with gender, age, grade, Dukes' stage, TNM stage, time to recurrence and 5-year survival (p > 0.05). FISH was applied to all 2+ and 3+ cases as well as some negative cases selected at random. Three were amplified (2 were 3+ and 1 was 2+). Similarly, HER-2 gene overexpression did not correlate with established prognostic indicators.
Conclusion
HER-2 protein is over expressed in 11% of colorectal cancer patients. The gene encoding HER-2 is amplified in 3% of cases. Overexpression of HER-2 is not a predictor of outcome. However, patients who over express HER-2 may respond to Herceptin therapy.
Similar content being viewed by others
Background
Colorectal cancer is the second commonest cause of cancer-related death in the United States and the Western World [1, 2]. The 5-year relative survival rate is approximately 45% demonstrating an improvement from 30 years ago when the survival rate was 30%. Modifications in adjuvant therapy have been central to this observed improvement. Cytotoxic agents such as irinotecan and oxaliplatin have improved survival while the development of monoclonal antibodies against growth factor receptors has augmented their effects. A significant improvement in the median overall survival in patients with metastatic colorectal cancer was achieved when Bevacizumab (a monoclonal antibody directed against the tyrosine kinase receptor, VEGF) was added to a chemotherapy regimen of oxaliplatin and 5-fluorouracil (P = 0.0024) [3].
The human epidermal growth factor receptor-2 (HER-2) is another member of the tyrosine kinase receptor superfamily. HER-2 protein is also known as c-erb-2 or neu. Slamon et al demonstrated that this is over expressed in 30% of patients with breast cancer [4]. Trastuzumab (a monoclonal antibody directed against HER-2) has impacted upon survival in approximately 20% of patients who over express HER-2 and is now established therapy in the treatment of metastatic breast cancer [5]. Other members of the family include HER-1, HER-3 and HER-4. They all possess an extracellular ligand binding domain, a membrane spanning region and a cytoplasmic domain with tyrosine kinase activity. It is understood that HER-2 heterodimerises with other HER receptors unlike the other family receptors which possess a direct binding ligand. In tumour model systems overexpression of the HER-2 gene correlates with mitogenesis, malignant transformation, increased cell motility, invasion and metastasis [6]. Overexpression of HER-2/neu in breast cancer is a useful marker of outcome. It correlates with a poor prognosis. Moreover, it is used to predict patient response to adjuvant chemotherapy and endocrine therapy and to select patients for immunotherapy with targeted monoclonal antibody therapy [7, 8]. Intuitively, patients who over express HER-2 should respond to Trastuzumab (Herceptin) therapy independent of the tissue of origin of the cancer. Herceptin has been shown to inhibit colony formation of the HCA-colon cancer cell line and HCA-7 tumour xenografts [9].
Several studies have reported a variety of protein and gene expression levels in colorectal cancer. Similarly there is a wide variability in the published literature in relation to survival benefit. This variety is predominantly due to a lack of standardisation of detection methods. Some studies have demonstrated up to 70% overexpression of cytoplasmic HER-2 [10, 11]. Cytoplasmic HER-2 is incapable of transmitting the strong mitogenic signal via heterodimerisation of other members of the EGFR family. Others have reported membranous overexpression in 50% of patients with colorectal cancer [12]. The current study employed the monoclonal antibody 4B5 which is used to determine suitability for Herceptin therapy in breast cancer in our unit. We employed a FISH technique validated for therapeutic use in breast cancer. The aim of the current study was to establish the presence of membranous HER-2 protein overexpression in colorectal cancer, determine if there is gene amplification and establish whether overexpression of HER-2 is a predictor of outcome.
Methods
A total of 132 patients were included for analysis. These represented consecutive patients who underwent colorectal resections at Mayo General Hospital from January 1st, 1998 to December 31st, 1999. The study was approved by the institutions' ethics committee. The study group consisted of 48 females and 84 males. The mean age was 67 years (range = 29 – 89 years). None of the patients had undergone preoperative chemotherapy or radiotherapy. The medical records of these patients were reviewed specifically regarding patient demographics, therapeutic strategies, pathological data and survival. Patients were followed up in accordance with international guidelines. Pathological subtypes included (number): adenomatous polyp (10), diverticulosis (7), IBD (5), ischaemia (2), Carcinoid (1), angiodysplasia (1) and colorectal cancer (106). Each specimen was formalin fixed and embedded in paraffin. Prior to inclusion each slide was verified by a pathologist.
Immunohistochemistry
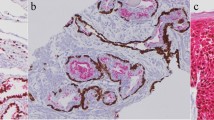
Staining for HER-2/neu protein was performed on 5 μm (micro-meter) thick slides using the Ventana PATHWAY HER-2 (4B5) mouse monoclonal antibody (Ventana Medical Systems, Tuscon, USA). There is significant correlation of staining between the CB11 antibody which is FDA approved and the HerceptTest. In our institution the 4B5 monoclonal antibody is utilised which is equally valid and used to determine suitability for herceptin therapy in breast cancer. Following deparaffinisation, antigen retrieval and incubation with blocking agent the 4B5 monoclonal antibody directed against HER-2/neu was incubated using an automated slide staining device. At the end of each incubation step, the Ventana automated slide stainer washed the sections and applied a cover slip to minimise evaporation of aqueous reagent. The primary antibody was then localised by a biotin-conjugated secondary antibody formulation that recognises mouse immunoglobulins. The specific antibody-secondary antibody-avidin/streptavidin-enzyme complex was then visualised with a diaminobenzidine stain. They were subsequently counterstained with haematoxylin, dehydrated and cover slips were mounted. Slides were viewed by two independent pathologists blinded to each others findings. Negative controls were created by the omission of primary antibody and replacement with phosphate buffered saline (PBS). Invasive breast cancer specimens were utilised as positive controls. Slides were scored using a four-tiered scoring system according to manufacturer's guidelines. Score 0 is defined as no staining or membranous staining in < 10% of tumour cells. Score 1+ is defined as faint membrane staining in > 10% of tumour cells. Score 2+ is defined as weak to moderate staining in > 10% of tumour cells and a score of 3+ is defined as strong staining of the entire membrane in > 10% of tumour cells. A score of 0 or 1+ was considered negative while a score of 2+ or 3+ was considered positive. Cytoplasmic staining may have been present but was not included in the determination of positivity.
Fluorescent insitu hybridisation (FISH) was applied to all 2+ and 3+ cases as well as a random selection of negative cases. This was conducted using the INFORM HER-2/neu plus probe kit. This technique utilises two fluorescent radiolabelled probes: LSI HER-2 (specific to the HER-2 gene locus) and CEP 17 (specific to the alpha satellite DNA sequence at the centromeric region of chromosome 17). The former stains orange while the latter stains green. The slides were evaluated for the HER-2 gene using a fluorescent microscope where a cell is considered to show amplification if > 4 signals of HER-2/neu is detected.
Statistical analysis was performed using SPSS version 11.5. HER-2 protein and gene expression were correlated with clinicopathological parameters and 5-year cancer-related survival using chi-squared testing. Patients who died within 30 days of surgery were excluded from the 5-year cancer-related survival. Patients were followed up for a median of 48.5 months (Range = 1–121 months). For all tests, P < 0.05 was considered to be statistically significant.
Results
One hundred and thirty two consecutive patients were included in the study. Twenty six of these had non-malignant disease.
Immunhistochemical detection of HER-2/neu overexpression
HER-2/neu overexpression was not detected in benign tissues. Ten percent of patients exhibited a score of 2+ or 3+ and were considered positive as shown in Table 1/Figure 1. Positive staining was found in 2 (7%) of the 27 rectal carcinomas and 9 (11%) of the 79 colon cancers. The interobserver agreement was 0.91 as illustrated in Table 2.
Immunohistochemical staining for HER-2/neu (Haematoxylin & eosin, magnification × 200). Breast cancer cells were used as a positive control (not shown). a.) Faint membrane staining is shown in > 10% of tumour cells (1+). b.) Weak to moderate staining of the entire membrane (2+). c.) Strong staining of the entire membrane in > 10%.
The clinical and pathological features of these patients are presented in Table 3. Tumours that over expressed HER-2 were predominantly poorly differentiated and Dukes C. This correlation was not significant (p = 0.72). There was no correlation between HER-2/neu overexpression and age, gender, lymphovascular invasion, TNM stage, perineural invasion or tumour size.
HER-2/neu gene amplification
FISH analysis demonstrated gene amplification in 2 rectal (both 3+) and one colon (2+) cancer (Table 1 & Figure 2). In randomly selected tumours which demonstrated negative staining for HER-2 (0+ and 1+) none revealed amplification of the gene. There was no correlation between gene expression and clinical or pathological parameters.
Correlation with survival
This was carried out on patients with cancer-related death who died a minimum of 30 days following resection. The 5-year survival for well, moderately and poorly differentiated cancer was 78%, 58% and 42% respectively. The 5-year survival by Dukes' stage for A, B, C, D were 86%, 78%, 53% and 13% respectively. There was no correlation between HER-2/neu protein overexpression and disease-free or overall survival as illustrated in Figure 3. (p = 0.9: p = 0.8 respectively)
Discussion
EGFR and HER-2/neu are therapeutic targets in a variety of malignancies due to their overexpression. These can be targeted utilising antibodies directed against the extracellular domains or tyrosine kinase inhibitors. These strategies have been successful in the area of breast cancer and EGFR has been effective in the treatment of metastatic colorectal cancer. Not all patients who overexpress HER-2/neu respond to treatment with Herceptin (25%). The published data report varying rates of HER-2 overexpression in colorectal cancer. The current study was undertaken with a view to establishing a potential role for Herceptin therapy in colorectal cancer by utilising an internationally validated detection method.
Our data demonstrates that HER-2 protein is overexpressed in 11% of cases while the gene is amplified in 3%. While this did not correlate with prognostic indices or survival all cases were poorly differentiated Dukes' C cancers. A lack of consistency between the two techniques has been previously described [12]. This may be interpreted by the hypothesis that protein expression is achieved by transcriptional activation of genes other than the HER-2 gene. Both techniques are used in determining treatment response in breast cancer provided the technique is validated. The wide range of protein (0–70%) and gene (0–30%) expression in colorectal cancer is largely due to the lack of standardisation of the detection methods [13–18]. High protein rates are often reported due to detectable cytoplasmic HER-2 which is not targeted by Herceptin. Immunohistochemistry is relatively inexpensive, widely available, easy to preserve, less time consuming and requires a routine microscope. Assessment by two pathologist with minimal interobserver variability improves the accuracy. The variability in antigen retrieval, antibody type and inconsistent storage of paraffin embedded tissues limits it accuracy. FISH uses a more objective scoring system, is automated and has a sensitivity of 96% and a specificity of 100% [19]. However, it is expensive, time consuming, requires a fluorescent microscope and it is difficult to distinguish tumor cells from normal stromal cells. Emerging results suggests that FISH is more accurate than immunohistochemistry in predicting patient outcome and response to herceptin [20].
We have not demonstrated that overexpression of HER-2 predicts survival however we have shown that it tends to appear in a more aggressive phenotype. Lazaris et al identified a 36% expression rate and a role as an predictor of poor outcome [21]. Similarly Park et al reported a 47% protein expression rate using a polyclonal antibody (Zymed laboratories, South San Francisco, USA) and correlated overexpression with a higher incidence of postoperative recurrence [12]. Conversely, Schuell et al demonstrated an overexpression rate of 4% using the validated HercepTest. This did not correlate with survival [22, 23]. The HER-2 overexpression rate of 11% demonstrated in the current study may approach significance in relation to poor prognosis in a larger patient cohort. The methodology utilised is internationally validated in selecting patients who undergo treatment with Herceptin for metastatic breast cancer.
A phase II trial in conjunction with the National Cancer Institute demonstrated low levels of HER-2 overexpression (8%) however when these patients with metastatic colorectal cancer were treated with Herceptin in combination with irinotecan 5 of 7 patients who overexpressed it responded to therapy [24]. Under the current staging system within a specific stage a variable spectrum of outcome exists (> 25% in stage II disease). The development of gene signatures may unfold subsets within a given stage who have a worse prognosis and therefore require different adjuvant therapies [25]. One of these genes may be the HER-2/neu gene.
Conclusion
We have not demonstrated compelling evidence supporting a potential role for Herceptin in colorectal carcinoma as shown in breast cancer. Similarly we have not revealed that it is an important prognostic indicator. Some patients who overexpress HER-2 (11%) will respond to Herceptin. The evolution of signature genes in colorectal cancer and molecular profiling may facilitate identification of the small subset of patients overexpressing HER-2 who will have a favourable response to Herceptin therapy.
References
Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ: Cancer statistics. Ca Cancer J Clin. 2003, 53: 5-26.
Steele RJC: Colorectal Surgery . 2005, Elsevier, 3: 41-67.
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F: Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. New Engl J Med. 2004, 3:350 (23): 2335-42. 10.1056/NEJMoa032691.
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL: Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987, 9;235 (4785): 177-82. 10.1126/science.3798106.
Leonard DS, Hill AD, Kelly L, Djikstra B, McDermott E, O' Higgins NJ: Anti-human epidermal growth factor receptor 2 monoclonal antibody therapy for breast cancer. Br J Surg. 2002, 89 (3): 262-71. 10.1046/j.0007-1323.2001.02022.x.
Olayioye MA, Neve RM, Lane HA, Hynes NE: The erbβ signalling network: heterodimerisation in development and cancer. EMBO J. 2000, 19: 3159-67. 10.1093/emboj/19.13.3159.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L: Use of chemotherapy plus a monoclonal antibody against HER-2 for metastatic breast cancer that over expresses HER-2. N Engl J Med. 2001, 344: 783-792. 10.1056/NEJM200103153441101.
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, Slamon DJ, Murphy M, Novotny WF, Burchmore M, Shak S, Stewart SJ, Press M: Efficacy and safety of trastuzumab as a single agent in first line treatment of HER-2 over expressing metastatic breast cancer. J Clin Oncol. 2002, 20 (3): 719-726. 10.1200/JCO.20.3.719.
Mann M, Sheng H, Shao J, Williams CS, Pisacane PI, Sliwkowski MX, DuBois RN: Targeting cyclooxygenase 2 and HER-2/neu pathway inhibits colorectal carcinoma growth. Gastroenterology. 2001, 120: 1713-9. 10.1053/gast.2001.24844.
Ross JS, McKenna BJ: The HER-2/neu oncogene in tumours of the gastrointestinal tract. Cancer Invest. 2001, 19: 554-68. 10.1081/CNV-100103852.
Osako T, Miyhara M, Inomata M, Kitano S, Kobayashi M: Immunohistochemical study of c-erbB-2 protein in colorectal cancer and the correlation with patient survival. Oncology. 1998, 55: 549-55. 10.1159/000011911.
Park DI, Kang MS, Oh SJ, Kim HJ, Cho YK, Sohn CI, Jeon WK, Kim BI, Han WK, Kim H, Ryu SH, Sepulveda AR: HER-2/neu overexpression is an independent prognostic factor in colorectal cancer. Int J Colorectal Dis. 2007, 22: 491-7. 10.1007/s00384-006-0192-8.
Caruso ML, Valentini AM: Immunohistochemical p53 overexpression correlated to c-erbB2 and cathepsin D proteins in colorectal cancer. Anticancer Res. 1996, 16: 3813-8.
Kapitanovic S, Radosevic S, Kapitanovic M, Andelinovic S, Ferencic Z, Tavalossi M, Primorać D, Sonicki Z, Spaventi S, Pavelic K, Spaventi R: The expression of p185 (HER-2/neu) correlates with the stage of disease and survival in colorectal cancer. Gastroenterology. 1997, 112: 1103-13. 10.1016/S0016-5085(97)70120-3.
McKay JA, Loane JF, Ross VG, Ameyaw MM, Murray GI, Cassidy J, McLeod HL: C-erbB-2 is not a major factor in the development of colorectal cancer. Br J Canc. 2002, 86: 568-573. 10.1038/sj.bjc.6600127.
D'Emilia J, Bulovas K, D'Ercole K, Wolf B, Steele G, Summerhayes IC: Expression of c-erbB2 gene product (p185) at different stages of neoplastic progression in the colon. Oncogene. 1989, 4: 1233-39.
Essapen S, Thomas H, Green M, De Vries C, Cook MG, Marks C, Topham C, Modjtahedi H: The expression and prognostic significance of HER-2 in CRC. Int J Oncol. 2004, 24 (20): 241-8.
Half E, Broaddus R, Danenburg KD, Danenburg PV, Ayers GD, Sinicrope FA: HER-2 receptor expression, localisation and activation in colorectal cancer cell lines and human tumours. Int J Cancer. 2004, 108: 540-548. 10.1002/ijc.11599.
Pauletti G, Godolphin W, Press MF, Slamon DJ: Detection and quantification of HER-2/neu gene amplification in human breast cancer archival material using fluorescence in situ hybridisation. Oncogene. 1996, 13: 63-72.
Winston JS, Ramanaryanan J, Levine E: HER-2/neu evaluation in breast cancer are we there yet?. Am J Clin Pathol. 2004, 121 (Suppl): S33-49.
Lazaris AC, Theodoropoulos GE, Anastassopulos T, Nakopoulou L, Panoussopoulos D, Papadimitriou K: Prognostic significance of p53 and c-erbB2 immunohistochemical evaluation in colorectal adenocarcinoma. Histol Histopathol. 1995, 10 (3): 661-8.
Schuell B, Gruenberger T, Scheithauer W, Zielinski Ch, Wrba F: Her-2/neu protein expression in colorectal cancer. BMC Cancer. 2006, 6: 123-10.1186/1471-2407-6-123.
Nathanson DR, Culliford AT, Shia J, Chen B, D'Alessio M, Zeng ZS, Nash GM, Gerald W, Barany F, Paty PB: Her-2/neu expression and gene amplification in colon cancer. Int J Cancer. 2003, 105: 796-802. 10.1002/ijc.11137.
Ramanathan RK, Hwang JJ, Zamboni WC, Sinicrope FA, Safran H, Wong MK, Earle M, Brufsky A, Evans T, Troetschel M, Walko C, Day R, Chen HX, Finkelstein S: Low expression of HER-2/neu in advanced colorectal cancer limits the usefulness of trastuzumab (Herceptin) and irinotecan therapy. A phase II trial. Cancer Invest. 2004, 22 (6): 858-65. 10.1081/CNV-200039645.
Jiang Y, Casey G, Lavery IC, Zhang Y, Talantov D, Martin-McGreevy M, Skacel M, Manilich E, Mazumder A, Atkins D, Delaney CP, Wang Y: Development of a Clinically Feasible Molecular Assay to Predict Recurrence of Stage II Colon Cancer. J Mol Diagn. 2008, 10 (4): 346-54. 10.2353/jmoldx.2008.080011.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/9/1/prepub
Acknowledgements
We would like to thank Astrazeneca, Ireland for their contribution to the funding of this project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DK designed and conducted the study. He prepared the manuscript and did the statistical analysis. GC collected the clinicopathological data. LOG performed the laboratory work. KB, RW and PW prepared and corrected the manuscript. FB and IB reviewed the slides, prepared the images and reviewed the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kavanagh, D.O., Chambers, G., O' Grady, L. et al. Is overexpression of HER-2 a predictor of prognosis in colorectal cancer?. BMC Cancer 9, 1 (2009). https://doi.org/10.1186/1471-2407-9-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-9-1