Abstract
Background
The EML4–ALK (echinoderm microtubule-associated protein-like 4 gene and the anaplastic lymphoma kinase gene) fusion oncogene represents a novel molecular target in a small subset of non–small–cell lung cancers (NSCLCs). The EML4–ALK fusion gene occurs generally in NSCLC without mutations in epidermal growth factor receptor (EGFR) and KRAS.
Case presentation
We report that a case of EML4–ALK-positive NSCLC with EGFR mutation had a response of stable disease to both an EGFR tyrosine kinase inhibitor (EGFR-TKI) and ALK inhibitor.
Conclusions
We described the first clinical report of a patient with EML4–ALK-positive NSCLC with EGFR mutation that had a response of stable disease to both single-agent EGFR-TKI and ALK inhibitor. EML4–ALK translocation may be associated with resistance to EGFR-TKI, and EGFR signaling may contribute to resistance to ALK inhibitor in EML4–ALK-positive NSCLC.
Similar content being viewed by others
Background
The EML4–ALK (echinoderm microtubule-associated protein-like 4 gene and the anaplastic lymphoma kinase gene) fusion oncogene was recently identified as a novel genetic alteration in non-small-cell lung cancer (NSCLC) [1]. EML4–ALK fusions have been detected in 2 to 7% of NSCLC patients. Patients harboring ALK rearrangements tend to be never and light smokers, have a history of adenocarcinoma, and be younger in age [1–6]. In general, the EML4–ALK fusion oncogene existed exclusively in NSCLC patients without the epidermal growth factor receptor (EGFR) gene mutation [1, 7, 8].
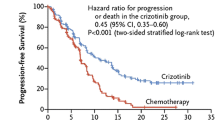
ALK inhibitors such as crizotinib are clinically effective in NSCLC patients harboring ALK rearrangements [9]. Crizotinib produced a high response rate and prolonged median progression-free survival among patients with ALK-positive NSCLC [9]. Crizotinib was recently approved by the US Food and Drug Administration and Japanese Ministry of Health, Labour and Welfare for the treatment of patients with advanced, ALK-rearranged NSCLC.
In this paper, we report a patient with NSCLC with concomitant ALK rearrangement and EGFR mutation that had a response of stable disease to both an EGFR tyrosine kinase inhibitor (EGFR-TKI) and ALK inhibitor.
Case presentation
In December 2009, a 55-year-old female who had never smoked was noted to have left lung opacity on a routine chest X-ray. No significant previous medical history was reported. Computed tomography (CT) scan of the chest revealed a 1.5 × 1.5 cm nodular lesion in the left upper lobe and hilar lymph node metastasis. Transthoracic needle biopsy histology revealed adenocarcinoma, and the histopathological subtype of the specimen was papillary adenocarcinoma with signet-ring cell components (Figure 1A-1C). The specimen was positive for periodic acid–Schiff (PAS) (Figure 1C). On immunohistochemical staining, the tumor cells were positive for thyroid transcription factor-1 (TTF-1) (Figure 1D). Laboratory findings were within normal range, except for the carcinoembryonic antigen (CEA) level of 158.0 ng/mL (normal range, 0 to 4.3 ng/mL) in the serum. She had multiple dorsal vertebra metastases (cT1N1M1b, stage IV).
Histology of the primary tumour. (A) and (B) shows a papillary adenocarcinoma (hematoxylin and eosin 200× magnification), (C) a mucin stain shows positive for both signet-ring and papillary morphology (PAS, 400× magnification). (D) immunohistochemical analysis of lung adenocarcinoma specimens with EML4-ALK fusion using a monoclonal anti-TTF-1 antibody (200× magnification).
Analysis for EGFR gene mutation was performed using a cytological specimen by means of the peptide nucleic acid–locked nucleic acid (PNA-LNA) polymerase-chain-reaction (PCR) clamp method as described previously [10, 11]. The specimen showed a deletion in exon 19 (L747-A750del T751S). We collected mRNA from the same tumor specimens using Pinpoint Slide RNA Isolation System in order to clarify whether there was EML4–ALK (echinoderm microtubule-associated protein-like 4 gene and the anaplastic lymphoma kinase gene) fusion gene in each tumor. Reverse transcription polymerase-chain-reaction (RT-PCR) followed by direct sequencing confirmed the presence of EML4–ALK variant 2 [1] (Figure 2). In addition, EML4–ALK was identified by using fluorescent in situ hybridization (FISH) for ALK rearrangements (Figure 3B) and was confirmed by immunohistochemistry for ALK expression in tumor [2] (Figure 3A).
A platinum doublet was chosen as first line therapy according to existing treatment protocol in 2009. Four cycles of combination chemotherapy comprising cisplatin and pemetrexed was administered at 3-week intervals. She was judged as having a stable disease. After 7 months, spinal magnetic resonance imaging (MRI) revealed progression of the dorsal vertebra lesions. Therefore, EGFR-TKI was chosen as a 2nd-line therapy. She received gefitinib therapy at 250 mg/day administered orally for 2 months. CT imaging of the chest showed that the pulmonary nodule was not growing after gefitinib therapy, and the tumor marker levels had not changed. However, spinal MRI demonstrated growing dorsal vertebra metastases 2 months after the start of gefitinib therapy. The carcinoembryonic antigen (CEA) level increased from 117 ng/ml to 250 ng/ml. Therefore, the patient was judged as having progressive disease. After local radiation therapy with a total of 30 Gy for dorsal metastases, a second EGFR-TKI was chosen given the stable primary disease. She received another EGFR-TKI, erlotinib (150 mg/day), as 3rd-line therapy. After being progression-free for 3 months, spinal MRI revealed a growing thoracic vertebra metastasis. She received 4th-line treatment with 2 cycles of docetaxel (DTX). However, her disease progressed 6 months later. Finally, she received a targeted inhibitor of ALK. The patient initially had SD associated with a temporary decrease in the CEA level from 743 ng/ml to 520 ng/ml, but her disease progressed after 4 months of therapy. The ALK inhibitor treatment was ceased and full supportive care was given. All lines of therapy were well tolerated.
Discussion
We presented a patient with NSCLC with concomitant ALK rearrangement and EGFR mutation that had a response of stable disease to both EGFR-TKI and ALK inhibitors. The presence of EML4–ALK generally seems to be mutually exclusive of the presence of EGFR or KRAS mutations in NSCLC [1, 7, 8]. Previous reports showed twelve cases of EML4–ALK-positive lung cancer with EGFR mutation [3, 12–17]. Only one patient with harboring ALK translocation and EGFR mutation was treated by ALK inhibitor has been reported [17]. Lee et al. reported two ALK-positive and EGFR-mutant NSCLC patient who did not respond to EGFR-TKI but achieved a durable partial response to ALK inhibitor [17]. The present patient was a woman with no history of smoking. Her pathological diagnosis was papillary adenocarcinoma with a signet-ring cell component, which was consistent with the previously reported characteristics of EML4–ALK-positive lung adenocarcinoma except for the EGFR mutation status [1–6]. It was reported that EGFR-TKI therapy among patients with advanced NSCLC and EGFR mutations revealed a response rate of more than 60% and progression-free survival of 9 to 14 months [11, 18, 19]. In addition, recent reports showed that ALK inhibition in NSCLC patients with the ALK rearrangement resulted in tumor shrinkage or stable disease in most patients [9]. Unfortunately, EGFR-TKI treatment was not effective in the tumor regression nor tumor marker level of present patient (disease might be controlled), but treatment with an ALK inhibitor resulted in SD with decreasing tumor markers. Therefore, this case showed that ALK rearrangement might be superior to EGFR mutation for the driver mutation.
It was reported that EML4–ALK fusion was associated with resistance to EGFR-TKIs [20]. Patients with NSCLC in the EML4–ALK cohort and the wild type cohort showed similar response rates to platinum-based combination chemotherapy and no difference in overall survival [20]. Whereas EGFR mutations confer sensitivity to EGFR-TKIs, EML4–ALK is strongly associated with resistance to EGFR-TKIs. In a previous case of concomitant EGFR mutation and ALK translocation, the patient presented the most durable response to an EGFR-TKI and was a case demonstrating no EML4–ALK expression by immunohistochemistry with an EML4–ALK rearrangement characterized by an isolated 3_ FISH signal [12]. Our patient presented a concurrent EML4-ALK rearrangement and ALK expression by immunohistochemistry; however, EGFR-TKI was not effective.
Among patients with both EML4–ALK rearrangement and EGFR mutation, in vitro studies showed that EGFR signaling can contribute to ALK inhibitor resistance in EML4–ALK NSCLC [14]. In addition, these findings suggested that a cancer cell line that harbors a concurrent ALK rearrangement and an EGFR mutation would be expected to be resistant to both single agent ALK and EGFR inhibitors [14]. We suggest that the combination of both ALK and EGFR inhibitors as early-line treatment may represent an effective therapy for this subset of NSCLC patients.
Conclusions
This is the first clinical report of a patient with EML4–ALK-positive NSCLC with EGFR mutation that had a response of stable disease to both single-agent EGFR-TKI and ALK inhibitor. The EML4–ALK fusion gene defines a new molecular subset of NSCLCs with distinct clinical and pathologic features. NSCLCs with ALK rearrangement are highly sensitive to ALK inhibition. However, EGFR signaling may contribute to ALK inhibitor resistance in EML4–ALK NSCLC. Therefore, we suggest that this provides a translational opportunity whereby laboratory studies should be undertaken to understand the biological link between ALK rearrangement and EGFR mutation, with a view to establishing whether there is preclinical justification for using combination therapy for NSCLC with concomitant ALK rearrangement and EGFR mutation.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Abbreviations
- EML4:
-
Echinoderm microtubule-associated protein-like 4
- ALK:
-
Anaplastic lymphoma kinase
- NSCLC:
-
Non-small cell lung cancer
- EGFR:
-
Epidermal growth factor receptor
- TKI:
-
Tyrosine kinase inhibitor
- CT:
-
Computed tomography
- PAS:
-
periodic acid–Schiff
- TTF-1:
-
Thyroid transcription factor-1
- PNA-LNA:
-
Peptide nucleic acid–locked nucleic acid
- PCR:
-
Polymerase chain reaction technique
- FISH:
-
Fluorescent in situ hybridization
- SD:
-
Stable disease
- MRI:
-
Magnetic resonance imaging (MRI)
- CEA:
-
Carcinoembryonic antigen
- RT-PCR:
-
Reverse transcription polymerase chain reaction.
References
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, Fujiwara S, Watanabe H, Kurashina K, Hatanaka H: Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007, 448 (7153): 561-566. 10.1038/nature05945.
Takeuchi K, Choi YL, Soda M, Inamura K, Togashi Y, Hatano S, Enomoto M, Takada S, Yamashita Y, Satoh Y: Multiplex reverse transcription-PCR screening for EML4-ALK fusion transcripts. Clin Can Res. 2008, 14 (20): 6618-6624. 10.1158/1078-0432.CCR-08-1018.
Koivunen JP, Mermel C, Zejnullahu K, Murphy C, Lifshits E, Holmes AJ, Choi HG, Kim J, Chiang D, Thomas R: EML4-ALK fusion gene and efficacy of an ALK kinase inhibitor in lung cancer. Clin Can Res. 2008, 14 (13): 4275-4283. 10.1158/1078-0432.CCR-08-0168.
Mano H: Non-solid oncogenes in solid tumors: EML4-ALK fusion genes in lung cancer. Cancer Sci. 2008, 99 (12): 2349-2355. 10.1111/j.1349-7006.2008.00972.x.
Wong DW, Leung EL, So KK, Tam IY, Sihoe AD, Cheng LC, Ho KK, Au JS, Chung LP, Pik Wong M: The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer. 2009, 115 (8): 1723-1733. 10.1002/cncr.24181.
Perner S, Wagner PL, Demichelis F, Mehra R, Lafargue CJ, Moss BJ, Arbogast S, Soltermann A, Weder W, Giordano TJ: EML4-ALK fusion lung cancer: a rare acquired event. Neoplasia. 2008, 10 (3): 298-302.
Inamura K, Takeuchi K, Togashi Y, Nomura K, Ninomiya H, Okui M, Satoh Y, Okumura S, Nakagawa K, Soda M: EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J Thorac Oncol. 2008, 3 (1): 13-17. 10.1097/JTO.0b013e31815e8b60.
Shinmura K, Kageyama S, Tao H, Bunai T, Suzuki M, Kamo T, Takamochi K, Suzuki K, Tanahashi M, Niwa H: EML4-ALK fusion transcripts, but no NPM-, TPM3-, CLTC-, ATIC-, or TFG-ALK fusion transcripts, in non-small cell lung carcinomas. Lung Cancer. 2008, 61 (2): 163-169. 10.1016/j.lungcan.2007.12.013.
Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, Ou SH, Dezube BJ, Janne PA, Costa DB: Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010, 363 (18): 1693-1703. 10.1056/NEJMoa1006448.
Nagai Y, Miyazawa H, Huqun , Tanaka T, Udagawa K, Kato M, Fukuyama S, Yokote A, Kobayashi K, Kanazawa M: Genetic heterogeneity of the epidermal growth factor receptor in non-small cell lung cancer cell lines revealed by a rapid and sensitive detection system, the peptide nucleic acid-locked nucleic acid PCR clamp. Cancer Res. 2005, 65 (16): 7276-7282. 10.1158/0008-5472.CAN-05-0331.
Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I: Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010, 362 (25): 2380-2388. 10.1056/NEJMoa0909530.
Popat S, Vieira de Araujo A, Min T, Swansbury J, Dainton M, Wotherspoon A, Lim E, Nicholson AG, O'Brien ME: Lung adenocarcinoma with concurrent exon 19 EGFR mutation and ALK rearrangement responding to erlotinib. J Thorac Oncol. 2011, 6 (11): 1962-1963. 10.1097/JTO.0b013e31822eec5e.
Tiseo M, Gelsomino F, Boggiani D, Bortesi B, Bartolotti M, Bozzetti C, Sammarelli G, Thai E, Ardizzoni A: EGFR and EML4-ALK gene mutations in NSCLC: a case report of erlotinib-resistant patient with both concomitant mutations. Lung Cancer. 2011, 71 (2): 241-243. 10.1016/j.lungcan.2010.11.014.
Sasaki T, Koivunen J, Ogino A, Yanagita M, Nikiforow S, Zheng W, Lathan C, Marcoux JP, Du J, Okuda K: A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Cancer Res. 2011, 71 (18): 6051-6060. 10.1158/0008-5472.CAN-11-1340.
Tanaka H, Hayashi A, Morimoto T, Taima K, Tanaka Y, Shimada M, Kurose A, Takanashi S, Okumura K: A case of lung adenocarcinoma harboring EGFR mutation and EML4-ALK fusion gene. BMC Cancer. 2012, 12 (1): 558-10.1186/1471-2407-12-558.
Kuo YW, Wu SG, Ho CC, Shih JY: Good response to gefitinib in lung adenocarcinoma harboring coexisting EML4-ALK fusion gene and EGFR mutation. J Thorac Oncol. 2010, 5 (12): 2039-2040. 10.1097/JTO.0b013e3181f43274.
Lee JK, Kim TM, Koh Y, Lee SH, Kim DW, Jeon YK, Chung DH, Yang SC, Kim YT, Kim YW: Differential sensitivities to tyrosine kinase inhibitors in NSCLC harboring EGFR mutation and ALK translocation. Lung Cancer. 2012, 77 (2): 460-463. 10.1016/j.lungcan.2012.04.012.
Fukuoka M, Wu YL, Thongprasert S, Sunpaweravong P, Leong SS, Sriuranpong V, Chao TY, Nakagawa K, Chu DT, Saijo N: Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol. 2011, 29 (21): 2866-2874. 10.1200/JCO.2010.33.4235.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, Seto T, Satouchi M, Tada H, Hirashima T: Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010, 11 (2): 121-128. 10.1016/S1470-2045(09)70364-X.
Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, Solomon B, Stubbs H, Admane S, McDermott U: Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009, 27 (26): 4247-4253. 10.1200/JCO.2009.22.6993.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/13/262/prepub
Acknowledgements
The authors wish to thank Mari Masuda for technical support in the sequence alignment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AM prepared the manuscript and the literature search; RN and MS reviewed and edited the manuscript; HM and AG corrected and revised the manuscript; KS, KK, SK, YM, MS and TS treated and observed the patient; MK and ST performed the histopathological, immunohistochemical examinations; and AY, KH, KT, NY and YI reviewed the manuscript. All authors read and approved of the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Miyanaga, A., Shimizu, K., Noro, R. et al. Activity of EGFR-tyrosine kinase and ALK inhibitors for EML4–ALK-rearranged non–small–cell lung cancer harbored coexisting EGFRmutation. BMC Cancer 13, 262 (2013). https://doi.org/10.1186/1471-2407-13-262
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-13-262