Abstract
Background
Schimke immuno-osseous dysplasia (SIOD, OMIM #242900) is an autosomal-recessive pleiotropic disorder characterized by spondyloepiphyseal dysplasia, renal dysfunction and T-cell immunodeficiency. SIOD is caused by mutations in the gene SMARCAL1.
Case presentation
We report the clinical and genetic diagnosis of a 5-years old girl with SIOD, referred to our Center because of nephrotic-range proteinuria occasionally detected during the follow-up for congenital hypothyroidism. Mutational analysis of SMARCAL1 gene was performed by polymerase chain reaction (PCR) and bidirectional sequencing. Sequence analysis revealed that patient was compound heterozygous for two SMARCAL1 mutations: a novel missense change (p.Arg247Pro) and a well-known nonsense mutation (p.Glu848*).
Conclusion
This report provided the clinical and genetic description of a mild phenotype of Schimke immuno-osseous dysplasia associated with nephrotic proteinuria, decreasing after combined therapy with ACE inhibitors and sartans. Our experience highlighted the importance of detailed clinical evaluation, appropriate genetic counseling and molecular testing, to provide timely treatment and more accurate prognosis.
Similar content being viewed by others
Background
Schimke Immuno-Osseous Dysplasia [SIOD; OMIM #242900] is a rare autosomal recessive multisystem disorder, firstly described in 1971 [1, 2]. Approximately 50 cases have been reported in the literature so far, without any apparent sex, ethnic or geographic predilection. The exact prevalence of the disease is unknown, in North America the incidence is estimated at 1:1,000,000 to 1:3,000,000 live births. Typical findings of SIOD are spondyloepiphyseal dysplasia with disproportionate growth failure, typical facial appearance, nephrotic syndrome with focal segmental glomerulosclerosis (FSGS) and progressive renal failure, recurrent lymphopenia, T-cell immunodeficiency, and pigment naevi [1–3]. Other features include hypothyroidism, episodic cerebral ischaemia and bone marrow failure [4]. The SIOD phenotype may range from a severe variant with in utero onset to a milder form with later onset [5, 6]. SIOD is caused by mutations in the gene encoding HepA-related protein (HARP) also known as SMARCAL1 [SWI/SNF-related, matrix associated, actin-dependent regulator of chromatin, subfamily a-like 1; Gene ID: 50485; NG_009771.1], a protein homologous to the sucrose non fermenting type 2 (SNF2) family of chromatin-remodeling proteins, required for transcriptional regulation, replication, repair, recombination, and covalent modification [7–11]. Biallelic putative loss of function mutations in SMARCAL1 gene are the only identified causes of SIOD, however approximately half of patients referred for molecular studies have no detectable mutations in the coding region of this gene, thus environmental, genetic, or epigenetic modifiers and the existence of endophenotypes of SIOD have been hypothesized [10].
Here, we report the clinical and genetic diagnosis of a 5-years old girl with SIOD, referred to our Center because of nephrotic-range proteinuria occasionally detected during the follow-up for congenital hypothyroidism.
Case presentation
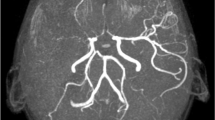
The patient was born at 29 week of gestation as the first child of healthy non-consanguineous Italian parents. Her birth weight was 720 g (<3rd percentile). Congenital hypothyroidism was quickly diagnosed and substitutive therapy was started at birth time. At 5-years, she was referred to our Pediatric Nephrology Center. At clinical examination she had disproportionately short stature (94 cm; <3rd percentile), low weight (13,5 kg; <3rd percentile), reduced occipitofrontal head circumference (OFC) (48,1 cm; <3rd percentile), dorsolumbar kyphoscoliosis, fine hair, pale skin, low nasal bridge. She had normal intelligence and never had severe infections, migraines or transient ischemic attacks. Moreover she did not present short neck or trunck, hyperpigmented macules, corneal opacities or hypertension. Laboratory data showed nephrotic range proteinuria (1,7 g/die; 125 mg/kg/die) and normal renal function (creatinine clearance 84,75 ml/min, according to the Schwartz-formula). Lymphopenia with T-cell deficiency was also detected. Skeletal radiograph revealed dorsolumbar kyphoscoliosis with unbalanced iliac crests, but other findings consistent with the diagnosis of spondyloepiphyseal dysplasia, such as ovoid and mildly flattened vertebral bodies, small deformed capital femoral epiphyses, and shallow dysplastic acetabular fossae, were absent. The renal biopsy was performed and revealed FSGS (Figure 1A-B). Treatment with ramipril and irbesartan resulted in a reduction of proteinuria (0,104 g/die). After two-years follow-up, the patient displays normal renal function without proteinuria and no episodes of infection or cerebrovascular complication.
Renal histology of SIOD patient. Light microscopy images (A, B) showing larger glomerular volume, with a sclerotic lesion of the glomerular tuft. The remaining part of the glomerulus shows focal and segmental matrix increase and mesangial proliferation. Diffuse tubular atrophy and rare arteriolar ialinosis are also present (A: PAS staining, B: Masson’s Trichrome stain; ×400).
On the basis of clinical and laboratory findings, a diagnosis of SIOD was suspected. After obtaining informed consent for genetic studies, genomic DNA was purified from peripheral blood samples of proband and all available family members (one sibling, mother and father) using standard procedures.
Mutational analysis of SMARCAL1 gene [NM_014140.3 GI:187761312; NG_009771.1 GI:223671908; GeneID: 50485] was performed by polymerase chain reaction (PCR) and bidirectional sequencing of the coding exons and intron/exon flanking regions, as previously described [12]. SMARCAL1 flanking intronic primers were designed using primer3 program (http://primer3.wi.mit.edu/). PCR products were sequenced using the Big Dye Terminator v3.1 cycle sequencing kit on 3130 Genetic Analyzer (Life Technologies, Ltd). SMARCAL1 mutation was named according to Human Genome Variation Society recommendations (http://www.hgvs.org/mutnomen) and NCBI Reference Sequence [NM_014140.3 GI:187761312]. The potential effect of novel missense mutation was analyzed using SIFT (Sorting Intolerant From Tolerant) programme [13] and Polyphen programme [14].
Sequence analysis revealed that patient was compound heterozygous for two mutations (Figure 2A): a novel missense mutation in exon 3 (c.740G > C), resulting in an arginine-to-proline substitution (p.Arg247Pro), inherited by the mother; and a nonsense paternally-derived mutation in exon 17 (c.2542G > T) resulting in the substitution of Glu848 with a stop codon (p.Glu848*) [9]. The healthy brother was wild type for detected mutations (data not shown). This study have been performed in accordance with the Declaration of Helsinki and was approved by the Ethical Committee of University Hospital in Foggia.
Conclusions
SIOD is a rare autosomal recessive pleiotropic disorder caused by mutations in SMARCAL1 gene [1, 2]. So far, about 55 different mutations in SMARCAL1 gene have been identified in SIOD patients from different ethnic backgrounds [9, 10, 15, 16]. The pathogenesis of SIOD is largely unknown. SMARCAL1 gene encodes the HepA-related protein (HARP), a member of the SNF2 family of ATPases, acting as chromatin remodelers within multi-protein complexes [11]. This protein is an ATP-driven annealing helicase, involved in a wide range of biological functions, including transcription, DNA replication, and DNA repair. SIOD patients exhibit a continuum from mild to severe disease. Severe form is characterized by intrauterine growth retardation, severe growth failure after birth, recurrent infections, hematological abnormalities, hypothyroidism, cerebrovascular disease and often death within the first 15-years. Mild form usually displays growth failure and renal dysfunction between 8–12 years, without infections or cerebrovascular disease [4–6]. Of note, our patient fulfilled all the criteria for the mild phenotype of SIOD, i.e., absence of disease symptoms in the 1st year of life [1], growth failure and nephrotic syndrome starting in childhood [2], normal thyroid function tests and [5] no infectious or cerebrovascular symptoms until now [4, 5]. However early recognition of characteristic growth retardation coupled with bone abnormalities may represent key clues for the diagnosis of this genetic disease even in mild form. Skeletal examination in these patients may show bone changes suggestive for spondyloepiphyseal dysplasia, driving the correct diagnosis.
Usually, patients with SMARCAL1 biallelic missense mutations or a missense and a nonsense mutation have a milder disease. Accordingly, our patient, compound heterozygous for a novel missense mutation (p.Arg247Pro) and a well-known nonsense mutation (p.Glu848*) [9], displayed a mild form. The missense mutation (p.Arg247Pro) within the first HARP domain (HARP1), described for the first time in this report, is located in a highest-conserved site of the multi-sequence alignment (Figure 2B) and is predicted to be a damaging change by SIFT (Sorting Intolerant From Tolerant) programme [13] with a score of 0.0 and a ‘probably damaging’ substitution by Polyphen-programme [14] with a score of 1.000. All SNF2 proteins are characterized by the presence of SWI/SNF helicase motifs but do not always exhibit helicase activity. SMARCAL1 protein has ATP-dependent annealing helicase activity, which helps to stabilize stalled replication forks and facilitate DNA repair during replication. Recently, it was shown that the conserved tandem HARP (2HP) domain dictates this annealing helicase activity, suggesting that the HARP domains are important determinants of the SMARCAL1 enzyme specificity [17]. The nonsense mutation, p.Glu848*, leading to a truncated SMARCAL1 protein of 847 aa, was previously reported in other SIOD patients with different ethnic origin [9].
The patient was referred to our attention because of onset of proteinuria in nephrotic range. Renal biopsy revealed FSGS, which is the most frequent renal pathological finding associated with SIOD, as described in a revision of 39 SIOD cases with proteinuria [18]. Nevertheless cases of minimal change disease, membranous nephropathy, mesangial proliferative glomerulonephritis and nephrophthisis have been also described [15, 18]. Kidney involvement in SIOD patients displays typically proteinuria evolving to overt nephrotic syndrome, usually diagnosed between 1–14 years [4–6, 9]. This genetic form of nephrotic syndrome usually does not respond to steroid treatment [6, 16]; nevertheless, transient reductions in proteinuria using ACE-inhibitors, NSAID or even cyclosporine-A have been documented [4–6, 9]. Our experience demonstrate that nephrotic proteinuria associated with a mild form of SIOD may respond to combined therapy with ACE- inhibitors and sartans, supporting the concept that several missense mutations in SMARCAL1 gene retain some residual function [15]. However most of patients, mainly with severe forms, progress to ESRD between 5–15 years of age. No relapse of proteinuria has been described in SIOD patients after renal transplantation [15], while the evolution of cerebrovascular and infectious complications do not seem to improve after transplantation.
In conclusion, we report a mild phenotypic expression of SIOD associated with a new genotype consisting of compound-heterozygosity for a known nonsense mutation and a novel SMARCAL1 missense change, characterized by nephrotic proteinuria, which decreased after combined therapy with ACE inhibitors and sartans. Our experience highlighted the importance of detailed clinical evaluation, appropriate genetic counseling and molecular testing, to provide timely treatment and more accurate prognosis.
Consent
Written informed consent was obtained from parents for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Authors’ information
LS: post-graduate school in Nephrology, University of Foggia; MG (PhD): Post-graduate school in Medical Genetics, permanent position as Biologist, University of Foggia; GSN: MD PhD, Assistant Professor of Clinical Pathology, University of Foggia; SD: laboratory technician, University of Foggia; FP, VC and MG (MD): Staff physician, Pediatric Nephrology Unit, Ospedale “Giovanni XXIII”, Bari; GG: Associate Professor of Nephrology, University of Foggia; LG: Full Professor of Nephrology, University of Bari.
Abbreviations
- HARP:
-
HepA-related protein
- PCR:
-
Polymerase chain reaction
- SIFT:
-
Sorting intolerant from tolerant
- SMARCAL1:
-
SWI/SNF-related, matrix associated, actin-dependent regulator of chromatin, subfamily a-like 1
- SNF2:
-
Sucrose non fermenting type 2
- NSAID:
-
Nonsteroidal anti- inflammatory drugs
- ACE-inhibitors:
-
Angiotensin-converting-enzyme inhibitors.
References
Schimke RN, Horton WA, King CR: Chondroitin-6-sulphaturia, defective cellular immunity, and nephrotic syndrome. Lancet. 1971, 2: 1088-1089.
Spranger J, Hinkel GK, Stoss H, Thoenes W, Wargowski D, Zepp F: Schimke immuno-osseous dysplasia: a newly recognized multisystem disease. J Pediatr. 1991, 119: 64-72. 10.1016/S0022-3476(05)81040-6.
Lücke T, Franke D, Clewing JM, Boerkoel CF, Ehrich JH, Das AM, Zivicnjak M: Schimke versus non-Schimke chronic kidney disease: an anthropometric approach. Pediatrics. 2006, 118: e400-e407. 10.1542/peds.2005-2614.
Boerkoel CF, O’Neill S, André JL, Benke PJ, Bogdanovíć R, Bulla M, Burguet A, Cockfield S, Cordeiro I, Ehrich JH, Fründ S, Geary DF, Ieshima A, Illies F, Joseph MW, Kaitila I, Lama G, Leheup B, Ludman MD, McLeod DR, Medeira A, Milford DV, Ormälä T, Rener-Primec Z, Santava A, Santos HG, Schmidt B, Smith GC, Spranger J, Zupancic N, et al: Manifestations and treatment of Schimke immuno- osseous dysplasia: 14 new cases and a review of the literature. Eur J Pediatr. 2000, 159: 1-7. 10.1007/s004310050001.
Saraiva JM, Dinis A, Resende C, Faria E, Gomes C, Correia AJ, Gil J, da Fonseca N: Schimke immuno-osseous dysplasia: case report and review of 25 patients. J Med Genet. 1999, 36: 786-789. 10.1136/jmg.36.10.786.
Ehrich JH, Burchert W, Schirg E, Krull F, Offner G, Hoyer PF, Brodehl J: Steroid resistant nephrotic syndrome associated with spondyloepiphyseal dysplasia, transient ischemic attacks and lymphopenia. Clin Nephrol. 1995, 43: 89-95.
Coleman MA, Eisen JA, Mohrenweiser HW: Cloning and characterization of HARP/SMARCAL1: a prokaryotic HepArelated SNF2 helicase protein from human and mouse. Genomics. 2000, 65: 274-282. 10.1006/geno.2000.6174.
Muthuswami R, Truman PA, Mesner LD, Hockensmith JW: A eukaryotic SWI2/SNF2 domain, an exquisite detector of double-stranded to single-stranded DNA transition elements. J Biol Chem. 2000, 275: 7648-7655. 10.1074/jbc.275.11.7648.
Boerkoel CF, Takashima H, John J, Yan J, Stankiewicz P, Rosenbarker L, André JL, Bogdanovic R, Burguet A, Cockfield S, Cordeiro I, Fründ S, Illies F, Joseph M, Kaitila I, Lama G, Loirat C, McLeod DR, Milford DV, Petty EM, Rodrigo F, Saraiva JM, Schmidt B, Smith GC, Spranger J, Stein A, Thiele H, Tizard J, Weksberg R, Lupski JR, et al: Mutant chromatin remodeling protein SMARCAL1 causes Schimke immuno osseous dysplasia. Nat Genet. 2002, 30: 215-220. 10.1038/ng821.
Clewing JM, Fryssira H, Goodman D, Smithson SF, Sloan EA, Lou S, Huang Y, Choi K, Lücke T, Alpay H, André JL, Asakura Y, Biebuyck-Gouge N, Bogdanovic R, Bonneau D, Cancrini C, Cochat P, Cockfield S, Collard L, Cordeiro I, Cormier-Daire V, Cransberg K, Cutka K, Deschenes G, Ehrich JH, Fründ S, Georgaki H, Guillen-Navarro E, Hinkelmann B, Kanariou M, et al: Schimke immunoosseous dysplasia: suggestions of genetic diversity. Hum Mutat. 2007, 28: 273-83. 10.1002/humu.20432.
Hall MC, Matson SW: Helicase motifs: the engine that powers DNA unwinding. Mol Microbiol. 1999, 34: 867-877. 10.1046/j.1365-2958.1999.01659.x.
Gigante M, D’Altilia M, Montemurno E, Diella S, Bruno F, Netti GS, Ranieri E, Stallone G, Infante B, Grandaliano G, Gesualdo L: Branchio-Oto-Renal Syndrome (BOR) associated with focal glomerulosclerosis in a patient with a novel EYA1 splice site mutation. BMC Nephrol. 2013, 14: 60-10.1186/1471-2369-14-60.
Sorting Intolerant From Tolerant (SIFT) programme web site. http://sift.jcvi.org/www/SIFT_enst_submit.html,
Polyphen programme web site. http://genetics.bwh.harvard.edu/pph2/,
Bökenkamp A, de Jong M, van Wijk JA, Block D, van Hagen JM, Ludwig M: R561C missense mutation in the SMARCAL1 gene associated with mild Schimke immuno-osseous dysplasia. Pediatr Nephrol. 2005, 20: 1724-1728. 10.1007/s00467-005-2047-x.
Zivicnjak M, Franke D, Zenker M, Hoyer J, Lücke T, Pape L, Ehrich JH: SMARCAL1 mutations: a cause of prepubertal idiopathic steroid-resistant nephritic syndrome. Pediatr Res. 2009, 65 (5): 564-568. 10.1203/PDR.0b013e3181998a74.
Ghosal G, Yuan J, Chen J: The HARP domain dictates the annealing helicase activity of HARP/SMARCAL1. EMBO Rep. 2011, 12: 574-80. 10.1038/embor.2011.74.
Ozdemir N, Alpay H, Bereket A, Bereket G, Biyikli N, Aydoğan M, Cakalağoğlu F, Kiliçaslan I, Akpinar I: Membranous nephropathy in Schimke immuno-osseous dysplasia. Pediatr Nephrol. 2006, 21: 870-872. 10.1007/s00467-006-0082-x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2369/15/41/prepub
Acknowledgements
We thank the family for consent to publish the data. This work was supported by MERIT Program n. RBNE08BNL7 from Italian Ministry of Education and University, granted to GSN, and by grant “Premio di ricerca Gianluca Montel, 2011/2012” from University of Foggia, awarded to MG (PhD).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
LS, FP, VC and MG (MD) participated in clinical evaluation, MG (PhD) and SD carried out molecular genetic studies, GSN analyzed data and drafted the manuscript, GG helped to draft the manuscript, and LG participated in design and coordination of study and gave the final approval. All authors’ read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Santangelo, L., Gigante, M., Netti, G.S. et al. A novel SMARCAL1 mutation associated with a mild phenotype of Schimke immuno-osseous dysplasia (SIOD). BMC Nephrol 15, 41 (2014). https://doi.org/10.1186/1471-2369-15-41
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2369-15-41