Abstract
Background
Creatinine secretion, as quantified by the ratio of creatinine clearance (CrCl) to glomerular filtration rate (GFR), may introduce another source of error when using serum creatinine concentration to estimate GFR. Few studies have examined determinants of the CrCl/GFR ratio. We sought to study whether higher levels of albuminuria would be associated with higher, and being non-Hispanic black with lower, CrCl/GFR ratio.
Methods
We did a cross-sectional analysis of 1342 patients with chronic kidney disease from the Chronic Renal Insufficiency Cohort (CRIC) who had baseline measure of iothalamate GFR (iGFR) and 24-hour urine collections. Our predictors included urine albumin as determined from 24-hour urine collections (categorized as: <30, 30-299, 300-2999 and ≥3000 mg), and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic). Our outcome was CrCl/iGFR ratio, a measure of creatinine secretion.
Results
Mean iGFR was 48.0 ± 19.9 mL/min/1.73 m2, median albuminuria was 84 mg per day, and 36.8% of the study participants were non-Hispanic black. Mean CrCl/iGFR ratio was 1.19 ± 0.48. There was no association between the CrCl/iGFR ratio and urine albumin (coefficient 0.11 [95% CI−0.01-0.22] for higest verus lowest levels of albuminuria, p = 0.07). Also, there was no association between race/ethnicity and CrCl/iGFR ratio (coefficient for non-Hispanic blacks was−0.03 [95% CI−0.09-0.03] compared with whites, p = 0.38).
Conclusions
Contrary to what had been suggested by prior smaller studies, CrCl/GFR ratio does not vary with degree of proteinuria or race/ethnicity. The ratio is also closer to 1.0 than reported by several frequently cited reports in the literature.
Similar content being viewed by others
Background
In clinical practice and research studies, kidney function is most often estimated using concentration of serum creatinine, an endogenous filtration marker. This is based on the assumption that creatinine clearance (CrCl) approximates GFR. In considering the limitations of serum creatinine-based estimates of glomerula filtration rate (GFR), much attention has been given to problems stemming from variations in creatinine production which may be reduced as a result of factors such as malnutrition, advanced age or liver disease. Less attention has been given to the fact that creatinine is cleared by the kidneys not only by filtration but also by tubular secretion. So variations in creatinine secretion may introduce another source of error when using serum creatinine concentration to estimate kidney function.
Prior research has shown or suggested that several factors influence the rate of tubular secretion of creatinine which can be quantified as the CrCl/GFR ratio [1]. CrCl/GFR ratio increases as GFR decreases [2, 3] (i.e. tubular secretion plays an increasing important role in renal excretion of creatinine as GFR falls). Other studies have reported that patients with high levels of proteinuria may have high CrCl/GFR ratio. For example, one study reported that patients with nephrotic range proteinuria and low serum albumin had higher tubular secretion of creatinine of 36 ml/min/1.73 m2 (vs. 24 ml/min/1.73 m2 for those with less severe nephrotic syndrome) [4]. Finally, some studies have suggested that African-American patients may have lower CrCl/GFR ratio than non-African Americans [5, 6].
However, these prior studies of the relation between CrCl and GFR have been limited by small sample sizes and inclusion of only a limited spectrum of kidney disease (such as only patients with glomerular disease) [7], and lack of calibration of serum creatinine measurements which render results harder to interpret as systemic errors in serum creatinine measurements may lead to higher or lower CrCl values [6]. In addition, some studies quantified urine protein via excretion of total protein rather than albumin. Measurement of total urine protein is not possible to standardize and is increasingly considered a suboptimal meter of renal dysfunction compared with measurement of albuminuria [8, 9].
To address these knowledge gaps, we explored factors which influence CrCl/GFR ratio in a large diverse cohort of patients with chronic kidney disease (CKD), who had calibrated serum creatinine measurements and quantification of 24-hour urine albumin [10, 11]. We a priori wanted to examine whether greater degree of albuminuria was associated with higher and being non-Hispanic black with lower CrCl/GFR ratio.
Methods
Study population
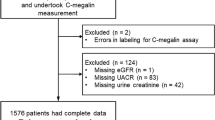
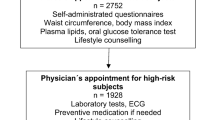
We used baseline data from a subset of participants in the Chronic Renal Insufficiency Cohort (CRIC) study. CRIC is a multicenter prospective cohort sponsored by the National Institutes of Diabetes, Digestive and Kidney Disease (NIDDK) that enrolled patients from seven clinical centers throughout the United States. The design and baseline characteristics of the CRIC cohort (including rationale for inclusion and exclusion criteria) have been published [10, 12]. Briefly, men and women between the ages of 21 and 74 were eligible for the study if they had reduced estimated GFR, based on Modification of Diet in Renal Disease (MDRD) study equation. Inclusion criteria were estimated GFR 20-70 ml/min per 1.73 m2 for person aged 21-44 years, 20-60 ml/min per 1.73 m2 for persons aged 45-64 years, and 20-50 ml/min per 1.73 m2 persons aged 65-74 years. Exclusion criteria included prior renal transplantation, polycystic kidney disease, multiple myeloma, recent use of immunosuppression, and severe comorbid illnesses, such as cirrhosis, HIV disease, and severe (New York Heart Association class III or IV) heart failure. A weighted random sample of approximately one third of the cohort (referred to as the subcohort) was assigned to undergo additional, more intensive testing, including 125I-iothalamate clearance studies to measure GFR. Enrollment started July 2003 and ended March 2007. Additional enrollment of Hispanic participants continued through August 2008 in one center (“Hispanic CRIC”). Of the 3939 participants in CRIC, we included in our study only the 1423 patients who participated in sub-study of 125I-iothalamate clearance. After excluding 81 enrollees who were missing 24-hour urine albumin, our final study sample was 1342.
Measures of kidney function
Our study sample underwent direct GFR measurement by urinary clearance of 125I-iothalamate (iGFR). iGFR was conducted using a protocol similar to that in prior studies [11, 13]. Briefly, after a water load and administration of saturated solution of potassium iodine (SSKI), 125I-iothalamate was injected subcutaneously. After a 60-to 90-min waiting period, timed collections of urine and serum were performed. Urine flow rate was maintained above 1 ml/min. The goal was to obtain four timed urine collection periods bracketed by blood draws to measure plasma iothalamate levels (P). Concurrent urine counts (U) and urine volumes (V) for each period were determined. GFR was calculated as weighted average UV/P and corrected for body surface area. In CRIC, 88% of subcohort enrollees had four or more urine collection periods, 6% had three, and 5% had two or fewer. Due to increased precision of measured GFR values with exclusion of the first clearance period, this measure was used as the reference standard in the analysis. The median coefficient of variation (CV) for the iGFR was 9.7%, excluding the first period [14].
Serum creatinine measurements were done in the CRIC central laboratory at University of Pennsylvania on the Hitachi Vitros 950 calibrated to the MDRD central laboratory at Cleveland Clinic [15] (because the original 4-variable MDRD equation [16] was used as the entry criteria for CRIC). For the analyses in this paper, we further calibrated the Cleveland Clinic creatinine to the standardized IDMS-traceable serum creatinine value as Standardized Cr = Cleveland Clinic serum creatinine*0.95 [17].
At baseline, urine creatinine and albumin excretion were determined from a 24-hour urine collection. Urine albumin was determined by immunoturbidometric assay (Roche Diagnostics) and urine creatinine was done spectrophotometrically with Jaffe method (Roche Diagnostics). The samples were rejected and re-collection attempted if total urine volumes were below 500 cc or collection times below 22 hours or more than 26 hours. All creatinine clearances were calculated in this paper as UV/P with standardized serum creatinine measurements.
Assessments of predictors
We identified a priori several predictors of interest: 24-hour urine albumin, and self-reported race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic) defined at the baseline CRIC visit. We classified 24-hr urine albumin excretion as < 30 mg, 30-299 mg, and ≧300 mg [9]. To allow for the detection of an effect in the nephrotic range, we further divided the last group, macro-albuminuria (also known as severely increased albuminuria), in to above or below 3000 mg.
Assessments of outcome
The outcome variable of our study was the CrCl to iGFR ratio. CrCl and iGFR were both expressed as ml/min normalized to body surface area.
Statistical analysis
Baseline characteristics of CRIC subcohort participants were described using mean ± standard deviation or median (25th-75th percentiles) for continuous variables and number (percentage) for categorical variables.
Linear regression was used to test univariate associations between the CrCl/iGFR ratio and a comprehensive list of baseline demographic and clinical characteristics (Table 1). Characteristics that were found to be significantly associated with CrCl/iGFR ratio were included in subsequent multivariable models.
We explored the distribution of CrCl/iGFR ratio and CrCl by quintiles of iGFR. Linear regression was to determine the association between CrCl/iGFR ratio and 24-hour urine albumin and race/ethnicity in crude and adjusted models. Because iGFR is in the denominator of the outcome, we did not include it as a predictor.
In a sensitivity, analysis to reduce the skewness of residuals, we examined log-transformed CrCl/iGFR ratio as the outcome of interest.
All statistical analyses were performed using STATA 12 (STATA Corp, College Station, TX). A p-value < 0.05 was considered statistically significant.
Regulatory approval
De-identified data for this analysis were retrieved from the National Institutes of Diabetes and Digestive and Kidney Disease (NIDDK) Data Repository (https://www.niddkrepository.org/niddk/home.doH) after appropriate institutional review board approval was obtained (University of California San Francisco Committee on Human Research IRB Number: 10-04231).
Results
Among the 1,342 participants in our study, the mean age was 56 years, 57% were men, and 37% were non-Hispanic black. The mean (± standard deviation [SD]) CrCl was 54.9 ± 27.2 mL/min/1.73 m2 and mean iGFR 48.0 ± 19.9 mL/min/1.73 m2 (Table 1). Mean CrCl/iGFR ratio was 1.19 ± 0.47 and median CrCl/iGFR ratio was 1.15 (with interquarile range [IQR] 0.92-1.39). The median time lapse between 24-hour urine collection and iGFR measurement was 0 days (IQR 0 to 11 days) (mean time lapse 21 days).
We found, similar to prior studies, that patients with lower iGFR had higher CrCl/iGFR ratios (Table 2).
Of the characteristics listed in Table 1, CKD patients with higher BUN, high creatinine and lower hemoglobin had higher CrCl/iGFR ratio. The only other factors associated with the CrCl/iGFR ratio were the use of loop diuretics (associated with higher CrCl/iGFR ratio of 0.09, p = 0.001) and hemoglobin A1C (each 1% increase in hemoglobin A1c was associated with a 0.02 lower CrCl/iGFR ratio, p = 0.007). There was no association with use of thiazide diuretics.
There was no significant correlation between degree of albuminuria and ratio of CrCl/iGFR (rs = 0.02, p = 0.40 in Spearman’s correlation test) (Figure 1). In unadjusted models, categories of albuminuria were not associated with higher CrCl/iGFR ratios (Table 3). Results were unchanged in multivariable analyses controlling for age, sex, race/ethnicity, use of loop diuretics and hemoglobin A1c levels (Table 3). Even patients with ≥ 3000 mg of 24-hour urine albumin did not appear to have increased tubular secretion of creatinine compared to normal albuminuria group. Additionally, CrCl/iGFR ratio in patients (N = 47) with serum albumin <3.0 g/dl was 1.21 ± 0.48 and that in with serum albumin ≥3.0 g/dl (N = 1260) was 1.19 ± 0.48 (p-value 0.89). Also there was no association between degree of albuminuria and the ratio of CrCl/iGFR within substrata of iGFR level (data not shown).
Mean CrCl/iGFR was not significantly different between non-Hispanic black and non-Hispanic white patients (Table 4). The results were similar after further adjusting for age, sex, race/ethnicity, use of loop diuretics and hemoglobin A1c levels. CRIC participants who were Hispanic also did not have statistically different CrCl/iGFR ratios compared with non-Hispanic white participants (Table 4). There was no association between race/ethnicity and the ratio of CrCl/iGFR within substrata of iGFR level.
Similar results were seen in a sensitivity analysis using log-transformed CrCl/iGFR ratio as the outcome (data not shown).
Discussion and conclusions
In this well characterized cohort of CKD patients with mean measured GFR of 48 m/min/1.73 m2, we found that the mean CrCl/GFR ratio was 1.19. This ratio is considerably lower than that reported by older papers in the literature (although similar to certain more recently published studies [18]). For example, in a frequently cited article based on 171 patients, Shemesh et al. reported that in the range of measured GFR of 40-80 ml/min/1.73 m2 (mean 60 ml/min/1.73 m2) the CrCl/GFR ratio was 1.57 [7, 19, 20]. Bauer et al. described CrCl/GFR ratios of 1.62-1.87 when measured GFR was 40-70 ml/min/1.73 m2[3]. Reasons for this potential difference may include the fact that both Shemesh and Bauer measured GFR using inulin clearance rather than iothalamate clearance and the former is known to be lower than the latter [21]. A second possibility is that prior CrCl values may be artifactually high as a result of serum creatinine calibration measurement problems which were not fully appreciated in prior studies. Another hypothesis is that CrCl/GFR ratio varies by patient characteristics. For example, the Shemesh paper only included patients with glomerular disease who presumably had greater proteinuria than the CRIC enrollees, although the degree of proteinuria was not reported.
Indeed some prior papers suggested that CrCl/GFR ratio increases at higher levels of proteinuria. Carrie et al. reported that the CrCl/GFR ratio was 1.22 for 10 patients with cardiac failure (and mean inulin clearance of 47 ml/min/1.73 m2) but it was 1.70 for 38 patients with nephrotic syndrome (and mean inulin clearance of 42 ml/min/1.73 m2) [22]. Branten et al. reported that in 42 patients with nephrotic syndrome (mean GFR 54 ml/min/1.73 m2), hypoalbuminemia was associated with more secretory clearance of creatinine and as a consequence, overestimation of GFR by endogenous CrCl is more pronounced in patients with nephrotic syndrome [4]. However, others have not observed that proteinuria influences the CrCl/GFR ratio [23–25]. Our results do not show an association between degree of proteinuria as assessed by 24-hr urine albumin and CrCl/iGFR ratio. Although the fraction of our study population with high grade proteinuria was relatively low, because of the large sample size, we still had more than 100 patients with albuminuria ≥ 3000 mg/day. We also did not find any association between hypoalbuminemia and tubular creatinine secretion, although our study did not include many patients with severe hypoalbuminemia (e.g. serum albumin <2.5 g/dl) [4].
Our study also contributes to the literature by assessing the relation between race/ethnicity and CrCl/iGFR ratio. Blacks in the U.S. population are known to have higher mean serum creatinine concentration than whites [26]. Previously, based on the relatively low CrCl/iGFR ratios (ranging from 1.01-1.21) reported out of an exclusively black CKD cohort, some investigators have speculated that there may be black-white differences in tubular handling of creatinine [6]. Our results do not support this hypothesis. We found that non-Hispanic white, and non-Hispanic black (and Hispanic) CRIC participants have similar CrCl/iGFR ratio. As alluded to before, comparing results from different publications may be confounded by differences in the exogenous filtration marker used to measure GFR and by serum creatinine calibration problems.
Our finding that use of loop diuretics was associated with higher CrCl/GFR has been noted before [27, 28]. Possible mechanisms for this include reduction in GFR due to tubule-glomerular feedback [29, 30] out of proportion to reduction in CrCl, hence resulting in a higher CrCl/iGFR ratio. But this rather speculative as we are not aware of any evidence for or against this hypothesis. Our report that HgA1c is associated with the CrCl/iGFR ratio is novel. However, since we screened for a large number of associations, we cannot rule out that this result is due to chance and should be evaluated in future studies.
We confirmed there was an inverse correlation between CrCl/iGFR with iGFR. This is consistent with the prior literature which showed that at progressive more severe degrees of CKD, tubular secretion of creatinine plays an increasing prominent role in clearance [3, 28, 31–33]. We interpreted the observation that CKD patients with higher BUN, high creatinine and lower hemoglobin had higher CrCl/iGFR ratio as being because higher BUN, high creatinine and lower hemoglobin reflect lower GFR values.
The strengths of our study are numerous and include a large, diverse sample, the wide range of GFR, the assessment of proteinuria using albuminuria, the calibration of serum creatinine measurements to an external accepted international gold standard, and the uniform assessment of GFR and CrCl across racial/ethnic groups which provide reliable information about potential racial/ethnic differences.
Limitations of our study include that iGFR and CrCl were not measured using the same UV/P blood and urine samples. Certain intrinsic renal diseases were not represented by study design such as polycystic kidney disease or myeloma kidney. We do not have information on use of trimethoprim and cimetidine, although the use of these medications are likely to be infrequent. Inaccuracies in 24-hour urine collection may have introduced random error and biased results towards the null. We did have to exclude some CRIC enrollees who were missing 24-hour albumin measurements but this should not have introduced bias given the small fraction (<6%). Our study was cross-sectional so we do not have information regarding evolution of CrCl/iGFR over time.
There are several implications of our study results. One, the CrCl/iGFR ratio is closer to 1.0 than reported by several frequently cited reports in the literature. So CrCl is closer to GFR better than the impression given by those some papers. Two, it is reassuring that factors such as degree of proteinuria (or others variables listed in Table 1) do not strongly influence CrCl/GFR ratio. Because if a multitude of factors influenced the CrCl/GFR ratio, then it would make it ever more challenging to rely on serum creatinine to estimate GFR. Three, we hope this line of work will bring fresh attention to creatinine secretion. Better understanding of determinants of creatinine secretion may have implications as a recent study reported that variants in the gene coding organic cation tranporter 2 influences both net tubular creatinine secretion and risk of end-stage renal disease [18].
To conclude, using calibrated creatinine measurements and iothalamate clearance to define GFR, we quantified the ratio of CrCl/iGFR in a large modern cohort. To our knowledge, this the largest study quantifying this important aspect of renal physiology.
References
Brod J, Sirota JH: The renal clearance of endogenous “Creatinine” in man. J Clin Invest. 1948, 27 (5): 645-654. 10.1172/JCI102012.
Berlyne GM, Varley H, Nilwarangkur S, Hoerni M: Endogenous-creatinine clearance and glomerular-filtration rate. Lancet. 1964, 2 (7365): 874-876.
Bauer JH, Brooks CS, Burch RN: Clinical appraisal of creatinine clearance as a measurement of glomerular filtration rate. Am J Kidney Dis. 1982, 2 (3): 337-346.
Branten AJ, Vervoort G, Wetzels JF: Serum creatinine is a poor marker of GFR in nephrotic syndrome. Nephrol Dial Transplant. 2005, 20 (4): 707-711. 10.1093/ndt/gfh719.
Coresh J, Toto RD, Kirk KA, Whelton PK, Massry S, Jones C, Agodoa L, Van Lente F: Creatinine clearance as a measure of GFR in screenees for the African-American study of kidney disease and hypertension pilot study. Am J Kidney Dis. 1998, 32 (1): 32-42. 10.1053/ajkd.1998.v32.pm9669421.
Hsu CY, Chertow GM, Curhan GC: Methodological issues in studying the epidemiology of mild to moderate chronic renal insufficiency. Kidney Int. 2002, 61 (5): 1567-1576. 10.1046/j.1523-1755.2002.00299.x.
Shemesh O, Golbetz H, Kriss JP, Myers BD: Limitations of creatinine as a filtration marker in glomerulopathic patients. Kidney Int. 1985, 28 (5): 830-838. 10.1038/ki.1985.205.
Martin H: Laboratory measurement of urine albumin and urine total protein in screening for proteinuria in chronic kidney disease. Clin Biochem Rev. 2011, 32 (2): 97-102.
Wheeler DC, Becker GJ: Summary of KDIGO guideline: what do we really know about management of blood pressure in patients with chronic kidney disease?. Kidney Int. 2013, 83 (3): 377-383. 10.1038/ki.2012.425.
Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, Townsend RR, Xie D, Cifelli D, Cohan J, et al: Chronic renal insufficiency cohort (CRIC) study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009, 4 (8): 1302-1311. 10.2215/CJN.00070109.
Hsu CY, Propert K, Xie D, Hamm L, He J, Miller E, Ojo A, Shlipak M, Teal V, Townsend R, et al: Measured GFR does not outperform estimated GFR in predicting CKD-related complications. J Am Soc Nephrol. 2011, 22 (10): 1931-1937. 10.1681/ASN.2010101077.
Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, Fink JC, Franklin-Becker ED, Go AS, Hamm LL, et al: The chronic renal insufficiency cohort (CRIC) study: design and methods. J Am Soc Nephrol. 2003, 14 (7 Suppl 2): S148-S153.
Levey AS, Berg RL, Gassman JJ, Hall PM, Walker WG: Creatinine filtration, secretion and excretion during progressive renal disease: modification of diet in renal disease (MDRD) study group. Kidney Int Suppl. 1989, 27: S73-S80.
Anderson AH, Yang W, Hsu CY, Joffe MM, Leonard MB, Xie D, Chen J, Greene T, Jaar BG, Kao P, et al: Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2012, 60 (2): 250-261. 10.1053/j.ajkd.2012.04.012.
Joffe M, Hsu CY, Feldman HI, Weir M, Landis JR, Hamm LL: Variability of creatinine measurements in clinical laboratories: results from the CRIC study. Am J Nephrol. 2010, 31 (5): 426-434. 10.1159/000296250.
Levey AS, Greene T, Kusek JW, Beck GJ: A simplified equation to predict glomerular filtration rate from serum creatinine. J Am Soc Nephrol. 2000, 11: 155A-abst
Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW, Van Lente F: Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007, 53 (4): 766-772. 10.1373/clinchem.2006.077180.
Reznichenko A, Sinkeler SJ, Snieder H, van den Born J, De Borst MH, Damman J, Van Dijk MC, Van Goor H, Hepkema BG, Hillebrands JL, et al: SLC22A2 is associated with tubular creatinine secretion and bias of estimated GFR in renal transplantation. Physiol Genomics. 2013, 45 (6): 201-209. 10.1152/physiolgenomics.00087.2012.
Levey AS, Perrone RD, Madias NE: Serum creatinine and renal function. Annu Rev Med. 1988, 39: 465-490. 10.1146/annurev.me.39.020188.002341.
K/DOQI: Clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002, 39 (2 Suppl 1): S1-S266.
Perrone RD, Steinman TI, Beck GJ, Skibinski CI, Royal HD, Lawlor M, Hunsicker LG: Utility of radioisotopic filtration markers in chronic renal-insufficiency–simultaneous comparison of I-125 iothalamate, Yb-169 Dtpa, Tc-99 m-Dtpa, and inulin. Am J Kidney Dis. 1990, 16 (3): 224-235.
Carrie BJ, Golbetz HV, Michaels AS, Myers BD: Creatinine: an inadequate filtration marker in glomerular diseases. Am J Med. 1980, 69 (2): 177-182. 10.1016/0002-9343(80)90376-9.
Anderson CF, Jaecks DM, Ballon HS, De Palma JR, Cutler RE: Renal handling of creatinine in nephrotic and non-nephrotic patients. Clin Sci. 1970, 38 (5): 555-562.
Hilton PJ, Roth Z, Lavender S, Jones NF: Creatinine clearance in patients with proteinuria. Lancet. 1969, 2 (7632): 1215-1216.
Kemperman FAW, Silberbusch J, Slaats EH, Prins AM, Weber JA, Krediet RT, Arisz L: Estimation of the glomerular filtration rate in NIDDM patients from plasma creatinine concentration after cimetidine administration. Diabetes Care. 1998, 21 (2): 216-220. 10.2337/diacare.21.2.216.
Jones CA, McQuillan GM, Kusek JW, Eberhardt MS, Herman WH, Coresh J, Salive M, Jones CP, Agodoa LY: Serum creatinine levels in the US population: third national health and nutrition examination survey. Am J Kidney Dis. 1998, 32 (6): 992-999. 10.1016/S0272-6386(98)70074-5.
Levey AS, Bosch JP, Coggins CH, et al: Effects of diet and antihypertensive therapy on creatinine clearance and serum creatinine concentration in the modification of diet in renal disease study. J Am Soc Nephrol. 1996, 7 (4): 556-566.
Caregaro L, Menon F, Angeli P, Amodio P, Merkel C, Bortoluzzi A, Alberino F, Gatta A: Limitations of serum creatinine level and creatinine clearance as filtration markers in cirrhosis. Arch Intern Med. 1994, 154 (2): 201-205. 10.1001/archinte.1994.00420020117013.
Gottlieb SS, Skettino SL, Wolff A, Beckman E, Fisher ML, Freudenberger R, Gladwell T, Marshall J, Cines M, Bennett D, et al: Effects of BG9719 (CVT-124), an A1-adenosine receptor antagonist, and furosemide on glomerular filtration rate and natriuresis in patients with congestive heart failure. J Am Coll Cardiol. 2000, 35 (1): 56-59. 10.1016/S0735-1097(99)00532-X.
Gottlieb SS, Brater DC, Thomas I, Havranek E, Bourge R, Goldman S, Dyer F, Gomez M, Bennett D, Ticho B, et al: BG9719 (CVT-124), an A1 adenosine receptor antagonist, protects against the decline in renal function observed with diuretic therapy. Circulation. 2002, 105 (11): 1348-1353. 10.1161/hc1102.105264.
Tobias GJ, Mc LR, Hopper J: Endogenous creatinine clearance: a valuable clinical test of glomerular filtration and a prognostic guide in chronic renal disease. N Engl J Med. 1962, 266: 317-323. 10.1056/NEJM196202152660701.
Kim KE, Onesti G, Ramirez O, Brest AN, Swartz C: Creatinine clearance in renal disease: a reappraisal. Br Med J. 1969, 4 (5674): 11-14. 10.1136/bmj.4.5674.11.
Bauer JH, Brooks CS, Burch RN: Renal function studies in man with advanced renal insufficiency. Am J Kidney Dis. 1982, 2 (1): 30-35.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2369/14/268/prepub
Acknowledgements
We thank Feng Lin for her technical assistance.
Supported by the National Institutes of Health DK88865 (Dr. Bansal), DK60902 (Dr. Go and Dr. Hsu) and DK92291 (Dr. Hsu) and Taipei Medical University-Wan Fang Hospital, Center of Excellence for Clinical Trial and Research in Neurology & Neurosurgery DOH101-TD-B-111-003 (Dr. Lin).
The CRIC study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The data from the CRIC study reported here were supplied by the NIDDK Central Repositories. This manuscript does not necessarily reflect the opinions or views of the CRIC study, the NIDDK Central Repositories, or the NIDDK.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YCL and CYH conceived and designed the study; ASG and CYH acquired the data; YCL and CYH drafted the manuscript; NB, EV and ASG revised it critically for important intellectual content. All authors analyzed/interpreted the data and gave final approval of the version to be published.
An erratum to this article is available at http://dx.doi.org/10.1186/1471-2369-15-85.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lin, Yc., Bansal, N., Vittinghoff, E. et al. Determinants of the creatinine clearance to glomerular filtration rate ratio in patients with chronic kidney disease: a cross-sectional study. BMC Nephrol 14, 268 (2013). https://doi.org/10.1186/1471-2369-14-268
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2369-14-268