Abstract
Background
Tumor Necrosis Factor-α (TNF-α) has been implicated in the pathogenesis of insulin resistance and obesity. The increased expression of TNF-α in adipose tissue has been shown to induce insulin resistance, and a polymorphism at position -308 in the promoter region ofTNF-α has been shown to increase transcription of the gene in adipocytes. Aim of this study is to investigate the role of the G-308A TNFα variant in obesity and to study the possible influence of this mutation on body fat distribution and on measures of obesity (including Fat Free Mass, Fat Mass, basal metabolic rate), insulin resistance (measured as HOMAIR), and lipid abnormalities. The G-308A TNFα polymorphism has been studied in 115 patients with obesity (mean BMI 33.9 ± 0.5) and in 79 normal lean subjects (mean BMI 24.3 ± 0.3).
Methods
The G-308A variant, detected by PCR amplification and Nco-1 digestion, determines the loss of a restriction site resulting in a single band of 107 bp [the (A) allele].
Results
The (A) allele frequencies of the G-308A TNFα polymorphism were 13.1% in the obese group and 14.6% in the lean subjects, with no significant difference between the two groups. Furthermore, no association was found with BMI classes, body fat distribution, HOMAIR, and metabolic abnormalities.
Conclusions
Our study did not detect any significant association of the G-308A TNFα polymorphism with obesity or with its clinical and metabolic abnormalities in this population. Our data suggests that, in our population, the G-308A TNFα polymorphism is unlikely to play a major role in the pathogenesis of these conditions.
Similar content being viewed by others
Background
Insulin resistance leading to defects in glucose and/or lipid metabolism is a characteristic feature of both obesity and type 2 diabetes. In obesity increased visceral fat distribution is considered important for the development of insulin resistance. Many evidences have linked Tumor Necrosis Factor-alpha (TNF-α) to the metabolic abnormalities of insulin resistance. Adipose tissue has been shown to be a site for TNF-α synthesis, with a direct correlation between levels of TNF-α, obesity and hyperinsulinemia [1]. It has been suggested that TNF may act as an important auto/paracrine regulator of fat cell function which serves to limit adipose tissue expansion, probably by inducing insulin resistance which may in turn cause metabolic disturbances
In vitro studies on cultured cells suggested that TNF-α may exert its anti-insulin effect by suppressing the phosphorylation of the insulin receptor and its substrates [2]. In transgenic animals overexpression of TNF-α mRNA in adipose tissue is associated with insulin resistance [3]. Neutralisation of circulating TNF-α in insulin-resistant obese mouse leads to a significant increase in insulin sensitivity, suggesting that elevated TNF-α levels may contribute to development of insulin resistance [4]. It has also been demonstrated that TNF-α blocks the action of insulin through its ability to inhibit insulin receptor tyrosine kinase activity [4–7] although other mechanisms, such as quantitative regulation of glucose transporters, have also been proposed [8].
Linkage analysis has shown that a marker near the TNF-α region on chromosome 6p21 was significantly linked with obesity in Pima Indians [9]. Mutation analysis has identified a G → A transition in the promoter region of TNF-α at position -308. This polymorphic variant has been shown to affect the promoter region of the TNF-α gene leading to a higher rate of transcription compared to the common allele [10]. Several association studies have been conducted on the G-308A variant, with conflicting results. Fernandez-Real and co-workers [11] have reported a significant association between the G-308A variant and insulin sensitivity, increased BMI and increased production of leptin, suggesting an important role in overeating and obesity. Furthermore, when the presence of the G-308A variant was correlated to measures of body fat analysed by bioelectric impedance, a significant association with percent body fat was found in obese subjects [11]. A recent Swedish study has found a correlation between increasing BMI and this mutation but only in females [12]. However, many other studies have reported negative results, with no correlation between this TNF-α mutation and insulin resistance or any other metabolic abnormality of the insulin resistance syndrome [13–15]. Moreover, large cohort studies in Chinese, Caucasians and American blacks did not shows significant correlation between G-308A polymorphism and insulin resistance or obesity [16, 17], suggesting, if present, only a marginal role of TNF-α in the pathogenesis of these metabolic conditions.
Aim of this study is to investigate in an Italian population the role of the G-308A TNF-α variant in obesity and to study its relation to body fat distribution, insulin resistance measured by HOMAIR, and metabolic abnormalities.
Methods
A total number of 194 Caucasian subjects were studied. The 115 obese subjects were consecutively recruited from the obesity clinic of the department of Clinical Sciences, University of Rome "La Sapienza". All obese patients were recruited on the basis of BMI > 28 Kg/m2, according to previously suggested criteria [18]. Body fat distribution was assessed by waist circumference (WC); the cut-points chosen to differentiate central from peripheral obesity were the following: WC>94 for men and WC>88 for women. These limits involve a trade-off between sensitivity and specificity and were recently described by Kopelman [19]. Furthermore, these limits take into account the metabolic complications of the android biotype. Ninety-eight of the obese subjects underwent bioelectric impedance for the determination of fat-free mass (FFM), fat mass (FAT), basal metabolic rate and % total body water (TBW) (Datasystem vers. 1, Medigroup Milan, Italy). Total fat mass was determined by subtracting FFM from total body weight. The accuracy of FFM determination was increased by using a multifrequency bioimpedance (1–5–10–50–100 KHz) and applying the equation described by Segal et al. [20]. Exclusion criteria were: presence of type 2 diabetes or first degree relatives with type 2 diabetes, presence of thyroid, liver or renal disease and presence of coronary artery disease (CAD).
Control subjects (n = 79) were unrelated individuals randomly chosen from a population of free living individuals screened for CAD risk factors. Exclusion criteria were: presence of BMI > 26, presence of type 2 diabetes or presence of type 2 diabetes in a first degree relative and presence of CAD. CAD was excluded by using the Rose questionnaire and ECG (Minnesota coding) [21]. In both obese and control subjects a complete medical history was obtained with a questionnaire and laboratory parameters including total cholesterol, HDL, LDL, triglycerides, blood glucose and fasting plasma insulin were evaluated as well.
The transition polymorphism G to A in the -308 position of the TNF-α gene was detected by PCR amplification as previously described [11], with the following primers: 5'-AGGCAATAGTTTTGAGGGCCAT-3' and 5'-TCCTCCCTGCTCCGATTCCG-3'. PCR products were digested with 10-fold excess Nco I restriction enzyme at 37°C for 45 minutes and visualised on 3% high resolution agarose gel stained with ethidium bromide. Nco I restriction digestion reveals a two-allele polymorphism that produces 3 bands of different sizes: a 107 bp fragment corresponding to the A allele (restriction site absent) and a set of 87 and 20 bp corresponding to the G allele (restriction site present, the wild-type).
Plasma insulin levels were measured on frozen sample using a radioimmunoassay (Biodata Insulin Kit, Milan, Italy) with an interassay coefficient of variation of 7.5 %.
Homeostasis model assessment for insulin resistance (HOMAIR) was calculated as described by Matthews et al [22].
Categorical variables were compared by chi-square or Fisher's exact test. Differences between continuous variables were evaluated by two-tailed Student's test. All p-values were corrected for differences in age. Genotype distributions between the study groups were compared by 2X2 and 2X3 contingency table and chi-square analysis.
Results
The clinical characteristics of the study subjects are shown in table 1. Obese and lean subjects were significantly different in age (p < 0.01); the two groups were comparable for sex distribution. Obese subjects showed higher fasting plasma insulin (p < 0.0001), although in the normal range, but there was no statistical difference in blood glucose between the two groups. The homeostasis model of assessment for insulin resistance (HOMAIR) was significantly higher in the obese group (p < 0.0003), indicating the presence of lower insulin sensitivity in the obese subjects, as expected. There was no difference between the two groups in the lipid profile.
Ninety-eight obese subjects were studied by bioelectric impedance and were divided into subjects with central and peripheral obesity, according to their body fat distribution: Body fat distribution was assessed by waist circumference (WC), which provides measures of upper body fat deposition and correlates with an increased risk of metabolic and cardiovascular complications [19]. In comparison with subjects with peripheral obesity, those with central obesity were significantly older (51.2 ± 1.6 vs. 39.4 ± 2.5, p < 0.001), had a higher BMI (35.5 ± 0.7 vs. 32.7 ± 1.9, p < 0.01) and a wider waist circumference (108.9 ± 5.0 vs. 90.6 ± 2.4, p < 0.0007). Centrally obese subjects were significantly different in fat-free mass and fat mass (0.007, data not shown). Furthermore, although fasting blood glucose and insulin were not significantly different between groups, HOMAIR was significantly higher in subjects with central obesity (5.79 ± 0.6 vs. 4.04 ± 0.4; p < 0.04), strongly suggesting the presence of a lower level of insulin sensitivity in this subgroup. Finally, total cholesterol, triglycerides and LDL cholesterol were significantly higher in patients with central obesity compared to the peripheral obesity subgroup (p < 0.01), although no difference was found in HDL cholesterol. Overall, these data confirm the expected findings of a worse metabolic profile in subjects with central obesity compared to those with peripheral obesity.
The distribution of the G-308A genotypes and allele frequencies between obese and control subjects was not statistically different (table 2). Observed frequencies were in Hardy-Weinberg equilibrium. Allele frequencies in the control group were similar to that reported in other studies [14, 17] in different ethnic groups. Furthermore, no significant difference was found when the two subgroups of obese subjects (centrally and peripherally obese) were analysed, indicating that the TNF-α polymorphism is not associated with body fat distribution (table 2). Finally, we did not find any association with gender (data not shown).
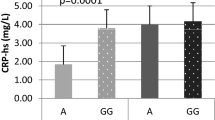
Assuming a dominant model of inheritance (only 4 subjects were homozygous for the mutation), we compared metabolic parameters between GA and AA carriers (n = 145) vs. non-carriers (GG) (n = 49) (table 3). There was no significant difference in fasting blood glucose, fasting plasma insulin nor in HOMAIR, suggesting a non-interference between glucose metabolic pathways and TNF-α gene. No significant difference was also detected between the groups in both lipid profile and body fat distribution parameters (TBW, FFM; FAT). There was a significant association between a lower BMI (p < 0.05) and carrier status. However, when the p-value was corrected for multiple comparisons this analysis did not reach significance.
Finally, in order to further investigate if there was a difference in frequency of the G-308A variant between different grades of BMI, we divided all the 194 subjects into three BMI classes according to WHO criteria [18] (table 4). In class 1 there were subjects with BMI < 25, in class 2 subjects with BMI = 25–29.9, in class 3 subjects with BMI > 30. Even if there was a slight decrease in heterozygosity with BMI increase, there was no significant difference in the frequency of the TNF-α variant between classes.
Discussion
Many evidences link TNF-α to the metabolic abnormalities of insulin resistance. Studies in cells suggested that TNF-α has an anti-insulin effect by suppressing the phosphorylation of the insulin receptor and its substrates [2, 4–7]. Neutralisation of circulating TNF-α by in vivo injection of soluble TNF-α receptor-immunoglobulin G chimeric protein leads to a significant increase in insulin sensitivity [23], and infusion of TNF-α during euglycemic hyperinsulinemic clamp blocks approximately half of the glucose uptake by muscle [24], suggesting that elevated TNFα levels may contribute to development of insulin resistance. The G-308A mutation in the promoter region of TNF-α acts in vitro as a much stronger trascriptional activator than the wild-type TNF-α[10], and it was suggested that a higher transcriptional activity would result in raised TNF-α concentrations followed by decreased insulin sensitivity [10]. However, the concentrations of circulating TNF-α measured in vivo in individuals with different degrees of obesity and insulin resistance did not correlate with metabolic abnormalities [25].
A wealth of genetic studies on the possible role of TNF-α in the etiopathogenesis of insulin-resistance and/or its associated metabolic abnormalities have yielded conflicting results. Linkage has been detected between a marker near TNF-α and obesity in Pima Indians [9] and a further study in a small population (38 subjects) [11] has confirmed this result showing a rise in BMI and fasting plasma insulin in subjects carrying the G-308A TNF-α polymorphism. Results from more recent studies [14, 15] investigating TNF-α gene effects on lipid and glucose metabolism were at variance with previous studies: thus, no correlation with either metabolic (fasting insulin, fasting glucose, HOMAIR) or anthropometric parameters (body fat distribution, FFM, TBW) were found, suggesting that there is no association between TNF-α polymorphism and these parameters.
Due to these contrasting results, the question of whether TNF-α gene is involved or not in the pathogenesis of an altered state in glucose metabolism and obesity still remains to be answered. Our results show no association between the TNFα G-308A mutation and fasting plasma insulin or HOMAIR, suggesting no link between TNFα G-308A mutation and decreased insulin sensitivity in our population
Moreover, comparison of anthropometric parameters between centrally and peripherally obese subjects did not show significant differences according to their TNFα polymorphism status, suggesting that the TNFα G-308A mutation does not play an important role in body fat distribution and its related parameters. Finally, no association between the G-308A polymorphism of TNFα gene and BMI was found in our cohort, a result similar to that found in previous studies [14–16]. Only a recent Swedish study [12] has detected a correlation between increasing BMI and this mutation, but only in females. In our study we did not find any association with gender.
In conclusion, our results suggest that the G-308A mutation of the TNFα gene is unlikely to play an important role in the development of obesity and its related metabolic abnormalities, such as insulin resistance and dyslipidemia, in this Italian population. These results are also in agreement with many other studies in different populations. It is possible that alterations in TNFα are the consequence, and not the primary cause, of the metabolic abnormalities found in insulin-resistance and its associated metabolic and clinical disorders.
References
Qi C, Pekala PH: Tumor necrosis factor-alpha-induced insulin resistance in adipocytes. Proc. Soc Exp Biol Med. 2000, 223 (21): 128-135. 10.1046/j.1525-1373.2000.22318.x.
Feinstein R, Kanety H, Papa MZ, Lunenfeld B, Karasik A: Tumor necrosis factor alpha suppresses insulin-induced tyrosine phosphorylation of insulin receptor and its substrates. J Biol Chem. 1993, 268: 26055-16058.
Teoman Uysal K, Wiesbrock SM, Marino MW, Hotamisligil GS: Protection from obesity-induced insulin resistance in mice lacking TNFα function. Nature. 1997, 389: 610-614. 10.1038/39335.
Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spielgma BM: IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNFα and obesity-induced insulin resistance. Science. 1996, 271: 665-668.
Kroder G, Bassenmaier B, Kellerer M, Capp E, Stoyanov B, Muhlhofer A, Berti L, Harikoshi H, Ulrich A, Haring H: Tumor Necrosis factor-α and hyperglycemia-induced insulin resistance: evidence for different mechanism and different effects on insulin signalling. J Clin Invest. 1996, 97: 1471-1477.
Kanety H, Feinstein R, Papa MZ, Hemi R, Karasik A: Tumor Necrosis Factor-α-induced phosphorylation of insulin receptor substrate-1 (IRS-1). J Biol Chem. 1993, 268: 16055-26058.
Hotamisligil GS, Budavari A, Murray D, Spiegelman BM: TNFα inhibits signalling from insulin receptor. Proc Natl Acad Sci USA. 1994, 91: 4854-4858.
Stephens JM, Pekala PH: Trancriptional repression of the C/EBP and GLUT4 genes in 3T3-L1 adipocytes by Tumor Necrosis Factor-α. J Biols Chem. 1992, 267(19): 13580-13584.
Norman RA, Bogardus C, Ravussin E: Linkage between obesity and marker near the tumor necrosis factor-alpha locus in Pima Indians. J Clin Invest. 1995, 96: 158-162.
Wilson AG, Simons JA, McDowell TL, McDevitt HO: Effects of polymorphism of the human Tumor Necrosis Factor α promoter on trascriptional activation. Proc Natl Acad Sci USA. 1997, 94: 3195-3199. 10.1073/pnas.94.7.3195.
Fernandez-Real JM, Gutierrez C, Ricart W, Casamitjana R, Fernandez-Castaner M, Vendrell J, Richart C, Soler J: The TNF-α gene NCO I polymorphism influences the relationship among insulin resistance, percent body fat, and increased serum leptin levels,. Diabetes. 1997, 46: 1468-1471.
Hoffstedt J, Eriksson P, Hellstrom L, Rossner S, Ryden M, Arner P: Excessive fat accumulation is associated with the TNF-alpha-308 G/A promoter polymorphism in women but not in men. Diabetologia. 2000, 43(1): 117-120. 10.1007/s001250050015.
Day CP, Grove J, Daly AK, Stewart MW, Avery PJ, Walker M: Tumor Necrosis Factor alpha gene promoter polymorphism and decreased insulin resistance. Diabetologia. 1998, 41(4): 430-34. 10.1007/s001250050926.
Koch M, Rett K, Volk A, Maerker E, Haist K, Weisser M, Retting A, Renn W, Haring HU: The tumor necrosis factor alpha -238 G → A and 308 G → A promoter polymorphisms are not associated with insulin sensitivity and insulin secretion in young healthy relatives of type II diabetic patients. Diabetologia. 2000, 43: 181-184. 10.1007/s001250050027.
Da Sliva B, Gaspur SM, Achenbach YH, Schuh TS, Kotla TJ, Liu K, Lowe WL: Lack of association between the G-308A polymorphism of the tumor necrosis factor-alpha gene and the insulin resistance syndrome. J Investig Med. 2000, 48(4): 236-44.
Lee SC, Pu YB, Thomas GN, Lee ZS, Tomlinson B, Cockram CS, Critchley , Chan JC: Tumor necrosis factor alpha gene G-308A polymorphism in the metabolic syndrome. Metabolism. 2000, 49(8): 1021-1024. 10.1053/meta.2000.7704.
Waltson J, Seibert M, Yen CJ, Cheskin LJ, Andersen RF: Tumor necrosis factor-a -238 and -308 polymorphisms do not associate with traits to obesity and insulin-resistance. Diabetes. 1999, 48(10): 2096-2098.
WHO Obesity: Prevention and management of the global epidemic. Report of a WHO consultation on obesity. Geneva (Switzerland):. World Health Organisation. 1997
Kopelman PG: Obesity as a medical problem. Nature. 2000, 404: 635-643.
Segal KR: Lean body mass estimation by bioelectrical impedance analysis: a four site cross-validation study. Am J Clin Nutr. 1988, 47: 7-14.
Rose GA, Blackburn H: Cardiovascular Survey Methods. 1st ed. No. 56. Geneva (Switzerland):. World Health Organization. 1968
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treaches DF, Turner RC: Homeostasis model assessment: insulin resistance and beta cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985, 28: 412-419.
Hotmansgili GS, Shargill NS, Spiegelman BM: Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistamce. Science. 1993, 259: 87-91.
Youd JM, Rattigan S, Clark MG: Acute impairment of insulin-mediated capillary recruitment and glucose uptake in rat skeletal muscle in vivo by TNF-alpha. Diabetes. 2000, 49 (11): 1904-1909.
Kellerer M, Rett K, Renn W, Groop L, Haring HU: Circulating TNF-alpha and leptin levels in offspring of NIDDM patients do not correlate to individual insulin sensitivity. Horm Metab Res. 1996, 28: 733-743.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/2/10/prepub
Acknowledgements
Financial support to this work was provided by the Faculty of Medicine (Research grant ex 60%) of the University of Rome "La Sapienza" and by the Ministry of the University and Scientific Research (MURST grant 9906021327-014, 1999), all to M.G. Baroni, and by the Ministry of Health (grant n. ICS 120.4/RF9911) to M. Arca
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Romeo, S., Sentinelli, F., Capici, F. et al. The G-308A variant of the Tumor Necrosis Factor-α (TNF-α) gene is not associated with obesity, insulin resistance and body fat distribution. BMC Med Genet 2, 10 (2001). https://doi.org/10.1186/1471-2350-2-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-2-10