Abstract
Background
Increased mammographic breast density is a moderate risk factor for breast cancer. Different scales have been proposed for classifying mammographic density. This study sought to assess intra-rater agreement for the most widely used scales (Wolfe, Tabár, BI-RADS and Boyd) and compare them in terms of classifying mammograms as high- or low-density.
Methods
The study covered 3572 mammograms drawn from women included in the DDM-Spain study, carried-out in seven Spanish Autonomous Regions. Each mammogram was read by an expert radiologist and classified using the Wolfe, Tabár, BI-RADS and Boyd scales. In addition, 375 mammograms randomly selected were read a second time to estimate intra-rater agreement for each scale using the kappa statistic. Owing to the ordinal nature of the scales, weighted kappa was computed. The entire set of mammograms (3572) was used to calculate agreement among the different scales in classifying high/low-density patterns, with the kappa statistic being computed on a pair-wise basis. High density was defined as follows: percentage of dense tissue greater than 50% for the Boyd, "heterogeneously dense and extremely dense" categories for the BI-RADS, categories P2 and DY for the Wolfe, and categories IV and V for the Tabár scales.
Results
There was good agreement between the first and second reading, with weighted kappa values of 0.84 for Wolfe, 0.71 for Tabár, 0.90 for BI-RADS, and 0.92 for Boyd scale. Furthermore, there was substantial agreement among the different scales in classifying high- versus low-density patterns. Agreement was almost perfect between the quantitative scales, Boyd and BI-RADS, and good for those based on the observed pattern, i.e., Tabár and Wolfe (kappa 0.81). Agreement was lower when comparing a pattern-based (Wolfe or Tabár) versus a quantitative-based (BI-RADS or Boyd) scale. Moreover, the Wolfe and Tabár scales classified more mammograms in the high-risk group, 46.61 and 37.32% respectively, while this percentage was lower for the quantitative scales (21.89% for BI-RADS and 21.86% for Boyd).
Conclusions
Visual scales of mammographic density show a high reproducibility when appropriate training is provided. Their ability to distinguish between high and low risk render them useful for routine use by breast cancer screening programs. Quantitative-based scales are more specific than pattern-based scales in classifying populations in the high-risk group.
Similar content being viewed by others
Background
Increased mammographic breast density is a moderate independent risk factor for breast cancer, ranking only behind age and family history of breast cancer[1, 2]. Different studies have reported an attributable risk of around 30% for mammographic densities of over 50%[3, 4], when classical risk factors, taken together, explain less than 50% of the overall incidence. Although different classifications have been used, the odds ratio for developing breast cancer for the most compared with the least dense breast tissue categories ranges from 1.8 to 6.0, with most studies yielding an odds ratio of 4.0 or greater[5]. Recently, measurement of breast density has been proposed as an intermediate phenotype for breast cancer, useful in epidemiologic, clinical and genetic studies[2]. The first classification was introduced by Wolfe in 1976[6], based on qualitative and quantitative criteria of breast parenchyma to describe four different patterns. Attempts to increase reproducibility entailed the creation of quantitative methods, the most widely used being that proposed by Boyd, which uses a semi-quantitative score of six categories[4]. In 1997, Tabár proposed a modification of Wolfe's classification, with five categories based on anatomic-mammographic correlations[7]. Another classification, Breast Imaging Reporting and Data System (BI-RADS), was developed in the USA to standardize mammography reports, reduce confusion in the interpretation of breast images, and facilitate the monitoring of results.
First edition of BI-RADS classification described four categories of density patterns, but later 2003 edition define them based on quantitative criteria as a quartiles of density percentages [8, 9]. At the end of the nineties computer-assisted measurements of breast density have been developed to calculate percentages of mammographic density but there are some limitations to the technique, such as the digitization of the images, time consumed, need for specific training, difficulty in mixing analog and digital mammograms, and the fact that such techniques continue to be non-volumetric[10, 11]. At present, this computer-assisted method is not routinely used in radiology units, and has not been validated for digital mammograms.
This present study sought to: assess the intra-rater reproducibility of the different visual scales of classification; and compare agreement among the Wolfe, Tabár, BI-RADS and Boyd scales in terms of classification into high- versus low-density groups. Lastly, we explored the variability of the Wolfe and Tabár qualitative pattern-based classifications with respect to the six categories of the Boyd semiquantitative scale.
Methods
Subjects and mammograms
We used data drawn from the "Determinants of Density in Mammography in Spain" (DDM-Spain) study. This was a cross-sectional study which aimed to identify genetic, reproductive and lifestyle characteristics associated with mammographic patterns/densities that might enhance the risk of developing breast cancer. Briefly, women aged 45 and over who attended the regional Breast Cancer Screening Programs at the recruiting centers established in Barcelona, Burgos, Corunna (Coruña), Palma de Mallorca, Pamplona, Valencia and Zaragoza from September 2006 through June 2007 were invited to participate in the study. Exclusion criteria of DDM-Spain included the following: women not born in Spain; evidence of previous breast or ovarian cancer; inability to answer the questionnaire; physical impairment to perform the mammogram; and previous breast surgery or implants. The study was reviewed and approved by the Bioethics Committee of the Instituto de Salud Carlos III (Madrid) and all subjects provided written consent. The intended sample size was 500 women per center, implying a total of 3500 women. The final sample consisted of 3572 women (range 496 to 534 per center). The average participation rate was 74.5%, ranging from 64.7% in Corunna to 84.0% in Zaragoza. Mammogram quality at each of these centers had been explored by a pilot study using 25 mammograms per center. As the cranio-caudal (CC) projection posed fewer technical problems, we decided to evaluate mammographic density using the CC projection from the left breast.
Of the total included in the study, 2040 mammograms were in analog format (those from Burgos, Corunna, Pamplona and Zaragoza) and the remaining 1532 were in digital format (those from Barcelona, Palma de Mallorca and Valencia).
Measurements
Mammographic density was evaluated by a single experienced radiologist (Dr. Francisco Ruíz-Perales). All mammograms were classified using the Wolfe, Tabár, BI-RADS and Boyd scales: analog mammograms were read in negatoscope (view box), and digital mammograms on a computer screen. Every mammogram (in total 3572) was read randomly in four different stages to prevent recall bias until every scale was completed to study comparability among scales.
To obtain a subsample of twice-read mammograms to explore intra-observer agreement each of the participant centers chose a set of 50-60 consecutive images using a random number between the first and last mammograms as initial. If the random number proposed was too near the last, the reading continued from the first. The second reading of a total of 375 mammograms was performed with the same procedure than first beginning within 1 to 66 days after the end of the previous reading to prevent recall bias.
Statistical methods
Intra-observer agreement was evaluated using the kappa coefficient, since it requires no assumption about correct categorization and includes correction for the degree of agreement that would be expected by chance alone[12]. Due to the ordinal nature of the scales, weighted kappa was also calculated.
Wolfe scale is compound of four categories defined as N1, P1, P2 and DY while Tabár proposed five different patterns from I to V (See table 1 and table 2 for further description of categories).
Quantitative based scales, BI-RADS and Boyd, are defined using percentages of density. BI-RADS into quartiles and Boyd divided into six categories of unequal intervals: "A" 0%; "B" > 0-10%; "C" > 10-25%; "D" > 25-50%; "E" > 50-75% and "F" > 75% (Table 3 and 4).
To compare different classification scales having different numbers of categories, a dichotomous re-classification was defined for each scale, grouping different categories into low- and high-risk groups (Table 1, 2, 3 and 4). The Wolfe classification low-risk group was formed by categories N1 and P1 and the high-risk group by categories P2 and DY. For Tabár classification, I-III were considered low-risk and IV-V high-risk. BI-RADS was divided into low-risk (almost entirely fat and scattered fibroglandular densities) and high-risk (heterogeneously dense and extremely dense). Finally, in the Boyd classification, mammograms classified as A, B, C and D were included in the low-risk group, and E and F categories as high-risk.
High/low-risk classifications enabled agreement between the four scales to be compared, using percentage agreement and the kappa statistic. Comparison between the pattern-based classification of the Wolfe, Tabár scales and semi-quantitative scales, BI-RADS and Boyd, was studied graphically to observe how their respective categories expressed density percentages.
Confidence intervals were calculated. Bootstrapping methods were used when more than two categories or weighted kappa were involved; to optimize the results, bootstrapping was performed with 5000 replications. In high/low-risk categorization, confidence intervals for the kappa statistic were calculated using a previously described analytical method[13].
All statistical analyses were performed using the Stata version 10 computer software program.
Results
Intra-observer agreement
Wolfe's classification
Table 1 shows agreement between the first and second measurements using the Wolfe scale, with 308 of the 375 (82.13%) images being consistently classified. Only 1.86% of the observations showed disagreement in two categories. The kappa value was 0.73 (p < 0.0001) and the weighted kappa value was 0.84 (p < 0.0001). Using aggregated data in two categories (low- and high-risk), the kappa statistic was 0.85 (p < 0.0001).
Kappa values for analog and digital measures were 0.78 (p < 0.0001, 95% CI: 0.706-0.846) and 0.67 (p < 0.0001, 95% CI: 0.575-0.764), and weighted kappa values were 00.87 (p < 0.0001, 95% CI: 0.808-0.916) and 0.78 (p < 0.0001, 95% CI: 0.686-0.856), respectively
Tabár's classification
Comparisons between first and second measures with Tabár classification are shown in Table 2. The percentage of total agreement was 82.93% (311 of 375 measures were exactly the same). Only 4.27% of the measures differed in two categories. The kappa value was 0.72 (p < 0.0001) and that of weighted kappa 0.71 (p < 0.0001). When the scale was divided into low and high risk, the kappa value was 0.80 (p < 0.0001)
Kappa values for analog and digital measures were 0.77 (p < 0.0001; 95% CI: 0.685-0.838) and 0.62 (p < 0.0001; 95% CI: 0.497-0.721), and weighted kappa values were 0.75 (p < 0.0001; 95% CI: 0.641-0.845) and 0.64 (p < 0.0001; 95% CI: 0.494-0.764), respectively.
BI-RADS classification
Using the BI-RADS scale, 315 of 375 images were classified in the same category (84% agreement). No observations differed in more than one category, as can be seen in Table 3. The kappa value for BI-RADS classification was 0.76 (p < 0.0001) and weighted kappa was 0.90 (p < 0.0001). High/low-risk classification resulted in a kappa value of 0.82 (p < 0.0001).
Kappa values for analog and digital measures were 0.76 (p < 0.0001; 95% CI: 0.683-0.829) and 0.76 (p < 0.0001; 95% CI: 0.676-0.842), and weighted kappa values were 0.90 (p < 0.0001; 95% CI: 0.864-0.932) and 0.90 (p < 0.0001; 95% CI: 0.860-0.938), respectively.
Boyd's classification
Table 4 summarizes the agreement between the first and second measure using the Boyd scale. Total agreement was 74.93% (281 of 375 measures were identically classified). There were no observations with disagreement in more than one category. The kappa value was 0.68 (p < 0.0001) and weighted kappa was 0.92 (p < 0.0001). Using the two-category scale, the kappa statistic was 0.82 (p < 0.0001).
Kappa values for analog and digital measures were 0.70 (p < 0.0001; 95% CI: 0.626-0.774) and 0.63 (p < 0.0001; 95% CI: 0.547-0.724), and weighted kappa values were 0.92 (p < 0.0001; 95% CI: 0.890-0.940) and 0.91 (p < 0.0001; 95% CI: 0.884-0.936), respectively
Comparability among scales
High/low-risk categorizations enabled the four scales to be compared. The bivariate study of interscale agreement is summarized in Table 5.
Wolfe's classification
Wolfe classified 53.39% of the mammograms as low-risk and 46.61% as high-risk. Total agreement between Wolfe's and the Boyd, BI-RADS and Tabár scales was 75.25%, 75.22% and 90.37% with kappa values of 0.49, 0.49 and 0.80, respectively.
Tabár's classification
Using Tabár's classification, 37.32% mammograms were classified as high-risk.
Whereas Tabár displayed almost perfect agreement with Wolfe (90.37% agreement and a kappa value of 0.80 (p < 0.00001)), agreement with BI-RADS and Boyd was lower (84.46% and 84.49%, respectively), with kappa values of 0.64 for both (p < 0.0001)
BI-RADS classification
BI-RADS classified 21.89% mammograms as high-risk. BI-RADS agreement with the other classifications was as follows: Wolfe, 75.22%, and a kappa value of 0.48 (p < 0.0001); Tabár, 84.46%, and a kappa value of 0.64; BI-RADS and Boyd, almost perfect (99.97% total agreement and a kappa value of almost 1.00, namely, 0.99992 with p < 0.0001).
Boyd's classification
Boyd classified 78.14% of mammograms as low-risk and 21.86% as high-risk. It showed almost perfect agreement with BI-RADS (99.97% total agreement and a kappa value of almost 1, namely, 0.9992, p < 0.0001), good agreement with Tabár (84.49% agreement and a kappa value of 0.64, p < 0.0001), and moderate agreement with Wolfe (75.25% agreement and a kappa value of 0.49, p < 0.0001).
Graphic distribution study of qualitative scales of mammographic density measurement (Wolfe, Tabár and BI-RADS) with respect to a semi-quantitative scale (Boyd)
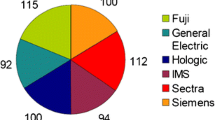
Figure 1 shows the distribution of the different qualitative (i.e., pattern-based) scales of mammographic density measurement with respect to Boyd's scale. Low-risk categories are represented in blue and high-risk categories in violet-purple. Boyd categories A, B, C and D correspond to low risk, and E and F to high risk.
None of the mammograms of low-risk categories of the Wolfe scale, N1 and P1, were included in the high-risk categories of the Boyd scale (E and F) and only one mammogram classified as low risk, category III, using Tabár scale was included in the high risk category E of Boyd scale. Categories N1 (Wolfe) and II (Tabár) are classified mainly into categories A or B of Boyd scale (≤ 10% of density) and categories P1 and III into B, C or D (> 0-50%). On the other hand, 24.75% of the mammograms included in high-risk categories P2 and DY using Wolfe method, were included in low-risk categories, almost all in D category, using Boyd scale. For Tabár scale the percentage was lower, 15.48% (15.34% in D).
Category-D mammograms, namely, those with 25% to 50% density, displayed a more heterogeneous distribution under Wolfe's and Tabár's systems.
Discussion
Different methods in use, subjective classifications, and the lack of a gold standard mean that misclassification is a potential problem when assessing mammographic density and potential breast cancer risk. Previous studies have measured inter- and intra-observer variability using experienced radiologists. Most of these studies report good or very good agreement[14–23]. Reliability studies of Wolfe's classification show kappa values ranging from 0.69 to 0.88 for inter-observer agreement, and 0.69 to 0.87 for intra-observer agreement[14–18]. In previous studies: Tabár inter-observer agreement obtained kappa values of 0.63 and of 0.75 for intra-observed agreement[19]; BI-RADS classification displayed only moderate agreement, with an overall kappa value for intra-observer agreement of 0.43-0.59[20, 21]; and Boyd's classification registered inter-observer agreement of 0.89[22] and a kappa value of 0.74[18], with a weighted kappa value for intra-observer agreement of 0.68-0.89[19, 23].
In our study, good intra-observer reproducibility was observed, particularly when weighted kappa was used. Only the Wolfe and Tabár scales showed disagreement in more than one category in 7 (1.86%) and 16 (4.27%) cases, respectively: six of these cases were classified on both scales with disagreement in two categories, perhaps due to specific characteristics of these mammograms which hindered their evaluation. Only one classification -Boyd's- registered a kappa value of under 0.70, namely, 0.68. Nevertheless, all the disagreements observed (25.06%) corresponded to differences in only one category. It should be noted that Boyd's classification is divided into six categories, with three categories -A, B and C- classifying densities under 25 percent with narrower range intervals than the rest. Half of all mammograms with different results in both readings belonged to these three categories. Taking into account the number of categories and the semi-quantitative nature of the Boyd scale, weighted kappa is a more appropriate estimator of concordance. Using this statistic, concordance for Boyd's scale was 0.92. The other classifications registered agreement percentages of 82% to 84%, and weighted kappa values of over 0.75. Previous studies using the BI-RADS scale reported moderate agreement, with kappa statistics of 0.43 to 0.59 for intra-observer studies[16, 17]. We obtained kappa and weighted kappa values of 0.76 and 0.90 respectively, showing very good agreement.
When comparing the different scales, kappa values for distinguishing high-density mammographic patterns ranged from 0.79 to 0.86, revealing almost perfect agreement. This good correlation among the different scales explains the consistency of results on the relationship between mammographic density and breast cancer obtained from different studies using different scales[1, 2]. It is interesting to note, however, that classifications, such as Tabár's and Wolfe's, which consider both qualitative and quantitative information on density, displayed lower concordance with the semi-quantitative scale. A more detailed analysis confirmed that these scales registered the greatest disagreement in mammograms in the intermediate dense-tissue percentage category, i.e., ranging from 25% to 50%. This means that categories associated to high risk of the Wolfe and Tabár scales are classify with a huge variability from 25 to 100% of density using quantitative based scales and some women are classified into low (< 50% of density) or high risk group depending on the method selected. It would have been interesting to ascertain to what extent qualitative information in such cases determined differences in breast cancer risk and the clinical relevance of classifying different population into high and low risk but our study was unable to address this issue directly.
Separate comparison between digital and analog images failed to reveal relevant differences, yielding weighted kappa values for analog versus digital of: 0.87 versus 0.78 using Wolfe's scale; 0.75 versus 0.64 using Tabár's scale; 0.90 versus 0.90 using the BI-RADS scale; and 0.92 versus 0.91 using Boyd's scale. Even though these differences did not attain statistical significance, the kappa values were always slightly higher when our reader examined analog images. This may reflect his longer experience with the old technology, since digital mammographic technology has only recently been introduced in Spanish screening programs.
Limitations are intra-observer design of the study and the lack of comparison with computer-assisted methods, which would result in more objective measurements of breast density, slightly higher agreement values, and the possibility of obtaining a measure of density percentages as a continuous variable. Furthermore, such methods are also dependent on observer experience, since the program has to be given some pointers to enable it to delimit the area in which it must calculate the percentage of the breast occupied by dense tissue[1, 2]. This technique has not been introduced in Spanish breast cancer screening programs, and no radiologist or technician with the necessary experimental training could be found who was able to use it. Previous studies have shown excellent reproducibility, with an intraclass correlation of over 0.9[11] and a Pearson correlation with r values of over 0.90[10], when this method was used on previously digitized analog images.
Conclusions
Visual classification of mammographic density patterns, besides being quick and easy to perform, is a relatively inexpensive method to implement in breast cancer screening programs. Our study confirms that, using an experienced reader, the four scales display very high reproducibility and are extremely consistent in identifying women with high-density patterns. Quantitative-based scales are more specific in classifying populations in the high-risk group.
Abbreviations
- BI-RADS:
-
Breast Imaging Reporting and Data System
- DDM-Spain study:
-
Determinants of Density in Mammography in Spain
References
Cummings SR, Tice JA, Bauer S, Browner WS, Cuzick J, Ziv E, Vogel V, Shepherd J, Vachon C, Smith-Bindman R, Kerlikowske K: Prevention of Breast Cancer in Postmenopausal Women: Approaches to Estimating and Reducing Risk. J Natl Cancer Inst. 2009, 101: 384-398. 10.1093/jnci/djp018.
Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, Paterson AD: Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005, 6: 798-808. 10.1016/S1470-2045(05)70390-9.
Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton L, Hoover R, Haile R: Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995, 87 (21): 1622-1629. 10.1093/jnci/87.21.1622.
Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, Lockwood GA, Tritchler DL, Yaffe MJ: Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995, 87: 670-675. 10.1093/jnci/87.9.670.
Harvey JA, Bovbjerg VE: Quantitative assessment of mammographic breast density: relationship with breast cancer risk. Radiology. 2004, 230: 29-41. 10.1148/radiol.2301020870.
Wolfe JN: Breast patterns as an index of risk for developing breast cancer. AJR Am J Roentgenol. 1976, 126: 1130-1137.
Gram IT, Funkhouser E, Tabar L: The Tabar classification of mammographic parenchymal patterns. Eur J Radiol. 1997, 24: 131-136. 10.1016/S0720-048X(96)01138-2.
American College of Radiology: ACR Breast imaging reporting and data system. 1993, Reston, VA: American College of Radiology
American College of Radiology: ACR breast imaging reporting and data system atlas. 2003, Reston, VA: American College of Radiology
Chang YH, Wang XH, Hardesty LA, Chang TS, Poller WR, Good WF, Gur D: Computerized assessment of tissue composition on digitized mammograms. Acad Radiol. 2002, 9: 899-905. 10.1016/S1076-6332(03)80459-2.
Byng JW, Yaffe MJ, Jong RA, Shumak RS, Lockwood GA, Tritchler DL, Boyd NF: Analysis of mammographic density and breast cancer risk from digitized mammograms. Radiographics. 1998, 18: 1587-1598.
Cohen J: A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960, 20: 37-46. 10.1177/001316446002000104.
Reichenheim ME: Confidence intervals for the kappa statistic. The Stata Journal. 2004, 4: 421-428.
Moskowitz M, Gartside P, McLaughlin C: Mammographic patterns as markers for high-risk benign breast disease and incident cancers. Radiology. 1980, 134: 293-295.
Boyd NF, O'Sullivan B, Campbell JE, Fishell E, Simor I, Cooke G, Germanson T: Bias and the association of mammographic parenchymal patterns with breast cancer. Br J Cancer. 1982, 45: 179-184.
Carlile T, Thompson DJ, Kopecky KJ, Gilbert FI, Krook PM, Present AJ, Russell HW, Threatt BA: Reproducibility and consistency in classification of breast parenchymal patterns. AJR Am J Roentgenol. 1983, 140: 1-7.
Toniolo P, Bleich AR, Beinart C, Koenig KL: Reproducibility of Wolfe's classification of mammographic parenchymal patterns. Prev Med. 1992, 21: 1-7. 10.1016/0091-7435(92)90001-X.
Gao J, Warren R, Warren-Forward H, Forbes JF: Reproducibility of visual assessment on mammographic density. Breast Cancer Res Treat. 2008, 108: 121-127. 10.1007/s10549-007-9581-0.
Jamal N, Ng KH, Looi LM, McLean D, Zulfiqar A, Tan SP, Liew WF, Shantini A, Ranganathan S: Quantitative assessment of breast density from digitized mammograms into Tabar's patterns. Phys Med Biol. 2006, 51: 5843-5857. 10.1088/0031-9155/51/22/008.
Berg WA, Campassi C, Langenberg P, Sexton MJ: Breast Imaging Reporting and Data System: inter- and intraobserver variability in feature analysis and final assessment. AJR Am J Roentgenol. 2000, 174: 1769-1777.
Kerlikowske K, Grady D, Barclay J, Frankel SD, Ominsky SH, Sickles EA, Ernster V: Variability and accuracy in mammographic interpretation using the American College of Radiology Breast Imaging Reporting and Data System. J Natl Cancer Inst. 1998, 90: 1801-1809. 10.1093/jnci/90.23.1801.
Jong R, Fishell E, Little L, Lockwood G, Boyd NF: Mammographic signs of potential relevance to breast cancer risk: the agreement of radiologists' classification. Eur J Cancer Prev. 1996, 5: 281-286. 10.1097/00008469-199608000-00008.
Lee-Han H, Cooke G, Boyd NF: Quantitative evaluation of mammographic densities: a comparison of methods of assessment. Eur J Cancer Prev. 1995, 4: 285-292. 10.1097/00008469-199508000-00003.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/10/485/prepub
Acknowledgements
This study was supported by research grant FIS PI060386 from Fondo de Investigación Sanitaria, Spain and by collaboration agreement EPY 1306/06 between Astra-Zeneca and the Carlos III Institute of Health.
We should like to thank all the women who participated in the DDM-Spain study for their contribution; the respective regional screening-program staff and the other members of DDM-Spain for their invaluable collaboration and effort: Soledad Abad, Manuela Alcaraz, Nuria Aragonés, Anna Cabanes, Monserrat Corujo, Ana-Belén Fernández, Pablo Fernández-Navarro, Milagros García-López, Marcela Guevara, Soledad Laso-Pablos,, Virginia Lope, Gonzalo López-Abente, Carmen Pedraz, Beatriz Pérez-Gómez, Roberto Pastor, Juana Vidan, Jesús Vioque.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MP was responsible for the study concept. NA, IGR, CSC, CS, PM, CV & DS were the main responsible of DDM-Study in the corresponding screening programs and provided valuable input to the study desing. FRP & JM conducted a pilot study to verify the quality of mammograms in the different programs. FRP evaluated mammographic density using the four scales. MG & MP performed the statistical analysis and prepared the first draft of the manuscript. The rest of the authors were involved in the field work of the study, recruiting participants, collecting the corresponding mammograms and the information needed to carry out the study. All authors critically revised the manuscript and suggested helpful comments that were subsequently introduced in the text. All authors read & approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Garrido-Estepa, M., Ruiz-Perales, F., Miranda, J. et al. Evaluation of mammographic density patterns: reproducibility and concordance among scales. BMC Cancer 10, 485 (2010). https://doi.org/10.1186/1471-2407-10-485
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-10-485