Abstract
Background
Heme oxygenase-1 is an inducible cytoprotective enzyme which handles oxidative stress by generating anti-oxidant bilirubin and vasodilating carbon monoxide. A (GT)n dinucleotide repeat and a -413A>T single nucleotide polymorphism have been reported in the promoter region of HMOX1 to both influence the occurrence of coronary artery disease and myocardial infarction. We sought to validate these observations in persons scheduled for coronary angiography.
Methods
We included 3219 subjects in the current analysis, 2526 with CAD including a subgroup of CAD and MI (n = 1339) and 693 controls. Coronary status was determined by coronary angiography. Risk factors and biochemical parameters (bilirubin, iron, LDL-C, HDL-C, and triglycerides) were determined by standard procedures. The dinucleotide repeat was analysed by PCR and subsequent sizing by capillary electrophoresis, the -413A>T polymorphism by PCR and RFLP.
Results
In the LURIC study the allele frequency for the -413A>T polymorphism is A = 0,589 and T = 0,411. The (GT)n repeats spread between 14 and 39 repeats with 22 (19.9%) and 29 (47.1%) as the two most common alleles. We found neither an association of the genotypes or allelic frequencies with any of the biochemical parameters nor with CAD or previous MI.
Conclusion
Although an association of these polymorphisms with the appearance of CAD and MI have been published before, our results strongly argue against a relevant role of the (GT)n repeat or the -413A>T SNP in the HMOX1 promoter in CAD or MI.
Similar content being viewed by others
Background
Low-grade inflammation and oxidation are important mechanisms involved in the complex pathological process of atherogenesis [1]. Several cardiovascular risk factors, such as smoking, type 2 diabetes, hypertension, and dyslipidemia, increase the production of reactive oxygen species (ROS) in the arterial wall. In response to oxidative stress the expression of endogenous stress proteins including heme oxygenase (HO) is increased. HO is a rate-limiting enzyme in the degradation of heme to biliverdin releasing equimolar quantities of free iron and carbon monoxide, a potent anti-apoptotic and proliferation promoting compound [2]. The reduction of biliverdin by biliverdin reductase leads to the generation of bilirubin, a potent endogenous antioxidant [3, 4]. Recently, it could be shown that bilirubin has an antiproliferative effect on vascular smooth muscle cells, too [5].
In humans two isoforms of heme oxygenase, HO-1 and HO-2, have been described. HO-1 is the inducible isoform, which is up-regulated by various exogenous stimuli, such as oxidative stress, hypoxia, or its own substrate heme [6, 7]. The enzyme is expressed in atherosclerotic lesions, vascular smooth muscle cells, endothelial cells, and several other tissues [8]. There are several lines of evidence that HO-1 has protective properties in the cardiovascular system. HO-1 provides protection against cellular proliferation and lesion formation after arterial injury [9]. In rats vascular remodelling following balloon injury was beneficially influenced after induction of HO-1 [10]. In addition, thrombus formation was suppressed by vascular HO-1 [11] and HO-1 inhibited vascular smooth muscle cell proliferation in vitro [12]. Overexpression of HO-1 in endothelial cells has not only improved the ability of these cells to resist oxidative stress but also enhances cell growth [13]. Thus, the up regulation of HO-1 in atherosclerotic lesions might be a physiological reaction to prevent atherosclerotic progression [14].
Two different polymorphisms in the HMOX1 promoter, a (GT) dinucleotide repeat and the -413A>T (rs2071746) single nucleotide polymorphism (SNP) are thought to be involved in the pathogenesis of cardiovascular disease by modulating the expression of HO-1 [15–24].
We investigated whether these variants are associated with angiographic coronary artery disease (CAD), myocardial infarction (MI), or mortality in a large cohort of individuals who had previously undergone coronary angiography.
Methods
Study design and participants
The Ludwigshafen Risk and Cardiovascular Health (LURIC) study includes consecutive white patients hospitalized for coronary angiography between July 1997 and January 2000. The study was approved by the ethics review committee at the "Landesärztekammer Rheinland-Pfalz" (Mainz, Germany). Written informed consent was obtained from each of the participants.
A detailed description of LURIC has been published [25]. Diabetes mellitus was diagnosed according to the criteria of the American Diabetes Association (ADA) [26]. Further, individuals with a history of diabetes or treatment with oral antidiabetics or insulin were considered diabetic. CAD has been defined angiographically using the maximum luminal narrowing estimated by visual analysis. Clinically relevant CAD was defined as the presence of a visible luminal narrowing (≥ 20% stenosis) in at least one of 15 coronary segments according to a classification of the American Heart Association [27]. We also provisionally defined CAD as the presence of at least one stenosis of 50 percent or more, again classifying individuals with stenosis less than 20 percent as controls. Previous MI was diagnosed if there was a conclusive positive history of myocardial infarction or if patients presented ST elevation. Hypertension was diagnosed if the systolic and/or diastolic blood pressure exceeded 140 and/or 90 mm Hg or if there was a history of hypertension, evident through the use of antihypertensive drugs. Individuals with either HDL cholesterol (HDL-C) <40 mg/dl or LDL cholesterol (LDL-C) >160 mg/dl or triglycerides >200 mg/dl were considered dyslipidemic.
We included 3219 patients in this study; all of them underwent coronary angiography. To rule out racial differences as a confounding factor the LURIC study was designed to recruit probands with German ancestry only. We did not include family members of the patients for this study.
Information on vital status was obtained from local person registries. No patients were lost to follow-up. Amongst the subjects included in this examination, 752 deaths (23.4%) had occurred during a median observation time of 7.97 years. Cardiovascular death (n = 473) included the following categories: sudden death, fatal myocardial infarction, death due to congestive heart failure, death immediately following intervention to treat CAD, fatal stroke and other causes of death due to CAD. All clinical assessments were made blinded to the knowledge of HMOX1 genotype.
Laboratory Procedures
Fasting blood samples were obtained by venipuncture in the early morning. Levels of cholesterol, triglycerides, bilirubin, iron, transferrin, and ferritin were determined with common laboratory procedures [25]. LDL-C and HDL-C were measured after separating lipoproteins with a combined ultracentrifugation-precipitation method.
Analysis of the HO-1 promoter variants
Genomic DNA was prepared from EDTA-anticoagulated peripheral blood by using a standard salting-out procedure. Genotypes of the -413A>T polymorphism were determined using polymerase chain reaction with a mismatched 5' primer to obtain an allele specific restriction site for HindIII in the amplicon (sense 5'-gtt cct gat gtt gcc cac caagct-3'; reverse 5'-tct gag aag ctg cag gct ctg-3'). In case of the A genotype a fragment of 163 bp and in case of the T genotype two fragments of 140 bp + 23 bp were obtained. To validate the method three samples of each genotype were sequenced; as internal control 184 DNA samples, blinded distributed within the samples, were genotyped twice. To confirm genotype assignment, the restriction fragments were analyzed independently by two scientists on two separate occasions. The results were scored blinded as to case-control status.
The microsatellite polymorphism was amplified according to the protocol described by Kaneda et al. [18] and analyzed on a MegaBASE500 sequencer. As controls two cloned alleles (22 & 30 repeats) were run in parallel. The respective sizes of the (GT)n repeats were each calculated using Genetic Profiler software (Amersham).
Statistics
Clinical and anthropometric characteristics were compared between CAD patients and controls by analysis of variance (ANOVA) or logistic regression. Covariable adjustments were carried out as indicated. Associations between categorical variables were examined by chi-square testing or logistic regression analysis. The frequencies of the HMOX1 alleles and genotypes in CAD+ and CAD- as well as in MI+ and MI- subjects were obtained by direct count and the deviation from Hardy-Weinberg equilibrium was examined by the chi-square test. In models assuming a co-dominant (additive) effect of the A-allele of the HMOX1 gene, the genotypes AA, AT and TT were coded as 0, 1, and 2, respectively. Genotypes were either treated as interval-scaled or categorical variables, the AA genotype being considered as the reference category in the latter case. When assuming a dominant effect, genotype TT was coded as 0, and AT and AA combined as 1, whereas assuming a recessive effect, genotypes TT and AT were coded as 0, and AA as 1. In a similar way the repeat classes (cut off S<25, L= 25, or S<27, L= 27, respectively) and both haplotypes (22-T, 29-A) were analyzed. To examine the relationship of the genotypes with total mortality and mortality from cardiovascular causes, we calculated hazard ratios and 95 percent confidence intervals (95% CI) using the Cox proportional hazards model. The criterion for statistical significance was p < 0.05. The SPSS statistical package (SPSS Inc., Chicago, IL, USA, version 15.0 for Windows XP) was used for all statistical analyses.
Results
Study participants – Baseline Characteristics
We included 3219 subjects in the current analysis. 693 were control subjects without CAD, 2526 were diagnosed CAD-positive by angiography and from these 1339 had suffered and survived a MI in the past. Compared to the control group, patients with CAD and with a former MI were significantly older, current or past smoker and type 2 diabetes were more prevalent (Table 1). Systemic Hypertension was only significantly higher in the CAD group compared to the control group, but not in the CAD and MI group. No significant differences were found for BMI.
CAD and CAD plus MI patients had higher fasting glucose, lower HDL-C, lower bilirubin serum levels and lower iron serum concentrations. After adjustment for use of lipid lowering drugs CAD patients had – compared to the control group – higher LDL-C (p < 0.002) and higher triglycerides (p < 0.012). No significant difference was found for the two last mentioned parameters for the CAD plus MI group (Table 1).
With regard to the tested biochemical parameters there were no significant differences between the CAD and the CAD plus MI patients.
-413A>T polymorphism
The overall allelic distribution in the LURIC study is A = 0,589 and T = 0,411. The genotypes were in Hardy-Weinberg equilibrium in both the CAD and the control group. There was no significant difference in the frequency of genotypes between CAD patients and controls (Table 2). Using logistic regression analysis to examine a possible association between the HMOX1 polymorphism and CAD we found no evidence for this association, regardless of whether or not we adjusted for conventional cardiovascular risk factors like age, gender, smoking, type 2 diabetes, dyslipidemia and hypertension (Table 3). Very similar results were obtained when we compared the -413A>T genotypes in patients with previous MI versus controls or CAD patients without MI (data not shown).
(GT)nrepeat
In the study group the (GT)n repeats spread between 14 and 39 repeats with 22 and 29 as the two most common alleles, which represents a shift of minus one repeat in comparison to published data. Although we used cloned and sequenced alleles as controls we cannot exclude that this is a methodical mistake.
According to the classification of Funk et al. [28], we chose a cut-off at 25 and in a second model according to Kaneda et al. [18] a cut-off at 27 repeats: class S (small) < 25 or 27 repeats and class L (large) ≥ 25 or 27 repeats, respectively. Similar to the results presented for the -413A>T polymorphism we found no significant differences in the distribution of the repeats (Table 2). In a logistic regression analysis no association could be found with CAD (Table 3) or MI (data not shown), irrespective of the chosen cut-off.
Chen et al. [17] described an association of the L allele (≥ 32 repeats) with CAD in type 2 diabetic patients. In a subgroup analysis of type 2 diabetic patients (n = 1035) we could not confirm this observation, the L alleles (≥ 32 repeats) were evenly distributed between cases and controls (allele frequency 5.2% versus 5.5%, p = 0.619).
Haplotypes
The small repeats, e.g. 22 – the most frequent ones in the class S alleles – are associated with the T allele, while the large repeats, e.g. 29, with the exception of very large repeats (34–38), are associated with the A allele (pairwise LD r2 = 0,63). Analysis of the two most common haplotypes, 22-T (19.9%) and 29-A (47.1%), did not generate new information with regard to cardiovascular disease; there was still no association with CAD or MI (data not shown).
We obtained similar results by using a stenosis of at least 50% in the coronary segments as the criterion for CAD in all of the above mentioned analysis (data not shown).
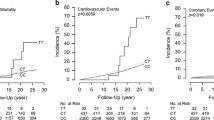
HMOX1 variants, all cause and cardiovascular mortality
Amongst the 3219 subjects included in this examination, 752 deaths (23.4%) had occurred during a median observation time of 7.97 years, from which 473 (14.7%) died from cardiovascular causes. Regardless whether or not we adjusted for age and gender, there was neither an association of the genetic markers of HMOX1 with mortality from all causes nor with cardiovascular mortality (Table 4).
HMOX1 variants and biochemical parameters
Products of the enzymatic action of HO-1 are iron and biliverdin, which in turn is converted to bilirubin. If promoter variants influence the systemic expression of HO-1 it might be possible to detect an association between HMOX1 genotypes and serum levels. However, we were not able to find any significant association between HMOX1 genotypes and serum levels of bilirubin (e.g. -413A>T and bilirubin (μmol/L): AA 10.78 ± 6.50, AT 11.12 ± 6.67, and TT 10.95 ± 5.99, means ± standard deviations) or iron, even after adjustment for age, gender, or other cardiovascular risk factors.
Previously a correlation of lipid parameters and the (GT)n repeat has been published [29]. To avoid a confounding by lipid lowering drugs we analyzed only those patients (n = 1648) not receiving lipid lowering therapy. We found a significant increase of HDL-C (mmol/L) only for homozygote carriers of the 29-A haplotype (0 – 1.02 ± 0.28, 1 – 1.03 ± 0.29, 2 – 1.08 ± 0.05, means ± standard deviations), which was robust against adjustment for age and gender (p = 0.006), but no association with LDL-C or triglycerides.
Discussion
The presented data show in a prospective case-control study of more than 3000 participants that neither the (GT)n dinucleotide repeat nor the -413A>T polymorphism in the HMOX1 promoter are associated with angiographic CAD, MI or survival rate in Caucasians undergoing coronary angiography.
The functional relevance of both variants in the HMOX1 promoter is still under debate. Yamada et al. described a higher response of reporter gene constructs with short (GT) repeats to H202 exposure in A549 and Hep3B cell [30]. Similar results were obtained by analyzing HO-1 mRNA and activity in lymphoblastoid cell lines from subjects homozygous for small or long repeats [31] or by analyzing the HO-1 expression in mononuclear cells from patients who underwent coronary angiography [24]. In all studies the short repeats were associated with a higher expression rate. However, Ono et al. [21, 32] showed by in vitro experiments with reporter gene constructs that the length of the (GT)n repeat did not influence the activity of the HMOX1 promoter in bovine aortic endothelial cells. They found that – instead of the (GT)n repeat – the responsible element was an A>T exchange at position -413, giving rise to a 4-fold increase of activity. Therefore further experiments are required to clear the functionality of these variants.
Irrespective of the unclear functional role there are several reports suggesting a role of the (GT)n repeat in the HMOX1 promoter in cardiovascular disease. Asian patients with a lower number of repeats were less susceptible to pulmonary emphysema and coronary artery disease [17, 18, 30]. Further, a lower number of repeats was associated with a lower restenosis rate after balloon dilatation in the femoral artery [15] suggesting a protective effect on restenosis. In support of this hypothesis, long repeats have been related to in-stent-restenosis after percutanous coronary intervention [20, 22]. However, data of Wijpkema et al. [33], who followed a group of about 3.000 patients for 10 months after successful percutanous coronary intervention, did not confirm the previous observations. Recently, the results of Wijpkema at el. have been confirmed by Tiroch et al, who studied 1357 patients 6 months after coronary stenting [34]. Like these two groups and in contrast to several smaller studies, we have not been able to confirm any influence of the (GT)n microsatellite in the promoter of the HMOX1 gene on the risk of CAD, a history of MI, and total or cardiovascular mortality.
It is not unusual, that association studies of genetic polymorphisms produce divergent results, especially if small numbers of cases and controls are examined. In many instances positive associations seen in small studies have been disproven in subsequent studies of larger cohorts. Both, our CAD and control group were substantially larger than the groups investigated in the other reports. The only report with a comparable number of participants is the study of Wijpkema et al. and their results are in line with ours [33]. In addition, the reliability of the former studies is challenged by the creation of three subclasses [17, 30, 31] or different cut-offs like S<23 [17], S<25 [15, 23], S<26 [20, 24], S<27 [18], and S<29 [22] without any rational explanation for these classifications. Especially in small cohorts the cut-off can substantially affect risk estimation. To avoid this problem we examined two common cut-offs (S<25 and S<27), with the minor allele representing 32.2% or 37.5%, respectively, and found no association with cardiovascular disease, irrespective of the chosen model. Therefore, we are confident that previous observations have overestimated the effect of the (GT)n repeat.
Concerning the -413A>T SNP only one study has been published before [21] showing a decreased risk of ischemic heart disease for homozygous carriers of the A allele in Japanese individuals. First, we found a switch in the allele distribution in Caucasians towards A as the major allele (A = 0,589 versus A = 0,442 in Japanese), confirming data of the HapMap consortium for Caucasians, and second we could not confirm any of the described associations. This is not unusual because it is well known that there is a significant genetic diversity between Caucasians and Asians. Furthermore the number of cases in the Japanese study was very low (MI = 393, angina pectoris = 204) [21].
On product of the enzymatic action of HO-1 is biliverdin, which in turn is converted to bilirubin. Biliverdin and bilirubin are both antioxidants, and higher serum levels of bilirubin are inversely related to the risk of CAD [14]. Actually, a similar relationship can be found in our study, the control group showing significantly higher serum levels of bilirubin (Table 1). In contrast to the hypothesis that genetic variants of HMOX1 associated with a higher expression would increase bilirubin serum levels we did not see any association between HMOX1 genotypes and bilirubin concentration. We can not exclude that other genes involved in bilirubin metabolism superpose the effect of different HMOX1 genotypes. One candidate gene is UGT1A1, coding for bilirubin uridine diphosphate-glucuronosyltransferase. This enzyme is responsible for the glucuronidation of bilirubin and thus enhances its elimination. Recently, a promoter variation (UGT1A1*28) has been associated with higher bilirubin serum levels and lower risk for coronary heart disease in the Framingham Heart Study [35]. The metabolism of iron is even more complicated and therefore it is not surprising that we did not see any correlation between HMOX1 genotypes and serum iron levels.
A methodological aspect of the present study that deserves discussion, like in many case-control association studies, is the appropriateness of the control group. Because angiography is relatively insensitive for early lesions that do not impact on the vascular lumen, early lesions undetectable by angiography could not be ruled out in controls, similar to coronary microvascular dysfunction. Nonetheless, coronary angiography remains a gold standard for the diagnosis of CAD, and for the definition of the coronary artery status, this may however be regarded as a strength of the study because of "controls" were also studied by angiography. This is crucial because the prevalence of clinically asymptomatic coronary atherosclerosis has been reported to be high at or above the age of 50 years [36]. Hence, angiography based recruitment of controls rules out that individuals with significant, yet clinically unapparent CAD are inadvertently allocated in the control group. Surprisingly, our control group appears well representative since the major cardiovascular risk factors occur at a similar frequency as in the general population [37].
Conclusion
In conclusion, the regulation of the HMOX1 gene may be determined, at least in part, by genetics, and reduced ability to induce HO-1 expression may be involved in the mechanism of coronary atherosclerosis. Nevertheless, neither the (GT)n dinucleotide repeat nor the -413A>T polymorphism of HMOX1 gene are reliable genetic markers for cardiovascular disease in Caucasians.
References
Ross R: Atherosclerosis – an inflammatory disease. N Engl J Med. 1999, 340 (2): 115-126. 10.1056/NEJM199901143400207.
Kim HP, Ryter SW, Choi AM: CO as a cellular signaling molecule. Annu Rev Pharmacol Toxicol. 2006, 46: 411-449. 10.1146/annurev.pharmtox.46.120604.141053.
Stocker R, Glazer AN, Ames BN: Antioxidant activity of albumin-bound bilirubin. Proc Natl Acad Sci USA. 1987, 84 (16): 5918-5922. 10.1073/pnas.84.16.5918.
Baranano DE, Rao M, Ferris CD, Snyder SH: Biliverdin reductase: a major physiologic cytoprotectant. Proc Natl Acad Sci USA. 2002, 99 (25): 16093-16098. 10.1073/pnas.252626999.
Ollinger R, Bilban M, Erat A, Froio A, McDaid J, Tyagi S, Csizmadia E, Graca-Souza AV, Liloia A, Soares MP, et al: Bilirubin: a natural inhibitor of vascular smooth muscle cell proliferation. Circulation. 2005, 112 (7): 1030-1039. 10.1161/CIRCULATIONAHA.104.528802.
Maines MD: The heme oxygenase system: a regulator of second messenger gases. Annu Rev Pharmacol Toxicol. 1997, 37: 517-554. 10.1146/annurev.pharmtox.37.1.517.
Otterbein LE, Choi AM: Heme oxygenase: colors of defense against cellular stress. Am J Physiol Lung Cell Mol Physiol. 2000, 279 (6): L1029-1037.
Wang LJ, Lee TS, Lee FY, Pai RC, Chau LY: Expression of heme oxygenase-1 in atherosclerotic lesions. Am J Pathol. 1998, 152 (3): 711-720.
Duckers HJ, Boehm M, True AL, Yet SF, San H, Park JL, Clinton Webb R, Lee ME, Nabel GJ, Nabel EG: Heme oxygenase-1 protects against vascular constriction and proliferation. Nat Med. 2001, 7 (6): 693-698. 10.1038/89068.
Tulis DA, Durante W, Peyton KJ, Evans AJ, Schafer AI: Heme oxygenase-1 attenuates vascular remodeling following balloon injury in rat carotid arteries. Atherosclerosis. 2001, 155 (1): 113-122. 10.1016/S0021-9150(00)00552-9.
Lindenblatt N, Bordel R, Schareck W, Menger MD, Vollmar B: Vascular heme oxygenase-1 induction suppresses microvascular thrombus formation in vivo. Arterioscler Thromb Vasc Biol. 2004, 24 (3): 601-606. 10.1161/01.ATV.0000118279.74056.8a.
Li Volti G, Wang J, Traganos F, Kappas A, Abraham NG: Differential effect of heme oxygenase-1 in endothelial and smooth muscle cell cycle progression. Biochem Biophys Res Commun. 2002, 296 (5): 1077-1082. 10.1016/S0006-291X(02)02054-5.
Abraham NG, Kushida T, McClung J, Weiss M, Quan S, Lafaro R, Darzynkiewicz Z, Wolin M: Heme oxygenase-1 attenuates glucose-mediated cell growth arrest and apoptosis in human microvessel endothelial cells. Circ Res. 2003, 93 (6): 507-514. 10.1161/01.RES.0000091828.36599.34.
Morita T: Heme oxygenase and atherosclerosis. Arterioscler Thromb Vasc Biol. 2005, 25 (9): 1786-1795. 10.1161/01.ATV.0000178169.95781.49.
Exner M, Schillinger M, Minar E, Mlekusch W, Schlerka G, Haumer M, Mannhalter C, Wagner O: Heme oxygenase-1 gene promoter microsatellite polymorphism is associated with restenosis after percutaneous transluminal angioplasty. J Endovasc Ther. 2001, 8 (5): 433-440. 10.1583/1545-1550(2001)008<0433:HOGPMP>2.0.CO;2.
Schillinger M, Exner M, Mlekusch W, Domanovits H, Huber K, Mannhalter C, Wagner O, Minar E: Heme oxygenase-1 gene promoter polymorphism is associated with abdominal aortic aneurysm. Thromb Res. 2002, 106 (2): 131-136. 10.1016/S0049-3848(02)00100-7.
Chen YH, Lin SJ, Lin MW, Tsai HL, Kuo SS, Chen JW, Charng MJ, Wu TC, Chen LC, Ding YA, et al: Microsatellite polymorphism in promoter of heme oxygenase-1 gene is associated with susceptibility to coronary artery disease in type 2 diabetic patients. Hum Genet. 2002, 111 (1): 1-8. 10.1007/s00439-002-0769-4.
Kaneda H, Ohno M, Taguchi J, Togo M, Hashimoto H, Ogasawara K, Aizawa T, Ishizaka N, Nagai R: Heme oxygenase-1 gene promoter polymorphism is associated with coronary artery disease in Japanese patients with coronary risk factors. Arterioscler Thromb Vasc Biol. 2002, 22 (10): 1680-1685. 10.1161/01.ATV.0000033515.96747.6F.
Schillinger M, Exner M, Minar E, Mlekusch W, Mullner M, Mannhalter C, Bach FH, Wagner O: Heme oxygenase-1 genotype and restenosis after balloon angioplasty: a novel vascular protective factor. J Am Coll Cardiol. 2004, 43 (6): 950-957. 10.1016/j.jacc.2003.09.058.
Chen YH, Chau LY, Lin MW, Chen LC, Yo MH, Chen JW, Lin SJ: Heme oxygenase-1 gene promotor microsatellite polymorphism is associated with angiographic restenosis after coronary stenting. Eur Heart J. 2004, 25 (1): 39-47. 10.1016/j.ehj.2003.10.009.
Ono K, Goto Y, Takagi S, Baba S, Tago N, Nonogi H, Iwai N: A promoter variant of the heme oxygenase-1 gene may reduce the incidence of ischemic heart disease in Japanese. Atherosclerosis. 2004, 173 (2): 315-319. 10.1016/j.atherosclerosis.2003.11.021.
Gulesserian T, Wenzel C, Endler G, Sunder-Plassmann R, Marsik C, Mannhalter C, Iordanova N, Gyongyosi M, Wojta J, Mustafa S, et al: Clinical restenosis after coronary stent implantation is associated with the heme oxygenase-1 gene promoter polymorphism and the heme oxygenase-1 +99G/C variant. Clin Chem. 2005, 51 (9): 1661-1665. 10.1373/clinchem.2005.051581.
Dick P, Schillinger M, Minar E, Mlekusch W, Amighi J, Sabeti S, Schlager O, Raith M, Endler G, Mannhalter C, et al: Haem oxygenase-1 genotype and cardiovascular adverse events in patients with peripheral artery disease. Eur J Clin Invest. 2005, 35 (12): 731-737. 10.1111/j.1365-2362.2005.01580.x.
Brydun A, Watari Y, Yamamoto Y, Okuhara K, Teragawa H, Kono F, Chayama K, Oshima T, Ozono R: Reduced expression of heme oxygenase-1 in patients with coronary atherosclerosis. Hypertens Res. 2007, 30 (4): 341-348. 10.1291/hypres.30.341.
Winkelmann BR, Marz W, Boehm BO, Zotz R, Hager J, Hellstern P, Senges J: Rationale and design of the LURIC study – a resource for functional genomics, pharmacogenomics and long-term prognosis of cardiovascular disease. Pharmacogenomics. 2001, 2 (1 Suppl 1): S1-73. 10.1517/14622416.2.1.S1.
Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997, 20 (7): 1183-1197.
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB: A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975, 51 (4 Suppl): 5-40.
Funk M, Endler G, Schillinger M, Mustafa S, Hsieh K, Exner M, Lalouschek W, Mannhalter C, Wagner O: The effect of a promoter polymorphism in the heme oxygenase-1 gene on the risk of ischaemic cerebrovascular events: the influence of other vascular risk factors. Thromb Res. 2004, 113 (3–4): 217-223. 10.1016/j.thromres.2004.03.003.
Endler G, Exner M, Schillinger M, Marculescu R, Sunder-Plassmann R, Raith M, Jordanova N, Wojta J, Mannhalter C, Wagner OF, et al: A microsatellite polymorphism in the heme oxygenase-1 gene promoter is associated with increased bilirubin and HDL levels but not with coronary artery disease. Thromb Haemost. 2004, 91 (1): 155-161.
Yamada N, Yamaya M, Okinaga S, Nakayama K, Sekizawa K, Shibahara S, Sasaki H: Microsatellite polymorphism in the heme oxygenase-1 gene promoter is associated with susceptibility to emphysema. Am J Hum Genet. 2000, 66 (1): 187-195. 10.1086/302729.
Hirai H, Kubo H, Yamaya M, Nakayama K, Numasaki M, Kobayashi S, Suzuki S, Shibahara S, Sasaki H: Microsatellite polymorphism in heme oxygenase-1 gene promoter is associated with susceptibility to oxidant-induced apoptosis in lymphoblastoid cell lines. Blood. 2003, 102 (5): 1619-1621. 10.1182/blood-2002-12-3733.
Ono K, Mannami T, Iwai N: Association of a promoter variant of the haeme oxygenase-1 gene with hypertension in women. J Hypertens. 2003, 21 (8): 1497-1503. 10.1097/00004872-200308000-00013.
Wijpkema JS, van Haelst PL, Monraats PS, Bruinenberg M, Zwinderman AH, Zijlstra F, Steege van der G, de Winter RJ, Doevendans PA, Waltenberger J, et al: Restenosis after percutaneous coronary intervention is associated with the angiotensin-II type-1 receptor 1166A/C polymorphism but not with polymorphisms of angiotensin-converting enzyme, angiotensin-II receptor, angiotensinogen or heme oxygenase-1. Pharmacogenet Genomics. 2006, 16 (5): 331-337. 10.1097/01.fpc.0000205001.07054.fa.
Tiroch K, Koch W, von Beckerath N, Kastrati A, Schomig A: Heme oxygenase-1 gene promoter polymorphism and restenosis following coronary stenting. Eur Heart J. 2007, 28 (8): 968-973. 10.1093/eurheartj/ehm036.
Lin JP, O'Donnell CJ, Schwaiger JP, Cupples LA, Lingenhel A, Hunt SC, Yang S, Kronenberg F: Association between the UGT1A1*28 allele, bilirubin levels, and coronary heart disease in the Framingham Heart Study. Circulation. 2006, 114 (14): 1476-1481. 10.1161/CIRCULATIONAHA.106.633206.
Tuzcu EM, Kapadia SR, Tutar E, Ziada KM, Hobbs RE, McCarthy PM, Young JB, Nissen SE: High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation. 2001, 103 (22): 2705-2710.
Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, Kastarinen M, Poulter N, Primatesta P, Rodriguez-Artalejo F, et al: Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. Jama. 2003, 289 (18): 2363-2369. 10.1001/jama.289.18.2363.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/10/36/prepub
Acknowledgements
We would like to thank S. von Karger and A. Schwentek (Freiburg) for technical assistance, the LURIC study team, the laboratory staff at the Ludwigshafen General Hospital and the universities of Freiburg and Ulm, and the German registration offices and local public health departments for their assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NL carried out the microsatellite analysis and contributed to the analysis and interpretation of the data as well as to the writing of the manuscript. KW participated in the design of the study and helped to perform the statistical analysis and to draft the manuscript. US and BW organised the follow-up within LURIC and contributed the survival data. BRW, BOB, and WM conceived of the LURIC study and participated in its design and coordination. MMH participated in the design of the study, carried out the SNP analysis, performed the statistical analysis and drafted the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lüblinghoff, N., Winkler, K., Winkelmann, B.R. et al. Genetic variants of the promoter of the heme oxygenase-1 gene and their influence on cardiovascular disease (The Ludwigshafen Risk and Cardiovascular Health Study). BMC Med Genet 10, 36 (2009). https://doi.org/10.1186/1471-2350-10-36
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-10-36