Abstract
Background
Accurate staging of colorectal cancer (CRC) with clinicopathological parameters is important for predicting prognosis and guiding treatment but provides no information about organ site of metastases. Patterns of genomic aberrations in primary colorectal tumors may reveal a chromosomal signature for organ specific metastases.
Methods
Array Comparative Genomic Hybridization (aCGH) was employed to asses DNA copy number changes in primary colorectal tumors of three distinctive patient groups. This included formalin-fixed, paraffin-embedded tissue of patients who developed liver metastases (LM; n = 36), metastases (PM; n = 37) and a group that remained metastases-free (M0; n = 25).
A novel statistical method for identifying recurrent copy number changes, KC-SMART, was used to find specific locations of genomic aberrations specific for various groups. We created a classifier for organ specific metastases based on the aCGH data using Prediction Analysis for Microarrays (PAM).
Results
Specifically in the tumors of primary CRC patients who subsequently developed liver metastasis, KC-SMART analysis identified genomic aberrations on chromosome 20q. LM-PAM, a shrunken centroids classifier for liver metastases occurrence, was able to distinguish the LM group from the other groups (M0&PM) with 80% accuracy (78% sensitivity and 86% specificity). The classification is predominantly based on chromosome 20q aberrations.
Conclusion
Liver specific CRC metastases may be predicted with a high accuracy based on specific genomic aberrations in the primary CRC tumor. The ability to predict the site of metastases is important for improvement of personalized patient management.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the second leading cause of cancer death in the Western world. Every year one million people worldwide will develop CRC[1]. The overall five-year survival is 57% and up to 50% of all patients will eventually develop metastases. Metastases are responsible for the great majority of cancer deaths, mainly metastatic liver disease. Even with surgery and modern chemotherapy most metastases are eventually fatal.
Besides lymphatic and haematogenous dissemination, CRC can spread into the intra-abdominal cavity and cause peritoneal metastases (PM).
Of all patients who die of advanced colorectal cancer, 60-70% show evidence of liver metastasis. Even with the use of targeted drugs, the overall survival in patients with non-resectable CRC liver metastases is only 2-years. In patients with resectable liver metastasis a 5-year survival of 30% can be achieved and up to 20% of the population will still be alive after 10 years. Eligibility for hepatic surgery depends on the possibility that all metastases are resectable and adequate liver preservation can be maintained. Therefore early detection of liver metastases is of utmost priority and will result in more radical surgery and thus long term survival[2].
Similar to liver metastasis, peritoneal metastasis is uniformly seen as a fatal condition. However, in the last decade survival has improved due to aggressive cytoreductive surgery in combination with hyperthermic intraperitoneal chemotherapy (HIPEC). Several predictors of outcome after HIPEC treatment, such as completeness of cytoreduction and number of affected intra-abdominal tumor regions, have been described. Patients who underwent complete cytoreduction in combination with HIPEC showed a 5-year survival of 22-49%. Early detection of peritoneal metastases will result in a better cytoreduction and less affected intra-abdominal regions[3]. In conclusion, early detection of liver and peritoneal metastasis will result in a tailored follow-up program and through this better patient outcome.
Accurate staging of CRC with clinicopathological parameters is important in predicting prognosis and guiding treatment but can currently not predict the site of metastases. Therefore, understanding of the molecular and cellular mechanisms underlying colorectal cancer formation, in particular progression to site of metastases is of utmost importance.
The development of CRC arises and develops through the adenoma-carcinoma sequence. This adenoma-carcinoma sequence is a well defined pathway of histopathological stages, each characterized by distinct mutations in oncogenes and tumor suppressor genes [4, 5]. Two molecular pathways have been well described; the microsatellite instability and the chromosomal instability pathway (reviewed by Jass et al) [4, 6, 7]. The majority of CRC (85%) are chromosomally unstable [5], characterized by allelic losses, chromosomal amplifications and translocations [8], whereas mismatch repair deficiency is the underlying cause of the remainder of CRCs.
Cardoso et al. reviewed multiple studies that have reported on the existence of chromosomal abnormalities and gene expression profiles in CRC [8]. With this approach they described several specific chromosomal loci and corresponding genes which play an important role in colorectal cancer progression. A meta-analysis by Diep et al. on 31 comparative genomic hybridization (CGH) studies, comprising a total 859 CRCs, described chromosomal alterations that occurred early in the establishment of primary CRC, as well as those that are present in the different Dukes' stages and in liver metastases[9].
So far, a number of chromosomal aberrations have been related to liver metastases in CRC [9–13]. Metha et al. studied the relation between the extent of chromosomal instability and the survival of patients with liver metastases. They showed that with a larger chromosomally unstable fraction in the liver metastases, survival for patients was better[14].
Various studies have described prognostic gene expression profiles for CRC patients although these profiles have very few genes in common [15–20]. Gene expression profiles have been described for breast cancer that predict site specific recurrence e.g., bone and lung metastases[21–23]. However, gene expression or genomic profiles in CRC that predict site specific recurrence have not been well studied.
Here, we investigated genome-wide chromosomal aberrations in defined groups of primary colorectal tumors to determine copy number signatures for site specific metastases. The understanding of the molecular and cellular mechanisms underlying colorectal cancer formation, progression to malignancy and site specific metastases are important to perform targeted follow-up and eventually develop targeted therapy in patients with CRC.
Methods
Patients and Tumor Specimens
We have used formalin-fixed, paraffin embedded (FFPE) primary colorectal tumors of three different groups. 356 patients were selected on the basis of their disease outcome in follow-up. Patients, who had developed metastases were treated in two specialized centers: liver metastasis (LUMC), peritoneal metastasis (NKI-AVL), whereas all of the non-metastasis group were treated for their primary tumor at the NKI-AVL. For the metastatic groups primary tumor material was obtained from several different pathology laboratories in the Netherlands. In total, 119 samples were retrieved, of which 98 samples remained after quality control. One group (n = 36) were patients who have been treated with Isolated Hepatic Perfusion (IHP) for the treatment of CRC metastases confined to the liver (LM)[24]. The second group (n = 37) were patients who have been treated with hyperthermal intraperitoneal chemotherapy (HIPEC) for the treatment of CRC metastases confined to the peritoneum (PM) [25]. The third group (n = 25) consisted of patients with CRC who did not develop metastases (M0). In this M0 group only two patients had a minimal follow-up of 12 months. All the others had a follow-up of at least 36 months. That implicates that 92% had a follow-up of at least 3-years. The M0 group showed a median follow-up of 103 months. The LM and PM groups were carefully screened to ensure these were free of distant metastases at time of treatment, other than the liver or the peritoneal surface, respectively [25, 26]. For that reason we characterized these two groups as single organ specific CRC metastases. In this study none of the primary tumors were treated neo-adjuvant with chemotherapy. We have used anonymized patient tissue material of patients who were consented for a HIPEC procedure (PM) or Liver perfusion (LM), or had not opted out for making left-over tissue available for research (M0), which followed standard procedures operational in the respective hospitals approved by the institutional IRB's or Board, which ever one was appropriate. Tissue handling and anonymization followed the Helsinki declaration.
Comparative Genomic Hybridization
DNA copy number changes were investigated using the 3.5 k bacterial artificial chromosomes (BAC) array performing array comparative genomic hybridization (aCGH)[27]. The human 3600 BAC/PAC genomic clone set, covering the full genome at 1 Mb spacing used for the production of our arrays, was obtained from the Welcome Trust Sanger Institute http://www.sanger.ac.uk/. Information on this clone set can be obtained at the BAC/PAC Resources Center Web Site http://bacpac.chori.org. The whole library was spotted in triplicate on every slide. To prevent slide batch spotting bias, samples were hybridized in random order http://microarrays.nki.nl/.
DNA isolation was performed as described earlier[28]. Briefly, genomic DNA was isolated by proteinase K digestion after deparaffination from 10 × 10 μm FFPE tissue sections containing at least 70% tumor cells from both the M0 and PM group. For the LM group DNA was isolated from FFPE tissue block punches. These punches were taken out of the tissue blocks in the area with at least 60% tumor cells. Reference DNA was isolated from peripheral blood lymphocytes from six healthy male individuals. It was pooled and sonicated until its median fragment length was similar to that of the test samples.
DNA quality was tested by measuring the maximum possible length of DNA to be amplified by a multiplex PCR as described elsewhere [29]. This mulitplex PCR produces DNA fragments of 100, 200, 300, and 400 bp. Samples of which at least 200 base pair fragments could be produced were of sufficient quality to be analyzed with aCGH[29] We initially selected 119 cases of which 98 passed the quality control. There were no significant differences in tumor/patient characteristics in the selected versus initial group.
Tumor DNA labelling was performed with ULS-Cy3 and ULS-Cy5 conjugates from the Universal Linkage System (ULS Kreatech Biotechnology, Amsterdam the Netherlands) [30]. Hybridisations on the arrays were done at our Central Microarray Facility, as described previously[27]. Data processing of the scanned microarray slide included signal intensity measurement with the ImaGene software program, followed by median pin-tip (c.q. sub array) normalization. Intensity ratios (Cy5/Cy3) were log2-transformed and triplicate spot measurements were averaged[27]. Microarray data have been deposited in NCBI's Gene Expression Omnibus (Edgar et al Nucleic Acids Res 2002) and are accessible through GEO Series accession numbers GSE20496.
For MSI analyses, DNA from paired normal and tumor samples was evaluated after PCR and fragments were analyzed using 2 mononucleotide markers (BAT 25 and BAT 40), and 6 dinucleotide markers (D1S158, D2S123, D5S346, D9S63, D17S250 and D18S58). A tumor was considered to be MSI-high in case three or more markers showed instability, MSI-low when only one marker showed instability and MSI-stable when none of the markers showed instability[16].
Data analysis
KC-SMART, a recently developed algorithm for identifying recurrent copy number changes, was used to identify specific locations of genomic gains and losses recurring at significant levels within the various groups [31]. Briefly, an aggregate profile of the aberrations is created by adding either the positive log2 values or the negative log2 values across all tumors. These aggregate profiles (one for gains and one for losses) are smoothed using locally weighted Gaussian kernel convolution, resulting in the Kernel Smoothed Estimate (KSE). KSEs computed for many randomized instances of the dataset are employed to generate a null distribution and establish a (multiple testing corrected) significance threshold (p = 0.05, Figure 1). All aberrations in the smoothed profile computed on the real data that exceed this threshold are deemed to be significantly recurrent in the dataset.
Visualisation of a three group KC-SMART analysis. This figure shows the Kernel Smoothed Estimated (KSEs) for the three groups analyzed in this study (Liver Metastases (LM), Peritoneal Metastases (PM) and No metastases (M0)). All chromosomes are plotted head-to-tail, Black dotted lines denote the end of chromosomes and magenta dotted line denote centromere locations.
In order to detect consistent differences in copy number changes between two groups, we employed comparative KC-SMART. This approach employs the signal-to-noise-ratio (SNR) to quantify the differences between the profiles of two groups of tumors. The SNR is a ratio of the absolute difference of the means of the classes and the sum of the average within-class standard deviation, analogous to the t-statistic. In order to calculate the SNR we produce smoothed profiles as described above for single tumors, instead of on an aggregate of the entire group. This smoothed profile is constructed on a grid with a grid spacing of 50,000 base pairs. For each grid point we calculate the SNR between two groups. To establish significance we permute the group labels 1000 times. Based on the results of this permutation, we are able to calculate the false discovery rate (FDR), and define a 1% FDR threshold. Any region for which the SNR exceeds this threshold, is significantly differentially aberrant between the two groups.
Logistic regression and its confidence intervals were calculated using the glm and stats packages of the statistical analysis software R http://www.r-project.org. Approximate absolute copy numbers for a certain genomic region were calculated from the averaged log2 measurements over all BAC clones mapped to the region.
We created two classifiers for organ specific metastases, using a shrunken centroids classifier (Prediction Analysis for Microarrays: PAM http://www-stat.stanford.edu/~tibs/PAM) on the aCGH data. The first classifier was trained to distinguish the LM group from a group consisting of both the PM and M0 groups together. The second classifier was trained to distinguish the PM group from the M0 group (additional figures).
Results
Patient and tumor characteristics
Patient and tumor characteristics like gender, tumor differentiation and MSI status, were not significantly different between the three patient groups (M0, PM and LM respectively) (Table 1). Groups differed for some characteristics that could be partly accounted for by the different selection criteria employed for each of the groups. For instance, for the tumor location more right-sided tumors were included in the M0 group, whereas the PM and LM group consisted of more left-sided colon and rectum tumors. There were relative more T4 tumors in the PM group compared with the M0 and LM group. Naturally, the M0 group showed no stage 4 patients and was therefore significantly different from the LM and PM group. The LM group had the highest percentage of Stage 4 patients.
Almost all patients were MSI stable (including MSI low) except for 1 patient in the PM group.
Comparative Genomic Hybridization and KC-SMART analysis
Genomic DNA of 98 tumor samples was hybridized to BAC-clone microarrays to obtain, for each BAC clone on the array, a log2 ratio of the fluorescence intensity ratio of the sample versus the reference for each of the three groups. We first analyzed the three groups (LM, PM, M0) separately with KC-SMART to detect regions of common aberrations across the samples in a group. See Figure 1.
The KC-SMART analysis showed that the three groups had an overall similar pattern of chromosomal aberrations, with the Pearson's correlation coefficient between the KSEs of the groups being 0.84 for the gains and 0.90 for the losses (Figure 1). Although the genomic instability in the three groups was similar overall, chromosome 20 was an exception.
To better identify chromosomal aberrations specific for the liver metastases group, we compared this group with the other two groups (M0 and PM) combined (Figure 2 and 3). Chromosome 20q was significantly more gained in the LM group compared with the other samples (Kernel Smoothed Estimate (KSE); p < 0.05), Bonferroni multiple testing corrected, Figure 2 top panel, aberrations exceeding the red lines). The comparative KC-SMART analysis yielded chromosome 20q with a FDR < 0,01 and several other regions with a FDR of <0.05 (Figure 2; lower panel). These other significant gains (FDR < 0.05) and losses specific for the LM group were located on chromosomes 5q, 7q, 8p, 8q,13q, 14q, 15q, 18p, 18q (Figure 2; lower panel and additional file 1 figure S1). Further investigation of the region gained on chromosome 20 showed that BAC clones encompassing the whole q-arm are gained in the LM group (Figure 3; KSE and SNR upper and lower panel respectively).
Gains and losses of the Liver Metastases (LM) samples versus the Peritoneal Metastases (PM) and No metastases (M0) samples. Shown here is the KSE (Kernel Smoothed Estimated) of the LM and PM groups in the upper panel. The lower panel shows the signal-to-noise (SNR) calculated between the two groups. The red dots represent the BAC clones used for the LM-PAM classifier. All chromosomes are plotted head-to-tail, Black dotted lines denote the end of chromosomes and magenta dotted line denote centromere locations. FDR = False Discovery Rate.
Logistic regression analysis to predict liver metastases recurrence based on the mean 20q profile of gains/losses for each group separately, showed for every 0.1 log2 20q amplification an odds ratio of 16.2 (90% CI: 2.3-141.2) for developing liver metastases. To test whether nodal status and the 20q mean log2 value are independent predictors of liver metastases, we added both terms to a logistic regression and determined the significance of the corresponding regression coefficients. Both coefficients were significant (20q: P < 0.00003, nodal status: P < 0.024). This shows that our prediction of liver metastases based on mean 20q log2 value is independent of nodal status.
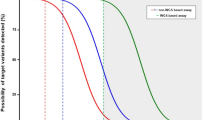
To investigate the predictive association of the 20q amplification we constructed a Receiver-Operator-Characteristic curve (ROC-curve) for the average log2 values of the chromosome 20q BAC clones. This simple measure already results in an Area Under the Curve (AUC) of 0.76 for predicting LM (Figure 4 red line).
ROC curve when using 20q as a predictive value for liver metastasis. This figures shows the Reciever-Operating Characteristic (ROC) curve for using the mean log2 ratio of the 20q BAC clones (red) or the mean log2 of the BAC clones that resulted from the LM-PAM classfier (blue). AUC = Area Under the Curve.
A LM-PAM classifier was able to separate the LM group from the other groups (M0 and PM) with 80% accuracy ((Figure 5 misclassification error 20%) (78% sensitivity and 86% specificity)). This LM-PAM classifier included 84 BAC clones and was significantly enriched for probes located on chromosome 20q (Additional file 2 table S1; marked green). Using the per-tumor class probabilities derived from the PAM classifier we also built a ROC-curve for this classifier which resulted in an AUC of 0.86 (Figure 4 blue line). Chromosome 20 is represented by 65 BAC clones on the BAC-array; 21 of these clones represent the p-arm and 44 the q-arm. From these 44 q-arm clones, 77% (34/44) were included in the LM-PAM classifier (Table 2; marked bold-italic). The rest of the BAC clones (50/84) in the LM-PAM classifier were distributed over 20 different chromosomal locations (Figure 2; lower panel and (Additional file 2 table S1).
PAM analysis of the Liver Metastases (1) versus the rest of the group (Peritoneal Metastases & No metastases) (2). The arrow indicates the cutoff location of the LM-PAM classifier and number (84) of BAC clones in classifier. PAM = Prediction Analysis for Microarrays. LM--PAM Classifier = Liver Metastases- Prediction Analysis for Microarrays classifier.
The second classifier was trained to distinguish the PM group from the M0 group. A PM-PAM classifier was able to separate the PM group from the M0 with 90% accuracy (Additional file 3 figure S2, misclassification error 10%). This PM-PAM classifier included 140 BAC clones and was, unlike the LM-PAM classifier, employing probes spread over the whole genome (Additional file 4 table S2).
Discussion
One of the challenges in CRC therapy lies in the early detection and treatment of CRC metastases. Elucidation of the molecular and cellular mechanisms of developing metastases will play an important role in future diagnostic and therapeutic interventions. A well established screening method to detect the genetic changes that underlie carcinogenesis is comparative genomic hybridization and was first introduced by Kallionemi and colleagues in 1992 [32]
In the present study we examine genome wide chromosomal aberrations in primary CRC to identify molecular markers predictive for liver metastases. The method we chose to examined genome wide chromosomal aberrations is a published and publically available method to look for recurrent copy number alterations and differential copy number alteration[31]. The KC-SMART method was applicable to our research questions and therefore used. An important principle in the analysis of this 20q amplification is that a threshold value can be (arbitrarily) set, but the logistic regression shows a continuous relationship between the aCGH measurement and the risk of a liver metastasis. Binarizing the predictive variable would cause information loss in this case. We believe that there is more information in the continuous mean log2 value of the 20q probes than just an on/off call.
To the best of our knowledge, this is the first study reporting a classifier predictive for liver metastases in primary CRC based on genomic aberrations. Our data demonstrate that primary colorectal tumors that developed liver metastases are characterized by an amplification of chromosome 20q. This amplification of chromosome 20q occurred significantly more often in the LM group compared to the other groups (PM and M0).
In this study there were significantly more left sided and rectum tumors in the LM group as compared to the PM group. So far, however, there is no evidence that peritoneal metastasis are related to the location of the primary colorectal tumor. These primary lesions are often characterized as mucinous T4 tumors which spread tumor cells into the peritoneal cavity[33]. It might be that left sided and rectum tumors could modify the penetrance of chromosome 20q and as result more frequently develop liver metastases. This could contribute to the fact that left sided and rectal tumors in our study result more frequently into liver metastases whereas right sided tumors more often into peritoneal metastases.
We created a classifier to predict liver metastases in patients with CRC. This LM-PAM classifier was able to identify patients who would develop liver metastases and resulted in an AUC of 0.86. Although the classifier was constructed by employing cross-validation to obtain unbiased error estimates, this result should be confirmed in an independent validation set. Logistic regression analysis on the mean 20q copy number ratio showed for every 0.1 log2 20q amplification an odds ratio of 16.2 (90% CI, 2.3-141.2) for developing liver metastases.
Amplification of chromosome 20q has been identified in several tumor types including breast, ovary, bladder, pancreas and stomach [32, 34–38]. In colorectal cancer, chromosome 20q has been related to tumor progression, liver metastases and as an indicator of worse patient survival [10–13, 16, 29, 39–42]. Knösel et al. created a progression model to identify relevant chromosomal imbalances specific for metastases but this model was not created to predict site of metastases in primary CRC [43]. Recently, Nakao et al. showed that specific copy number aberrations were linked to nodal metastases and reported a significant difference in 20q amplification in primary colorectal tumors between patients who had liver metastases at time of surgery and those who had no liver metastases. Unfortunately, they did not propose a prediction model for liver metastases [44, 45]. Diep et al. presented a genetic pathway for CRC progression based on a meta-analysis of 31 CGH studies. They identified specific chromosomal alterations linked to different stages of tumor progression and liver metastases and found that the majority of chromosomal alterations were present in both primary carcinomas and liver metastases. They showed that the number of alterations increases in the transition from primary carcinomas to liver metastases. Furthermore, they showed that the role of chromosome 20q was evident in patients with Dukes D classification [9].
Hence, across all studies, chromosome 20q is of importance in the development of liver metastases. Therefore, more understanding of the candidate genes located on chromosome 20q may guide us to understand the biological mechanisms in the development of liver metastases. So far, several genes located on 20q have been described to play an important role in tumor progression and liver metastases. For example genes such as CAS/CSE1L, NABC1, ZNF217, Aurora2 (BTAK, STK15), LIVIN, PTK6, HD54, EEF1A2, PSMA7, TPX2, AURKA and the ubiquitin-conjugating enzyme E2C (UBE2C) [10–13, 45–51].
These candidate genes located on chromosome 20q should be taken into account when examining new targeted therapeutic regimens for patients with CRC. For example, chromosome 20q amplification in CRC showed in an in vitro study response to Kinesin-5 Inhibitor. This inhibitor plays a role in the mitotic spindle function in the cell. Resistance to Kinesin was dominated by amplification of chromosome 20q. It was suggested that AURKA and the TPX2 gene located on 20q were the genes resistance for the Kinesin-5 Inhibitor[51]. Amplification of 20q could therefore be a potential target for novel antimitotic cancer therapies.
In summary, organ specific CRC metastases localization can be predicted by a LM-PAM classifier on the basis of specific genomic aberrations in the primary colorectal tumor. The validation of the LM-PAM classifier will further potentiate its role as a tool in clinical practice. As a result, patients at risk for developing liver metastases should be frequently screened with modern imaging tools and are most likely to benefit from additional chemotherapy.
We show the possibility for specific CGH profiles to predict CRC metastases target organ with 80% precision. This is the first tool to do this and as such may provide the information to guide individual treatment protocols. In daily clinical practice q-PCR or FISH probes could be used on FFPE tissue for detecting patients at risk based on a 20q amplification. We are now developing an MLPA analysis of chromosome 20q to identify specific regions involved in the development of liver metastasis.
Conclusion
The ability to predict liver metastases based on specific genomic aberrations in the CRC is important for understanding the biology of the tumor, to perform tailored follow-up and eventually develop targeted therapy in patients with CRC. Further research should be done by investigation specific target regions of chromosome 20q.
References
Weitz J, Koch M, Debus J, Hohler T, Galle PR, Buchler MW: Colorectal cancer. Lancet. 2005, 365: 153-165. 10.1016/S0140-6736(05)17706-X.
Abdel-Misih SR, Schmidt CR, Bloomston PM: Update and review of the multidisciplinary management of stage IV colorectal cancer with liver metastases. World J Surg Oncol. 2009, 7: 72-10.1186/1477-7819-7-72.
Verwaal VJ, Bruin S, Boot H, van Slooten G, van Tinteren H: 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol. 2008, 15: 2426-2432. 10.1245/s10434-008-9966-2.
Fearon ER, Vogelstein B: A genetic model for colorectal tumorigenesis. Cell. 1990, 61: 759-767. 10.1016/0092-8674(90)90186-I.
Lengauer C, Kinzler KW, Vogelstein B: Genetic instability in colorectal cancers. Nature. 1997, 386: 623-627. 10.1038/386623a0.
Jass JR: Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007, 50: 113-130. 10.1111/j.1365-2559.2006.02549.x.
Jass JR, Whitehall VL, Young J, Leggett BA: Emerging concepts in colorectal neoplasia. Gastroenterology. 2002, 123: 862-876. 10.1053/gast.2002.35392.
Cardoso J, Boer J, Morreau H, Fodde R: Expression and genomic profiling of colorectal cancer. Biochim Biophys Acta. 2007, 1775: 103-137.
Diep CB, Kleivi K, Ribeiro FR, Teixeira MR, Lindgjaerde OC, Lothe RA: The order of genetic events associated with colorectal cancer progression inferred from meta-analysis of copy number changes. Genes Chromosomes Cancer. 2006, 45: 31-41. 10.1002/gcc.20261.
Hidaka S, Yasutake T, Takeshita H, Kondo M, Tsuji T, Nanashima A, Sawai T, Yamaguchi H, Nakagoe T, Ayabe H, et al: Differences in 20q13.2 copy number between colorectal cancers with and without liver metastasis. Clin Cancer Res. 2000, 6: 2712-2717.
Aragane H, Sakakura C, Nakanishi M, Yasuoka R, Fujita Y, Taniguchi H, Hagiwara A, Yamaguchi T, Abe T, Inazawa J, et al: Chromosomal aberrations in colorectal cancers and liver metastases analyzed by comparative genomic hybridization. Int J Cancer. 2001, 94: 623-629. 10.1002/ijc.1522.
Aust DE, Muders M, Kohler A, Schmidt M, Diebold J, Muller C, Lohrs U, Waldman FM, Baretton GB: Prognostic relevance of 20q13 gains in sporadic colorectal cancers: a FISH analysis. Scand J Gastroenterol. 2004, 39: 766-772. 10.1080/00365520410003191.
Korn WM, Yasutake T, Kuo WL, Warren RS, Collins C, Tomita M, Gray J, Waldman FM: Chromosome arm 20q gains and other genomic alterations in colorectal cancer metastatic to liver, as analyzed by comparative genomic hybridization and fluorescence in situ hybridization. Genes Chromosomes Cancer. 1999, 25: 82-90. 10.1002/(SICI)1098-2264(199906)25:2<82::AID-GCC2>3.0.CO;2-6.
Mehta KR, Nakao K, Zuraek MB, Ruan DT, Bergsland EK, Venook AP, Moore DH, Tokuyasu TA, Jain AN, Warren RS, et al: Fractional genomic alteration detected by array-based comparative genomic hybridization independently predicts survival after hepatic resection for metastatic colorectal cancer. Clin Cancer Res. 2005, 11: 1791-1797. 10.1158/1078-0432.CCR-04-1418.
Arango D, Laiho P, Kokko A, Alhopuro P, Sammalkorpi H, Salovaara R, Nicorici D, Hautaniemi S, Alazzouzi H, Mecklin JP, et al: Gene-expression profiling predicts recurrence in Dukes' C colorectal cancer. Gastroenterology. 2005, 129: 874-884. 10.1053/j.gastro.2005.06.066.
Barrier A, Boelle PY, Roser F, Gregg J, Tse C, Brault D, Lacaine F, Houry S, Huguier M, Franc B, et al: Stage II colon cancer prognosis prediction by tumor gene expression profiling. J Clin Oncol. 2006, 24: 4685-4691. 10.1200/JCO.2005.05.0229.
Eschrich S, Yang I, Bloom G, Kwong KY, Boulware D, Cantor A, Coppola D, Kruhoffer M, Aaltonen L, Orntoft TF, et al: Molecular staging for survival prediction of colorectal cancer patients. J Clin Oncol. 2005, 23: 3526-3535. 10.1200/JCO.2005.00.695.
Koehler A, Bataille F, Schmid C, Ruemmele P, Waldeck A, Blaszyk H, Hartmann A, Hofstaedter F, Dietmaier W: Gene expression profiling of colorectal cancer and metastases divides tumours according to their clinicopathological stage. J Pathol. 2004, 204: 65-74. 10.1002/path.1606.
Lin YH, Friederichs J, Black MA, Mages J, Rosenberg R, Guilford PJ, Phillips V, Thompson-Fawcett M, Kasabov N, Toro T, et al: Multiple gene expression classifiers from different array platforms predict poor prognosis of colorectal cancer. Clin Cancer Res. 2007, 13: 498-507. 10.1158/1078-0432.CCR-05-2734.
Wang Y, Jatkoe T, Zhang Y, Mutch MG, Talantov D, Jiang J, McLeod HL, Atkins D: Gene expression profiles and molecular markers to predict recurrence of Dukes' B colon cancer. J Clin Oncol. 2004, 22: 1564-1571. 10.1200/JCO.2004.08.186.
Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, Foekens JA, Martens JW: Subtypes of breast cancer show preferential site of relapse. Cancer Res. 2008, 68: 3108-3114. 10.1158/0008-5472.CAN-07-5644.
Smid M, Wang Y, Klijn JG, Sieuwerts AM, Zhang Y, Atkins D, Martens JW, Foekens JA: Genes associated with breast cancer metastatic to bone. J Clin Oncol. 2006, 24: 2261-2267. 10.1200/JCO.2005.03.8802.
Landemaine T, Jackson A, Bellahcene A, Rucci N, Sin S, Abad BM, Sierra A, Boudinet A, Guinebretiere JM, Ricevuto E, et al: A six-gene signature predicting breast cancer lung metastasis. Cancer Res. 2008, 68: 6092-6099. 10.1158/0008-5472.CAN-08-0436.
van Iersel LB, Verlaan MR, Vahrmeijer AL, van Persijn van Meerten EL, Tijl FG, Sparidans RW, Gelderblom H, Kuppen PJ, Tollenaar RA, van de Velde CJ: Hepatic artery infusion of high-dose melphalan at reduced flow during isolated hepatic perfusion for the treatment of colorectal metastases confined to the liver: a clinical and pharmacologic evaluation. Eur J Surg Oncol. 2007, 33: 874-881.
Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H, Zoetmulder FA: Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol. 2003, 21: 3737-3743. 10.1200/JCO.2003.04.187.
Marinelli A, Vahrmeijer AL, van de Velde CJ: Phase I/II studies of isolated hepatic perfusion with mitomycin C or melphalan in patients with colorectal cancer hepatic metastases. Recent Results Cancer Res. 1998, 147: 83-94.
Joosse SA, van Beers EH, Nederlof PM: Automated array-CGH optimized for archival formalin-fixed, paraffin-embedded tumor material. BMC Cancer. 2007, 7: 43-10.1186/1471-2407-7-43.
Joosse SA, van Beers EH, Tielen IH, Horlings H, Peterse JL, Hoogerbrugge N, Ligtenberg MJ, Wessels LF, Axwijk P, Verhoef S, et al: Prediction of BRCA1-association in hereditary non-BRCA1/2 breast carcinomas with array-CGH. Breast Cancer Res Treat. 2009, 116: 479-489. 10.1007/s10549-008-0117-z.
van Beers EH, Joosse SA, Ligtenberg MJ, Fles R, Hogervorst FB, Verhoef S, Nederlof PM: A multiplex PCR predictor for aCGH success of FFPE samples. Br J Cancer. 2006, 94: 333-337. 10.1038/sj.bjc.6602889.
Raap AK, van der Burg MJ, Knijnenburg J, Meershoek E, Rosenberg C, Gray JW, Wiegant J, Hodgson JG, Tanke HJ: Array comparative genomic hybridization with cyanin cis-platinum-labeled DNAs. Biotechniques. 2004, 37: 130-134.
Klijn C, Holstege H, de Ridder J, Liu X, Reinders M, Jonkers J, Wessels L: Identification of cancer genes using a statistical framework for multiexperiment analysis of nondiscretized array CGH data. Nucleic Acids Res. 2008, 36: e13-10.1093/nar/gkm1143.
Kallioniemi A, Kallioniemi OP, Sudar D, Rutovitz D, Gray JW, Waldman F, Pinkel D: Comparative genomic hybridization for molecular cytogenetic analysis of solid tumors. Science. 1992, 258: 818-821. 10.1126/science.1359641.
Lemmens VE, Klaver YL, Verwaal VJ, Rutten HJ, Coebergh JW, de Hingh IH: Predictors and survival of synchronous peritoneal carcinomatosis of colorectal origin: A population-based study. Int J Cancer. 2010
Kallioniemi OP, Kallioniemi A, Kurisu W, Thor A, Chen LC, Smith HS, Waldman FM, Pinkel D, Gray JW: ERBB2 amplification in breast cancer analyzed by fluorescence in situ hybridization. Proc Natl Acad Sci USA. 1992, 89: 5321-5325. 10.1073/pnas.89.12.5321.
Kallioniemi A, Kallioniemi OP, Citro G, Sauter G, DeVries S, Kerschmann R, Caroll P, Waldman F: Identification of gains and losses of DNA sequences in primary bladder cancer by comparative genomic hybridization. Genes Chromosomes Cancer. 1995, 12: 213-219. 10.1002/gcc.2870120309.
Iwabuchi H, Sakamoto M, Sakunaga H, Ma YY, Carcangiu ML, Pinkel D, Yang-Feng TL, Gray JW: Genetic analysis of benign, low-grade, and high-grade ovarian tumors. Cancer Res. 1995, 55: 6172-6180.
Fukushige S, Waldman FM, Kimura M, Abe T, Furukawa T, Sunamura M, Kobari M, Horii A: Frequent gain of copy number on the long arm of chromosome 20 in human pancreatic adenocarcinoma. Genes Chromosomes Cancer. 1997, 19: 161-169. 10.1002/(SICI)1098-2264(199707)19:3<161::AID-GCC5>3.0.CO;2-W.
Weiss MM, Snijders AM, Kuipers EJ, Ylstra B, Pinkel D, Meuwissen SG, van Diest PJ, Albertson DG, Meijer GA: Determination of amplicon boundaries at 20q13.2 in tissue samples of human gastric adenocarcinomas by high-resolution microarray comparative genomic hybridization. J Pathol. 2003, 200: 320-326. 10.1002/path.1359.
Postma C, Terwischa S, Hermsen MA, van der Sijp JR, Meijer GA: Gain of chromosome 20q is an indicator of poor prognosis in colorectal cancer. Cell Oncol. 2007, 29: 73-75.
Nanashima A, Yamaguchi H, Yasutake T, Sawai T, Kusano H, Tagawa Y, Nakagoe T, Ayabe H: Gain of chromosome 20 is a frequent aberration in liver metastasis of colorectal cancers. Dig Dis Sci. 1997, 42: 1388-1393. 10.1023/A:1018885803931.
Carvalho B, Postma C, Mongera S, Hopmans E, Diskin S, van de Wiel MA, van Criekinge W, Thas O, Matthai A, Cuesta MA, et al: Multiple putative oncogenes at the chromosome 20q amplicon contribute to colorectal adenoma to carcinoma progression. Gut. 2009, 58: 79-89. 10.1136/gut.2007.143065.
Hermsen M, Postma C, Baak J, Weiss M, Rapallo A, Sciutto A, Roemen G, Arends JW, Williams R, Giaretti W, et al: Colorectal adenoma to carcinoma progression follows multiple pathways of chromosomal instability. Gastroenterology. 2002, 123: 1109-1119. 10.1053/gast.2002.36051.
Knosel T, Schluns K, Stein U, Schwabe H, Schlag PM, Dietel M, Petersen I: Chromosomal alterations during lymphatic and liver metastasis formation of colorectal cancer. Neoplasia. 2004, 6: 23-28.
Nakao M, Kawauchi S, Furuya T, Uchiyama T, Adachi J, Okada T, Ikemoto K, Oga A, Sasaki K: Identification of DNA copy number aberrations associated with metastases of colorectal cancer using array CGH profiles. Cancer Genet Cytogenet. 2009, 188: 70-76. 10.1016/j.cancergencyto.2008.09.013.
Nakao K, Shibusawa M, Ishihara A, Yoshizawa H, Tsunoda A, Kusano M, Kurose A, Makita T, Sasaki K: Genetic changes in colorectal carcinoma tumors with liver metastases analyzed by comparative genomic hybridization and DNA ploidy. Cancer. 2001, 91: 721-726. 10.1002/1097-0142(20010215)91:4<721::AID-CNCR1057>3.0.CO;2-3.
Hu XT, Chen W, Wang D, Shi QL, Zhang FB, Liao YQ, Jin M, He C: The proteasome subunit PSMA7 located on the 20q13 amplicon is overexpressed and associated with liver metastasis in colorectal cancer. Oncol Rep. 2008, 19: 441-446.
Rooney PH, Boonsong A, McFadyen MC, McLeod HL, Cassidy J, Curran S, Murray GI: The candidate oncogene ZNF217 is frequently amplified in colon cancer. J Pathol. 2004, 204: 282-288. 10.1002/path.1632.
Cowger JJ, Zhao Q, Isovic M, Torchia J: Biochemical characterization of the zinc-finger protein 217 transcriptional repressor complex: identification of a ZNF217 consensus recognition sequence. Oncogene. 2007, 26: 3378-3386. 10.1038/sj.onc.1210126.
Douglas EJ, Fiegler H, Rowan A, Halford S, Bicknell DC, Bodmer W, Tomlinson IP, Carter NP: Array comparative genomic hybridization analysis of colorectal cancer cell lines and primary carcinomas. Cancer Res. 2004, 64: 4817-4825. 10.1158/0008-5472.CAN-04-0328.
Takahashi Y, Ishii Y, Nishida Y, Ikarashi M, Nagata T, Nakamura T, Yamamori S, Asai S: Detection of aberrations of ubiquitin-conjugating enzyme E2C gene (UBE2C) in advanced colon cancer with liver metastases by DNA microarray and two-color FISH. Cancer Genet Cytogenet. 2006, 168: 30-35. 10.1016/j.cancergencyto.2005.12.011.
Jackson AL, Mao M, Kobayashi S, Ward T, Biery M, Dai H, Bartz SR, Linsley PS: Chromosome 20q amplification regulates in vitro response to Kinesin-5 inhibitor. Cancer Inform. 2008, 6: 147-164.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/10/662/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SCB: participated in the study design, coordination and data collection, carried out the CGH arrays, participated in the statistical analysis and drafted the manuscript. CK: performed the statistical analysis, participated in the study design and helped to draft the manuscript. G-JL: participated in the study design, participated in the tissue recruitment and participated in collecting patient data. LMB: helped to perform the CGH analysis. SAJ: participated in the statistical analysis and helped to perform the CGH analysis and helped to draft the manuscript. EHvB: participated in the statistical analysis and helped to perform the CGH analysis and helped to draft the manuscript. VJV: participated in the study design and helped to draft the manuscript. HM: participated in the tissue recruitment. LFW: helped to perform the statistical analysis participated in the study design and helped to draft the manuscript. M-LFvV: participated in the study design, performed the histological classification and helped to draft the manuscript. RAEMT: participated in the study design and helped to draft the manuscript. LJv 'tV: conceived of the study, participated in the study design, performed the supervision and coordination and helped to draft the manuscript. All authors read and approved the manuscript.
Electronic supplementary material
12885_2010_2461_MOESM2_ESM.PDF
Additional file 2: Table S1. BAC locations (84) used for the LM-PAM classifier (Figure 4). (PDF 11 KB)
12885_2010_2461_MOESM3_ESM.PDF
Additional file 3: Figure S2. PAM analysis of the Peritoneal Metastases (PM) (2) versus the No metastases (M0) group (3). Arrow: location of the classifier and number (140) of BAC clones in classifier. (PDF 192 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bruin, S.C., Klijn, C., Liefers, GJ. et al. Specific genomic aberrations in primary colorectal cancer are associated with liver metastases. BMC Cancer 10, 662 (2010). https://doi.org/10.1186/1471-2407-10-662
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-10-662