Abstract
Background
Reliable antenatal identification of pre-eclampsia and small for gestational age is crucial to judicious allocation of monitoring resources and use of preventative treatment with the prospect of improving maternal/perinatal outcome. The purpose of this systematic review was to determine the accuracy of five serum analytes used in Down's serum screening for prediction of pre-eclampsia and/or small for gestational age.
Methods
The data sources included Medline, Embase, Cochrane library, Medion (inception to February 2007), hand searching of relevant journals, reference list checking of included articles, contact with experts. Two reviewers independently selected the articles in which the accuracy of an analyte used in Downs's serum screening before the 25th gestational week was associated with the occurrence of pre-eclampsia and/or small for gestational age without language restrictions. Two authors independently extracted data on study characteristics, quality and results.
Results
Five serum screening markers were evaluated. 44 studies, testing 169,637 pregnant women (4376 pre-eclampsia cases) and 86 studies, testing 382,005 women (20,339 fetal growth restriction cases) met the selection criteria. The results showed low predictive accuracy overall. For pre-eclampsia the best predictor was inhibin A>2.79MoM positive likelihood ratio 19.52 (8.33,45.79) and negative likelihood ratio 0.30 (0.13,0.68) (single study). For small for gestational age it was AFP>2.0MoM to predict birth weight < 10th centile with birth < 37 weeks positive likelihood ratio 27.96 (8.02,97.48) and negative likelihood ratio 0.78 (0.55,1.11) (single study). A potential clinical application using aspirin as a treatment is given as an example.
There were methodological and reporting limitations in the included studies thus studies were heterogeneous giving pooled results with wide confidence intervals.
Conclusion
Down's serum screening analytes have low predictive accuracy for pre-eclampsia and small for gestational age. They may be a useful means of risk assessment or of use in prediction when combined with other tests.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Pre-eclampsia (PET) and small for gestational age (SGA) remain significant causes of perinatal death and childhood disability [1–3]. PET has significant health implications for the mother with complications including adult respiratory distress syndrome, coagulopathy, renal and liver failure and stroke. Babies affected by SGA on reaching adulthood are at greater risk of developing cardiovascular disease, hypertension, and non-insulin dependent diabetes [4, 5]. Both PET and SGA are characterized by a failure of the trophoblast invasion (at 16–22 weeks) into the spiral arteries.
Second trimester serum screening for Down's syndrome is routinely offered to women in the United Kingdom and United States, either with the triple test (alpha-fetoprotein (AFP), human chorionic gonadotrophin (HCG) and unconjugated estriol) or with the addition of inhibin A as the quadruple test. More recently first trimester screening with fetal nuchal translucency, HCG and pregnancy associated plasma protein A (PAPP-A) has provided an earlier, more effective screening method [6]. Due to their origin and sites of metabolism these biochemical markers may be useful in the prediction of PET and SGA, there are however conflicting reports in the literature. Maternal serum levels of these analytes have been shown to be associated with adverse outcome [7, 8] with low levels of PAPP-A having been suggested as a marker for impaired placental function and placentation [9]. There are studies however reporting contrasting views [10].
Reliable antenatal identification of PET and SGA is crucial to judicious allocation of monitoring resources and use of preventative treatment [11] with the prospect of improving maternal and perinatal outcome. The variation in the design of research on accuracy of tests for prediction of PET and SGA, the scatter of this research across many databases and languages, and the dearth of clear collated up-to-date summaries of this literature contribute to the uncertainty about the best screening and monitoring strategies [12]. Systematic reviews of the literature can improve our ability to identify those pregnancies at increased risk of developing PET and SGA making additional use of test results already obtained for Down syndrome screening.
The purpose of our review was to investigate the accuracy of serum biochemical markers used in first and second trimester Down syndrome serum screening in predicting PET and/or SGA. We systematically reviewed the available literature and meta-analysed the data.
Methods
The systematic review was based on our previously published prospective protocols [13, 14] designed using widely recommended methods [15–18]. The protocols are available as Additional files 1 and 2.
Data sources and searches
Electronic searches were performed by experienced clinical librarians targeting the prediction of PET and SGA. We searched Medline, Embase, the Cochrane Library (2006;4) and Medion from inception until February 2007. The search strategies are detailed in the published protocols [13, 14] and in Additional file 3. The reference lists of all included primary and review articles were examined to identify cited articles not captured by electronic searches. No language restrictions were applied.
Study selection
The first stage of study selection was the scrutinizing of the database by two reviewers to identify articles from title and/or abstract. In a second stage, a search based on keywords for each of the analytes under review was performed within the Reference Manager database. The results of this search were scrutinized by a second reviewer. In the final stage of study selection the full papers of identified articles were obtained with final inclusion or exclusion decisions made after independent and duplicate examination of the papers. We included studies that reported on singleton pregnancies at any level of risk in any healthcare setting using any serum biochemical test used in Down syndrome serum screening before the 25th week of gestation. Test accuracy studies allowing generation of 2 × 2 tables were included.
Data extraction and Study Quality Assessment
Further details on inclusion and exclusion criteria and extracted clinical, methodological and statistical data can be found in the published protocols.
Acceptable reference standards for PET were: persistent systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg with proteinuria ≥ 0.3 g/24 hours or ≥ 1+ dipstick (= 30 mg/dl in a single urine sample), new after 20 weeks of gestation. Severe PET was defined as SBP ≥ 160 mmHg or DBP ≥ 110 mmHg with proteinuria ≥ 2.0 g/24 hours or ≥ 3+ dipstick, or of early onset < 34 weeks gestation. Superimposed PET was defined as the development of proteinuria ≥ 0.3 g/24 hours or ≥ 1+ dipstick after 20 weeks gestation in chronically hypertensive patients [19]. Acceptable reference standards for SGA included birth weight < 10th centile adjusted for gestational age and based on local population values and absolute birth weight threshold < 2500 g. Severe SGA was defined as birth weight < 5th or < 3rd centile or < 1750 g or and preterm SGA for SGA leading to delivery < 37 weeks. Neonatal ponderal index < 10th centile, skin fold thickness, and mid-arm circumference/head circumference were also assessed [20–24].
Disagreements were resolved by consensus or arbitration of a third reviewer. For multiple/duplicate publication of the same data set, the most recent and/or complete study was included only.
All included manuscripts were assessed by at least one reviewer for study and reporting quality using validated tools [25–30]. Methodological quality was defined as the confidence that the study design, conduct and analysis have minimized biases in addressing the research question, thereby focusing on the internal validity (i.e. the degree to which the results of an observation are correct for the patients being studied). Items considered important for a good quality paper were prospective design with consecutive recruitment, full verification of the test result with reference standard (> 90%), adequate description of the index test and use of appropriate reference standard, and application of any preventative treatments. Additional quality items were assessed for SGA papers; whether they excluded cases of PET from the results, whether fetuses with chromosomal and structural anomalies were excluded and whether stillbirths and intrauterine deaths were excluded from the results. Further explanation of the quality assessment can be found in Additional file 4.
We excluded from the statistical analysis any paper with a case-control design as this type of design in diagnostic test accuracy studies has been shown to be associated with bias and over/under estimation of accuracy [29].
Data synthesis and Analysis
From the 2 × 2 tables the following were calculated with their 95% confidence intervals for individual studies; sensitivity (true positive rate), specificity (true negative rate) and the likelihood ratios (LR, the ratio of the probability of the specific test result in people who do have the disease to the probability in people who do not). LRs indicate by how much a given test result raises or lowers the probability of having the disease and have been recommended by Evidence-based Medicine Groups [31, 32]. Results were pooled among groups of studies with similar characteristics, the same threshold for the index test (PET and SGA), same reference standard threshold for (SGA) and the same trimester for testing. Where 2 × 2 tables contained zero cells, 0.5 was added to each cell to enable calculations.
Sub-groups were defined at the start of the review based on clinical criteria known to affect prognosis, method of index test or study quality: level of risk of population (high or low based on authors assessment and calculated incidence rates from results); type of assay used for index test; whether babies with chromosomal anomalies were excluded from the results; use of preventative treatment; quality of study. Sub-group analyses were performed where there were at least 3 studies with similar characteristics within that group.
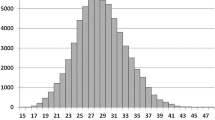
Heterogeneity was assessed graphically by looking at the distribution of the sensitivities and specificities in the receiver operating characteristic (ROC) space and LRs as a measurement of accuracy size using a Forest plot. The loglikelihood and X2 test were used to assess for heterogeneity statistically. When X2 p value > 0.05 (homogenous data) the fixed effect pooling method was used; where there was heterogeneity random effects pooling was used. Summary ROC plots were produced (data not shown). Sensitivity analysis was performed to check the robustness of our results. A p value of < 0.05 was used throughout for statistical significance.
All statistical analyses were performed using Meta-Disc software http://www.hrc.es/investigacion/metadisc.html and Statsdirect for drawing the Forest plots.
Clinical application
The clinical impact of estimates of accuracy for a screening test depend on how the results of the test alter the patient's pre-test probability of disease, based on disease prevalence. The post-test probability can then be combined with estimates of effectiveness for known treatments [33]. From this data we can then calculate the number of women needed to be tested (number needed to test- NNTest), using a particular serum marker, to prevent one case of SGA with a particular treatment and the number needed to treat (NNTreat), the number of test positive women needed to be treated to prevent one case of SGA. In this review clinical application will be assessed using aspirin as this is the only treatment with any level of effectiveness for PET and SGA [11, 34].
Results
Literature identification, study characteristics, and quality
Figure 1 summarises the process of literature identification and selection. Tables detailing the individual study characteristics of the included studies are available in Additional file 5. There were twenty studies that reported on both PET and SGA.
Pre-eclampsia
There were 44 included studies for pre-eclampsia [7, 9, 35–75] reporting on 169,637 women (4376 preeclamptic women, incidence 2.6%). Among these 44 studies, there were 35 cohort studies and nine case-control studies [41, 43, 44, 48, 51, 55, 63, 72, 73]. There were nine prospective studies, 10 retrospective and 25 were unclearly designed. Calculated incidence rates of PET ranged from 0.6–44%. Incidence rates of PET correlated poorly with descriptions of "high" or "low" risk study populations. Four of the studies were in "high-risk" populations (one in IVF patients, one in patients with abnormal uterine artery Doppler and two in patients with chronic hypertension) and in three of these studies the incidence of PET was > 4%. However in 15 of the "low-risk" studies the incidence was > 4% and in one study in which the inclusion criteria were unclearly reported. The remaining 25 studies were in low risk, screening populations with a calculated incidence of PET < 4%.
Ten studies were performed in the first trimester, 32 studies at a mean gestation between 15 to 20 weeks and two studies 20 to 24 weeks.
The quality assessment of included studies for PET is summarized in Figure 2. There was poor reporting of patient selection criteria, description of index and reference tests and blinding of the reference test. Only two studies reported clearly whether preventative treatment had been used. The nine case control studies were excluded from the final meta-analysis, leaving 35 cohort studies for analysis.
Small for gestational age
There were 86 included studies for SGA [7, 9, 37, 39, 47, 51, 53–55, 57, 59–61, 64–67, 69, 74, 76–141], reporting on 382,005 women (20339 cases of SGA, incidence 5.32%). Among these studies, there were 61 cohort studies and 25 case control studies [53, 55, 76, 77, 82–85, 88, 89, 94, 96, 97, 104, 113, 116, 119, 123–125, 130, 131, 133, 135, 140]. Thirty-one studies were prospective, 17 retrospective and 38 of unclear design. Calculated incidence rates of SGA correlated well with the threshold used in 78 of studies and poorly in 8, incidence range for birth weight < 10th centile was 1.2–63%. Three of the studies were performed in high risk populations, whereas the remainder were performed in low risk or screening populations. Due to the inclusion criteria of the studies the majority of tests were performed between 15 to 20 weeks. There were ten studies reporting on first trimester screening. Fifty studies reported on birth weight < 10th centile, 13 on birth weight < 5th centile, 27 on birth weight < 2500 g, 1 on birth weight < 1500 g, 1 on birth weight < 15th centile and 12 reported no threshold.
The quality assessment of included studies for SGA revealed deficiencies (Figure 2). Only 40 studies contained an adequate description of the performance of the index test. None of the studies reported clearly on the performance of the reference standard. Blinding of the reference test was also poorly reported as was the use of any treatment in between the index test and reference standard. These items of quality of study design are important in diagnostic accuracy reviews.
Four papers only distinguished between SGA with PET and SGA alone; intrauterine deaths and stillbirths were excluded from the results for SGA in only 16 papers, in the remainder it was unclear; chromosomal and structural anomalies were excluded from 62 studies, unclear in 24
Twenty-five case control studies and eight studies [78, 81, 98, 105, 122, 127, 129, 138] in which thresholds for SGA were not defined were excluded from the final meta-analysis, leaving 53 studies.
Data analysis
For both analysis for PET and analysis for SGA, there was significant heterogeneity in all results. As a consequence of this the random effects model was used throughout the study.
Maternal serum alpha fetoprotein (AFP)
The results for AFP are summarized in Figure 3, all studies were performed in the second trimester. For PET there were sixteen studies included in the meta-analysis. Thresholds that were most commonly used were > 2.0MoM (multiples of median) (10 studies) and > 2.5MoM (6 studies). The most accurate predictor was AFP>2.0 MoM; LR+ 2.36 (1.46,3.83), LR- 0.96 (0.95,0.98). (One study had a better positive LR however this threshold was chosen from receiver operating curve analysis AFP>1.28MoM; LR+ 3.30 (2.00,5.43), LR- 0.44(0.22,0.90)).
Forest Plot showing likelihood ratio of a positive and negative test result with 95% confidence intervals (95% CI) for studies of alpha feto-protein (AFP) to predict pre-eclampsia and small for gestational age (birth weight threshold as indicated). Results with diamonds are pooled results (number of studies as indicated), results with squares are single studies. The number of women included in the studies is shown, all studies second trimester testing.
For SGA there were thirty studies included in the meta-analysis. The commonest threshold used were > 2.0MoM (10 studies) and > 2.5MoM (5 studies) to predict birth weight < 10th centile. The best predictor for birth weight < 10th centile was AFP<10th centile; LR+ 8.80 (5.57,13.91), LR- 0.02 (0.00,0.34), this was a single study. For birth weight < 5th centile and birth weight < 2500 g, AFP>3.0MoM was the most accurate predictor. The most accurate predictor overall was AFP>2.0MoM to predict severe SGA (birth weight < 10th centile with birth < 37 weeks): LR+ 27.96 (8.02,97.48), LR- 0.78 (0.55, 1.11).
Maternal serum human chorionic gonadotrophin (HCG)
The results for HCG are summarized in Figure 4. There were forty seven studies overall evaluating HCG, nine for free β-HCG, eight total β-HCG and 30 total HCG. For PET there were 21 included studies in the meta-analysis, 3 looked at testing in the first trimester. The commonest thresholds used were HCG>2.0MoM (12 studies), HCG>2.5MoM (4 studies) and HCG>3.0MoM (3 studies). The most accurate predictor was HCG>2.0MoM with second trimester testing; LR+ 2.45 (1.57,3.84), LR- 0.89 (0.83,0.96). There was one study looking at severe PET as the outcome, results showed no improvement in prediction.
Forest Plot showing likelihood ratio of a positive and negative test result with 95% confidence intervals (95% CI) for studies of human chorionic gonadotrophin (HCG) to predict pre-eclampsia and small for gestational age (birth weight threshold as indicated). Results with diamonds are pooled results (number of studies as indicated), results with squares are single studies. The number of women included in the studies is shown. (a first trimester testing).
For SGA there were 22 included studies in the meta-analysis, 5 looked at testing in the first trimester. The commonest thresholds used were HCG>2.0MoM (7 studies) and HCG>2.5MoM (4 studies) for birth weight < 10th centile. The most accurate predictor for birth weight < 10th centile was HCG>2.0MoM; LR+ 1.74 (1.48,2.04), LR- 0.95 (0.93,0.96). For birth weight < 5th centile HCG>2.0MoM in the second trimester was the most accurate and for birth weight < 2500 g HCG>2.5MoM.
Maternal serum unconjugated Estriol
The results for unconjugated estriol are summarized in Figure 5, all studies were performed in the second trimester. For PET there were 4 included studies, the commonest threshold being estriol<0.5MoM (2 studies), this was also the most accurate predictor; LR+ 1.50 (1.02,2.19), LR- 0.99 (0.97,1.00).
Forest Plot showing likelihood ratio of a positive and negative test result with 95% confidence intervals (95% CI) for studies of estriol to predict pre-eclampsia and small for gestational age (birth weight threshold as indicated). Results with diamonds are pooled results (number of studies as indicated), results with squares are single studies. The number of women included in the studies is shown, all studies second trimester testing.
For SGA there were 7 included studies, the commonest threshold was estriol<0.75MoM (2 studies) for birth weight < 10th centile. The most accurate predictor for birth weight < 10th centile was estriol<0.75MoM; LR+ 2.54 (1.54,4.19), LR- 0.75 (0.63,0.89). For birth weight < 5th centile there were 2 studies for estriol<0.5 MoM; LR+ 6.54 (0.98,43.91), LR- 0.59 (0.03,13.28).
Maternal serum pregnancy associated plasma protein A (PAPP-A)
The results for PAPP-A are summarized in Figure 6. For PET there were 16 included studies, all performed in the first trimester, the commonest threshold was PAPP-A<5th centile (5 studies) and PAPP-A<10th centile (3 studies). The most accurate predictor was PAPP-A<5th centile; LR+ 2.10 (1.57,2.81), LR- 0.95 (0.93,0.98).
Forest Plot showing likelihood ratio of a positive and negative test result with 95% confidence intervals (95% CI) for studies of pregnancy associated plasma protein A (PAPPA) to predict pre-eclampsia and small for gestational age (birth weight threshold as indicated). Results with diamonds are pooled results (number of studies as indicated), results with squares are single studies. The number of women included in the studies is shown. (a first trimester testing).
For SGA there were 10 included studies, 7 were performed in the first trimester, the commonest thresholds were PAPP-A < 5th centile (4 studies), PAPP-A<10th centile (5 studies) for birth weight < 10th centile. The most accurate predictor for birth weight < 10th centile was PAPP-A<1st centile; LR+ 3.50 (2.53,4.82), LR- 0.98 (0.97,0.99). For birth weight < 5th centile, the most accurate predictor was again PAPP-A<1st centile; LR+ 4.36 (3.27,5.80), LR- 0.97 (0.96,0.98).
Maternal serum inhibin A
The results for inhibin A are summarized in Figure 7. For PET there were 6 included studies, 1 performed in the first trimester, the commonest threshold being inhibin A>2.0MoM (2 studies) with a LR+ 6.00 (5.12,7.03), LR- 0.72 (0.48,1.09). The most accurate predictor for PET was inhibin A>2.79MoM; LR+ 19.52 (8.33,45.79), LR- 0.30 (0.13,0.68), however this result was derived from one study using a receiver operating characteristic curve to determine threshold.
Forest Plot showing likelihood ratio of a positive and negative test result with 95% confidence intervals (95% CI) for studies of Inhibin A to predict pre-eclampsia and small for gestational age (birth weight threshold as indicated). Results with diamonds are pooled results (number of studies as indicated), results with squares are single studies. The number of women included in the studies is shown. (a first trimester testing).
For SGA there was only one study, looking at second trimester testing, using a cut-off of inhibin A>2.0MoM, the results for prediction of birth weight < 10th centile were LR+ 4.45 (3.92,5.06), LR- 0.92 (0.91,0.93) and birth weight < 5th centile; LR+ 4.91 (4.20,5.73), LR- 0.89 (0.87,0.91).
Triple test (serum AFP, HCG and unconjugated estriol)
There were no included studies for PET. For SGA there were 2 studies, second trimester testing, with different cut-offs for prediction of birth weight < 10th centile: triple test > 1:190 LR+ 1.07 (0.60,1.91), LR- 0.98 (0.82,1.17) and triple test>1:250 LR+ 2.71 (1.77,4.17), LR- 1.19 (0.01,2.47).
Gestation of testing
Table 1 shows the different results achieved where testing was performed in both the first and second trimester. Overall for HCG, testing in the second trimester was more accurate.
Sub-group and sensitivity analysis
For sub group analysis, a sub-group had to include at least three studies within each analyte and threshold and thus was only possible for calculated incidence of disease. The results for sub-group analysis are shown in Table 2. There was no significant difference between the subgroups.
Most of the studies included in the review excluded fetuses with other structural or chromosomal anomalies from the results and included live births only thus subgroup analysis could not be performed in these areas. Sensitivity analysis including only those studies with these characteristics showed no significant difference. The same was true for the assessment of study quality i.e. most studies were of a similar quality to make sub-group analysis impossible but sensitivity analysis showed no difference when extremely low quality studies were excluded.
Forest plots of sensitivity and specificity are shown in Additional file 6. Summary receiver operating characteristic curves are available from the authors on request.
Clinical application with aspirin
The results for clinical application with aspirin for SGA are shown in Table 3 and for PET in Table 4. The results show that by testing with inhibin A for PET or SGA in a low risk population we can reduce the number of women needed to treat to prevent one case of SGA from 90 to 30 and for PET from 323 to 27, having to test 909 and 469 women respectively.
Discussion
We evaluated the accuracy of five serum screening markers used in Down's syndrome screening. The results showed low predictive accuracy overall. For PET the best predictor was inhibin A>2.79MoM. However, it is important to point out that this threshold was determined from a receiver operating characteristic curve and based on a single study. For SGA the best predictor overall for birth weight < 10th centile was AFP<10th centile while AFP>3.0MoM was the best predictor of birth weight < 5th centile. These results were both based on single studies. AFP and inhibin A showed improvements in predictive accuracy when looking at severe disease for SGA and PET respectively. HCG showed improved prediction when comparing second trimester to first trimester testing.
The strength of our review and validity of its findings lies in the methodological strengths used. We complied with existing guidelines for the reporting of systematic reviews [18] and also guidelines specific to the reporting of systematic reviews of observational studies [142]. We performed extensive literature searches without language restrictions. We paid careful attention to assessment of quality of study design and reporting (The Quorum statement for this review is shown in Additional file 7).
Previously published reviews in this area are restricted to a systematic review evaluating predictive tests for PET [143]. This review concluded that the tests investigated had a low predictive value, the methodology of this review has however been criticized [144] and was restricted in the thresholds and tests it reviewed. To our knowledge there are no previously reported systematic reviews in this area for SGA.
We have primarily reported likelihood ratios in this review as they are thought to be more clinically meaningful than sensitivities and specificities, the use of likelihood ratios allowing us to determine post test probabilities of disease based on Bayes' theorem. Recent research suggests that independently pooled likelihood ratios should be interpreted with caution as positive and negative likelihood ratios are related statistics (just like sensitivity and specificity) [145]. We also pooled sensitivity and specificity and found no difference in the interpretation of the results. Bivariate meta-analysis is a new statistical technique that explicitly incorporates the correlation between sensitivity and specificity in a single model [146], its use is however not yet widespread nor is it easily interpreted.
Our assessment of study quality was hindered by lack of clear reporting, which is a common problem in diagnostic reviews as standards for quality and checklists for assessing it are fairly new. It has been previously reported that poor study design and conduct can affect the estimates of diagnostic accuracy [28, 29] however, it is not entirely clear how individual aspects of quality may effect this and to what magnitude particularly in the area of Obstetrics. Application of quality scores has been shown to be of little value on diagnostic reviews [147] however, due to the lack of clear reporting it was not possible to perform sub-group analysis based on individual quality criteria.
One of the areas in which reporting was uniformly poor was in the details provided regarding performance of the reference standard. In PET definitions have changed over time with previous definitions including change increases in blood pressure. The measurement of blood pressure was poorly reported. It is important to record diastolic blood pressure with Korotkoff phase V as this is more reliably recorded and reflects true diastolic blood pressure [148–150]. For SGA there is still no convincing evidence as to which is the best definition of the condition at birth nor which is the best predictor of future infant and childhood morbidity and mortality for term infants. Population based birth weight standards were the most commonly used, however it is important to realize that these do not distinguish between the small healthy infant and the compromised infant. Customised growth charts that are adjusted for sex, gestation, parity, maternal weight and height and ethnicity, have been shown to improve the detection of infants at risk of stillbirth [151] while neonatal indices have been shown to identify the malnourished infant at risk of peripartum asphyxia [152]. Unfortunately these were rarely used as outcome measures in the included reviews.
Confounding factors in measurement of serum screening markers but mainly AFP is its association with intrauterine death, preterm labour and chromosomal and structural anomalies [54, 57, 60]. Ideally all the included papers in this review should have included only women with live births and fetuses with no other chromosomal or structural anomalies, this however was not always clearly reported. Sensitivity analysis, including only studies that did report exclusion of these subjects showed no significant difference in estimates of test accuracy.
In this review we have also assumed that the markers act independently but this may not be the case. The relationship between PET and SGA must also be taken into account. For HCG measurement the risk of SGA has been shown by logistic regression to be dependent on the presence of PET [99]. Ideally included cases of SGA for this review would have been those where there was no PET but this was again poorly reported.
When assessing the clinical relevance of these tests it is important to look at severe disease as this causes the majority of maternal, fetal and neonatal complications and thus prediction and prevention of this form of disease would have the greatest health impact. For the studies included in the meta-analysis there were only three that had results for either severe PET or SGA and these were insufficient to make an accurate assessment of the prediction of this form of disease.
The calculations of NNTreat and NNTest show that we can reduce the number of women needed to treat with aspirin to prevent one case of SGA/PET if we first test with a serum screening marker and then only treat the test positives. As aspirin is not routinely used as a treatment these calculations serve to contextualize the predictive value of these markers as individual tests. The costs of introducing aspirin as a treatment would need to be balanced against the costs of the test, costs of failing to treat the women with a false negative result that then go on to develop disease and any patient costs in terms of anxiety from screening and over treatment in the false positive category. To thus calculate the true clinical effectiveness of these tests these results would need to be incorporated in to a full cost-effectiveness analysis.
As PET and SGA are diseases with relatively low prevalence a clinically useful test would need to have a high positive LR (> 10) and low negative LR (< 0.10) [153]. From the results of this review it is unlikely that any one serum screening marker in isolation will provide this. Future research should thus concentrate in two areas. The first should be to address the limitations within the primary literature as identified by this review; poor reporting, exclusion of intrauterine deaths and chromosomal and structural anomalies from the results, separation of PET and SGA, prediction of severe disease. This may not necessarily require further primary research as there are sufficient large, well designed cohort studies available but meta-analysis based on individual patient data. Secondly future research should focus on combinations of markers as predictors and combinations of tests such as serum screening markers and uterine artery Doppler [154] to improve the predictive accuracy to a clinically useful value.
As Down's serum screening is routinely performed in many developed countries the cost of implementing use of these results as a predictive test for PET and SGA would be small. However as aspirin is the only preventative treatment with any proven benefit in these conditions and has minimal adverse events this cost has to be compared to that of implementing aspirin treatment to all pregnant women.
Conclusion
Down's serum screening analytes have low predictive accuracy for pre-eclampsia and small for gestational age. They may be a useful means of risk assessment or of use in prediction when combined with other tests.
References
Hay WW, Catz CS, Grave GD, Yaffe SJ: Workshop summary: fetal growth: its regulation and disorders. Pediatrics. 1997, 99 (6): 585-591.
McIntire DJ, Bloom SL, Casey BM, Levenko KJ: Birth weight in relation to morbidity and mortality among newborn infants. N Eng J Med. 1999, 340 (16): 1234-1238. 10.1056/NEJM199904223401603.
Taylor DJ, Howie PW: Fetal growth achievement and neurodevelopmental disability. Br J Obstet Gynaecol. 1989, 96 (7): 789-794.
Rich-Edwards J, Colditz G, Stampfer M, Willett W, Gillman M, Hennekens C: Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann Intern Med. 1999, 130 (4 Pt 1): 278-284.
Barker DJ: The developmental origins of chromic adult disease. Acta Paediatr Suppl. 2004, 93 (446): 26-33.
Wapner R, Thom E, Simpson JL, Pergament E, Silver R, Filkins K: First trimester screening for trisomies 21 and 18. N Eng J Med. 2003, 349 (15): 1405-1413. 10.1056/NEJMoa025273.
Yaron Y, Cherry M, Kramer RL, O'Brien JE, Hallak M, Johnson MP, Evans MI: Second-trimester maternal serum marker screening: maternal serum alpha-fetoprotein, beta-human chorionic gonadotropin, estriol, and their various combinations as predictors of pregnancy outcome. Am J Obstet Gynecol. 1999, 181 (4): 968-974. 10.1016/S0002-9378(99)70334-0.
Aquilina J, Maplethorpe R, Ellis P, Harrington K: Correlation between second trimester maternal serum inhibin-A and human chorionic gonadotrophin for the prediction of pre-eclampsia. Placenta. 2000, 21 (5–6): 487-492. 10.1053/plac.2000.0540.
Ong CY, Liao AW, Spencer K, Munim S, Nicolaides KH: First trimester maternal serum free beta human chorionic gonadotrophin and pregnancy associated plasma protein A as predictors of pregnancy complications. BJOG. 2000, 107 (10): 1265-1270. 10.1111/j.1471-0528.2000.tb11618.x.
Morssink LP, Kornman LH, Hallahan TW, Kloosterman MD, Beckhuis JR, De Wolf BT, Montingh A: Maternal serum levels of free beta-hCG and PAPP-A in the first trimester of pregnancy are not associated with subsequent fetal growth retardation or preterm delivery. Prenat Diagn. 1998, 18 (2): 147-152. 10.1002/(SICI)1097-0223(199802)18:2<147::AID-PD231>3.0.CO;2-W.
Askie L, Duley L, Henderson-Smart D, Stewart L: Antiplatelet agents for preventing pre-eclampsia: a meta-analysis of individual patient data. Lancet. 2007, 369 (9575): 1791-1798. 10.1016/S0140-6736(07)60712-0.
Coomarasamy A, Frisk NM, Gee H, Robson SC: The Investigation and Management of the Small for Gestational Age Fetus. Guideline No 31 Nov 2002. 2003, RCOG, London
Cnossen JS, Post van der JAM, Mol BW, Khan KS, Meads C, der Riet G: Prediction of pre-eclampsia: a protocol for systematic reviews of test accuracy. BMC Pregnancy and Childbirth. 2006, 6: 29-10.1186/1471-2393-6-29.
Morris RK, Khan K, Coomarasamy A, Robson S, Kleijnen J: The value of prediciting fetal growth restriction and compromise of its wellbeing: Systematic quantitative overviews (meta-analysis) of test accuracy literature. BMC Pregnancy and Childbirth. 2007, 7: 3-10.1186/1471-2393-7-3.
Cochrane Methods Working Group on Systematic Reviews of Screening and Diagnostic Tests: Recommended methods. 1996
Deeks J: Systematic reviews in health care: systematic reviews of diagnostic and screening tests. BMJ. 2001, 323 (7305): 157-162. 10.1136/bmj.323.7305.157.
Irwig L, Tosteson AN, Gatsonis C, Low J, Colditz G, Chalmers TC, Mosteller F: Guidelines for meta-analyses evaluating diagnostic tests. Ann Intern Med. 1994, 120 (8): 667-676.
Khan KS, Dinnes J, Kleijnen J: Systematic reviews to evaluate diagnostic tests. Eur J Obstet Gynecol Reprod Biol. 2001, 95 (1): 6-11. 10.1016/S0301-2115(00)00463-2.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM: The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001, 20 (1): IX-XIV. 10.1081/PRG-100104165.
McCowan LM, Harding JE, Stewart AW: Customized birthweight centiles predict SGA pregnancies with perinatal morbidity. BJOG. 2005, 112 (8): 1026-1033.
Owen P, Farrell T, Hardwick JC, Khan KS: Relationship between customised birthweight centiles and neonatal anthropometric features of growth restriction. BJOG. 2002, 109 (6): 658-662. 10.1111/j.1471-0528.2002.01367.x.
Fay RA, Dey PL, Saadie CM, Buhl JA, Gebski VJ: Ponderal index: a better definition of the 'at risk' group with intrauterine growth problems than birth-weight for gestational age in term infants. Aust N Z J Obstet Gynaecol. 1991, 31 (1): 17-19. 10.1111/j.1479-828X.1991.tb02755.x.
Tamim H, Beydoun H, Itani M, Khogali M, Chokr I, Yunis KA, The National Collaborative Perinatal Neonatal Network: Predicting neonatal outcomes: birthweight, body mass index or ponderal index?. J Perinat Med. 2004, 32 (6): 509-513. 10.1515/JPM.2004.120.
Excler J, Sann L, Lasne Y, Picard J: Anthropometric assessment of nutritional status in newborn infants. Discriminative value of mid arm circumference and of skinfold thickness. Early Hum Dev. 1985, 11 (2): 169-178. 10.1016/0378-3782(85)90104-5.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J: The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003, 3: 25-10.1186/1471-2288-3-25.
Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J: Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol. 2006, 6: 9-10.1186/1471-2288-6-9.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Orwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC, the STARD Group: Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ. 2003, 326 (7379): 41-44. 10.1136/bmj.326.7379.41.
Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, Meulen van der JH, Bossuyt PM: Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999, 282 (11): 1061-1066. 10.1001/jama.282.11.1061.
Rutjes AW, Reitsma J, Di N, Smidt N, van Rijn J, Bossuyt PM: Evidence of bias and variation in diagnostic accuracy studies. CMAJ. 2006, 174 (4): 469-476.
Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J: Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess. 2004, 8 (25): iii, 1-234.
Honest H, Khan KS: Reporting of measures of accuracy in systematic reviews of diagnostic literature. BMC Health Serv Resh. 2002, 2 (1): 4-10.1186/1472-6963-2-4.
Jaeschke R, Guyatt GH, Sackett DL: Users' guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994, 271 (9): 703-707. 10.1001/jama.271.9.703.
Khan K, Chien PF: Seizure prophylaxis in hypertensive pregnancies: a framework for making clinical decisions. Br J Obstet Gynaecol. 1997, 104 (10): 1173-1179.
Gulmezoglu M, de OM, Villar J: Effectiveness of interventions to prevent or treat impaired fetal growth. Obstet Gynecol Surv. 1997, 52 (2): 139-149. 10.1097/00006254-199702000-00023.
Florio P, Reis FM, Pezzani I, Luisi S, Severi FM, Petraglia F: The addition of activin A and inhibin A measurement to uterine artery Doppler velocimetry to improve the early prediction of pre-eclampsia. Ultrasound Obstet Gynecol. 2003, 21 (2): 165-169. 10.1002/uog.29.
Zeeman GG, Alexander JM, McIntire DD, Byrd W, Leveno KJ: Inhibin-A and superimposed preeclampsia in women with chronic hypertension. Obstet Gynecol. 2003, 101 (2): 232-236. 10.1016/S0029-7844(02)02640-6.
Yaron Y, Ochshorn Y, Heifetz S, Lehavi O, Sapir Y, Orr-Urtreger A: First trimester maternal serum free human chorionic gonadotropin as a predictor of adverse pregnancy outcome. Fetal Diagn Ther. 2002, 17 (6): 352-356. 10.1159/000065384.
Yaron Y, Heifetz S, Ochshorn Y, Lehavi O, Orr-Urtreger A: Decreased first trimester PAPP-A is a predictor of adverse pregnancy outcome. Prenat Diagn. 2002, 22 (9): 778-782. 10.1002/pd.407.
Smith GC, Stenhouse EJ, Crossley JA, Aitken DA, Cameron AD, Connor JM: Early pregnancy levels of pregnancy-associated plasma protein a and the risk of intrauterine growth restriction, premature birth, preeclampsia, and stillbirth. J Clin Endocrinol Metab. 2002, 8 ((4)7): 1762-1767. 10.1210/jc.87.4.1762.
Aquilina J, Thompson O, Thilaganathan B, Harrington K: Improved early prediction of pre-eclampsia by combining second-trimester maternal serum inhibin-A and uterine artery Doppler. Ultrasound Obstet Gynecol. 2001, 17 (16): 477-484. 10.1046/j.1469-0705.2001.00382.x.
Lee LC, Sheu BC, Shau WY, Liu DM, Lai TJ, Lee YH, Huang SC: Mid-trimester beta-hCG levels incorporated in a multifactorial model for the prediction of severe pre-eclampsia. Prenat Diagn. 2000, 20 (9): 738-743. 10.1002/1097-0223(200009)20:9<738::AID-PD917>3.0.CO;2-R.
Leung TN, Chung TK, Madsen G, Lam CWK, Lam PKW, Walters WAW, Smith R: Analysis of mid-trimester corticotrophin-releasing hormone and alpha-fetoprotein concentrations for predicting pre-eclampsia. Hum Reprod. 2000, 15 (8): 1813-1818. 10.1093/humrep/15.8.1813.
Muttukrishna S, North RA, Morris J, Schellenberg JC, Taylor RS, Asselin J, Ledger W, Groome N, Redman CWG: Serum inhibin A and activin A are elevated prior to the onset of pre-eclampsia. Hum Reprod. 2000, 15 (7): 1640-1645. 10.1093/humrep/15.7.1640.
Lambert-Messerlian GM, Silver HM, Petraglia F, Luisi S, Pelzani I, Maybruck WM, Hogge WA, Hanley-Yanez K, Roberts JM: Second-trimester levels of maternal serum human chorionic gonadotropin and inhibin a as predictors of preeclampsia in the third trimester of pregnancy. J Soc Gynecol Investig. 2000, 7 (3): 170-174. 10.1016/S1071-5576(00)00050-2.
Sebire NJ, Roberts L, Noble P, Wallace E, Nicolaides KH: Raised maternal serum inhibin A concentration at 10 to 14 weeks of gestation is associated with pre-eclampsia. BJOG. 2000, 107 (6): 795-797. 10.1111/j.1471-0528.2000.tb13343.x.
Stamilio DM, Sehdev HM, Morgan MA, Propert K, Macones GA: Can antenatal clinical and biochemical markers predict the development of severe preeclampsia?. Am J Obstet Gynecol. 2000, 182 (3): 589-594. 10.1067/mob.2000.103890.
Haddad B, Abirached F, Louis-Sylvestre C, Le Blond J, Paniel BJ, Zorn JR: Predictive value of early human chorionic gonadotrophin serum profiles for fetal growth retardation. Hum Reprod. 1999, 14 (11): 2872-2875. 10.1093/humrep/14.11.2872.
Raty R, Koskinen P, Alanen A, Irjala K, Matinlauri I, Ekblad U: Prediction of pre-eclampsia with maternal mid-trimester total renin, inhibin A, AFP and free beta-hCG levels. Prenat Diagn. 1999, 19 (2): 122-127. 10.1002/(SICI)1097-0223(199902)19:2<122::AID-PD491>3.0.CO;2-R.
Pouta AM, Hartikainen AL, Vuolteenaho OJ, Ruokonen AO, Laatikainen TJ: Midtrimester N-terminal proatrial natriuretic peptide, free beta hCG, and alpha-fetoprotein in predicting preeclampsia. Obstet Gynecol. 1998, 91 (6): 940-944. 10.1016/S0029-7844(98)00112-4.
Luckas M, Hawe J, Meekins J, Neilson J, Walkinshaw S: Second trimester serum free beta human chorionic gonadotrophin levels as a predictor of pre-eclampsia. Acta Obstet Gynecol Scand. 1998, 77 (4): 381-384. 10.1034/j.1600-0412.1998.770404.x.
Onderoglu LS, Kabukcu A: Elevated second trimester human chorionic gonadotropin level associated with adverse pregnancy outcome. Int J Gynaecol Obstet. 1997, 56 (3): 245-249. 10.1016/S0020-7292(96)02830-5.
Ashour AM, Lieberman ES, Haug LE, Repke JT: The value of elevated second-trimester beta-human chorionic gonadotropin in predicting development of preeclampsia. Am J Obstet Gynecol. 1997, 176 (2): 438-442. 10.1016/S0002-9378(97)70512-X.
Jauniaux E, Gulbis B, Tunkel S, Ramsay B, Campbell S, Meuris S: Maternal serum testing for alpha-fetoprotein and human chorionic gonadotropin in high-risk pregnancies. Prenat Diagn. 1996, 16 (12): 1129-1135. 10.1002/(SICI)1097-0223(199612)16:12<1129::AID-PD9>3.0.CO;2-I.
Waller DK, Lustig LS, Cunningham GC, Feuchtbaum LB, Hook EB: The association between maternal serum alpha-fetoprotein and preterm birth, small for gestational age infants, preeclampsia, and placental complications. Obstet Gynecol. 1996, 88 (5): 816-822. 10.1016/0029-7844(96)00310-9.
Heinonen S, Ryynanen M, Kirkinen P, Saarikoski S: Elevated midtrimester maternal serum hCG in chromosomally normal pregnancies is associated with preeclampsia and velamentous umbilical cord insertion. Am J Perinatol. 1996, 13 (7): 437-441.
Muller F, Savey L, Le Fiblec B, Bussieres L, Ndayizamba G, Colau JC, Giraudet P: Maternal serum human chorionic gonadotropin level at fifteen weeks is a predictor for preeclampsia. Am J Obstet Gynecol. 1996, 175 (1): 37-40. 10.1016/S0002-9378(96)70247-8.
Wenstrom KD, Owen J, Davis RO, Brumfield CG: Prognostic significance of unexplained elevated amniotic fluid alpha-fetoprotein. Obstet Gynecol. 1996, 87 (2): 213-216. 10.1016/0029-7844(95)00377-0.
Vaillant P, David E, Constant I, Athmani B, Devulder G, Fievet P, Gondry J, Boulanger JC, Fardelone P, Fournier A: Validity in nulliparas of increased beta-human chorionic gonadotrophin at mid-term for predicting pregnancy-induced hypertension complicated with proteinuria and intrauterine growth retardation. Nephron. 1996, 72 (4): 557-563.
Simpson JL, Palomaki GE, Mercer B, Haddow JE, Andersen R, Sibai B, Elias S: Associations between adverse perinatal outcome and serially obtained second- and third-trimester maternal serum alpha-fetoprotein measurements. Am J Obstet Gynecol. 1995, 173 (6): 1742-1748. 10.1016/0002-9378(95)90420-4.
Milunsky A, Jick SS, Bruell CL, Maclaughlin DS, Tsung YK, Jick H, Rothman KJ, Willett W: Predictive values, relative risks, and overall benefits of high and low maternal serum alpha-fetoprotein screening in singleton pregnancies: new epidemiologic data. Am J Obstet Gynecol. 1989, 161 (2): 291-297.
Capeless EL, Kelleher PC, Walters CP: Elevated maternal serum alpha-fetoprotein levels and maternal risk factors: Their association with pregnancy complications. J Reprod Med. 1992, 37 (3): 257-260.
Morssink LP, Heringa MP, Beekhuis JR, De Wolf BT, Mantingh A: The association between hypertensive disorders of pregnancy and abnormal second-trimester maternal serum levels of hCG and alpha-fetoprotein. Obstet Gynecol. 1997, 89 (5 Pt 1): 666-670. 10.1016/S0029-7844(97)00088-4.
Roes EM, Gaytant MA, Thomas CM, Raijmakers MTM, Zusterzeel PLM, Peters WHM, Steegers EAP: First trimester inhibin-A concentrations and later development of preeclampsia. Acta Obstet Gynecol Scand. 2004, 83 (1): 117-10.1111/j.1600-0412.2004.00140.x.
Audibert F, Benchimol Y, Benattar C, Champagne C, Frydman R: Prediction of preeclampsia or intrauterine growth restriction by second trimester serum screening and uterine Doppler velocimetry. Fetal Diagn Ther. 2005, 20 (1): 48-53. 10.1159/000081369.
Brajenovic-Milic B, Tislaric D, Zuvic-Butorac M, Back J, Petrovic O, Ristic S, Mimica M, Kapovic M: Elevated second-trimester free beta-hCG as an isolated finding and pregnancy outcomes. Fetal Diagn Ther. 2004, 19 (6): 483-487. 10.1159/000080159.
Dugoff L, Hobbins JC, Malone FD, Porter TF, Luthy D, Comstock CH, Hankins G, Berkowitz RL, Merkatz I, Craigo SD, Timor-Tritsch IE, Carr SR, Wolfe HM, Vidavar J, D'Alton ME: First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: a population-based screening study (the FASTER Trial). Am J Obstet Gynecol. 2004, 191 (4): 1446-1451. 10.1016/j.ajog.2004.06.052.
Dugoff L, Hobbins JC, Malone FD, Vidaver J, Sullivan L, Canick JA, Lambert-Messerlian GM, Porter TF, Luthy DA, Comstock CH, Saade G, Eddleman K, Merkatz IR, Craigo SD, Timor-Tritsch IE, Carr SR, Wolfe HM, D'Alton ME, FASTER Trial Research Consortium: Quad screen as a predictor of adverse pregnancy outcome. Obstet Gynecol. 2005, 106 (2): 260-267.
Ay E, Kavak ZN, Elter K, Gokaslan H, Pekin T: Screening for pre-eclampsia by using maternal serum inhibin A, activin A, human chorionic gonadotropin, unconjugated estriol, and alpha-fetoprotein levels and uterine artery Doppler in the second trimester of pregnancy. Aust N Z J Obstet Gynaecol. 2005, 45 (4): 283-288. 10.1111/j.1479-828X.2005.00412.x.
Hershkovitz R, De SM, Kingdom J: Mid-trimester placentation assessment in high-risk pregnancies using maternal serum screening and uterine artery Doppler. Hypertens Pregnancy. 2005, 24 (3): 273-280. 10.1080/10641950500280995.
Roiz-Hernandez J, de JC-M, Fernandez-Mejia M: Human chorionic gonadotropin levels between 16 and 21 weeks of pregnancy and prediction of pre-eclampsia. Int J Gynaecol Obstet. 2006, 92 (2): 101-105. 10.1016/j.ijgo.2005.10.002.
Spencer K, Yu CK, Cowans NJ, Otigbah C, Nicolaides KH: Prediction of pregnancy complications by first-trimester maternal serum PAPP-A and free beta-hCG and with second-trimester uterine artery Doppler. Prenat Diagn. 2005, 25 (10): 949-953. 10.1002/pd.1251.
Spencer K, Yu CK, Savvidou M, Papageorghiou AT, Nicolaides KH: Prediction of pre-eclampsia by uterine artery Doppler ultrasonography and maternal serum pregnancy-associated plasma protein-A, free beta-human chorionic gonadotropin, activin A and inhibin A at 22 + 0 to 24 + 6 weeks' gestation. Ultrasound Obstet Gynecol. 2006, 27 (6): 559-564. 10.1002/uog.2676.
Wald NJ, Morris JK, Ibison J, Wu T, George LM: Screening in early pregnancy for pre-eclampsia using Down syndrome quadruple test markers. Prenat Diagn. 2006, 26 (6): 559-564. 10.1002/pd.1459.
Pilalis A, Souka AP, Antsaklis P, Daskalakis G, Papantoniou N, Mesogitis S, Antsaklis A: Screening for pre-eclampsia and fetal growth restriction by uterine artery Doppler and PAPP-A at 11–14 weeks' gestation. Ultrasound Obstet Gynecol. 2007, 29 (2): 135-140. 10.1002/uog.3881.
Kowalczyk TD, Cabaniss ML, Cusmano L: Association of low unconjugated estriol in the second trimester and adverse pregnancy outcome. Obstet Gynecol. 1998, 91 (3): 396-400. 10.1016/S0029-7844(97)00677-7.
Akinbiyi AA: Unexplained elevated maternal serum alpha-fetoprotein in singleton pregnancies as a predictor of fetal risk. Int J Gynaecol Obstet. 1996, 53 (1): 17-21. 10.1016/0020-7292(95)02633-9.
Benn PA, Horne D, Briganti S, Rodis JF, Clive JM: Elevated second-trimester maternal serum hCG alone or in combination with elevated alpha-fetoprotein. Obstet Gynecol. 1996, 87 (2): 217-222. 10.1016/0029-7844(95)00390-8.
Bernstein IM, Barth RA, Miller R, Capeless EL: Elevated maternal serum alpha-fetoprotein: association with placental sonolucencies, fetomaternal hemorrhage, vaginal bleeding, and pregnancy outcome in the absence of fetal anomalies. Obstet Gynecol. 1992, 79 (1): 71-74.
Bewley S, Chard T, Grudzinskas G, Cooper D, Campbell S: Early prediction of uteroplacental complications of pregnancy using Doppler ultrasound, placental function tests and combination testing. Ultrasound Obstet Gynecol. 1992, 2 (5): 333-337. 10.1046/j.1469-0705.1992.02050333.x.
Bloxam DL, Williams NR, Waskett RJ, Stewart SG: Disturbed zinc metabolism and reduced birthweight related to raised maternal serum alpha-fetoprotein in normal human pregnancies. [Review] [49 refs]. Acta Obstet Gynecol Scand. 1994, 73 (10): 758-764. 10.3109/00016349409072500.
Brazerol WF, Grover S, Donnenfeld AE: Unexplained elevated maternal serum alpha-fetoprotein levels and perinatal outcome in an urban clinic population. Am J Obstet Gynecol. 1994, 171 (4): 1030-1035.
Bremme K, Eneroth P, Nilsson B, Marsk L, Hagenfeldt L: Outcome of pregnancy in relation to maternal serum alpha-fetoprotein levels in the second trimester. An evaluation of a screening program and a longitudinal follow-up. Gynecol Obstet Invest. 1988, 26 (3): 191-205.
Brock DJ, Barron L, Raab GM: The potential of mid-trimester maternal plasma alpha-fetoprotein measurement in predicting infants of low birth weight. Br J Obstet Gynaecol. 1980, 87 (7): 582-585.
Buckland CM, Thom H, Campbell AG: Maternal serum alpha-fetoprotein levels in low birth weight singleton pregnancies. J Perinat Med. 1984, 12 (3): 127-132.
Burton BK: Outcome of pregnancy in patients with unexplained elevated or low levels of maternal serum alpha-fetoprotein. Obstetrics & Gynecology. 1988, 72 (5): 709-713.
Chapman SJ, Brumfield CG, Wenstrom KD, Dubard MB: Pregnancy outcomes following false-positive multiple marker screening tests. Am J Perinatol. 1997, 14 (8): 475-478.
Chard T, Rice A, Kitau MJ, Hird V, Grudzinskas JG, Nysenbaum AM: Mid-trimester levels of alphafetoprotein in the screening of low birthweight. Br J Obstet Gynaecol. 1986, 93 (1): 36-38.
Chitayat D, Farrell SA, Huang T, Meier C, Wyatt PR, Summers AM: Double-positive maternal serum screening results for down syndrome and open neural tube defects: An indicator for fetal structural or chromosomal abnormalities and adverse obstetric outcomes. Am J Obstet Gynecol. 2002, 187 (3): 758-763. 10.1067/mob.2002.125240.
Cho S, Durfee KK, Keel BA, Parks LH: Perinatal outcomes in a prospective matched pair study of pregnancy and unexplained elevated or low AFP screening. J Perinat Med. 1997, 25 (6): 476-483.
Cox MU, Kingdom J, Whittle M, McNay M, Fleming J, Bowman A, Crossley J, Aitken D: [Unexplained increase in maternal plasma in alpha-fetoproteins in the second trimester of pregnancy: perinatal results]. Rev Chil Obstet Ginecol. 1995, 60 (3): 174-180.
Cusick W, Rodis JF, Vintzileos AM, Albini SM, McMahon M, Campbell WA: Predicting pregnancy outcome from the degree of maternal serum alpha-fetoprotein elevation. J Reprod Med. 1996, 41 (5): 327-332.
Di MM, Piazzi G, Ferrari A, Lotzniker M, Gerola O, Spinillo A: A simultaneous evaluation of second trimester serum AFP, hCG and unconjugated oestriol as predictors of small for gestational age births. Italian Journal of Gynaecology & Obstetrics. 1998, 10 (4): 155-159.
Doran TA, Valentine GH, Wong PY, Wielgosz G, Benzie RJ, Soltan HC, Jenner MR, Morland PA, Montogomery RJ, Allen LC: Maternal serum alpha-fetoprotein screening: report of a Canadian pilot project. CMAJ. 1987, 137 (4): 285-293.
Dungan JS, Shulman LP, Phillips OP, Simpson JL, Meyer NL, Grevengood C, Elias S: Positive serum screening for fetal Down syndrome does not predict adverse pregnancy outcome in absence of fetal aneuploidy. J Soc Gynecol Investig. 1994, 1 (1): 55-58.
Duric K, Skrablin S, Lesin J, Kalafatic D, Kuvacic I, Suchanek E: Second trimester total human chorionic gonadotropin, alpha-fetoprotein and unconjugated estriol in predicting pregnancy complications other than fetal aneuploidy. Eur J Obstet Gynecol Reprod Biol. 2003, 110 (1): 12-15. 10.1016/S0301-2115(03)00081-2.
Endres LK, Krotz S, Grobman WA: Isolated low second-trimester maternal serum beta-human chorionic gonadotropin is not associated with adverse pregnancy outcome. Am J Obstet Gynecol. 2003, 189 (3): 755-757. 10.1067/S0002-9378(03)00655-0.
Evans J, Stokes IM: Outcome of pregnancies associated with raised serum and normal amniotic fluid alpha fetoprotein concentrations. Br Med J (Clin Res Ed). 1984, 288 (6429): 1494-
Ghosh A, Tang MH, Tai D, Nie G, Ma HK: Justification of maternal serum alphafetoprotein screening in a population with low incidence of neural tube defects. Prenat Diagn. 1986, 6 (2): 83-87. 10.1002/pd.1970060202.
Gonen R, Perez R, David M, Dar H, Merksamer R, Sharf M: The association between unexplained second-trimester maternal serum hCG elevation and pregnancy complications. Obstet Gynecol. 1992, 80 (1): 83-86.
Gordon YB, Lewis JD, Leighton M, Kitau MJ, Clarke PC, Chard T: Maternal serum alpha-fetoprotein levels as an index of fetal risk. Am J Obstet Gynecol. 1979, 133 (4): 422-424.
Haddow JE, Kloza EM, Smith DE, Knight GJ: Data from an alpha-fetoprotein pilot screening program in Maine. Obstet Gynecol. 1983, 62 (5): 556-60.
Haddow JE, Knight GJ, Kloza EM, Palomaki GE: Alpha-fetoprotein, vaginal bleeding and pregnancy risk. Br J Obstet Gynaecol. 1986, 93 (6): 589-593.
Haddow JE, Palomaki GE, Knight GJ: Can low birth weight after elevated maternal serum alpha-fetoprotein be explained by maternal weight?. Obstet Gynecol. 1987, 70 (1): 26-28.
Hamilton MP, Abdalla HI, Whitfield CR: Significance of raised maternal serum alpha-fetoprotein in singleton pregnancies with normally formed fetuses. Obstet Gynecol. 1985, 65 (4): 465-470.
Hayashi M, Kohzu H: [Clinical studies on maternal serum alpha-fetoprotein (MSAFP) of 532 cases – the median value, pregnancy outcomes and clinical evaluation]. Nippon Sanka Fujinka Gakkai Zasshi. 1992, 44 (10): 1211-1218.
Heikkila A, Makkonen N, Heinonen S, Kirkinen P: Elevated maternal serum hCG in the second trimester increases prematurity rate and need for neonatal intensive care in primiparous preeclamptic pregnancies. Hypertens Pregnancy. 2001, 20 (1): 99-106.
Heinonen S, Ryynanen M, Kirkinen P: The effects on fetal development of high alpha-fetoprotein and maternal smoking. Am J Public Health. 1999, 89 (4): 561-563.
Hershkovitz R, Erez O, Sheiner E, Landau D, Mankuta D, Mazor M: Elevated maternal mid-trimester chorionic gonadotropin > or = 4 MoM is associated with fetal cerebral blood flow redistribution. Acta Obstet Gynecol Scand. 2003, 8 ((1)2): 22-27. 10.1034/j.1600-0412.2003.820104.x.
Kavak ZN, Basgul A, Elter K, Uygur M, Gokaslan H: The efficacy of first-trimester PAPP-A and free betahCG levels for predicting adverse pregnancy outcome. J Perinat Med. 2006, 34 (2): 145-148. 10.1515/JPM.2006.026.
Kim SY, Kim SK, Lee JS, Kim IK, Lee K: The prediction of adverse pregnancy outcome using low unconjugated estriol in the second trimester of pregnancy without risk of Down's syndrome. Yonsei Med J. 2000, 41 (2): 226-229.
Kiran TS, Bethel J, Bhal PS: Correlation of abnormal second trimester maternal serum alpha-fetoprotein (MSAFP) levels and adverse pregnancy outcome. J Obstet Gynaecol. 2005, 25 (3): 253-256. 10.1080/01443610500060693.
Krantz D, Goetzl L, Simpson JL, Thom E, Zachery J, Hallahan TW, Silver R, Pergament E, Platt LD, Filkins K, Johnson A, Mahoney M, Hogge WA, Wilson RD, Mohide P, Hershey D, Wapner R, First Trimester Maternal Serum Biochemistry and Fetal Nuchal Translucency Screening (BUN) Study Group: Association of extreme first-trimester free human chorionic gonadotropin-beta, pregnancy-associated plasma protein A, and nuchal translucency with intrauterine growth restriction and other adverse pregnancy outcomes. Am J Obstet Gynecol. 2004, 191 (4): 1452-1458. 10.1016/j.ajog.2004.05.068.
Kuo PL, Lin CC, Lin YH, Guo HR: Placental sonolucency and pregnancy outcome in women with elevated second trimester serum alpha-fetoprotein levels. J Formos Med Assoc. 2003, 102 (5): 319-325.
Kwik M, Morris J: Association between first trimester maternal serum pregnancy associated plasma protein-A and adverse pregnancy outcome. Aust N Z J Obstet Gynaecol. 2003, 43 (6): 438-442. 10.1046/j.0004-8666.2003.00126.x.
Legge M, Duff GB, Pike L, Aickin DR: Second trimester maternal serum alpha-fetoprotein as an indicator of fetal risk. Aust N Z J Obstet Gynaecol. 1985, 25 (4): 266-268. 10.1111/j.1479-828X.1985.tb00741.x.
Lepage N, Chitayat D, Kingdom J, Huang T: Association between second-trimester isolated high maternal serum maternal serum human chorionic gonadotropin levels and obstetric complications in singleton and twin pregnancies. Am J Obstet Gynecol. 2003, 188 (5): 1354-1359. 10.1067/mob.2003.278.
Lieppman RE, Williams MA, Cheng EY, Resta R, Zingheim R, Hickok DE, Luthy DA: An association between elevated levels of human chorionic gonadotropin in the midtrimester and adverse pregnancy outcome. Am J Obstet Gynecol. 1993, 168 (6 Pt 1): 1852-1856.
Markestad T, Bergsjo P, Aakvaag A, Lie RT, Jacobsen G, Hoffman HJ, Bakketeig LS: Prediction of fetal growth based on maternal serum concentrations of human chorionic gonadotropin, human placental lactogen and estriol. Acta Obstet Gynecol Scand Suppl. 1997, 165: 50-55.
Milunsky A, Nebiolo L: Maternal serum triple analyte screening and adverse pregnancy outcome. Fetal Diagn Ther. 1996, 11 (4): 249-253.
Miyakoshi K, Tanaka M, Gabionza D, Ishimoto H, Miyazaki T, Yoshimura Y: Prediction of smallness for gestational age by maternal serum human chorionic gonadotropin levels and by uterine artery Doppler study. Fetal Diagn Ther. 2001, 16 (1): 42-46. 10.1159/000053879.
Morssink LP, Kornman LH, Beekhuis JR, De Wolf BT, Mantingh A: Abnormal levels of maternal serum human chorionic gonadotropin and alpha-fetoprotein in the second trimester: relation to fetal weight and preterm delivery. Prenat Diagn. 1995, 15 (11): 1041-1046. 10.1002/pd.1970151109.
Mwambingu FT: Association between unaccountably high maternal alpha feto-protein and increased fetal risk. Acta Obstet Gynecol Scand. 1985, 64 (3): 275-276.
Naylor CS, Porto M, Cohen B, Garite TJ: Pregnancy outcome in Hispanic patients with unexplained positive triple marker screening for Down syndrome. J Matern Fetal Med. 2001, 10 (1): 20-22. 10.1080/714052710.
Odibo AO, Sehdev HM, Stamilio DM, Macones GA: Evaluating the thresholds of abnormal second trimester multiple marker screening tests associated with intra-uterine growth restriction. Am J Perinatol. 2006, 23 (6): 363-7. 10.1055/s-2006-947724.
Ogle R, Jauniaux E, Pahal GS, Dell E, Sheldrake A, Rodeck C: Serum screening for Down syndrome and adverse pregnancy outcomes: a case-controlled study. Prenat Diagn. 2000, 20 (2): 96-99. 10.1002/(SICI)1097-0223(200002)20:2<96::AID-PD766>3.0.CO;2-#.
Pergament E, Stein AK, Fiddler M, Cho NH, Kupferminc MJ: Adverse pregnancy outcome after a false-positive screen for Down syndrome using multiple markers. Obstet Gynecol. 1995, 86 (2): 255-258. 10.1016/0029-7844(95)00108-4.
Roop AP, Boughman JA, Blitzer MG: Study of the relationship between elevated maternal serum alpha-fetoprotein and adverse pregnancy outcome. Maryland Medical Journal. 1991, 40 (9): 779-784.
Secher NJ, Eriksen PS, Hansen PK, Lenstrup C, Thisted J: High maternal serum alpha-fetoprotein and low birthweight. A study concerning possible correlation between maternal weight, smoking, and serum alpha-fetoprotein and subsequent birthweight and gestational age. Am J Perinatol. 1985, 2 (2): 78-81.
Smith GC, Shah I, Crossley JA, Aitken DA, Pell JP, Nelson SM, Cameron AD, Connor MJ, Dobbie R: Pregnancy-associated plasma protein A and alpha-fetoprotein and prediction of adverse perinatal outcome. Obstet Gynecol. 2006, 107 (1): 161-6.
Sritippayawan S, Vachirasrisoontra C: Adverse pregnancy outcomes after a false-positive second trimester serum screen for Down syndrome in Thai pregnant women. J Med Assoc Thai. 2005, 88 (4): 449-454.
Summers AM, Huang T, Meier C, Wyatt PR: The implications of a false positive second-trimester serum screen for Down syndrome. Obstet Gynecol. 2003, 101 (6): 1301-1306. 10.1016/S0029-7844(03)00235-7.
Tanaka M, Natori M, Ishimoto , Gohda N, Kiyokawa K, Yamauchi J, Miyazaki T, Kpbayashi T, Nozawa S: [Screening for adverse perinatal outcome by biomarkers in maternal serum; a comparison of elevated maternal serum alpha-fetoprotein versus human chorionic gonadotropin]. Nippon Sanka Fujinka Gakkai Zasshi. 1994, 46 (11): 1229-1233.
Towner D, Gandhi S, El KD: Obstetric outcomes in women with elevated maternal serum human chorionic gonadotropin. Am J Obstet Gynecol. 2006, 194 (6): 1676-81. 10.1016/j.ajog.2006.03.011.
Tul N, Pusenjak S, Osredkar J, Spencer K, Novak-Antolic Z: Predicting complications of pregnancy with first-trimester maternal serum free-betahCG, PAPP-A and inhibin-A. Prenat Diagn. 2003, 23 (12): 990-996. 10.1002/pd.735.
Wald N, Cuckle H, Stirrat GM, Bennett MJ, Turnbull AC: Maternal serum-alpha-fetoprotein and low birth-weight. Lancet. 1977, 2 (8032): 268-270. 10.1016/S0140-6736(77)90953-9.
Wald NJ, Cuckle HS, Boreham J, Turnbull AC: Maternal serum alpha-fetoprotein and birth weight. Br J Obstet Gynaecol. 1980, 87 (10): 860-863.
Weiner CP, Grant SS, Williamson RA: Relationship between second trimester maternal serum alpha-fetoprotein and umbilical artery Doppler velocimetry and their association with preterm delivery. Am J Perinatol. 1991, 8 (4): 263-268.
Wenstrom KD, Sipes SL, Williamson RA, Grant SS, Trawick DC, Estle LC: Prediction of pregnancy outcome with single versus serial maternal serum alpha-fetoprotein tests. Am J Obstet Gynecol. 1992, 167 (6): 1529-1533.
Westergaard JG, Teisner B, Hau J, Grudzinskas JG: Placental protein measurements in complicated pregnancies. I. Intrauterine growth retardation. Br J Obstet Gynaecol. 1984, 91 (12): 1216-1223.
Williams MA, Hickok DE, Zingheim RW, Luthy DA, Kimelman J, Nyberg DA, Mahon BS: Elevated maternal serum alpha-fetoprotein levels and midtrimester placental abnormalities in relation to subsequent adverse pregnancy outcomes. Am J Obstet Gynecol. 1992, 167 (4 Pt 1): 1032-1037.
Zarzour SJ, Gabert HA, Diket AL, St AM, Miller JM: Abnormal maternal serum alpha fetoprotein and pregnancy outcome. J Matern Fetal Med. 1998, 7 (6): 304-307. 10.1002/(SICI)1520-6661(199811/12)7:6<304::AID-MFM9>3.0.CO;2-4.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Beccker BJ, Sipe TA, Thacker SB: Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000, 283 (15): 2008-2012. 10.1001/jama.283.15.2008.
Conde-Agudelo A, Villar J, Lindheimer M: World health organization systematic review of screening tests for preeclampsia. Obstet Gynecol. 2004, 104 (6): 1367-1391.
Cnossen JC, Mol BW, Post van der JAM, Bossuyt PM, ter Riet G: World health organization systematic review of screening tests for pre-eclampsia. Obstet Gynecol. 2005, 105 (5 Pt 1): 1151-1152.
Zwinderman AH, Bossuyt PM: We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med. 2007.
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH: Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005, 58 (10): 982-990. 10.1016/j.jclinepi.2005.02.022.
Whiting P, Harbord R, Kleijnen J: No role for quality scores in systematic reviews of diagnostic accuracy studies. BMC Med Res Methodol. 2005, 5: 19-10.1186/1471-2288-5-19.
Brown MA, Hague WM, Higgins J, Lowe S, McCowan L, Oats J, Peek MJ, Rowan JA, Walters NJ: The detection, investigation and management of hypertension in pregnancy: full consensus statement. Aust N Z J Obstet Gynaecol. 2000, 40 (2): 139-155. 10.1111/j.1479-828X.2000.tb01137.x.
Shennan A, Gupta M, Halligan A, Taylor DJ, de Swiet M: Lack of reproducibility in pregnancy of Korotkoff phase IV as measured by mercury sphygmomanometry. Lancet. 1996, 347 (8995): 139-142. 10.1016/S0140-6736(96)90338-4.
Brown MA, Reiter L, Smith B, Buddle ML, Morris R, Whitworth JA: Measuring blood pressure in pregnant women: A comparison of direct and indirect methods. Am J Obstet Gynecol. 1994, 171 (3): 661-667.
Clausson B, Gardosi J, Francis A, Cnattingius S: Perinatal outcome in SGA births defined by customised versus population based birthweight standards. BJOG. 2001, 108 (8): 830-834. 10.1016/S0306-5456(00)00205-9.
Scott K, Usher R: Fetal malnutrition: its incidence, causes and effects. Am J Obstet Gynecol. 1986, 94 (7): 951-963.
Deeks J, Altman D: Diagnostic tests: Likelihood ratios. BMJ. 2004, 329 (7458): 168-169. 10.1136/bmj.329.7458.168.
Konchak PS, Bernstein IM, Capeless EL: Uterine artery Doppler velocimetry in the detection of adverse obstetric outcomes in women with unexplained elevated maternal serum alpha-fetoprotein levels. Am J Obstet Gynecol. 1995, 173 (4): 1115-1119. 10.1016/0002-9378(95)91336-X.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2393/8/33/prepub
Acknowledgements
Faridi van Etten, Amsterdam Medical Center for help with searches. This study was supported by two project grants from Wellbeing of Women (NBTF626\03) and NHS Health Technology Assessment UK (01/64). The funding sources had no role in the collection, analysis, or interpretation of the data or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
The following authors were responsible for the study concept and design: RKM, JSC, GtR, BWM, JAMvdP, JK, KSK, SCR. The following authors were responsible for acquisition of data: RKM, JSC, ML, BWM.
Analysis and interpretation of data was performed by the following authors: RKM, JSC, KSK. Drafting of the manuscript was performed by: RKM, JSC, ML, GtR, BWM, JAMvdP, KSK, JK, SCR. Statistical analysis was performed by: RKM, JSC, KSK. All authors read and approved the final manuscript.
RKM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Electronic supplementary material
12884_2008_177_MOESM1_ESM.pdf
Additional file 1: "Prediction of pre-eclampsia: a protocol for systematic reviews of test accuracy." Study protocol for pre-eclampsia systematic reviews. (PDF 297 KB)
12884_2008_177_MOESM2_ESM.pdf
Additional file 2: "The value of predicting restriction of fetal growth and compromise of its wellbeing: Systematic quantitative overviews (meta-analysis) of test accuracy literature." Study protocol for fetal growth restriction systematic reviews. (PDF 264 KB)
12884_2008_177_MOESM3_ESM.doc
Additional file 3: "Search strategies for biochemical markers used in Down's serum screening to predict preeclampsia/small for gestational age." Electronic search strategies for systematic reviews. (DOC 64 KB)
12884_2008_177_MOESM4_ESM.doc
Additional file 4: "Guide to QUADAS for Down's syndrome markers to predict pre-eclampsia/small for gestational age." Guide to quality assessment of included papers in review using QUADAS tool. (DOC 42 KB)
12884_2008_177_MOESM5_ESM.doc
Additional file 5: "Study characteristics of studies of included studies for maternal serum biochemical (Down syndrome) screening to predict pre-eclampsia and small for gestational age." (DOC 250 KB)
12884_2008_177_MOESM6_ESM.doc
Additional file 6: "Forest plots of sensitivity and specificity." Results of sensitivity and specificity displayed as Forest plots. (DOC 645 KB)
12884_2008_177_MOESM7_ESM.bmp
Additional file 7: "Improving the quality of reports of meta-analyses of randomised controlled trials: the Quorum Statement checklist." The Quorum statement checklist. (BMP 963 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Morris, R.K., Cnossen, J.S., Langejans, M. et al. Serum screening with Down's syndrome markers to predict pre-eclampsia and small for gestational age: Systematic review and meta-analysis. BMC Pregnancy Childbirth 8, 33 (2008). https://doi.org/10.1186/1471-2393-8-33
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2393-8-33