Abstract
Background
Abnormal hemostasis in cancer patients has previously been described, however the correlation between the plasma fibrinogen level and cancer metastasis and prognosis has not been reported in a large-scale clinical study.
Methods
Preoperative plasma fibrinogen levels were retrospectively examined in 405 patients who underwent surgery for advanced gastric cancer. The association of fibrinogen levels with clinical/pathological findings and clinical outcome was evaluated.
Results
There was a positive correlation between plasma fibrinogen levels and the depth of invasion (p < 0.05). Hyperfibrinogenemia (>310 mg/dl) was independently associated with lymph node (Odds Ratio; 2.342, P = 0.0032) and liver (Odds Ratio; 2.933, P = 0.0147) metastasis, not with peritoneal metastasis in this series. Patients with hyperfibrinogenemia showed worse clinical outcome in T2 gastric cancer, however, there was no correlation of plasma fibrinogen level with prognosis in T3/T4 gastric cancer.
Conclusion
Our results might support the idea that hyperfibrinogenemia can augment lymphatic and hematogeneous metastasis of advanced gastric cancer, which is major determinant of the prognosis in T2 gastric cancer. Therefore, in the situation without peritoneal involvement, hyperfibrinogenemia is a useful biomarker to predict the possible metastasis and worse clinical outcome in T2 gastric cancer.
Similar content being viewed by others
Background
An increased frequency of thrombosis in patients with gastrointestinal cancer was first documented in 1865 [1]. Since then, a number of studies have focused on the relationship between various cancers and hemostatic factors. Abnormalities in blood coagulation are detectable in patients with malignancy, including thrombocytosis and elevated markers of coagulation activation such as fragment 1+2, thrombin-antithrombin III complexes (TAT), fibrinopeptide A (FPA), and D-Dimer [2–4]. More recently, a correlation between these factors and the prognosis of malignancies was documented. Thrombocytosis is thought to be associated with poor prognosis in gastric cancer [5], as well as esophageal cancer [6], lung cancer [7], colon cancer [7], renal cell carcinoma [8], and gynecological malignancies [9], D-Dimer is also reported to be associated with poor prognosis in patients with lung cancer [10, 11] and colorectal cancer [12, 13] as well as being a good predictor of survival and disease progression.
Fibrinogen, an essential hemostatic factor, is converted to fibrin (a final product of the hemostatic pathway) by activated thrombin. Dvorak suggested that elevated fibrinogen concentrations were frequently observed in cancer patients with malignant disease [14]. Moreover, in gastric cancer, preoperative plasma fibrinogen levels correlate with extent of tumor [15]. In our previous study, we found that preoperative plasma fibrinogen level was a useful predictor for lymph node metastasis in patients with gastric cancer [16]. Tumor marker carcinoembryonic antigen (CEA) as well as inflammatory biomarker C-reactive protein (CRP) did not show the independent association with lymph node metastasis, suggesting that hyperfibrinogenemia was not a simple result of cancer progression and might support the metastatic process by providing beneficial microenvironment around the tumor. This idea can be partially supported by recent studies in fibrinogen-deficient mice that revealed hematogeneous and lymphatic metastases were greatly reduced, indicating the positive roles of fibrinogen in the metastatic progression of cancer [17–19]. Taken together with our previous results, we hypothesized that fibrinogen might augment metastasis in human as well, and a higher level of plasma fibrinogen might be a good clinical marker of metastatic disease and worse clinical outcome. Based on this assumption, we focused on the possible impact of preoperative plasma fibrinogen level on gastric cancer prognosis. We retrospectively examined the preoperative plasma fibrinogen level of patients with advanced gastric cancer who underwent gastrectomy, and evaluated an association of these findings with clinical and pathological factors as well as clinical outcome.
Methods
A total of 442 patients with advanced gastric cancer underwent gastrectomy between January 1985 and December 1999 at the First Department of Surgery, University of Tokyo Hospital, Tokyo. Oral consent was obtained from each patient for blood test. Among them, plasma fibrinogen levels were evaluated before surgery in 424 patients. Because the plasma fibrinogen level is critically affected by the presence of inflammation, liver cirrhosis and chronic renal failure, five patients with apparent acute inflammatory disease (two with acute cholecystitis, three with acute peritonitis due to stomach perforation), 10 patients with liver cirrhosis and four patients with chronic renal failure were excluded from the study to minimize confounding factors. The remaining 405 patients were enrolled in this study. We also evaluated fibrinogen levels in 387 patients with early gastric cancer and 124 patients with non-inflammatory benign disease who underwent surgery during the same period. Our protocol was approved by the ethics committee of faculty of medicine, the University of Tokyo.
In this study we referred to the classifications established by the Japanese Research Society for Gastric Cancer [20] which define T1 as a lesion confined to the mucosal or submucosal layer; T2 as a tumor invading the proper muscle layer or subserosa; T3 as a tumor penetrating serosal without invasion of adjacent structures; and T4 as a tumor invading adjacent structures. Histological classifications were defined as follows: differentiated carcinoma – well and moderately differentiated tubular adenocarcinoma and papillary adenocarcinoma; undifferentiated carcinoma – poorly differentiated adenocarcinoma, signet ring cell carcinoma and mucinous carcinoma.
The preoperative plasma fibrinogen level was measured from early morning samples taken before breakfast five to ten days before surgery. It had been determined by Clauss clotting method using DADE Thrombin Reagent™ and Coagrex-700™ automated coagulometer (both from Sysmex, Kobe, Japan). The reference range of plasma fibrinogen level was defined as between 210 and 310 mg/dl according to the mean value ± 2 SD of healthy volunteers; plasma fibrinogen levels above 310 mg/dl were defined as hyperfibrinogenemia tentatively in this study.
Statistical analysis was carried out using JMP 5.1 (SAS Institute, Cary, NC). Plasma fibrinogen levels were compared with one-way ANOVA followed by the SNK test. The association of fibrinogen levels with clinicopathological factors was assessed with Fisher's exact test. A multivariate stepwise logistic regression analysis was performed to identify independent variables that were correlated with hematogenous and lymphatic metastasis. The Kaplan-Meier method was used to estimate the distribution of survival curve, and log-rank test was used to compare the distributions between the groups with or without hyperfibrinogenemia. P < 0.05 was considered significant for all statistical analyses.
Results
The association of plasma fibrinogen level with the depth of invasion and metastatic disease in gastric cancer
The mean ± standard deviation (SD) plasma fibrinogen level in the 792 patients studied was 289.5 ± 81.3 mg/dl, which was not statistically different from patients with benign disease (278.1 ± 43.5) (Figure 1). However, when patients were classified into 3 groups according to the T classification of gastric cancer, patients with T2 and T3/T4 cancer showed significantly higher fibrinogen levels than those with benign disease or those with T1 cancer (T2 304.3 ± 85.0, p < 0.01; T3/T4 327.8 ± 101.2, p < 0.01). Interestingly, an increase in the plasma fibrinogen level correlated with an increase in the depth of invasion, showing a statistically significant difference among patients when evaluated by ANOVA (p < 0.0001). The fibrinogen levels in patients with localized disease, lymph node metastases, liver metastasis and peritoneal metastasis were summarized in Table 1. In patients with localized disease, preoperative fibrinogen level (mean value; 266.6) was significantly lower than that in patients with lymph node metastasis (320.5; P < 0.0001), liver metastasis (356.6; P < 0.0001), peritoneal metastasis (345.0; P < 0.0001).
Plasma fibrinogen level of 124 patients with benign disease and 792 patients with gastric cancer. Note that there is no difference in fibrinogen levels between benign and cancer patients, although it gradually increases with increasing depth of cancer invasion (one way ANOVA with SNK test; p < 0.0001). Values are the mean (standard deviation) levels for individual patients. *The mean values of plasma fibrinogen were significantly different between the groups of T1 and T2 (P < 0.01), between the groups of T1 and T3/T4 (P < 0.01), and between the groups of T2 and T3/T4 (p < 0.01).
The association of hyperfibrinogenemia with lymph node, liver, and peritoneal metastasis in advanced gastric cancer
Of 405 patients with advanced cancer, lymph node metastases in 301 patients, liver metastases in 28, and peritoneal metastases in 41 were identified. Univariate analysis revealed that lymph node metastases were significantly associated with many pathologic factors such as size of the tumor, serosal invasion, lymphatic and venous involvement as well as plasma fibrinogen level (Table 2). Multivariate analysis indicated that hyperfibrinogenemia showed an independent association with lymph node metastases with an odds ratio of 2.342 (p < 0.01) (Table 3). Subsequently, we focused on distant hematogeneous and peritoneal metastases. In individuals with advanced gastric cancer, hyperfibrinogenemia showed a positive association with liver metastasis (p < 0.01), not with peritoneal dissemination, by univariate analysis (Table 2). Multivariate analysis showed that hyperfibrinogenemia, in addition to differentiated histology and venous involvement, remained independently associated with liver metastasis with an odds ratio of 2.933 (p < 0.05) (Table 3).
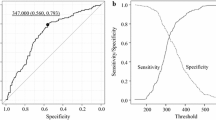
The clinical outcome in T2 and T3/T4 gastric cancer with or without hyperfibrinogenemia
In T2 gastric cancer, patients without hyperfibrinogenemia showed an extremely good outcome even in the population with advanced cancer, and the survival rate was significantly lower for patients with hyperfibrinogenemia (P = 0.001; log-rank test) (Figure 2A). In marked contrast, hyperfibrinogenemia did not show any correlation with 5-year survival rate in T3/T4 gastric cancer, i.e. cancer invading beyond the serosal (Figure 2B).
Overall survival after surgery for 240 patients with T2 gastric cancer (A) and 165 patients with T3/T4 gastric cancer (B) according to the existence of hyperfibrinogenemia. The group with hyperfibrinogenemia (>310 mg/dl) showed a significantly lower survival rate than another group (≤310 mg/dl) in T2 cancer. There was no statistically significant survival difference in T3/T4 cancer according to the plasma fibrinogen level.
Discussion
A link between hyperfibrinogenemia and cardiovascular diseases such as coronary heart disease, stroke and peripheral vascular disease was previously revealed [21]. Similarly, a recent study by Preston and colleagues indicates that fibrinogen production is upregulated in patients with pancreatic adenocarcinoma, although the tumor stage was not determined [22]. This suggests a positive role for fibrinogen in the progression of malignant diseases. In the present study we found that fibrinogen levels in patients with gastric cancer did not show statistically significant difference from those in individuals with benign diseases. However, the plasma fibrinogen level gradually increased with increasing depth of tumor, and the fibrinogen levels of patients with advanced gastric cancer were significantly higher than patients with benign diseases or early tumors. Moreover, the fibrinogen levels were also significantly higher in patients with metastatic disease, which essentially supports the previous study of another group [15]. Hyperfibrinogenemia is a clinically relevant event in advanced stage and our results strongly suggest that fibrinogen is involved in the progression of gastric cancer during the latter phase of the disease.
Recent studies in fibrinogen deficient mice provide clear evidence that fibrinogen plays a crucial role in hematogenous and lymphatic metastasis of cancer cells [18]. They showed that fibrinogen (Aα-chain)-deficient mice with intravenously transferred Lewis lung carcinoma (LLC) or B16 melanoma had a significantly reduced incidence of lung metastasis compared with wild type mice [17]. Also, the number of metastases in regional lymph nodes and the lungs of these transgenic mice was markedly reduced when LLC was subcutaneously inoculated [18]. These results raised the possibility that hyperfibrinogenemia might function to enhance metastasis formation as compared to the low fibrinogen level. As a fact, hyperfibrinogenemia showed an independent association with lymph node metastasis in human gastric cancer [16]. Interestingly, there was no remarkable difference in the growth of subcutaneously transplanted tumors between fibrinogen-deficient and wild type mice [18], indicating that fibrinogen plays a major role in the development of metastases but not in the growth of the primary tumor. This is exactly consistent with our human study in which patients with early gastric cancer had a similar plasma fibrinogen level to benign subjects.
In our study, we found that plasma fibrinogen level was associated with worse prognosis in T2 gastric cancer as well as lymphatic and hematogenous metastasis. The impact of hyperfibrinogenemia, however, was not found in T3/T4 gastric cancer. T3/T4 gastric cancers are serosal-infiltrating tumors, which enhances the potential to have occult metastatic foci on the peritoneum and/or form the overt peritoneal metastasis. As a fact, peritoneum is the major site of recurrence in T3/T4 gastric cancers [23–25], and the prognosis of T3/T4 cancers mainly determined by this type of recurrence. In contrast, T2 cancer has a less frequency of peritoneal metastasis as compared with T3/T4 cancer and liver or lymph node relapse seems to be major determinant of clinical outcome in T2 cancer. In our study, however, we found no association of hyperfibrinogenemia with peritoneal metastasis, although hyperfibrinogenemia was an independently associated factor with lymph node and liver metastasis. We speculate that peritoneal metastasis has a strong impact on the clinical outcome in T3/T4 gastric cancer and therefore plasma fibrinogen level was not a prognostic marker in this population. These results suggested that some patients with hyperfibrinogenemia could not be cured by surgical modalities in T2 gastric cancer and chemotherapy might be required for the improvement of survival in this population. The clinical benefit of neoadjuvant and/or adjuvant chemotherapy has not been clearly determined in T2 gastric cancer. From our data, we can conclude that patients with hyperfibrinogenemia might be good candidates for neoadjuvant and/or adjuvant chemotherapy in T2 gastric cancer. Patients with T3/T4 gastric cancer will be candidates regardless of the plasma fibrinogen level.
Fibrinogen may enhance metastasis through several possible mechanisms. Firstly, the soluble form of fibrinogen could serve as the bridging molecule between tumor cells and host cells. Fibrinogen is a dimeric molecule with multiple integrin or non-integrin binding motifs, and malignant cells often express high levels of fibrinogen receptors, such as α5β1, αvβ3 integrins or ICAM-1 molecule. If fibrinogen were to bind to ICAM-1 on endothelial cells, it might promote stable adhesion of tumor cells to the endothelium of target organs. In addition, tumor cells and platelets can form large aggregates through the binding of fibrinogen, because platelet αIIbβ3 integrin receptors have a high affinity for fibrinogen. These aggregates effectively form microemboli in target organs, which can protect tumor cells from the innate immune system [26, 27]. A study by Palumbo and colleagues found that the number of tumor cells located in the lung was markedly decreased in fibrinogen deficient mice after 4–24 hours of tumor inoculation, but at no earlier time points. This suggests that fibrinogen is essential for the sustained adherence of tumor cells to the endothelia of target organs [17].
Recent studies have shown that thrombin might also be an important modulator of cancer metastasis in vivo. During the conversion of prothrombin to thrombin by prothrombinase, the polypeptide prothrombin fragment 1+2 (F1+2) is released. The plasma F1+2 level is therefore a useful marker of thrombin generation. A number of studies have shown that F1+2 plasma levels are elevated in patients with specific types of malignancies [4, 28, 29] but not in other types [30–32]. Rahr and coworkers reported no difference in plasma F1+2 levels between patients with and without gastric cancer [32]. In the present study, prothrombin time (PT) was examined in each patient and no significant association with the presence of cancer, metastasis, tumor stage or plasma fibrinogen level was found (data not shown). Moreover, Kerlin and co-workers recently demonstrated that elevated fibrinogen levels in hyperfibrinogenemia transgenic mice with suppressed thrombin activity do not alter the incidence or extent of thrombus formation [33]. It therefore seems unlikely that high fibrinogen levels are associated with systemic thrombin activation and subsequent enhancement of fibrin formation in gastric cancer.
Although there is sufficient evidence to suggest that elevated fibrinogen levels might aid the development of metastatic lesions, we cannot ignore the possibility that this elevation is simply the result of the tumor mass spreading. Fibrinogen, which is one of the major acute phase proteins produced by the liver, is greatly enhanced in response to infection or other inflammatory disorders. Indeed, the fibrinogen level of all of the patients with preoperative acute inflammatory disorders was high. Inflammatory proteins, such as IL-6 or CRP, are reported to be higher in cancer patients compared to non-cancer patients. In our previous study, we found that CRP level did not show an independent association with lymphatic metastasis although plasma fibrinogen level did [16], suggesting that hyperfibrinogenemia, different from high serum CRP, may not be a simple by-product of inflammatory response caused by tumor progression but might have some etiologic relevance for tumor metastasis and accordingly relationship with clinical outcome in gastric cancer. In this retrospective study as well as our previous study, however, we could not show the exact causal relationship between hyperfibrinogenemia and cancer metastasis.
Conclusion
Metastasis is the unequivocal hallmark of cancer. The acquisition of metastatic ability leads to clinically incurable disease and resultingly worse clinical outcome for most cancer cell types. Our data, together with the results of basic experiments in previous studies, raises the idea that hyperfibrinogenemia causally imparts the hematogenous and lymphatic metastatic progression in patients with advanced gastric cancer, and is not simply the result of tumor progression. It also has a prognostic value in T2 gastric cancer, which might suggest hyperfibrinogenemia has the potential to be prognostic marker in other cancer type with less frequent peritoneal metastasis. Routinely examined plasma fibrinogen level is not only the factor to assess the perioperative hemorrhagic risk but also a useful biomarker to predict the possible metastasis and worse prognosis in T2 gastric cancer.
Abbreviations
- TAT:
-
fibrinopeptide A
- FPA:
-
carcinoembryonic antigen
- CEA:
-
C-reactive protein
- CRP:
-
Lewis lung carcinoma
- LLC:
-
prothrombin fragment 1+2
- F1+2:
-
prothrombin time PT
References
Trousseau A: Phlegmasia alba dolens. Clinique Medicale de L'Hotel Dieu de Paris. 1865, Paris , Balliere, 654-656. 2nd
Sun NC, McAfee WM, Hum GJ, Weiner JM: Hemostatic abnormalities in malignancy, a prospective study of one hundred eight patients. Part I. Coagulation studies. Am J Clin Pathol. 1979, 71 (1): 10-16.
Luzzatto G, Schafer AI: The prethrombotic state in cancer. Semin Oncol. 1990, 17 (2): 147-159.
Lopez Y, Paloma MJ, Rifon J, Cuesta B, Paramo JA: Measurement of prethrombotic markers in the assessment of acquired hypercoagulable states. Thromb Res. 1999, 93 (2): 71-78. 10.1016/S0049-3848(98)00165-0.
Ikeda M, Furukawa H, Imamura H, Shimizu J, Ishida H, Masutani S, Tatsuta M, Satomi T: Poor prognosis associated with thrombocytosis in patients with gastric cancer. Ann Surg Oncol. 2002, 9 (3): 287-291. 10.1245/aso.2002.9.3.287.
Shimada H, Oohira G, Okazumi S, Matsubara H, Nabeya Y, Hayashi H, Takeda A, Gunji Y, Ochiai T: Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg. 2004, 198 (5): 737-741. 10.1016/j.jamcollsurg.2004.01.022.
Costantini V, Zacharski LR, Moritz TE, Edwards RL: The platelet count in carcinoma of the lung and colon. Thromb Haemost. 1990, 64 (4): 501-505.
Symbas NP, Townsend MF, El-Galley R, Keane TE, Graham SD, Petros JA: Poor prognosis associated with thrombocytosis in patients with renal cell carcinoma. BJU Int. 2000, 86 (3): 203-207. 10.1046/j.1464-410x.2000.00792.x.
Hernandez E, Donohue KA, Anderson LL, Heller PB, Stehman FB: The significance of thrombocytosis in patients with locally advanced cervical carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2000, 78 (2): 137-142. 10.1006/gyno.2000.5838.
Unsal E, Atalay F, Atikcan S, Yilmaz A: Prognostic significance of hemostatic parameters in patients with lung cancer. Respir Med. 2004, 98 (2): 93-98. 10.1016/j.rmed.2003.07.001.
Buccheri G, Torchio P, Ferrigno D: Plasma levels of D-dimer in lung carcinoma: clinical and prognostic significance. Cancer. 2003, 97 (12): 3044-3052. 10.1002/cncr.11432.
Oya M, Akiyama Y, Okuyama T, Ishikawa H: High preoperative plasma D-dimer level is associated with advanced tumor stage and short survival after curative resection in patients with colorectal cancer. Jpn J Clin Oncol. 2001, 31 (8): 388-394. 10.1093/jjco/hye075.
Blackwell K, Hurwitz H, Lieberman G, Novotny W, Snyder S, Dewhirst M, Greenberg C: Circulating D-dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer. 2004, 101 (1): 77-82. 10.1002/cncr.20336.
Dvorak HF: Thrombosis and cancer. Hum Pathol. 1987, 18 (3): 275-284.
Lee JH, Ryu KW, Kim S, Bae JM: Preoperative plasma fibrinogen levels in gastric cancer patients correlate with extent of tumor. Hepatogastroenterology. 2004, 51 (60): 1860-1863.
Yamashita H, Kitayama J, Nagawa H: Hyperfibrinogenemia is a useful predictor for lymphatic metastasis in human gastric cancer. Jpn J Clin Oncol. 2005, 35 (10): 595-600. 10.1093/jjco/hyi150.
Palumbo JS, Kombrinck KW, Drew AF, Grimes TS, Kiser JH, Degen JL, Bugge TH: Fibrinogen is an important determinant of the metastatic potential of circulating tumor cells. Blood. 2000, 96 (10): 3302-3309.
Palumbo JS, Potter JM, Kaplan LS, Talmage K, Jackson DG, Degen JL: Spontaneous hematogenous and lymphatic metastasis, but not primary tumor growth or angiogenesis, is diminished in fibrinogen-deficient mice. Cancer Res. 2002, 62 (23): 6966-6972.
Palumbo JS, Talmage KE, Massari JV, La Jeunesse CM, Flick MJ, Kombrinck KW, Jirouskova M, Degen JL: Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood. 2005, 105 (1): 178-185. 10.1182/blood-2004-06-2272.
Japanese Gastric Cancer A: Japanese Classification of Gastric Carcinoma - 2nd English Edition. Gastric Cancer. 1998, 1 (1): 10-24. 10.1007/PL00011681.
Ernst E, Koenig W: Fibrinogen and cardiovascular risk. Vasc Med. 1997, 2 (2): 115-125.
Preston T, Slater C, McMillan DC, Falconer JS, Shenkin A, Fearon KC: Fibrinogen synthesis is elevated in fasting cancer patients with an acute phase response. J Nutr. 1998, 128 (8): 1355-1360.
Roukos DH, Lorenz M, Karakostas K, Paraschou P, Batsis C, Kappas AM: Pathological serosa and node-based classification accurately predicts gastric cancer recurrence risk and outcome, and determines potential and limitation of a Japanese-style extensive surgery for Western patients: a prospective with quality control 10-year follow-up study. Br J Cancer. 2001, 84 (12): 1602-1609. 10.1054/bjoc.2001.1720.
Moriguchi S, Maehara Y, Korenaga D, Sugimachi K, Nose Y: Risk factors which predict pattern of recurrence after curative surgery for patients with advanced gastric cancer. Surg Oncol. 1992, 1 (5): 341-346. 10.1016/0960-7404(92)90034-I.
Otsuji E, Kuriu Y, Ichikawa D, Okamoto K, Ochiai T, Hagiwara A, Yamagishi H: Time to death and pattern of death in recurrence following curative resection of gastric carcinoma: analysis based on depth of invasion. World J Surg. 2004, 28 (9): 866-869. 10.1007/s00268-004-7359-7.
Yano H, J. K, Hatano K, Tsuno N, Osada T, Watanabe T, Tsuruo T, Muto T, Nagawa H: Clustered cancer cells show a distinct adhesion behavior from single cell form under physiological shear conditions. J Exp Clin Cancer Res. 2001, 20 (3): 407-412.
Nieswandt B, Hafner M, Echtenacher B, Mannel DN: Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res. 1999, 59 (6): 1295-1300.
Iversen LH, Thorlacius-Ussing O: Relationship of coagulation test abnormalities to tumour burden and postoperative DVT in resected colorectal cancer. Thromb Haemost. 2002, 87 (3): 402-408.
Roselli M, Mineo TC, Basili S, Mariotti S, Martini F, Bellotti A, Ambrogi V, Spila A, D'Alessandro R, Gazzaniga PP, Guadagni F, Ferroni P: Vascular endothelial growth factor (VEGF-A) plasma levels in non-small cell lung cancer: relationship with coagulation and platelet activation markers. Thromb Haemost. 2003, 89 (1): 177-184.
Di Micco P, Romano M, Niglio A, Nozzolillo P, Federico A, Petronella P, Nunziata L, Di Micco B, Torella R: Alteration of haemostasis in non-metastatic gastric cancer. Dig Liver Dis. 2001, 33 (7): 546-550. 10.1016/S1590-8658(01)80105-5.
Wojtukiewicz MZ, Rucinska M, Zimnoch L, Jaromin J, Piotrowski Z, Rozanska-Kudelska M, Kisiel W, Kudryk BJ: Expression of prothrombin fragment 1+2 in cancer tissue as an indicator of local activation of blood coagulation. Thromb Res. 2000, 97 (5): 335-342. 10.1016/S0049-3848(99)00169-3.
Rahr HB, Sorensen JV, Larsen JF, Jensen FS, Bredahl C: Markers of coagulation and fibrinolysis in portal blood from patients with and without gastric malignancy. Scand J Gastroenterol. 1994, 29 (6): 516-521.
Kerlin B, Cooley BC, Isermann BH, Hernandez I, Sood R, Zogg M, Hendrickson SB, Mosesson MW, Lord S, Weiler H: Cause-effect relation between hyperfibrinogenemia and vascular disease. Blood. 2004, 103 (5): 1728-1734. 10.1182/blood-2003-08-2886.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/6/147/prepub
Acknowledgements
Studies were supported by a grant from a Grant-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan and by a Grant from the Ministry of Health and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
HY have been involved in preparing the manuscript for submission and made substantial contributions to conception and design, acquisition of data, and analyses and interpretation of data;
JK contributed to analyses and interpretation of data and their interpretation and was involved in revising the manuscript for important intellectual content;
NK and YY have been involved in plasma fibrinogen measurement and data analyses;
HN participated in the design of the study and was involved in discussion of the results.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Yamashita, H., Kitayama, J., Kanno, N. et al. Hyperfibrinogenemia is associated with lymphatic as well as hematogenous metastasis and worse clinical outcome in T2 gastric cancer. BMC Cancer 6, 147 (2006). https://doi.org/10.1186/1471-2407-6-147
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-6-147