Abstract
Background
Recent studies suggest that glaucoma is a neurodegenerative disease in which secondary degenerative losses occur after primary insult by raised Intraocular pressure (IOP) or by other associated factors. It has been reported that polymorphisms in the IL1A and IL1B genes are associated with Primary Open Angle Glaucoma (POAG). The purpose of our study was to investigate the role of these polymorphisms in eastern Indian POAG patients.
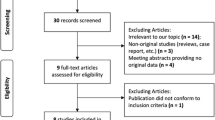
Methods
The study involved 315 unrelated POAG patients, consisting of 116 High Tension Glaucoma (HTG) patients with intra ocular pressure (IOP) > 21 mmHg and 199 non-HTG patients (presenting IOP < 20 mmHg), and 301 healthy controls from eastern India. Genotypes were determined by polymerase chain reaction and restriction digestion for three single nucleotide polymorphisms (SNPs): IL1A (-889C/T; rs1800587), IL1B (-511C/T; rs16944) and IL1B (3953C/T; rs1143634). Haplotype frequency was determined by Haploview 4.1 software. The association of individual SNPs and major haplotypes was evaluated using chi-square statistics. The p-value was corrected for multiple tests by Bonferroni method.
Results
No significant difference was observed in the allele and genotype frequencies for IL1A and IL1B SNPs between total pool of POAG patients and controls. However, on segregating the patient pool to HTG and non-HTG groups, weak association was observed for IL1A polymorphism (-889C/T) where -889C allele was found to portray risk (OR = 1.380; 95% CI = 1.041-1.830; p = 0.025) for non-HTG patients. Similarly, 3953T allele of IL1B polymorphism (+3953C/T) was observed to confer risk to HTG group (OR = 1.561; 95% CI = 1.022-2.385; p = 0.039). On haplotype analysis it was observed that TTC was significantly underrepresented in non-HTG patients (OR = 0.538; 95% CI = 0.356- 0.815; p = 0.003) while TCT haplotype was overrepresented in HTG patients (OR = 1.784; 95% CI = 1.084- 2.937; p = 0.022) compared to control pool. However, after correction for multiple tests by Bonferroni method, an association of only TTC haplotype with non-HTG cases sustained (pcorrected = 0.015) and expected to confer protection.
Conclusion
The study suggests that the genomic region containing the IL1 gene cluster influences the POAG pathogenesis mostly in non-HTG patients in eastern India. A similar study in additional and larger cohorts of patients in other population groups is necessary to further substantiate the observation.
Similar content being viewed by others
Background
Glaucoma is a heterogeneous group of optic neuropathy, characterized by typical visual field loss, often associated with elevated intra ocular pressure. It affects over 60 million people worldwide and is the second largest cause of blindness after cataract [1]. Among different subtypes of glaucoma, Primary Open Angle Glaucoma (POAG) is the most frequently occurring subtype. Till date 25 loci have been implicated in the pathogenesis of POAG with three underlying genes, i.e. Myocilin [2], Optineurin [3] and WDR36 [4]. Recent studies suggest that POAG is caused mainly by genetic predisposition and interaction with other risk factors. It is estimated that 72% of all POAG cases represent the inherited and familial form of the disease that does not show a clear pattern of Mendelian inheritance [5].
POAG results from progressive excavation of the optic disc with corresponding loss of vision by raised Intraocular pressure (IOP) or by other associated factors. However, a substantial number of POAG patients have normal IOP - a condition referred to as normal tension glaucoma (NTG). The main aqueous outflow pathway, controlling IOP, consists of series of endothelial cell-lined channels in the angle of the anterior chamber such as the trabecular meshwork (TM), Schlemm's canal, the collector channels and the episcleral venous system. Accumulation of extraneous materials or cells within the TM, alterations in the cell structure, accelerated TM cell death and collapse of trabecular beams as a result of oxidative stress, vascular dysregulation and aging causes reduced outflow in open angle glaucoma. The cells surviving the sublethal injury tend to mount a protective response involving the expression of new genes [6].
It has been suggested that, in addition to other contributing factors, immune system in the body may have a role in neuro-degeneration in glaucoma [7]. For example, antibody levels against some of the self proteins [8, 9] e.g. anti-NSE antibody [10], antibodies to heat shock proteins [11] and beta 2 glycoproteins [12] have been reported to be significantly higher in glaucoma patients. It has been reported that Interleukin-1 (IL1), an inflammatory cytokine, is involved in ischemic and excitotoxic damage in the retina [6]. Unlike the normal TM cells, glaucomatous cells show endogenous expression of IL1. In vitro experiments show that a stress response specific to the aqueous outflow pathway is activated in the TM cells and controlled by an Interleukin-1 (IL1) autocrine feedback loop through transcription factor NF-kappaB [6]. It has also been suggested that the chronic activation of the stress response in the aqueous outflow pathways might initiate and exacerbate high tension glaucoma (HTG) [6].
Shaftel et al have demonstrated that IL1 protein promotes the development of β-amyloid deposits in Alzheimer's patients [13]. Similar β-amyloid plaques are found in the Retinal Ganglion Cells (RGC) of mouse with experimental glaucoma. Drugs which work to prevent this buildup of the β-amyloid protein in Alzheimer brains can be used to treat glaucoma in animal models [14]. Interestingly, studies conducted on Japanese and German population groups suggest a high frequency of POAG in patients with Alzheimer's disease (AD) [15, 16]. Both AD and glaucoma show similar neuronal degeneration. Moreover, patients with AD shows high level of axonal degeneration of the optic nerve and retinal cell damage, especially ganglion cells [17, 18]. The ε4 allele of APOE has been shown to be significantly over expressed in AD and glaucoma patients, though the contribution remains controversial [19, 20]. Thus glaucoma may be viewed as a neuro-degenerative disorder similar to that of Alzheimer's with common genetic risk factors, mechanisms and pathways.
Several SNPs in the IL1 gene cluster (i.e. IL1A -889C/T; IL1B -511 C/T & 3953C/T) have been reported to be associated with Alzheimer's disease [21, 22]. Recently these SNPs have also been examined for association with POAG through multiple studies in Chinese population [23–27]. Two independent studies by Wang et al [25] and Lin et al [24] have claimed association of POAG with IL1A (-889 C/T) and IL1B (3953 C/T) SNPs, respectively. However, a recent study by How et al [23] reported a lack of association of these polymorphisms with the disease.
In the context of developing information on the potential involvement of the IL1 gene cluster in POAG, we aimed to investigate the role of this genomic region using the well-studied three SNPs (IL1A -889C/T, IL1B -511C/T, IL1B +3953C/T) (Figure 1) in eastern Indian patient cohort.
Location of the SNPs in IL1 gene cluster IL1 alpha , IL1 beta , IL1 receptor antagonist (RN). The promoter regions and coding sequences of the genes are shown in light and dark shaded boxes. The dbSNP refrence SNP ID for each SNP is provided. rs1800587 and rs16944 are located in the promoter (p) region of IL1A and IL1B, respectively while rs1143634 represents a synonymous SNP (F105F) in the coding (c) sequence of IL1B gene. The genomic distances between the SNPs are also shown.
Methods
Selection of study subjects
The patients with POAG and control subjects were recruited for the study from Dristipradip Eye Clinic, Kolkata. Individuals in both the cohorts are inhabitants of Kolkata, West Bengal (eastern India), speak Bengali language, and belong to the Indo-European linguistic group. The patient cohort consisted of 315 POAG patients consisting of 116 patients with presenting IOP > 21 mmHg, considered as high tension glaucoma (HTG) cases and 199 non-HTG patients with presenting IOP < 20 mmHg.
Diagnosis of POAG involved clinical, ocular and systemic examinations. Intraocular pressure (IOP) was measured by Goldmann applanation tonometry (Haag-Streit USA Inc., Mason, OH) followed by pachymetry (Ocuscan A, Alcon, Texas, USA). A Goldman 3-mirror gonioscope (Ocular Instrument, Bellevue, WA) was used to assess the angles of the anterior chamber and the optic disc. The optic disc was also evaluated with a +78D lens. Automated threshold field analysis was done using the Humphrey Field Analyzer II (Carl Zeiss, Dublin, CA). The retinal nerve fiber layer (RNFL) was investigated by Scanning Laser Polarimetry (SLP) with variable corneal compensation technique (GDx-Vcc, Carl Zeiss, Dublin, CA).
An increased intraocular pressure above 21 mmHg, significant cupping of the optic disc (> 0.7) with or without peripapillary changes and the presence of clinically open angle (angle of the anterior chamber) on Gonioscopy raised the suspicion of POAG, which was confirmed by typical reproducible visual field changes, viz. arcuate, Bjerrum, Seidel, paracentral and annular scotoma and nasal steps and Scanning Laser Polarimetry for RNFL analysis (Nerve fibre Indicator > 30). The pre-perimetric cases were identified by RNFL analysis. These patients were categorised as the HTG patients. There was also another group of individuals, the non-HTG patients, who had an IOP less than 20 mmHg on presentation but had cupping of the optic disc, RNFL loss diagnosed by SLP and visual field changes characteristic of POAG. In each case the IOP has been corrected for central corneal thickness (CCT). Thus, the patient pool consisted of 315 adult onset open angle glaucoma cases. The age at diagnosis ranged from 42 to 88 years, with a mean ± standard deviation of 64 ± 10 years. However, individuals with any history of inflammation or ocular trauma (past and present) and ocular hypertension were excluded from this study.
In this study, 301 controls were recruited following the criteria which include: age > 40 years (mean age ± SD, 55.7 ± 10.7 years), without any family history of glaucoma or ocular hypertension, IOP less than 20 mmHg in both eyes in at least last two check ups, CCT greater than 500 μm in both eyes, no visual field defect, normal Scanning Laser Polarimeter parameters (i.e. a good yellowish bow type scan pattern, deviation map within normal limit, a good double hump pattern in conduction map, TSNIT parameters within normal limit, Nerve Fibre Indicator < 30 for both eyes), cup discs were physiological and similar in both eyes, cup to disc ratio < 0.2, no defect in disc rim or margin and no sphincter haemorrhage around the disc. Individuals with high myopia, diabetes and hypertension were excluded from the control group.
Collection of blood samples and genomic DNA preparation
Eight milliliters of peripheral blood was collected with EDTA from the POAG patients and normal individuals with their written consent. Genomic DNA was prepared from fresh whole blood using the PAX gene blood DNA isolation kit (Qiagen, Hilden, Germany). The DNA was dissolved in TE (10 mM Tris-HCl, 1 mM EDTA, pH 8.0). The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board.
Genotyping
Genotyping was done by polymerase chain reaction and restriction digestion (PCR-RFLP). All the PCR reaction was carried out in 20 μl reaction volume using 80 ng of total genomic DNA with Ex Prime Taq Premix (GeNet Bio, South Korea) with specific primers for IL1A (-889C/T), IL1B (-511C/T) and IL1B (3953C/T) (Integrated DNA Technologies, Coralville, Iowa, USA) as described previously [25, 27]. The PCR conditions were as follows: an initial denaturation at 95°C for 4 mins followed by 30 cycles of 30 secs of denaturation at 95°C, 30 secs of annealing at 58-60°C and 30 secs of extension at 72°C, with a final extension at 72°C for 4 mins. All the PCR products were detected on a 6% polyacrylamide gel with ethidium-bromide staining. The PCR products for both IL1A and IL1B were subjected to restriction digestion with appropriate enzymes from NEB (New England Biolabs Inc. Beverly, MA) for 3 hrs at optimum temperatures as described previously [25, 27]. The digested products were analyzed on a 6% polyacrylamide gel and the alleles were scored as described in earlier studies [25, 27].
Bioinformatics and Statistical analysis
Haplotypes and their frequencies were determined for comparison between patients and controls using Haploview 4.1 software http://www.broad.mit.edu/mpg/haploview[28]. The allele frequencies of the SNP and haplotypes were compared between patients and controls using chi square test. The p-values were corrected for multiple testing by Bonferroni method.
Results
Lack of association between IL1A and IL1Bpolymorphisms and POAG
On genotyping 315 patients for three selected SNPs, IL1A (-889C/T), IL1B (-511C/T) and IL1B (3953C/T), no significant association was observed with the POAG. However, on further sub-dividing the patients according to their presenting IOP, i.e. IOP > 21 mmHg (HTG) and the IOP < 20 mmHg (non-HTG), marginal associations were observed in non-HTG patient group and HTG patient group with IL1A (-889C) allele (OR = 1.380; 95% CI = 1.041- 1.830; p = 0.025) and IL1B (+3953T) allele (OR = 1.561; 95% CI = 1.022- 2.385; p = 0.039), respectively. However, the observed association was nullified after Bonferroni correction for multiple tests (Table 1). Therefore, our data did not unequivocally suggest having an association with the three SNPs examined.
IL1haplotype distribution among patient and control group
Haplotype analysis revealed presence of total eight haplotypes in both patients and controls. No significant LD was observed between the three SNPs genotyped (Figure 2). Among the eight haplotypes, five (CTC, CCC, TTC, TCT, TCC) represented the majority of chromosomes (~95%) in both POAG patients and controls (Table 2). The remaining three haplotypes (TTT, CTT, CCT) were in much lower frequency (i.e. up to max. 3.5%) and not considered for further analysis as predicted number of patients and controls carrying these haplotypes were too small for carrying out any association study. Thus for haplotypes five tests were considered for Bonferroni correction. Among the five major haplotypes TTC haplotype was significantly under-represented in non-HTG patient group (OR = 0.538.; 95% CI = 0.356-0.815; p = 0.003) as well as the entire POAG (OR = 0.697; 95% CI = 0.498-0.976; p = 0.036) group compared to the control group (Table 2). However after correction for multiple tests by Bonferroni method, the association for POAG group did not sustain. Thus, it appears that the lower p-value for POAG is contributed entirely due to the association with the non-HTG group since no significant association of TTC haplotype was observed with HTG patient group. On the other hand, TCT haplotype was found to be over-represented in HTG patient group (OR = 1.784; 95% CI = 1.084-2.937; p = 0.022) but the association was nullified after correction for multiple tests (Table 2).
LD structure between the three SNPs in POAG patients and controls. No significant LD was observed between the three SNPs. The LD value was calculated using Haploview 4.1 software. The values in the boxes are the r-squared pairwise LD values given by the software. The standard r-squared color scheme is followed here i.e the extent of LD increases with darker shades.
In an attempt to examine whether the effect of the TTC haplotypes in non-HTG patients is related to age, we divided these patients into two groups: (i) up to 50 years, and (ii) above 50 years. We observed that only the patients above 50 years TTC haplotype appeared to have a protective effect (OR = 0.477; 95% CI = 0.287- 0.792; p = 0.004) (Table 3) even after Bonferroni correction.
Discussion
Glaucoma being a complex disease, understanding of the molecular mechanism underlying its pathogenesis is limited. In addition to the identified genetic loci linked to POAG, other genetic factors e.g. OPA1, Apolipoprotein E, CYP1B1, E-cahderin, OPTC have been reported to elevate the risk of retinal degeneration characteristic of glaucoma [20, 29–32]. However, the interplay of genetic factors and environmental cues causing POAG pathogenesis remains almost unexplored.
The association of the immune system with glaucoma has seemingly conflicting aspects as neuroprotective or neurodestructive. T-cell-mediated immune response may initially be beneficial to limit neurodegeneration. However, a failure to properly control aberrant, stress-induced immune response likely converts the protective immunity to an autoimmune neurodegenerative process that can facilitate the progression of neurodegeneration in some glaucoma patients specially in Normal Tension Glaucoma (NTG) cases [8]. Proliferating cytokines, such as IL1 has been reported [6] to have a role in the immune response in glaucoma patients. The IL1 induces the expression and processing of β-amyloid expression protein (APP), resulting in the increased production of secreted APP and further activation of microglia and overexpression of IL1 [33]. Studies show a higher expression of such microglial cells in glaucomatous optic nerve heads, which may play a role in neurodegeneration [8]. IL1 has been shown to promote optic nerve damage by increasing the synthesis of matrix mellanoproteinase-9 (MMP) in glaucoma mouse model, which mimics some aspects of glaucoma [34, 35]. IL1 has also been reported to be involved in increased generation of reactive oxygen species (ROS) [36] and nitric oxide synthesis [37], implicated in retinal ganglion cell damage leading to neurodegeneration.
Previous studies [6, 24, 25] suggest that single nucleotide polymorphisms (SNPs) in IL1 gene cluster could influence glaucoma pathogenesis. Such studies have been carried out so far exclusively in Chinese population groups. For example, Wang et al [25] reported that the IL1A (-889T) allele is significantly over-represented in HTG patients with an IOP > 21 mmHg but not with NTG cases. Lin et al [24] reported a possible association of the IL1B (+3953T) polymorphism with POAG in a study carried out in a smaller number of patients which could not be further replicated in recent studies by Wang et al [27] in NTG patients and by How et al in POAG [23] patients (Table 4). Such variation might be due to overall genome of the population groups under study. However, lack of information about the ethnicity and interrelationship between these populations [23–27] limits further analysis of the data.
We observed weak association of IL1A (-889C) allele and IL1B (+3953T) allele with non-HTG and HTG patient groups respectively but these associations, if any, did not sustain after Bonferroni correction for multiple tests. However, haplotype analysis based on these 3 SNPs examined, suggests one of the haplotype (TTC) provides protection for non-HTG patients above 50 years of age. This indicates that age also has an effect on this association. It is possible that many patients in our cohort with IOP < 20 mmHg represent NTG but we prefer to describe those as non-HTG cases in the absence of rigorous monitoring of diurnal variations of IOP in all the patients. It appears that apparent association of the IL1 haplotype with entire POAG patient group is due to high attributable protection of TTC haplotype only for non-HTG cases.
It would be a worthwhile effort to examine association of these haplotypes in other population groups of India. A recent study carried out by the Indian Genome Variation Consortium shows that the Indian population is divided into 4 distinct linguistic groups - Indo-European, Austro Asiatic, Tibeto-Burman and Dravidian, and there exists high degree inter-population variance in allele frequencies due to their genetic diversity [38]. Among the previous studies in Chinese population, How et al reported lack of association of the haplotypes with POAG patients [23]. Lack of required information in other pervious publications [23–27] prevented us from attempting a meta-analysis of the data to examine the effect of these haplotypes on glaucoma pathogenesis.
It has been reported that IL1A (-889T) allele upregulates transcription of the gene and thus increases the level of the gene product in Alzheimer's disease [39] as well as the plasma level of IL1B [40]. IL1B (+3953T) allele is known to increase the level of IL1B production at least by four fold compared to IL1B (+3953C) allele. It is possible that IL1A (-889C) allele and IL1B (+3953T) allele influence the risk of non-HTG and HTG respectively by altering the expression of the respective proteins [41]. However, since the genomic region represented by specific haplotype (and not just this SNP) is associated with non-HTG cases, it appears likely that other yet unidentified variant might be influencing the course of pathogenesis. We plan to explore the question further by fine mapping the genomic region with additional SNPs and then finding the suspect variant (if any) by deep sequencing the minimum critical region. It is also certainly very important that such studies are replicated in larger and more importantly in additional glaucoma patient cohorts to examine whether the IL1 locus has a major effect on glaucoma pathogenesis. Interestingly, the IL1 gene cluster (2q13) resides in close proximity to one of the POAG loci (GLC1B at 2cen-2q13), also linked to NTG cases [42]. It would be interesting to explore whether there is more than one genomic region associated with POAG in this segment of chromosome 2. Finally, understanding the role of IL 1 in glaucoma pathogenesis and identification of predisposing variants might pave the way for better management of the disease through prevention and treatment as appropriate.
Conclusion
Our data suggest that IL1A and IL1B SNPs studied are not associated with POAG. However, haplotype constructed with these SNPs are associated with POAG, specifically in non-HTG patients above 50 years of age, which might be due to additional variants located in the genomic region examined. The observation needs to be further vindicated by similar studies in larger and additional cohort of POAG patients.
References
Quigley HA, Broman AT: The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006, 90 (3): 262-267. 10.1136/bjo.2005.081224.
Stone EM, Fingert JH, Alward WL, Nguyen TD, Polansky JR, Sunden SL, Nishimura D, Clark AF, Nystuen A, Nichols BE, et al: Identification of a gene that causes primary open angle glaucoma. Science (New York, NY). 1997, 275 (5300): 668-670.
Rezaie T, Child A, Hitchings R, Brice G, Miller L, Coca-Prados M, Heon E, Krupin T, Ritch R, Kreutzer D, et al: Adult-onset primary open-angle glaucoma caused by mutations in optineurin. Science. 2002, 295 (5557): 1077-1079. 10.1126/science.1066901.
Monemi S, Spaeth G, DaSilva A, Popinchalk S, Ilitchev E, Liebmann J, Ritch R, Heon E, Crick RP, Child A, et al: Identification of a novel adult-onset primary open-angle glaucoma (POAG) gene on 5q22.1. Hum Mol Genet. 2005, 14 (6): 725-733. 10.1093/hmg/ddi068.
Gong G, Kosoko-Lasaki S, Haynatzki G, Lynch HT, Lynch JA, Wilson MR: Inherited, familial and sporadic primary open-angle glaucoma. J Natl Med Assoc. 2007, 99 (5): 559-563.
Wang N, Chintala SK, Fini ME, Schuman JS: Activation of a tissue-specific stress response in the aqueous outflow pathway of the eye defines the glaucoma disease phenotype. Nat Med. 2001, 7 (3): 304-309. 10.1038/85446.
Halpern DL, Grosskreutz CL: Glaucomatous optic neuropathy: mechanisms of disease. Ophthalmol Clin North Am. 2002, 15 (1): 61-68. 10.1016/S0896-1549(01)00012-8.
Tezel G, Wax MB: The immune system and glaucoma. Curr Opin Ophthalmol. 2004, 15 (2): 80-84. 10.1097/00055735-200404000-00003.
Tezel G, Yang J, Wax MB: Heat shock proteins, immunity and glaucoma. Brain Res Bull. 2004, 62 (6): 473-480. 10.1016/S0361-9230(03)00074-1.
Ikeda Y, Maruyama I, Nakazawa M, Ohguro H: Clinical significance of serum antibody against neuron-specific enolase in glaucoma patients. Jpn J Ophthalmol. 2002, 46 (1): 13-17. 10.1016/S0021-5155(01)00455-5.
Tezel G, Seigel GM, Wax MB: Autoantibodies to small heat shock proteins in glaucoma. Invest Ophthalmol Vis Sci. 1998, 39 (12): 2277-2287.
Latalska M, Gerkowicz M, Kosior-Jarecka E, Koziol-Montewka M, Pietras-Trzpiel M: [Serum and aqueous humor antibodies to beta-2 glycoprotein I in patients with glaucoma and cataract]. Klin Oczna. 2004, 106 (1-2 Suppl): 162-163.
Shaftel SS, Griffin WS, O'Banion MK: The role of interleukin-1 in neuroinflammation and Alzheimer disease: an evolving perspective. J Neuroinflammation. 2008, 5: 7-10.1186/1742-2094-5-7.
Guo L, Salt TE, Luong V, Wood N, Cheung W, Maass A, Ferrari G, Russo-Marie F, Sillito AM, Cheetham ME, et al: Targeting amyloid-beta in glaucoma treatment. Proc Natl Acad Sci USA. 2007, 104 (33): 13444-13449. 10.1073/pnas.0703707104.
Bayer AU, Ferrari F, Erb C: High occurrence rate of glaucoma among patients with Alzheimer's disease. European neurology. 2002, 47 (3): 165-168. 10.1159/000047976.
Tamura H, Kawakami H, Kanamoto T, Kato T, Yokoyama T, Sasaki K, Izumi Y, Matsumoto M, Mishima HK: High frequency of open-angle glaucoma in Japanese patients with Alzheimer's disease. J Neurol Sci. 2006, 246 (1-2): 79-83. 10.1016/j.jns.2006.02.009.
Hinton DR, Sadun AA, Blanks JC, Miller CA: Optic-nerve degeneration in Alzheimer's disease. The New England journal of medicine. 1986, 315 (8): 485-487. 10.1056/NEJM198608213150804.
Weinreb RN, Khaw PT: Primary open-angle glaucoma. Lancet. 2004, 363 (9422): 1711-1720. 10.1016/S0140-6736(04)16257-0.
Ressiniotis T, Griffiths PG, Birch M, Keers S, Chinnery PF: The role of apolipoprotein E gene polymorphisms in primary open-angle glaucoma. Archives of ophthalmology. 2004, 122 (2): 258-261. 10.1001/archopht.122.2.258.
Vickers JC, Craig JE, Stankovich J, McCormack GH, West AK, Dickinson JL, McCartney PJ, Coote MA, Healey DL, Mackey DA: The apolipoprotein epsilon4 gene is associated with elevated risk of normal tension glaucoma. Mol Vis. 2002, 8: 389-393.
Du Y, Dodel RC, Eastwood BJ, Bales KR, Gao F, Lohmuller F, Muller U, Kurz A, Zimmer R, Evans RM, et al: Association of an interleukin 1 alpha polymorphism with Alzheimer's disease. Neurology. 2000, 55 (4): 480-483.
Nicoll JA, Mrak RE, Graham DI, Stewart J, Wilcock G, MacGowan S, Esiri MM, Murray LS, Dewar D, Love S, et al: Association of interleukin-1 gene polymorphisms with Alzheimer's disease. Ann Neurol. 2000, 47 (3): 365-368. 10.1002/1531-8249(200003)47:3<365::AID-ANA13>3.0.CO;2-G.
How AC, Aung T, Chew X, Yong VH, Lim MC, Lee KY, Toh JY, Li Y, Liu J, Vithana EN: Lack of association between interleukin-1 gene cluster polymorphisms and glaucoma in Chinese subjects. Invest Ophthalmol Vis Sci. 2007, 48 (5): 2123-2126. 10.1167/iovs.06-1213.
Lin HJ, Tsai SC, Tsai FJ, Chen WC, Tsai JJ, Hsu CD: Association of interleukin 1beta and receptor antagonist gene polymorphisms with primary open-angle glaucoma. Ophthalmologica. 2003, 217 (5): 358-364. 10.1159/000071352.
Wang CY, Shen YC, Lo FY, Su CH, Lee SH, Lin KH, Tsai HY, Kuo NW, Fan SS: Polymorphism in the IL-1alpha (-889) locus associated with elevated risk of primary open angle glaucoma. Mol Vis. 2006, 12: 1380-1385.
Wang CY, Shen YC, Lo FY, Su CH, Lee SH, Tsai HY, Fan SS: Normal tension glaucoma is not associated with the interleukin -1alpha (-889) genetic polymorphism. J Glaucoma. 2007, 16 (2): 230-233. 10.1097/IJG.0b013e3180300818.
Wang CY, Shen YC, Su CH, Lo FY, Lee SH, Tsai HY, Fan SS: Investigation of the association between interleukin-1beta polymorphism and normal tension glaucoma. Mol Vis. 2007, 13: 719-723.
Barrett JC, Fry B, Maller J, Daly MJ: Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics (Oxford, England). 2005, 21 (2): 263-265. 10.1093/bioinformatics/bth457.
Acharya M, Mookherjee S, Bhattacharjee A, Bandyopadhyay AK, Daulat Thakur SK, Bhaduri G, Sen A, Ray K: Primary role of CYP1B1 in Indian juvenile-onset POAG patients. Mol Vis. 2006, 12: 399-404.
Acharya M, Mookherjee S, Bhattacharjee A, Thakur SK, Bandyopadhyay AK, Sen A, Chakrabarti S, Ray K: Evaluation of the OPTC gene in primary open angle glaucoma: functional significance of a silent change. BMC Mol Biol. 2007, 8 (1): 21-10.1186/1471-2199-8-21.
Bhattacharjee A, Banerjee D, Mookherjee S, Acharya M, Banerjee A, Ray A, Sen A, Variation Consortium TI, Ray K: Leu432Val polymorphism in CYP1B1 as a susceptible factor towards predisposition to primary open-angle glaucoma. Mol Vis. 2008, 14: 841-850.
Lin HJ, Tsai FJ, Hung P, Chen WC, Chen HY, Fan SS, Tsai SW: Association of E-cadherin gene 3'-UTR C/T polymorphism with primary open angle glaucoma. Ophthalmic research. 2006, 38 (1): 44-48. 10.1159/000089523.
Barger SW, Harmon AD: Microglial activation by Alzheimer amyloid precursor protein and modulation by apolipoprotein E. Nature. 1997, 388 (6645): 878-881. 10.1038/42257.
Chintala SK, Zhang X, Austin JS, Fini ME: Deficiency in matrix metalloproteinase gelatinase B (MMP-9) protects against retinal ganglion cell death after optic nerve ligation. The Journal of biological chemistry. 2002, 277 (49): 47461-47468. 10.1074/jbc.M204824200.
Zhang X, Chintala SK: Influence of interleukin-1 beta induction and mitogen-activated protein kinase phosphorylation on optic nerve ligation-induced matrix metalloproteinase-9 activation in the retina. Experimental eye research. 2004, 78 (4): 849-860. 10.1016/j.exer.2003.10.018.
Levin LA: Direct and indirect approaches to neuroprotective therapy of glaucomatous optic neuropathy. Survey of ophthalmology. 1999, 43 (Suppl 1): S98-101. 10.1016/S0039-6257(99)00027-2.
Neufeld AH, Sawada A, Becker B: Inhibition of nitric-oxide synthase 2 by aminoguanidine provides neuroprotection of retinal ganglion cells in a rat model of chronic glaucoma. Proceedings of the National Academy of Sciences of the United States of America. 1999, 96 (17): 9944-9948. 10.1073/pnas.96.17.9944.
Genetic landscape of the people of India: a canvas for disease gene exploration. Journal of genetics. 2008, 87 (1): 3-20. 10.1007/s12041-008-0002-x.
Dominici R, Cattaneo M, Malferrari G, Archi D, Mariani C, Grimaldi LM, Biunno I: Cloning and functional analysis of the allelic polymorphism in the transcription regulatory region of interleukin-1 alpha. Immunogenetics. 2002, 54 (2): 82-86. 10.1007/s00251-002-0445-9.
Hulkkonen J, Laippala P, Hurme M: A rare allele combination of the interleukin-1 gene complex is associated with high interleukin-1 beta plasma levels in healthy individuals. Eur Cytokine Netw. 2000, 11 (2): 251-255.
Hall SK, Perregaux DG, Gabel CA, Woodworth T, Durham LK, Huizinga TW, Breedveld FC, Seymour AB: Correlation of polymorphic variation in the promoter region of the interleukin-1 beta gene with secretion of interleukin-1 beta protein. Arthritis and rheumatism. 2004, 50 (6): 1976-1983. 10.1002/art.20310.
Stoilova D, Child A, Trifan OC, Crick RP, Coakes RL, Sarfarazi M: Localization of a locus (GLC1B) for adult-onset primary open angle glaucoma to the 2cen-q13 region. Genomics. 1996, 36 (1): 142-150. 10.1006/geno.1996.0434.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/11/99/prepub
Acknowledgements
The authors are thankful to the patients who participated in this study. The Council of Scientific and Industrial Research, Govt. of India supported the study through funding grants (MLP-0016 and SIP-007) and pre-doctoral fellowships to SM, DB, SC. AB is supported by a post-doctoral fellowship from Department of Biotechnology, India. We are also thankful to the Mr. Kausik Bhattacharya, who worked as summer trainee in our lab, for his excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SM, DB, SC and AB carried out the wet lab experiments and also involved in data analysis. SM, DB has prepared the manuscript. IM gave intellectual inputs in statistical analysis of the data. AS led the group of ophthalmologist in Dristi Pradip Eye clinic and selected the patient and control samples used in the study. KR conceived the study, led the group in designing experimental strategies and provided intellectual input for giving final shape of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mookherjee, S., Banerjee, D., Chakraborty, S. et al. Association of IL1A and IL1B loci with primary open angle glaucoma. BMC Med Genet 11, 99 (2010). https://doi.org/10.1186/1471-2350-11-99
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-11-99