Abstract
Background
Metastatic malignant melanoma to the liver resulting in fulminant hepatic failure is a rare occurrence.
Case presentation
A 46 year old man presented to hospital with massive hepatomegaly, elevated liver enzymes and increased lactate three weeks following resection of a malignant melanoma from his shoulder (Clark level 5). Initially stable, he decompensated 24 to 48 hours subsequent to presentation with respiratory failure requiring mechanical ventilation, distributive shock requiring high dose vasopressor infusion, coagulopathy refractory to plasma infusion, progressive rise in liver enzymes and severe metabolic abnormalities including hyperkalemia, acidosis, hyperphosphatemia, hyperuricemia and hypocalcemia. Refractory to aggressive physiologic support he received palliation. Autopsy revealed >80% liver infiltration by metastatic malignant melanoma.
Conclusion
We report a case of fulminant hepatic failure secondary to metastatic malignant melanoma infiltration of the liver.
Similar content being viewed by others
Background
Malignant melanoma is a common malignancy that has the potential to metastasize to any site including the liver [1]. However, liver metastases secondary to melanoma rarely result in fulminant hepatic failure [2–5] and do not typically cause significant systemic disease. We cared for a patient with malignant melanoma who developed fulminant acute liver failure and multi-system organ failure.
Case presentation
A previously healthy 46-year old man on no medications was diagnosed with a Clark Level 5 malignant melanoma on his left shoulder following resection of a mole under local anesthetic. The lesion was subsequently reported as a melanoma and three weeks following his resection, before he could undergo a metastatic work-up, he presented to hospital with nausea, vomiting and right upper quadrant pain. He did not appear toxic, he was afebrile, and physical examination was unremarkable but for a tender right upper quadrant and hepatomegaly. Laboratory investigations demonstrated leukocytosis, modestly elevated liver enzymes, and lactic acidosis. Computed tomography scanning revealed marked hepatomegaly with an extensive infiltrative process and ultrasound demonstrated normal bile ducts. Baseline imaging of his abdomen was planned for staging, however it was not conducted prior to his presentation to hospital.
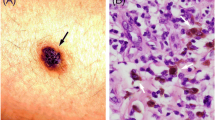
On day two of his admission the patient deteriorated with respiratory failure requiring endotracheal intubation and mechanical ventilation. He had oliguria, and hypotension refractory to fluid resuscitation. Rapidly progressive multi-system organ failure developed with anuria/azotemia requiring continuous renal replacement therapy. Liver failure ensued as evidenced by coagulopathy refractory to plasma infusions and by progressive transaminitis and hyperbilirubinema. He developed distributive shock requiring maximal pressor support. There were significant biochemical derangements including hyperkalemia, acidosis, hyperphosphatemia, hyperuricemia and hypocalcemia. Hemodialysis was commenced to rectify the hyperkalemia and acidosis that was refractory to continuous renal replacement therapy. An aggressive resuscitative and treatment approach was undertaken to allow confirmation that the liver lesions were melanoma and not a potentially treatable infection or lymphoma. An ultrasound guided transjugular biopsy of the liver was performed in the intensive care unit. Based on a frozen section diagnosis of malignant infiltration of the liver, high dose corticosteroid therapy was commenced. The patient continued to deteriorate despite maximal physiologic support and palliative measures were instituted after discussion with the next-of-kin. He succumbed to his illness on day-4 of admission. Autopsy revealed >80% liver infiltration by melanoma (Figure 1), a diagnosis verified by an immunohistochemical phenotype of S-100 and HMB-45 positive cells (Figure 2).
Conclusion
Our patient had a rare presentation of metastatic melanoma to the liver associated with fulminant liver failure, shock, and multisystem organ failure. Although acute liver failure has been reported subsequent to infiltration of the liver by lymphoma [6], breast [7], gastric [8], and lung cancer [9], there are only rare patients with melanoma associated with fulminant hepatic failure. We conducted an English language search of MEDLINE using the terms hepatic failure and melanoma and only identified four cases of melanoma associated with liver failure [2–5]. The natural history of acute liver failure is typically a rapid progression of liver dysfunction leading to multi-organ failure and subsequently death. Significant rise in lactate dehydrogenase was seen in our patient and this has been previously reported as an ominous sign of acute liver failure [2, 5].
The patient's biochemical derangements of severe hyperkalemia, acidosis, hyperphosphatemia, hyperuricemia, hypocalcemia and markedly elevated lactate dehydrogenase most likely represent the natural progression of acute liver failure due to massive hepatic necrosis secondary to tumor burden. However, the patient's biochemical profile can also be seen in tumor lysis syndrome. Tumor lysis syndrome has been reported as a complication of malignant melanoma, however in the context of treatment with chemotherapy [10, 11] and corticosteroids [12]. No cases of tumor lysis syndrome have ever been reported to occur spontaneously from malignant melanoma infiltration of the liver. However, spontaneous development of tumor lysis syndrome in other solid tumors without exposure to chemotherapy has been reported in the literature [13–15]. Whether the rapid deterioration of the patient was completely attributable to fulminant hepatic failure or a component of tumor lysis syndrome was involved, this case highlights the potential aggressiveness of malignant melanoma.
The underlying pathophysiology of the acute liver failure in our patient was likely secondary to ischemic injury arising from infiltration of the sinusoids and invasion of hepatic vessels. Hepatic ischemia has been proposed as the mechanism by which lymphoma may cause fulminant hepatic failure [16, 17] and is supported by the marked rise in aspartate aminotransferase and lactate dehydrogenase seen in our patient.
In summary, we report an unusual case of fulminant hepatic failure associated with multisystem organ failure resulting from metastatic melanoma replacing the vast majority of the liver. Although rare, our case would portend that malignant melanoma metastasizing to the liver can cause fulminant hepatic failure. Thus, in patients with a history of malignancy who present in acute liver failure clinical suspicion for malignant infiltration of the liver should be considered and ruled out before referral for consideration for liver transplantation.
References
Desmond RA, Soong SJ: Epidemiology of malignant melanoma. Surg Clin North Am. 2003, 83: 1-29. 10.1016/S0039-6109(02)00092-0.
Te HS, Schiano TD, Kahaleh M, Lissoos TW, Baker AL, Hart J, Conjeevaram HS: Fulminant hepatic failure secondary to malignant melanoma: Case report and review of the literature. American Journal of Gastroenterology. 1999, 94: 262-266. 10.1111/j.1572-0241.1999.00811.x.
Montero JL, Muntane J, Heras S, Ortega R, Fraga E, De lat Mata M: Acute liver failure cause by diffuse hepatic melanoma infiltration. Journal of Hepatology. 2002, 37: 540-541. 10.1016/S0168-8278(02)00219-2.
Bouloux PMG, Scott RJ, Goligher JE, Kindell C: Fulminant hepatic failure secondary to diffuse liver infiltration by melanoma. The Royal Society of Medicine. 1986, 79: 302-303.
Misuzu T, Watanabe S, Masaki T, Kurokohchi K, Kinekawa F, Inoue H, Uchida N, Kuriyama S: Fulimnant hepatic failure caused by malignant melanoma of unknown primary origin. J Gastroenterol. 2004, 39 (8): 804-806.
Braude S, Gimson AES, Portmann B: Fulminant hepatic failure in non-Hodgkin's lymphoma. Postgrad Med J. 1982, 58: 301-304.
Schneider R, Cohen A: Fulminant hepatic failure complicating metastatic breast carcinoma. S Med J. 1984, 77: 84-86.
Sawabe M, Kato Y, Ohashi I: Diffuse intrasinusoidal metastasis of gastric carcinoma to the liver leding to fulminant hepatic failure. Cancer. 1990, 65: 169-173.
McQuire BM, Cherwitz DL, Rabe KM: Small-cell carcionoma of the lung manifesting as acute hepatic failure. Mayo Clin Proc. 1997, 72: 133-139.
Stoves J, Richardson D, Patel H: Tumor lysis syndrome in a patient with metastatic melanoma treated with biochemotherapy. Nephrol Dial Transplant. 2001, 16: 188-189. 10.1093/ndt/16.1.188.
Castro MP, VanAuken J, Spencer-Cisek P, Legha S, Sponzo RW: Acute tumor lysis syndrome associated with concurrent biochemotherapy of metastatic melanoma: a case report and review of the literature. Cancer. 1999, 85: 1055-1059. 10.1002/(SICI)1097-0142(19990301)85:5<1055::AID-CNCR7>3.0.CO;2-3.
Habib GS, Saliba WR: Tumor lysis syndrome after hydrocortisone treatment in metastatic melanoma: a case report and review of the literature. Am J Med Sci. 2002, 323: 155-157. 10.1097/00000441-200203000-00007.
Woo IS, Kim JS, Park MJ, Lee MS, Cheon RW: Spontaneous acute tumor lysis syndrome with advanced gastric cancer. J Korean Med Sci. 2001, 16 (1): 115-118.
Feld J, Mehta H, Burkes RL: Acute spontaneous tumor lysis syndrome in adenocarcinoma of lung: a case report. Am J Clin Oncol. 2000, 23 (5): 491-493.
Vaisban E, Braester A, Mosenzon O, Kolin M, Horn Y: Spontaneous tumor lysis syndrome in solid tumors: really a rare condition?. Am J Med Sci. 2003, 25 (1): 38-40. 10.1097/00000441-200301000-00008.
Vardareli E, Dundar E, Aslan V, Gulbas Z: Acute liver failure due to Hodgkin's lymphoma. Med Prin Prac. 2004, 13: 372-374. 10.1159/000080477.
Lettieri CJ, Berg BW: Clinical features of Non-Hodgkin's lymphoma presenting with acute liver failure: a report of five cases and the review of published experiences. Am J Gastroenterol. 2003, 98: 1641-1646. 10.1111/j.1572-0241.2003.07536.x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/5/67/prepub
Acknowledgements
Informed consent to report this case was obtained from the patient's next of kin.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
GK conducted the literature review and wrote the first manuscript draft. SM was the pathologist. BC was the nephrologist and KL was the attending intensivist caring for the patient. All authors contributed to the revisions of and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kaplan, G.G., Medlicott, S., Culleton, B. et al. Acute hepatic failure and multi-system organ failure secondary to replacement of the liver with metastatic melanoma. BMC Cancer 5, 67 (2005). https://doi.org/10.1186/1471-2407-5-67
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-5-67