Abstract
Background
Mucinous ovarian carcinoma have a poorer prognosis compared with other histological subtypes. The aim of this study was to evaluate, retrospectively, the activity of chemotherapy in patients with platinum sensitive recurrent mucinous ovarian cancer.
Methods
The SOCRATES study retrospectively assessed the pattern of care of a cohort of patients with recurrent platinum-sensitive ovarian cancer observed in the years 2000–2002 in 37 Italian centres. Data were collected between April and September 2005. Patients with recurrent ovarian cancer with > 6 months of platinum free interval were considered eligible.
Results
Twenty patients with mucinous histotype and 388 patients with other histotypes were analyzed. At baseline, mucinous tumours differed from the others for an higher number of patients with lower tumor grading (p = 0.0056) and less advanced FIGO stage (p = 0.025). At time of recurrence, a statistically significant difference was found in performance status (worse in mucinous, p = 0.024). About 20% of patients underwent secondary cytoreduction in both groups, but a lower number of patients were optimally debulked in the mucinous group (p = 0.03). Patients with mucinous cancer received more frequently single agent platinum than platinum based-combination therapy or other non-platinum schedules as second line therapy (p = 0.026), with a response rate lower than in non-mucinous group (36.4% vs 62.6%, respectively, p = 0.04). Median time to progression and overall survival were worse for mucinous ovarian cancer. Finally, mucinous cancer received a lower number of chemotherapy lines (p = 0.0023).
Conclusion
This analysis shows that platinum sensitive mucinous ovarian cancer has a poor response to chemotherapy. Studies dedicated to this histological subgroup are needed.
Similar content being viewed by others
Background
Mucinous carcinoma of the ovary accounts for 5–10% of all primary epithelial ovarian cancer [1]. Patients with mucinous ovarian cancer generally undergo the same first- and second-line treatment as patients with other histological subtypes [2]. However, very few reports in the literature have been published on this topic and activity of chemotherapy has been described in a limited number of patients and only in the first-line setting [3–6]. It has recently been shown in two different series of 27 and 45 patients, that advanced mucinous ovarian carcinoma have a poor response to first line chemotherapy [3, 6]. Thus, resistance to chemotherapy has been claimed as one of the main cause of the worse prognosis of mucinous ovarian cancer [3].
The SOCRATES (Study of an Ovarian Cancer cohort Recurred After first-line Treament: a rEstrospectivy Survey) study was planned to retrospectively assess the pattern of care of patients with recurrent platinum-sensitive ovarian cancer observed in Italy in the years 2000–2002 [7]. Using this cohort of patients we evaluated the response of mucinous cancer to chemotherapy in the recurrent setting.
Methods
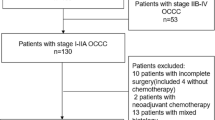
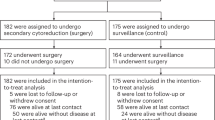
Patients with recurrent advanced ovarian cancer and a recurrence free interval (RFI) longer than 6 months were considered eligible for the study. The patients were observed in the years 2000–2002 in 37 Italian centres. Data were collected between April and September 2005. Four-hundred-ninety-three patient files were screened and 408 were considered eligible and analyzed in the present study.
The descriptive analysis of the data has been performed in 2 different subgroups identified according to histology: mucinous cancer and non-mucinous cancer. No central pathology assessment of the cancer samples was done.
Clinical, pathological and treatment characteristics at initial diagnosis, as well as at recurrence, including surgical and medical treatment (up to 6 lines of chemotherapy) of the recurrence were considered. Response rate was calculated considering RECIST [8] or Ca 125 criteria [9].
Overall survival was defined as the time elapsed between recurrence diagnosis and the date of death or the date of last follow-up information for live patients. Time to progression and overall survival were described y the Kaplan-Meier product limit method [10].
Differences among baseline variables were analyzed by the Student t test and Wilcoxon rank test for quantitative variables, and by the Mantel Haenszel test and the Chi-square method for the qualitative variables. Differences were considered statistically significant when p < 0.05.
All analysis was done using SAS® (SAS Institute Inc., Cary, NC, USA-version 9.1.3) statistical software.
Results
Mucinous tumors were diagnosed in 20 patients, as compared with 388 patients with other histological subtypes (table 1). Median age, performance status, results of primary surgery were similar between the two groups. In mucinous ovarian cancer, the grading of the tumors was lower than in the other subtypes (p = 0.0056) and stage at diagnosis was less advanced (p = 0.025)
The main characteristics of the patients at time of recurrence are shown in table 2. A statistically significant difference was found in performance status, that was worse in the mucinous group (p = 0.024), while no differences were found in the number of disease sites, age and recurrence free interval.
About 20% of patients underwent secondary cytoreduction in both groups, with a lower number of patients optimally debulked (no residual disease) in the group of patients with mucinous cancer (p = 0.03). The majority of patients with mucinous tumours had increased CA 125 levels at recurrence (85%).
Details on second-line chemotherapy are shown in the table 3. Patients with mucinous cancer received as second line therapy more frequently single agent platinum (42.1%) than platinum-combination therapy (31.6%) or other non-platinum chemotherapy (26.3%) (p = 0.026). The response rate (CR + PR) to the second line chemotherapy was lower in mucinous cancer than in non-mucinous one (36.4% vs 62.6%, respectively, p = 0.04). Moreover, patients with mucinous cancer received a lower number of lines of chemotherapy as compared to the other histotypes (p = 0.0023). Median progression free survival was 4.5 months in the mucinous and 8 months in non-mucinous group (p = 0.0292). Overall median survival from recurrence was 17.9 months in the mucinous and 28.8 months in non-mucinous group (p = 0.0028) (Figure 1).
In the mucinous cancer group responses were obtained with carboplatin, cisplatin, and carboplatin/paclitaxel (2 responses in patients with 6–12 months and 2 responses in patients with > 12 recurrence free interval). Among patients treated with non platinum-agents, no response was observed at second line, while responses were achieved in third-fourth line with paclitaxel (1/2 patients), topotecan (1/4 patients) and cyclophosphamide (1/1); no activity was observed with liposomal doxorubicin (0/4 patients) and gemcitabine (0/1 patient).
Discussion
This retrospective study indicates that recurrent mucinous ovarian cancer has a lower response rate to chemotherapy and a worst prognosis compared to non-mucinous subtypes. Moreover, patients receive less chemotherapy lines for recurrence as compared to other histotypes and when undergo secondary cytoreduction, this is less effective. At our knowledge, this analysis describes for the first time the response rate to second line chemotherapy in patients with platinum sensistive mucinous ovarian cancer. At baseline, the only main characteristic differentiating mucinous from non-mucinous tumour was the lower grade of the cancer, according to what previously observed [4]. Although we have not enough data to state that the poor response to chemotherapy is related to the lower grade of the tumours, it is possible to speculate that recurrent low grade cancer may benefit from a more aggressive attempt of cytoreduction before medical therapy. Unfortunately, in our series the patients that underwent secondary cytoreduction did not achieve the goal of obtaining an absence of residual disease; of course, the small number of patients does not allow to reach a definitive conclusion regarding the role of surgery in the treatment of recurrent mucinous ovarian cancer. No other disease related characteristics differed between mucinous and non-mucinous patients at recurrence.
Mucinous carcinomas of the ovary includes 5–10% of ovarian carcinomas, although recent refinements in the interpretation of the histological features of noninvasive and metastatic mucinous carcinomas suggest that this may be an overestimate [1, 11]. Clinical stage is the most important predictor of survival in mucinous ovarian carcinoma. The early stages confer a better overall prognosis for survival [11, 12], while the advanced disease has been associated with a poorer survival compared to the other histological subgroups [11–13].
The rarity of the disease is the main reason of the paucity of literature data regarding the activity of chemotherapy in this entity. Cloven [14] have shown, "in vitro", that the frequency of extreme drug resistance to chemotherapeutic agents differs significantly among histological subtypes of epithelial ovarian cancer. These authors demonstrated that mucinous ovarian cancer cells are more frequently resistant to cisplatin, but less frequently resistant to topotecan and doxorubicin compared to papillary serous tumors [14], however clinical data are lacking.
In a case-controlled study Hess [3] showed, on 27 mucinous and 54 other histological types,, that patients with advanced mucinous ovarian cancer have a poorer response to platinum-based first-line chemotherapy compared with patients with other histological subtypes, along with a worse survival. In this series, only 37% of the patients were treated with carboplatin/paclitaxel combination as first-line treatment, while the remainder received carboplatin alone or platinum plus anthracyclines. The overall response rate was 26% in first-line chemotherapy, while the response rate in second- and third-line chemotherapy was not reported [3]. A poor response to first line chemotherapy has been described by the Hellenic Cooperative Group [6]. In a previous study, we also showed in 21 consecutive patients with mucinous ovarian cancer treated in a single institution that the response rate to first line chemotherapy was significantly lower than that found in the other histological subgroups, with paclitaxel being the only drug showing activity in second line [4].
Platinum-sensitive recurrent ovarian cancer is usually treated with carboplatin/paclitaxel or carboplatin/gemcitabine, based on the trials showing superiority of combination chemotherapy versus single agent carboplatin [15, 16]. In our study an higher proportion of patients with mucinous cancer was treated at recurrence with single agent platinum than with platinum based combination therapy or other non platinum agents. Data clearly indicate that patients with recurrent mucinous ovarian cancer with a recurrence free interval higher than 6 months can respond to a platinum re-treatment, although the response rate is lower than that observed in non-mucinous cancer. Overall, recurrent mucinous cancer patients receive less chemotherapy lines than the others, probably also due to the lack of data in the literature showing activity for the chemotherapy agents more frequently used in this disease.
Here we report for the first time some responses to paclitaxel, topotecan and cyclophosphamide, while no response was observed with liposomal doxorubicin and gemcitabine. Overall the response rate to non-platinum agents was quite poor.
A possible limitation of our report is the retrospective nature of the analysis: therefore, survival data should be interpreted with caution. Another weakness of the study may be the lack of a central pathology review, to confirm these were mucinous ovarian cancers versus metastatic malignancies of gastrointestinal origin. However, the differential diagnosis between gastrointestinal and ovarian cancer is a major problem at time of initial diagnosis. In fact, in the case of our series of recurrent ovarian cancer this limitation may be less important since it is likely that during the disease free interval the potential presence of a primary gastrointestinal cancer would have been diagnosed. Moreover, a worse performance status was found in patients with mucinous tumors: however, due to the small number of patients, no definite conclusions can be drawn regarding the potential effect of performance status on the poor survival of patients with mucinous tumors.
Conventional parameters used to predict the clinical behaviour of advanced ovarian cancer may not adequately correlate with prognosis in mucinous carcinoma. Several studies have shown that mucinous ovarian cancer has a different pattern of expression of some molecular factors compared to the other subtypes. It is possible that a better understanding of tumour biology may help in determining which patients with mucinous ovarian cancer would benefit from traditional chemotherapy or should receive alternative chemotherapy agents. Several studies have shown that RAS mutations (specifically at KRAS codon 12) are prevalent in ovarian cancers of mucinous histology but not in tumors of non-mucinous histologies [17, 19]. On the contrary, mutation of p53, which is considered important in defining sensitivity to paclitaxel, is less frequent in mucinous tumors [20]. Again, some studies have found that the expression of COX-2 was much less frequent in mucinous cancer than in serous and endometroid ovarian cancers [21, 22]. Chemotherapy decisions tailored to the biology of mucinous ovarian cancer should be investigated in the future. The rarity of the disease should not discourage the assessment, in clinical trials, of the activity of different drugs, choosing first among those active in gastrointestinal cancer. Furthermore, "in vitro" drug response assays could be very useful to select patients that are likely to be resistant to traditional chemotherapy for whom to suggest an alternative, experimental treatment.
Conclusion
In conclusion, we showed that mucinous ovarian cancer has a poor response to chemotherapy in the recurrence setting along with a worst prognosis. Responses to platinum re-treatment are less frequent than in non-mucinous cancer, while anecdotal responses occur with non-platinum agents. Studies with alternative chemotherapy combinations are mandatory in this histological subgroup.
References
Harrison ML, Jameson G, Gore ME: Mucinous ovarian cancer. Int J Gynecol Oncol. 2007
du Bois A, Quinn M, Thigpen T, Vermorken J, Avall-Lundqvist E, Bookman M, Bowtell D, Brady M, Casado A, Cervantes A, Eisenhauer E, Friedlaender M, Fujiwara K, Grenman S, Guastalla JP, Harper P, Hogberg T, Kaye S, Kitchener H, Kristensen G, Mannel R, Meier W, Miller B, Neijt JP, Oza A, Ozols R, Parmar M, Pecorelli S, Pfisterer J, Poveda A, Provencher D, Pujade-Lauraine E, Randall M, Rochon J, Rustin G, Sagae S, Stehman F, Stuart G, Trimble E, Vasey P, Vergote I, Verheijen R, Wagner U, Gynecologic Cancer Intergroup; AGO-OVAR; ANZGOG; EORTC; GEICO; GINECO; GOG; JGOG; MRC/NCRI; NCIC-CTG; NCI-US; NSGO; RTOG; SGCTG; IGCS; Organizational team of the two prior International OCC: 2004 consensus statements on the management of ovarian cancer: final document of the 3rd International Gynecologic Cancer Intergroup Ovarian Cancer Consensus Conference (GCIG OCCC 2004). Ann Oncol. 2005, viii7-12. 10.1093/annonc/mdi961. Suppl 8
Hess V, A'Hern R, Nasiri N, King DM, Blake PR, Barton DP, Shepherd JH, Ind T, Bridges J, Harrington K, Kaye SB, Gore ME: Mucinous epithelial ovarian cancer: a separate entity requiring specific treatment. J Clin Oncol. 2004, 22: 1040-1044. 10.1200/JCO.2004.08.078.
Pisano C, Greggi S, Tambaro R, Losito S, Iodice F, Di Maio M, Ferrari E, Falanga M, Formato R, Iaffaioli VR, Pignata S: Activity of chemotherapy in mucinous epithelial ovarian cancer: a retrospective study. Anticancer Res. 2005, 25: 3501-3505.
Enomoto T, Kuragakin C, Yamasaki M: Is clear cell carcinoma and mucinous carcinoma of ovary sensitive to combination chemotherapy with paclitaxel and carboplatin?. Proc Am Soc Clin Oncol. 2003, 22 (A1797): 447-
Pectasides D, Fonutrilas G, Aravantinos G, Kalofanos HP, Efstathion E, Salamalekis E: stage mucinous epithelial ovarian cancer; the Hellenic Cooperative Oncology Group experience. Gynecol Oncol. 2005, 99: 788-790. 10.1016/j.ygyno.2005.07.022.
Pignata S, Ferrandina G, Scarfone G, Scollo P, Odicino F, Selvaggi L, Katsaros D, Frigerio L, Mereu L, Grezzi F, Manzione L, Lauria R, Breda E, Martorio G, Ballardini M, Vernaglia Lombardi A, Sorio R, Tumolo S, Costa B, Magni G, Perrone F, Favalli G: Extending the platinum-free interval with a non platinum therapy in platinum sensitive recurrent ovarian cancer: results from the SOCRATES retrospective study. Oncology. 2007, 71: 320-326. 10.1159/000108592.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG: New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000, 92: 205-216. 10.1093/jnci/92.3.205.
Rustin GJ, Nelstrop AE, McClean P, Brady MF, McGuire WP, Hoskins WJ, Mitchell H, Lambert HE: Defining response of ovarian carcinoma to initial chemotherapy according to serum Ca 125. J Clin Oncol. 1996, 14: 1545-1550.
Kaplan EL, Meier P: Non parametric estimation from incomplete observation. J Am Stat Assoc. 1958, 53: 457-481. 10.2307/2281868.
Kikkawa F, Nawa A, Kajiyama H, Shibata K, Ino K, Nomura S: Clinical Charcateristics and prognosis of mucinous tumours of the ovary. Gynecol Oncol. 2006, 103: 171-175. 10.1016/j.ygyno.2006.02.015.
McGuire V, Jesser CA, Whittemore AS: Survival among U.S. women with invasive epithelial ovarian cancer. Gynecol Oncol. 2002, 84: 399-403. 10.1006/gyno.2001.6536.
Omura GA, Brady MF, Homesley HD, Yordan E, Major FJ, Buchsbaum HJ, Park RC: Long-term follow-up and prognostic factor analysis in advanced ovarian carcinoma: The Ginecologic Oncology Group experience. J Clin Oncol. 1991, 9: 1138-1150.
Cloven NG, Kyshtoobayeva A, Burger RA, Yu IR, Fruehauf JP: In vitro chemoresistance and biomarker profiles are unique for histologic subtypes of epithelial ovariancancer. Gynecol Oncol. 2004, 92: 160-6. 10.1016/j.ygyno.2003.09.030.
Parmar MK, Ledermann JA, Colombo N, du Bois A, Delaloye JF, Kristensen GB, Wheeler S, Swart AM, Qian W, Torri V, Floriani I, Jayson G, Lamont A, Trope C, ICON and AGO Collaborators: Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: the ICON4/AGO-OVAR-2.2 trial. Lancet. 2003, 361: 2099-2106. 10.1016/S0140-6736(03)13718-X.
Pfisterer J, Plante M, Vergote I, du Bois A, Hirte H, Lacave AJ, Wagner U, Stahle A, Stuart G, Kimmig R, Olbricht S, Le T, Emerich J, Kuhn W, Bentley J, Jackisch C, Luck HJ, Rochon J, Zimmermann AH, Eisenhauer E, AGO-OVAR; NCIC CTG; EORTC GCG: Gemcitabine/carboplatin (GC) vs. carboplatin (C) in platinum sensitive recurrent ovarian cancer (OVCA). J Clin Oncol. 2006, 24: 4699-707. 10.1200/JCO.2006.06.0913.
Enomoto T, Weghorst CM, Inoue M, Tanizawa O, Rice JM: K-ras activation occur frequently in mucinous adenocarcinomas and rarely in other common epithelial tumors of the ovary. J Pathol. 1991, 139: 777-85.
Ichikawa Y, Nishida M, Suzuki H, Yoshida S, Tsunoda H, Kubo T, Uchida K, Miwa M: Mutation of K-ras protooncogene is associated with histological subtype in human mucinous ovarian tumors. Cancer Res. 1994, 54: 33-5.
Cuatrecasas M, Villanueva A, Matias-Guiu X, Prat J: K-ras mutations in mucinous ovarian tumors: a clinicopathologic and molecular study of 95 cases. Cancer. 1997, 79: 1581-6. 10.1002/(SICI)1097-0142(19970415)79:8<1581::AID-CNCR21>3.0.CO;2-T.
Reles A, Wen WH, Schmider A, Gee C, Runnebaum IB, Kilian U, Jones LA, El-Naggar A, Minguillon C, Schönborn I, Reich O, Kreienberg R, Lichtenegger W, Press MF: Correlation of p53 mutation to platinum-based chemotherapy and shortened survival in ovarian cancer. Clin Cancer Res. 2001, 7 (10): 2984-2997.
Matsumoto Y, Ishiko O, Deguchi M, Nakagawa E, Ogita S: Cyclooxigenase-2 expression in normal ovaries and epithelial ovarian neoplasm. Int J Mol Med. 2001, 8: 31-6.
Denkert C, Köbel M, Pest S, Koch I, Berger S, Schwabe M, Siegert A, Reles A, Klosterhalfen B, Hauptmann S: Expression of cyclooxygenase 2 is an independent prognostic factor in human ovarian carcinoma. Am J Pathol. 2002, 160: 893-903.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/8/252/prepub
Acknowledgements
The SOCRATES project was supported by an unrestricted grant from GSK Italy. The MITO group is supported by a project grant from Associazione Italiana per la Ricerca sul Cancro. The authors remember Giovanni Favalli, recently deceased, that was a member of the SOCRATES board.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SP, GF, GS, PS participated in the design of the study; GM performed the statistical analysis. SP conceived of the study, and participated in its design and coordination. FO, GC, DK, AV, LM, FG, LM, RL, EB, DGA, MB, AVL, RS, GM, DP, AM significantly contributed to data collection. All authors read and approved the final manuscript. Additional co-authors and participating institution are listed in the additional file 1.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Pignata, S., Ferrandina, G., Scarfone, G. et al. Activity of chemotherapy in mucinous ovarian cancer with a recurrence free interval of more than 6 months: results from the SOCRATES retrospective study. BMC Cancer 8, 252 (2008). https://doi.org/10.1186/1471-2407-8-252
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-8-252