Abstract
Background
Recent studies have shown that older mothers who deliver at preterm gestation have lower neonatal mortality rates compared with younger mothers who deliver at preterm gestation. We examined the effect of maternal age on gestational age-specific perinatal mortality.
Methods
We compared fetal, neonatal and perinatal mortality rates among singleton births in the United States, 2003–2005, to mothers aged ≥35 versus 20–29 years. The analysis was stratified by gestational age and perinatal mortality rates were contrasted by maternal age at earlier (22–33 weeks) and later gestation (≥34 weeks). Gestational age-specific perinatal mortality rates were calculated using the traditional perinatal formulation (deaths among births at any gestation divided by total births at that gestation) and also the fetuses-at-risk model (deaths among births at any gestation divided by fetuses-at-risk of death at that gestation).
Logistic regression was used to estimate adjusted odds ratios (AOR) for perinatal death.
Results
Under the traditional approach, fetal death rates at 22–33 weeks were non-significantly lower among older mothers (AOR 0.97, 95% confidence interval [CI] 0.91-1.03), while rates were significantly higher among older mothers at ≥34 weeks (AOR 1.66, 95% CI 1.56-1.76). Neonatal death rates were significantly lower among older compared with younger mothers at 22–33 weeks (AOR=0.93, 95% CI 0.88-0.98) but higher at ≥34 weeks (AOR 1.26, 95% CI 1.21-1.31). Under the fetuses-at-risk model, both rates were higher among older vs younger mothers at early gestation (AOR for fetal and neonatal mortality 1.35, 95% CI 1.27-1.43 and 1.31, 95% CI 1.24-1.38, respectively) and late gestation (AOR for fetal and neonatal mortality 1.66, 95% CI 1.56-1.76) and 1.21, 95% CI 1.14-1.29, respectively).
Conclusions
Although the traditional prognostic perspective on the risk of perinatal death among older versus younger mothers varies by gestational age at birth, the causal fetuses-at-risk model reveals a consistently elevated risk of perinatal death at all gestational ages among older mothers.
Similar content being viewed by others
Background
The trend towards delayed childbearing has accelerated in industrialized countries during recent decades. In Canada, the mean maternal age at childbirth increased substantially in four decades from 23.7 years in 1969 to 29.4 years in 2009 [1, 2]. More recently, the proportion of live births to women age 35 years or older in Canada doubled from 9.2% in 1991 to 18.3% in 2009 [1, 2]. Similar changes were observed in the United States, where the average maternal age increased from 25.0 to 27.5 years between 1980 and 2009 [3, 4], and the proportion of live births to mothers 35 years old or older increased from 4.9% in 1980 to 14.2% in 2009 [3, 4]. Childbearing in industrialized countries in Europe, Australia and New Zealand followed the same trend [5–7].
While the trend towards delayed childbearing continues, the effect of maternal age on birth outcomes remains a subject of some controversy. Most studies have demonstrated an increased risk for preterm birth, intrauterine growth restriction, fetal death and neonatal death among singletons born to older mothers [8–10]. However, recent studies have suggested a favourable effect of advanced maternal age on neonatal death and serious neonatal morbidity among infants born at early gestation or low birth weight [11, 12].
Our objective was to resolve the conflicting findings regarding the effect of advanced maternal age on fetal, neonatal and perinatal mortality at early gestation. We, therefore, carried out a study comparing gestational age-specific rates of fetal, neonatal and perinatal death among singleton infants born to mothers aged 20–29 years versus those born to mothers aged ≥35 years.
Methods
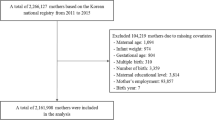
We used population-based data on singleton births in the United States from the National Centre for Health Statistics (NCHS). Information in the NCHS birth/infant death and fetal death files was abstracted from birth certificates [13], with the birth-infant death linkage carried out by the NCHS (cohort linked birth-infant death file). The most recently available cohort files for the years 2003 to 2005 that linked infant deaths (up to 1 year of age) to birth certificates were used for the study. We included all infants born between 22 and 43 weeks of gestation, based on the clinical estimate of gestation at birth as this estimate is more accurate than gestational age based on menstrual dates [14–17]. This estimate of gestational age was provided by the health care provider, without specification of the source (i.e., whether based on clinical examination, ultrasound, etc.).
States that did not report the clinical estimate of gestational age were not included in the analysis. We also excluded births weighing less than 500 grams birth weight in order to avoid potential bias due to variable birth registration at the borderline of viability [18]. Information about maternal age and maternal and infant risk factors including education, race, parity, marital status, and infant’s gender was also obtained from NCHS files. Young mothers were defined as those aged 20–29 years at the time of birth, while older mothers were those aged 35 years or more. Fetal death was defined as death occurring before delivery, and neonatal death was defined as death during the first 28 days after birth. Perinatal death included both fetal and neonatal death (obstetric definition of perinatal death) [19].
Gestational age-specific fetal, neonatal, and perinatal rates were calculated using two different approaches: the traditional method and the fetuses-at-risk approach. Under the traditional method of calculating gestational age-specific fetal, neonatal and perinatal mortality, mortality rates were obtained by dividing the number of deaths at any gestation by the number of total births (or live births) at that gestation. Under the fetuses-at-risk approach, gestational age-specific mortality rates were calculated as the number of deaths at any gestation divided by the number of fetuses at risk of death at that gestation. Thus all fetuses in utero who were at risk of stillbirth were included in the denominator for gestational age-specific stillbirth rates [20, 21]. Similarly, fetuses in utero who were at risk of birth and neonatal death at that gestation were included in the denominator for gestational age-specific neonatal death rates [21].
Logistic regression was used to estimate odds ratios and 95% confidence intervals and to adjust for confounders including maternal education (some college education vs high school or less), marital status (unmarried vs married), parity (nulliparous vs multiparous women, based on the total number of previous births), race (non-Hispanic white vs African American, Hispanic and other), smoking during pregnancy, infant’s gender and congenital anomalies (yes/no). To contrast the effects of maternal age on perinatal outcomes at early versus later gestation, two separate models were constructed for births at early (22–33 weeks) and late gestation (34–43 weeks). Under the traditional approach, logistic regression models for early gestation fetal, neonatal or perinatal death included only live births and fetal deaths at 22–33 weeks. In contrast, under the fetuses-at-risk approach, all ongoing pregnancies at 22 weeks gestation (i.e. all births at ≥22 weeks) were included in the logistic regression models examining death at early gestation. In this early gestation model, the outcome included fetal death, neonatal death or perinatal death at 22–33 weeks gestation only. Fetal and neonatal deaths and all live births that occurred after 33 weeks gestation were treated as survivors in this early gestation model and censored at 33 weeks. Logistic regression models examining fetal, neonatal and perinatal death at later gestation (≥34 weeks) included all ongoing pregnancies at 34 weeks gestation. The numerator and denominators were identical under the traditional and fetuses-at-risk approach in this analysis, as the total number of births at ≥34 weeks represented the number ongoing pregnancies at 34 weeks gestation. The only difference between the two approaches was for neonatal death; only live births were included in the denominator under the traditional model, whereas all births were included in the fetuses-at-risk formulation.
This study was exempted from ethics approval as analyses were performed on publicly accessible de-identified data. All analyses were carried out using SAS software, version 9.2 (SAS Institute Inc., Cary NC). A two-tailed P value <0.05 was considered significant.
Results
There were 5,456,260 singleton births to mothers aged 20–29 years and 1,390,435 singleton births to mothers aged 35 years or more in the United States between 2003 and 2005. Fetal death rates were 3.1 per 1000 total births among younger mothers and 4.0 per 1000 total births among older mothers, while neonatal mortality rates were 2.5 per 1000 live births among younger mothers and 2.8 per 1000 live births among older mothers (Table 1). The rates of perinatal death were 5.6 among younger mothers and 6.8 per 1000 total births among older mothers. Older mothers were more likely to be married, multiparous, non-Hispanic white, non-smokers and educated as compared with younger mothers (Table 1). The gestational age distribution among older mothers was shifted towards lower gestational ages and older mothers were more likely to have had very low birth weight or high birth weight infants (P<0.001, Table 1).
Under the traditional approach, gestational age-specific fetal, neonatal and perinatal death rates declined with increasing gestation (Figures 1A, 2A, 3A, Table 2). The rate of fetal death at 22–33 weeks gestation was 76.4 per 1000 total births among mothers aged 35 years and older was and this was not significantly different from the fetal mortality rate at 22–33 weeks of 75.6 per 1000 total births among mothers aged 20–29 years (crude odds ratio 1.01, 95% CI 0.97-1.06, Table 3). However, fetal death rates at 34–43 weeks were substantially higher among older mothers compared with younger mothers (crude odds ratio 1.45, 95% CI 1.39-1.51; Figure 1A, Tables 2 and 3). Figure 2 shows gestational age-specific neonatal death rates among older vs younger mothers at early gestation (Table 2). The rate of neonatal death at 22–33 weeks gestation was 67.4 per 1,000 live births among mothers aged 35 years or older and this was significantly lower than the neonatal mortality rate of 72.9 per 1,000 live births among mothers 20–29 years of age (odds ratio 0.93, 95% CI 0.88-0.97, Table 3). On the other hand, neonatal mortality rates at later gestation (34–43 weeks) were higher among older mothers compared with younger mothers (odds ratio 1.13, 95% CI 1.07-1.20; Table 3). Adjustment for confounders strengthened the relationships between older maternal age and perinatal death but did not substantially change the results at early or late gestation (Table 3).
Under the fetuses-at-risk approach, gestational age-specific fetal, neonatal and perinatal death rates increased with increasing gestational age (Figures 1B, 2B, 3B). Fetal death rates were higher among older compared with younger mothers (Figures 1B, 2B and 3B, Table 2, Table 3) at both early gestation (odds ratio 1.21, 95% CI 1.16-1.26) and at later gestation (odds ratio 1.45, 95% CI 1.39-1.51). A similar association was observed for neonatal death rates, with older mothers having higher rates of neonatal death than younger women at early gestation (odds ratio 1.11, 95% CI 1.05-1.16) and at late gestation (odds ratio 1.13, 95% CI 1.07-1.19). Adjustment for potential confounders increased the strength of the association between older maternal age and fetal and neonatal mortality at early and late gestation (Table 3).
Discussion
Our study showed that under the traditional perinatal model, fetal mortality rates at early gestation (22–33 weeks) were non-significantly lower among older vs younger mothers, while neonatal mortality and perinatal mortality rates at early gestation were significantly lower among older women. The opposite was true at later gestation (34–43 weeks), with fetal, neonatal and perinatal mortality rates being higher among older mothers compared with younger mothers. In contrast, the fetuses-at-risk model showed a more consistent picture with older mothers having higher rates of fetal, neonatal and perinatal death at all gestational ages.
Our results provide a comprehensive overview of the findings of previous studies including those restricted to births at early gestation [11], and low birth weight births [12]. Further, our study shows that maternal age contrasts under the tradition perinatal model result in intersecting mortality curves if perinatal death rates among older vs younger mothers are contrasted at early and late gestation. The phenomenon of intersecting perinatal mortality curves has been demonstrated for numerous other determinants including maternal smoking, parity, plurality, infant sex, altitude, race, pregnancy complications such as hypertension, etc [22–30]. Thus the apparent survival advantage that preterm infants of older mothers appear to enjoy is also seen among preterm/low birth weight infants of mothers who smoke compared with preterm/low birth weight infants of mothers do not smoke [29]. This same survival advantage is also observed among preterm/low birth weight infants of women with twin pregnancies (vs those who have singleton pregnancies) [24] and women who have pregnancy complications such as hypertensive disorders (versus those who do not have pregnancy complications) [30]. Although it is tempting to explain away the survival advantage in each of these contrasts with ad hoc explanations, such intersecting perinatal mortality curves are a general phenomenon and the ideal explanation should seek to parsimoniously address all these various contrasts. The fetuses-at-risk approach is a general solution to this paradox in so far as it provides a biologically plausible and consistent result; under this formulation smokers have higher perinatal mortality rates compared with non-smokers at all gestational ages [29], twins have higher perinatal mortality compared with singletons at all gestational ages [24] and women with hypertensive disorders have higher rates of perinatal mortality rates than women without hypertensive disorders at all gestational ages [30].
Disparate results obtained from traditional vs fetuses-at-risk approaches highlight two different perspectives: prognostic (i.e., predictive or acausal) and causal [21]. The traditional approach provides an accurate prognostic perspective for the newborn infant and has utility in predicting neonatal death. Under the traditional model, gestational age serves as an excellent predictor for neonatal mortality and infants born to older mothers at early gestation are observed to have a more favourable prognosis as compared with infants born to younger mothers. The fetuses-at-risk model, on the other hand, provides insights into the biologic role of maternal age (and other factors responsible for intersecting perinatal mortality curves such as smoking, plurality, hypertension in pregnancy) from a fetal perspective. It has little prognostic value but represents a causal model [31, 32] which suggests that older maternal age is causally associated with a higher risk of fetal and neonatal death at early and late gestation. Our study also demonstrates that (causal) etiologic studies restricted to births at early gestation (or low birth weight births) may yield biased results if they use traditional measures of gestational age-specific perinatal mortality since they ignore the biologic continuum of pregnancy [11, 12, 33, 34]. Whereas results based on the traditional model yield valid prognostic estimates, any causal inference based on these associations (whether related to the effect or older maternal age, smoking or hypertensive disorders) is likely biased. The reason for the acausal nature of traditional models and the causal nature of the fetuses-at-risk model relates to how these two models treat gestational age: in the traditional model gestation age is a determinant, whereas in the fetuses-at risk model it represents survival time [27, 31]. Treating gestational age as survival time permits the estimation of incidence rates which are central to causal inference.
While the fetuses-at-risk-based measures of gestational age-specific perinatal mortality represent a causal model, there are some conceptual challenges regarding the optimal analytical approach to model these time-to-event perinatal data [35]. The Cox model constitutes a robust analytical tool for multivariable survival analysis which assumes that censoring is non-informative. This creates a significant problem in perinatal studies wherein stillbirth and live birth represent competing risks in studies of stillbirth (and stillbirth and neonatal death represent competing risks in studies of neonatal death). The competing risk issue between stillbirth and neonatal death is simply resolved by using perinatal death as an outcome, though there are socio-cultural reasons that may require studies to focus on stillbirths or neonatal deaths separately. Logistic regression analyses based on fetuses-at-risk approach and focusing on perinatal death (as done in this study) offer a practical analytical approach to avoiding some of these problems and also address the potential bias introduced by the traditional approach when examining causal associations at early gestation [36].
The strength of our study includes the use of a large population-based dataset with information collected according to uniform protocols across the United States [13]. The limitations include some degree of data inaccuracy that is inevitable in large administrative databases. The ascertainment of gestational age in vital statistics has been traditionally based on menstrual dating, although a clinical estimate of gestation based on early ultrasound is available for recent years [14]. In this study we used the more accurate clinical estimate of gestation and excluded births without such an estimate [14–17]. Some congenital anomalies were likely underreported and this may have affected some estimates in our study. We did not have information on socio-economic status, body mass index and behavioural factors such as substance use or alcohol consumption that are known to be associated with maternal age and perinatal outcomes. Finally, we ascribed time of fetal or neonatal death to the time of birth (in gestational weeks). The former assumption was made because time of fetal death was not available in our data source. For neonatal deaths, we assumed an antepartum cause of death among infants who died during the neonatal period. The time between birth and neonatal death was therefore considered a latent period between the birth of a compromised fetus and neonatal death.
Conclusion
In summary, our study demonstrates that contrasts of traditional gestational age-specific perinatal mortality rates among older versus younger mothers result in the intersecting perinatal mortality curves. The traditional perinatal model provides a varying prognostic perspective on the effect of older maternal age, with protection against neonatal/perinatal death observed at early gestation and an increased risk of neonatal/perinatal death observed at later gestation. On the other hand, the fetuses-at-risk model provides a consistent causal perspective on the effect of older maternal age, with an increased risk of fetal, neonatal and perinatal death observed at all gestational ages. This underscores the need for a proper conceptualization of gestational age-specific perinatal mortality in studies examining causal associations.
Abbreviations
- AOR:
-
Adjusted odds ratio
- NCHS:
-
National Centre for Health Statistics.
References
Statistics Canada, Canadian Vital Statistics, Birth and Stillbirth Databases 3231 and 3234. CANSIM Tables number 102–4515: Live births and fetal deaths (stillbirths), by type (single or multiple), Canada, provinces and territories, annual (number). http://estat.statcan.gc.ca/cgi-win/cnsmcgi.pgm?LANG=E&CIITables=3871&ResultTemplate=ESTAT\CII_FLST&ROOTDIR=ESTAT/&LangFldr=English/&C2DB=. Table number 102–4515. Accessed in April 2013.
Statistics Canada: Births 2009. 2012, Ottawa: Minister of Industry, Catalogue no. 84F0210X. http://www.statcan.gc.ca/pub/84f0210x/84f0210x2009000-eng.pdf. Accessed in April 2013
Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Kirmeyer S, Mathews TJ, Wilson E: Births: Final data for. 2009, http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_01.pdf Accessed: January 2012, . National Vital Statistics Reports 2011. Volume 60, Number 1
National Center for Health Statistics: Vital Statistics of the United States, 1980, Vol. 1, Natality. DHHS Pub. No. (PHS) 85–1100. Public Health Service. 1984, Washington. U.S: Government Printing Office, http://www.cdc.gov/nchs/data/vsus/nat80_1acc.pdf Accessed: January 2012
European Commision: Eurostat yearbook 2002; The statistical guide to Europe, Data 1990–2000. 2002, Luxembourg: Office for Official Publications of the European Communities, 30-http://epp.eurostat.ec.europa.eu/cache/ITY_OFFPUB/KS-40-01-319/EN/KS-40-01-319-EN.PDF Accessed: April 2013, 92-894-1750-1
Office for Official Publications of the European Communities Luxembourg: Eurostat yearbook. 2006, 68,74-http://epp.eurostat.ec.europa.eu/cache/ITY_OFFPUB/KS-CD-06-001/EN/KS-CD-06-001-EN.PDF Accessed: January 2012, –07; Europe in figures. 2007. Catalogue number: KS-CD-06-001-EN-N
Linacre S: Australian social trends 2007. International fertility comparisons. Catalogue No. 4102.0. 2008, Australian Bureau of Statistics, http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/3938C73A2EBD6847CA25732F001C910D/$File/41020_International%20fertility%20comparison_2007.pdf Accessed: January 2012
Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R: The perinatal effects of delayed childbearing. Obstet Gynecol. 2005, 105: 1410-1418. 10.1097/01.AOG.0000163256.83313.36.
Cnattingius S, Forman MR, Berendes HW, Isotalo L: Delayed childbearing and risk of adverse perinatal outcome. A population-based study. JAMA. 1992, 268: 886-890. 10.1001/jama.1992.03490070068044.
Huang L, Sauve R, Birkett N, Fergusson D, van WC: Maternal age and risk of stillbirth: a systematic review. CMAJ. 2008, 178: 165-172.
Kanungo J, James A, McMillan D, Lodha A, Faucher D, Lee SK, Shah PS: Advanced maternal age and the outcome of preterm neonates. Obstet Gynecol. 2011, 118: 872-877. 10.1097/AOG.0b013e31822add60.
Vohr BR, Tyson JE, Wright LL, Perritt RL, Li L, Poole WK: Maternal age, multiple birth, and extremely low birth weight infants. J Pediatr. 2009, 154: 498-503. 10.1016/j.jpeds.2008.10.044.
Department of Health and Human Services, Centre for Disease Control and Prevention, National Centre for Health Statistics, Division of Vital Statistics: Public Use Data File Documentation. 2005, Period Linked Birth/Infant Death Data Set. http://www.cdc.gov/nchs/data_access/Vitalstatsonline.htm Accessed: Dec 2011
Wier ML, Pearl M, Kharrazi M: Gestational age estimation on United States live birth certificates: a historical overview. Paediatr Perinat Epidemiol. 2007, 21 (Suppl 2): 4-12.
Mustafa G, David RJ: Comparative accuracy of clinical estimate versus menstrual gestational age in computerized birth certificates. Public Health Rep. 2001, 116 (1): 15-21. 10.1016/S0033-3549(04)50018-3.
Joseph KS, Huang L, Liu S, Ananth CV, Allen AC, Sauve R: Reconciling the high rates of preterm and postterm birth in the United States. Obstet Gynecol. 2007, 109 (4): 813-822. 10.1097/01.AOG.0000255661.13792.c1.
Ananth CV: Menstrual versus clinical estimate of gestational age dating in the United States: temporal trends and variability in indices of perinatal outcomes. Paediatr Perinat Epidemiol. 2007, 21 (Suppl 2): 22-30.
Joseph KS, Liu S, Rouleau J, Lisonkova S, Hutcheon JA, Sauve R, Allen AC, Kramer MS: Influence of definition based versus pragmatic birth registration on international comparisons of perinatal and infant mortality: population based retrospective study. BMJ. 2012, 344: e746-10.1136/bmj.e746.
Williams Obstetrics. 23nd ed. Edited by: Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. 2010, Toronto, Canada: McGraw- Hill, 3-
Yudkin PL, Wood L, Redman CW: Risk of unexplained stillbirth at different gestational ages. Lancet. 1987, 1: 1192-1194.
Joseph KS: Incidence-based measures of birth, growth restriction, and death can free perinatal epidemiology from erroneous concepts of risk. J Clin Epidemiol. 2004, 57: 889-897. 10.1016/j.jclinepi.2003.11.018.
Yeushalmy J: The relationship of parents’ cigarette smoking to outcome of pregnancy—implications as to the problem of inferring causation from observed associations. Am J Epidemiol. 1971, 93: 443-456.
Wilcox AJ: Birth weight and perinatal mortality: the effect of maternal smoking. Am J Epidemiol. 1993, 137: 1098-1104.
Joseph KS, Liu S, Demissie K: A parsimonious explanation for intersecting perinatal mortality curves: understanding the effect of plurality and of parity. BMC Pregnancy Childbirth. 2003, 3: 3-10.1186/1471-2393-3-3.
Joseph KS: Exegesis on effect modification – biological or spurious?. Paediatr Perinat Epidemiol. 2009, 23: 417-420. 10.1111/j.1365-3016.2009.01051.x.
Hernandez-Díaz S, Schisterman EF, Hernan MA: The birth-weight “paradox” uncovered?. Am J Epidemiol. 2006, 164: 1115-1120. 10.1093/aje/kwj275.
Basso O, Wilcox AJ: Intersecting birthweight-specific mortality curves: solving the riddle. Am J Epidemiol. 2009, 169: 787-797. 10.1093/aje/kwp024.
Platt RW, Joseph KS, Ananth CV, Grondines J, Abrahamowicz M, Kramer MS: A proportional hazards model with time-dependent covariates and time-varying effects for analysis of fetal and infant death. Am J Epidemiol. 2004, 160: 199-206. 10.1093/aje/kwh201.
Joseph KS, Demissie K, Platt RW, Ananth CV, McCarthy BJ, Kramer MS: A parsimonious explanation for intersecting perinatal mortality curves: understanding the effect of race and of maternal smoking. BMC Pregnancy Childbirth. 2004, 4: 7-10.1186/1471-2393-4-7.
Hutcheon JA, Lisonkova S, Joseph KS: Epidemiology of pre-eclampsia and the other hypertensive disorders in pregnancy. Best Pract Res Clin Obstetr Gynaecol. 2011, 25: 391-403. 10.1016/j.bpobgyn.2011.01.006.
Joseph KS: Theory of obstetrics: the fetuses-at-risk approach as a causal paradigm. JOGC. 2004, 26: 953-960.
Joseph KS: The fetuses-at-risk approach: clarification of semantic and conceptual misapprehension. BMC Pregnancy Childbirth. 2008, 8: 11-10.1186/1471-2393-8-11.
Chen XK, Wen SW, Smith G, Yang Q, Walker M: Pregnancy-induced hypertension is associated with lower infant mortality in preterm singletons. BJOG. 2006, 113: 544-551. 10.1111/j.1471-0528.2006.00898.x.
Piper JM, Langer O, Xenakis EM, McFarland M, Elliott BD, Berkus MD: Perinatal outcome in growth-restricted fetuses: do hypertensive and normotensive pregnancies differ?. Obstet Gynecol. 1996, 88: 194-199. 10.1016/0029-7844(96)02169-2.
Platt RW: The fetuses-at-risk-approach: an evolving paradigm. Reproductive and perinatal epidemiology. Edited by: Buck Lois G, Platt RW. Oxford University Press. Inc, 978-0-19-538790-2
Auger N, Delezire P, Harper S, Platt RW: Maternal education and stillbirth: estimating gestational-age-specific and cause-specific associations. Epidemiology. 2012, 23 (2): 247-254. 10.1097/EDE.0b013e31824587bc.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2393/13/87/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None of the authors have a personal financial relationship relevant to this article.
Authors’ contribution
SL and KSJ contributed to the conception and design of the study, SL conducted the data analysis and drafted the manuscript and EP and KSJ revised the manuscript for intellectual content; all authors approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lisonkova, S., Paré, E. & Joseph, K. Does advanced maternal age confer a survival advantage to infants born at early gestation?. BMC Pregnancy Childbirth 13, 87 (2013). https://doi.org/10.1186/1471-2393-13-87
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2393-13-87