Abstract
Background
Plasma level of high-density lipoprotein-cholesterol (HDL-C), a heritable trait, is an important determinant of susceptibility to atherosclerosis. Non-synonymous and regulatory single nucleotide polymorphisms (SNPs) in genes implicated in HDL-C synthesis and metabolism are likely to influence plasma HDL-C, apolipoprotein A-I (apo A-I) levels and severity of coronary atherosclerosis.
Methods
We genotyped 784 unrelated Caucasian individuals from two sets of populations (Lipoprotein and Coronary Atherosclerosis Study- LCAS, N = 333 and TexGen, N = 451) for 94 SNPs in 42 candidate genes by 5' nuclease assays. We tested the distribution of the phenotypes by the Shapiro-Wilk normality test. We used Box-Cox regression to analyze associations of the non-normally distributed phenotypes (plasma HDL-C and apo A-I levels) with the genotypes. We included sex, age, body mass index (BMI), diabetes mellitus (DM), and cigarette smoking as covariates. We calculated the q values as indicators of the false positive discovery rate (FDR).
Results
Plasma HDL-C levels were associated with sex (higher in females), BMI (inversely), smoking (lower in smokers), DM (lower in those with DM) and SNPs in APOA5, APOC2, CETP, LPL and LIPC (each q ≤0.01). Likewise, plasma apo A-I levels, available in the LCAS subset, were associated with SNPs in CETP, APOA5, and APOC2 as well as with BMI, sex and age (all q values ≤0.03). The APOA5 variant S19W was also associated with minimal lumen diameter (MLD) of coronary atherosclerotic lesions, a quantitative index of severity of coronary atherosclerosis (q = 0.018); mean number of coronary artery occlusions (p = 0.034) at the baseline and progression of coronary atherosclerosis, as indicated by the loss of MLD.
Conclusion
Putatively functional variants of APOA2, APOA5, APOC2, CETP, LPL, LIPC and SOAT2 are independent genetic determinants of plasma HDL-C levels. The non-synonymous S19W SNP in APOA5 is also an independent determinant of plasma apo A-I level, severity of coronary atherosclerosis and its progression.
Similar content being viewed by others
Background
Coronary artery disease is the most common cause of death in the western hemisphere and is expected to become the leading cause of morbidity and mortality in the world by the year 2020 [1]. Plasma high-density lipoprotein-cholesterol (HDL-C) level is a major determinant of susceptibility to coronary atherosclerosis in the general population [2–7]. A low plasma HDL-C level is the most common lipid abnormality found in families with premature coronary atherosclerosis [2]. Plasma HDL-C level is inversely associated with the progression of coronary atherosclerosis and cardiovascular mortality [3–7]. In contrast, raising the plasma high HDL-C level, even modestly, with the exception of inhibition of cholesteryl ester transfer protein (CETP) with torcetrapib, protects against atherosclerosis and reduces adverse cardiovascular events [4, 8–10].
Genetic studies of Mendelian traits have firmly established the impact of genetic mutations on plasma HDL-C levels. A prototypic example is Tangier disease, wherein mutations in ABCA1 lead to very low plasma HDL-C and apolipoprotein (apo) A-I levels and premature coronary atherosclerosis [11, 12]. Plasma HDL-C level in the general population is also a heritable trait. Heritability of plasma HDL-C level has been estimated to be greater than 50% in most studies [13–18]. The estimates of heritability in the Strong Heart Family Study and HERITAGE family study were 50% and 52%, respectively [14, 15]. Unlike the Mendelian disorders, however, the specific genetic variants that contribute to plasma HDL-C levels in the general population are largely unknown. The advent of genome-wide association studies (GWAS) has raised considerable interest in identifying novel genetic determinants of complex traits, such as plasma HDL-C. Accordingly, several genes that influence plasma HDL-C levels have been identified [19, 20]. Collectively, the associated variants in GWAS accounted for only 5-8% of the variation in the plasma HDL-C levels [19, 20]. Hence, much of the heritability of plasma HDL-C levels has remained unexplained.
We genotyped 784 unrelated Caucasian individuals from two independent populations of Lipoprotein and Coronary Atherosclerosis Study (N = 333) and TexGen (N = 451) for 94 non-synonymous or regulatory single nucleotide polymorphisms (SNPs) in 42 genes implicated in HDL-C biosynthesis and metabolism. We analyzed association of the SNPs with plasma HDL-C and apo A-I levels as well as with the severity and progression of coronary atherosclerosis.
Methods
Study population
All participants signed informed consent for the genetic studies and the institutional review board approved the study. We include 784 unrelated Caucasians, comprised of the LCAS subpopulation (N = 333) and the TexGen subpopulation (N = 451). The study design and the main results of the LCAS have been published [21]. In brief, the main LCAS included 372 Caucasians who had at least 1 coronary lesion causing 30% to 75% luminal diameter stenosis on quantitative coronary angiography and had a plasma low-density lipoprotein-cholesterol (LDL-C) level of 115 to 190 mg/dl despite diet. DNA samples from 333 Caucasians were available. The baseline values of plasma total cholesterol, LDL-C, HDL-C, triglyceride (TG) and apolipoprotein levels were measured in all participants at the baseline. Quantitative indices of severity of coronary atherosclerosis were measured in 289 participants.
Given the relatively small sample size of the LCAS population, we recruited 451 patients from outpatient clinics (the TexGen study). The TexGen subpopulation was matched for age and the mean plasma HDL-C level to the LCAS subpopulation. Because of the small number of females in the LCAS population, we included relatively more females in the TexGen subpopulation. Individuals taking medications with direct effects on plasma HDL-C levels, such as niacin and fibrates were not included in the study. Those with advanced co-morbid conditions, including malignancies, advanced heart failure or valvular heart disease were not included. Demographic data were collected and fasting plasma total cholesterol, HDL-C, LDL-C and TG levels were measured in all TexGen participants.
Selection of the candidate genes and SNPs
We selected the candidate genes based on a prior knowledge of their involvement in pathways leading to synthesis, maturation, or catabolism of HDL-C in humans or in experimental animals. Upon selection of the candidate genes, we searched the SNP database (dbSNP Build 129) to identify non-synonymous SNPs and the regulatory SNPs in the 5' or 3' regions of the genes of interest. We included only SNPs that have been validated, have a known minor allele frequency (MAF) in the database or were previously shown to be associated with plasma HDL-C levels. Given the size of the study population, we mostly selected the SNPs that had known minor allele frequencies (MAFs) of > 0.1, while realizing that the MAFs could differ in our study population. In view of the presence of a very large number of SNP in each gene locus, the selected SNPs comprised only a fraction of the total SNPs in the candidate genes loci. We genotyped the selected SNPs by fluorogenic 5' nucleotidase (Taqman) assays using an ABI PRISM® 7900HT Real-Time PCR instrument. The PCR conditions were 1 cycle at 95°C for 10 min, followed by 40 cycles at 92°C for 15 sec and 60°C for 1 min as recommended by the manufacturer (Applied Biosystems, Foster City, CA). Investigators who had no knowledge of the angiographic and clinical data performed the genotyping.
Since there was no known candidate SNP in ATP5B, a high affinity HDL-C receptor for apo A-I [22], we sequenced its entire coding region, 3' untranslated sequence and a 2 kbp 5' genomic fragment in 50 randomly selected individuals from the LCAS subpopulation. We performed the sequencing using the Big Dye Terminator Cycle Sequencing Ready Reaction Kit on an ABI Genetic Analyzers in sense and anti-sense directions. The sequences were analyzed and "Blasted" against the genome databases.
Statistical analysis
We expressed the parametric variables as mean ± SD and tested the variables for Gaussian distribution by the Shapiro-Wilk normality test. We tested the distribution of genotypes of each SNP for departure of the Hardy-Weinberg equilibrium (HWE) by the X2 test using a web-based program http://www.oege.org/software/hwe-mr-calc.shtml[23]. We compared the mean values between the two groups by the t test and analyzed the non-parametric variables by the Fisher exact test. We assigned indicators to genotypes as 0, 1 and 2 to represent 0, 1 and 2 copies of the common allele (additive genetic model). Likewise, we assigned indicators 0 and 1 to females and males, respectively. Since the distributions of plasma HDL-C and apo A-I levels deviated significantly from normality, we analyzed associations between the predictors and plasma HDL-C and apo A-I levels by Box-Cox regression analysis using likelihood ratio tests (16,000 iterations). We analyzed each potential predictor separately and included those with p values ≤ 0.10 in the multivariate Box-Cox regression analysis to determine independent association of the predictors with the phenotypes. We calculated the False positive Discovery Rate (FDR) for the results of multivariate analysis by calculating the q values by the method of Storey and Tibshirani [24]. All statistical analyses were performed using STATA, IC 10.1 for Macintosh.
Results
Characteristics of the study population
The baseline characteristics of the study population including the characteristics of the LCAS and TexGen subpopulations are shown in Table 1. The subpopulations were matched for age and mean plasma HDL-C levels. There were more females and more individuals with diabetes mellitus in the TexGen subpopulation. There were modest albeit statistically significant differences in body weight (~3.4 Kg), body mass index (BMI, ~1.2 Kg/m2), mean systolic or diastolic blood pressure (1-3 mmHg) and the history of myocardial infarction between the two subpopulations (Table 1).
As would be expected, mean plasma HDL-C levels were similar between the two groups. However, plasma total cholesterol and LDL-C levels were significantly higher in the LCAS subpopulations, as a high plasma LDL-C level was a requirement for inclusion in the LCAS. Plasma apolipoprotein levels and quantitative indices of severity of coronary atherosclerosis were available only in the LCAS subpopulation (Table 1).
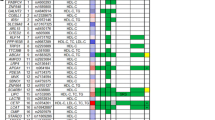
Candidate genes and SNPs
The list of biologically plausible candidate genes and SNPs analyzed in the present study and the MAFs in the entire population are shown in Additional File 1. The genotypes of all but 3 SNPs followed the HWE. The genotypes of SNPs rs4301822 in APOF, rs2306985 in MTP and rs2038068 in PPARD showed significant departure from the HWE (p < 0.05). The departure may reflect genotyping errors or the population genetic structure. Therefore, they were not included in the subsequent association analyses.
Independent predictors of plasma HDL-C levels
Plasma HDL-C and apo A-I deviated significantly from the normal Gaussian distributions (z = 8.473, p < 0.00001 for HDL-C and z = 6.386, p < 0.00001). Likewise, the log10 transformed HDL-C levels were non-normally distributed (z = 2.360, p = 0.00913). Therefore, Box-Cox regression analysis was used to determine association of the potential predictors with plasma HDL-C and apo A-I levels. Sex, body mass index (BMI), diabetes mellitus (DM) and cigarette smoking were independent predictors of plasma HDL-C and apoA-I levels (Tables 2 and 3). The FDR for each of the observed associations of sex, BMI, DM and smoking all were very low (less than 0.1%). Therefore, they were included in the subsequent analyses as covariates.
We genotyped the study population for 94 SNPs in 42 genes (Additional File 1). Three SNPs were very rare and 2 not detected in the LCAS subpopulation. Therefore, we analyzed 89 SNPs in the entire population and included any potentially significance association, defined as p < 0.05, in the multivariate analysis. SNPs in APOA5, APOC2, CETP, LIPC and LPL were independent predictors of plasma HDL-C levels (Table 4). The FDR for each of the above genes was ≤ 1 percent. Considering that plasma HDL-C, DM and BMI may share common genetic etiology as part of the metabolic syndrome; we repeated the Box-Cox regression analysis after removal of BMI and DM from the analysis as covariates. The results, shown in Table 2, identify APOA2 and SOAT2 variants, in addition to SNPs in APOA5, APOC2, CETP, LIPC and LPL also as independent determinants of plasma HDL-C levels.
We also determined independent association of SNPs with plasma HDL-C levels as a non-parametric phenotype of less or greater than the median value of 43 mg/dl by logistic regression analysis (robust method). The results were largely concordant with the results of Box-Cox regression analysis, as sex, BMI, DM and smoking as well as SNPs in APOA5, CETP and LPL were independent predictors of plasma HDL-C levels (all q values ≤ 0.06).
Since plasma triglyceride and HDL-C levels may share common genetic determinants, we analyzed the association of plasma triglyceride levels with the demographic variables and SNPs in APOA5, APOC2, CETP, LIPC and LPL. We used Box-Cox regression for the analysis because of non-normal distribution of plasma triglyceride levels. The main determinants of plasma triglyceride levels in the present study population were BMI and LPL variants, while age and APOA5 had modest effects (Data not presented).
Independent predictors of plasma apo A-I levels
Plasma apo A-I levels also did not follow a normal distribution. Therefore, we tested the association of plasma apo A-I levels with demographic predictors and SNP by Box-Cox regression. Sex (higher in females), BMI (inversely), age (positively) and SNPs in MTP, CETP, APOC2, APOA5 and SCARB1 were independent predictors of plasma apo A-I levels (Table 3).
SNPs and severity of coronary atherosclerosis
There was no significant association between the demographic variables and the severity of coronary atherosclerosis at the baseline. However, baseline MLD was associated with the rs3135506 (S19W) SNP in APOA5. Those with the uncommon allele (GA only, no AA) had more severe coronary atherosclerosis than those with the common genotype (GG). The mean MLD was 1.42 ± 0.43 mm in those with the GA genotype (N = 11) and 1.69 ± 0.69 (N = 278) in those with the GG genotype (t = 2.204, p = 0.014, q = 0.021). Likewise, the number of coronary occlusion was greater in those with the GA as compared to those with the GG genotype (0.064 ± 0.67 vs. 0.28 ± 0.54, respectively, p = 0.034). It merits noting that the observed association with the severity of coronary artery disease was concordant with the effects of the SNP on plasma HDL-C (~6 mg/dl lower in those with GA genotype) and apo A-I (~13 mg/dl lower in those with the GA genotype) levels. The MTP variants (rs2306986) were also associated with the MLD at the baseline. The mean MLD was 1.66 ± 0.40 mm in individuals with the GG genotype (N = 273) as compared to 1.94 ± 0.34 mm in those with the GC genotype (N = 16, t = -2.8084, p = 0.0027, q = 0.008).
SNPs and progression of coronary atherosclerosis
Plasma levels of HDL-C (regression coefficient: 0.004, 95% CI: [0.002-0.006], t = 3.36, p = 0.001) and treatment with fluvastatin (regression coefficient: 0.084, 95% CI: [0.032-0.136], t = 3.19, p = 0.002) were independent predictors of the progression of coronary atherosclerosis (change in MLD) in the LCAS population [21]. Therefore, we included HDL-C levels and treatment with fluvastatin as covariates in the genetic analysis. Progression of coronary atherosclerosis as determined by the change in MLD during the 2.5 years follow up, was associated with S19W SNP in APOA5. Those with the uncommon genotype (AG) had greater loss of MLD (0.25 ± 0.23 mm) over the follow up period than those with the common genotype (-0.05 ± 0.25 mm, p = 0.0048).
Discussion
We analyzed association of plasma HDL-C levels with 89 putatively functional SNPs in 42 biologically candidate genes in a well-characterized Caucasian population. The results show that SNPs in genes encoding apo A-II (APOA2) apo A-V (APOA5), apo C-II (APOC2), cholesteryl ester transfer protein (CETP), hepatic lipase (LIPC), lipoprotein lipase (LPL) and Sterol O-acyltransferase 2 (SOAT2) as well as demographic variables sex, BMI, DM and smoking were independent predictors of plasma HDL-C levels. The false positive discovery rates (q values) for the observed associations were less than 5%, which is considered low. Consistent with the above, SNPs in CETP, APOC2 and APOA5 were also independent predictors of plasma apo A-I levels. Likewise, the APOA5 variant was also associated with the severity of coronary atherosclerosis at the baseline as well as progression of coronary atherosclerosis over a 2.5 years period.
The results of the present study are largely in accord with the known biological effects of the genes in HDL-C biosynthesis, maturation and catabolism and largely supported by the previous data for SNPs in APOA5, CETP, LIPC and LPL genes [20, 25–31]. An interesting finding was the concordant association of the S19W SNP in APOA5 with plasma HDL-C and apo A-I levels as well as the severity of coronary atherosclerosis and its progression. APOA5 encodes apo A-V, which is a component of HDL-C and an important determinant of plasma triglyceride levels. The APOA5 S19W variant has been previously associated with hypertriglyceridemia as well as with plasma HDL-C levels [19, 32]. However, the findings regarding the associations of the S19W SNP with the severity and progression of coronary atherosclerosis are new and in harmony with the effects of the APOA5 variants on plasma HDL-C, apo A-I and triglyceride levels. Thus, the findings further substantiate the clinical significance of APOA5 variants in coronary atherosclerosis.
The observed associations of plasma HDL-C and apo A-I levels with APOC2 variants are also novel, albeit intrinsic to the candidate gene approach is a prior biological plausibility of the candidates and hence, the findings were not unexpected. Apo C-II is an activator of lipoprotein lipase (LPL) and a regulator of plasma triglyceride levels. Loss-of-function mutations in APOC2 and LPL are associated with severe hypertriglyceridemia [33]. As in the present study, variants of LPL have been previously associated with plasma HDL-C levels [34].
Association studies that include multiple SNPs have an inherent risk of spurious associations. To shed some light on the possibility of association by chance alone, we calculated the FDR. We note the FDR for the above associations between plasma HDL-C and SNPs were quite low (q values of ≤ 0.01). Equally striking is the absence of significant associations between plasma HDL-C levels and SNPs in many of the selected genes that have been previously implicated - through studies in humans or animals - in HDL-C biosynthesis and metabolism. Various factors may contribute to the null results for the above genes including the characteristics of the study population, competing factors (demographic predictors), and conservative approach to analysis as well as the possibility of type II statistical error. The latter is typically due to interplay between the sample size of the study population, frequencies of the alleles and the effect sizes. Despite our a prior focus on common SNPs, the MAFs of 18 SNPs in our study population were <0. 05. Unless the uncommon alleles impart major effects on the plasma HDL-C levels, detection of a significant association would require a much larger population. Nevertheless, at an MAF of 0.05, assuming Hard-Weinberg equilibrium, the sample size of the study population provided 85% power to detect a 5 mg/dl difference in the mean plasma HDL-C levels between the common and uncommon genotypes, when α is set at 0.05. A larger sample size would be required to detect a smaller effect or the effects of even less frequent alleles. Likewise, we note that the secondary findings in the present study, namely, the observed associations between SNPs and the quantitative indices of severity of coronary atherosclerosis merit testing for replications. Finally, the study population was comprised of self-described Caucasians, which may not represent a genetically homogenous population. Hence, the results may be subject to possible population stratification.
The study is by no means comprehensive of all known genes and SNPs with possible roles in the HDL-C biosynthesis, maturation, conversion and/or catabolism. Recently SNPs in GALNT2, which encodes N-actetylgalactosaminyltransferase 2 locus were shown to be associated with plasma HDL-C and triglyceride levels in GWAS [19, 35]. Similarly, SNPs at the MMAB/MVK locus, which encode mevalonate kinase and methylmalonic aciduria cblB type, respectively have also been associated with plasma HDL-C levels [20]. SNPs in VNN1 encoding pantetheinase or vannin 1 have also been associated with plasma HDL-C levels [36]. Additional genes in animal models also have been associated with plasma HDL-C levels, such as Sirt1, encoding sirtuin 1 [37]. We did not include these new genes primarily because their functional roles in HDL-C biosynthesis and metabolism have not yet been determined.
Conclusion
We genotyped 784 Caucasian individuals for 94 candidate functional SNPs in 42 biologically plausible candidate genes implicated in HDL-C biosynthesis and metabolism. We report that SNPs in APOA2, APOA5, APOC2, CETP, LIPC and LPL are independent determinants of plasma HDL-C levels. SNPs in APOA5 are also associated with plasma apo A-I level, severity of coronary atherosclerosis as well as its progression.
References
Lopez AD, Murray CC: The global burden of disease, 1990-2020. NatMed. 1998, 4: 1241-1243.
Genest JJ, Martin-Munley SS, McNamara JR, Ordovas JM, Jenner J, Myers RH, Silberman SR, Wilson PW, Salem DN, Schaefer EJ: Familial lipoprotein disorders in patients with premature coronary artery disease. Circulation. 1992, 85: 2025-2033.
Ballantyne CM, Herd JA, Ferlic LL, Dunn JK, Farmer JA, Jones PH, Schein JR, Gotto AM: Influence of low HDL on progression of coronary artery disease and response to fluvastatin therapy. Circulation. 1999, 99: 736-743.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, Huttunen JK, Kaitaniemi P, Koskinen P, Manninen V: Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987, 317: 1237-1245.
Ballantyne CM, Olsson AG, Cook TJ, Mercuri MF, Pedersen TR, Kjekshus J: Influence of low high-density lipoprotein cholesterol and elevated triglyceride on coronary heart disease events and response to simvastatin therapy in 4S. Circulation. 2001, 104: 3046-3051. 10.1161/hc5001.100624.
Goldbourt U, Yaari S, Medalie JH: Isolated Low HDL Cholesterol As a Risk Factor for Coronary Heart Disease Mortality: A 21-Year Follow-up of 8000 Men. Arteriosclerosis, Thrombosis, and Vascular Biology. 1997, 17: 107-113.
Robins SJ, Collins D, Wittes JT, Papademetriou V, Deedwania PC, Schaefer EJ, McNamara JR, Kashyap ML, Hershman JM, Wexler LF, et al: Relation of gemfibrozil treatment and lipid levels with major coronary events: VA-HIT: a randomized controlled trial. JAMA: The Journal of the American Medical Association. 2001, 285: 1585-1591. 10.1001/jama.285.12.1585.
Bloomfield Rubins H, Davenport J, Babikian V, Brass LM, Collins D, Wexler L, Wagner S, Papademetriou V, Rutan G, Robins SJ: Reduction in Stroke With Gemfibrozil in Men With Coronary Heart Disease and Low HDL Cholesterol: The Veterans Affairs HDL Intervention Trial (VA-HIT). Circulation. 2001, 103: 2828-2833.
Brown BG, Zhao XQ, Chait A, Fisher LD, Cheung MC, Morse JS, Dowdy AA, Marino EK, Bolson EL, Alaupovic P, et al: Simvastatin and Niacin, Antioxidant Vitamins, or the Combination for the Prevention of Coronary Disease. The New England Journal Of Medicine. 2001, 345: 1583-1592. 10.1056/NEJMoa011090.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJP, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, et al: Effects of Torcetrapib in Patients at High Risk for Coronary Events. The New England Journal Of Medicine. 2007, 357: 2109-2122. 10.1056/NEJMoa0706628.
Brooks-Wilson A, Marcil M, Clee SM, Zhang LH, Roomp K, van Dam M, Yu L, Brewer C, Collins JA, Molhuizen HO, et al: Mutations in ABC1 in Tangier disease and familial high-density lipoprotein deficiency. NatGenet. 1999, 22: 336-345.
Bodzioch M, Orso E, Klucken J, Langmann T, Bottcher A, Diederich W, Drobnik W, Barlage S, Buchler C, Porsch-Ozcurumez M, et al: The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. NatGenet. 1999, 22: 347-351.
Mathias RA, Roy-Gagnon MH, Justice CM, Papanicolaou GJ, Fan YT, Pugh EW, Wilson AF: Comparison of year-of-exam- and age-matched estimates of heritability in the Framingham Heart Study data. BMCGenet. 2003, 4 (Suppl 1): S36-
North KE, Howard BV, Welty TK, Best LG, Lee ET, Yeh JL, Fabsitz RR, Roman MJ, MacCluer JW: Genetic and environmental contributions to cardiovascular disease risk in American Indians: the strong heart family study. American Journal of Epidemiology. 2003, 157: 303-314. 10.1093/aje/kwf208.
Perusse L, Rice T, Despres JP, Bergeron J, Province MA, Gagnon J, Leon AS, Rao DC, Skinner JS, Wilmore JH, et al: Familial resemblance of plasma lipids, lipoproteins and postheparin lipoprotein and hepatic lipases in the HERITAGE Family Study. ArteriosclerThrombVascBiol. 1997, 17: 3263-3269.
Brenn T: Genetic and environmental effects on coronary heart disease risk factors in northern Norway. The cardiovascular disease study in Finnmark. AnnHumGenet. 1994, 58 (Pt 4): 369-379.
Namboodiri KK, Kaplan EB, Heuch I, Elston RC, Green PP, Rao DC, Laskarzewski P, Glueck CJ, Rifkind BM: The Collaborative Lipid Research Clinics Family Study: biological and cultural determinants of familial resemblance for plasma lipids and lipoproteins. GenetEpidemiol. 1985, 2: 227-254.
Rao DC, Laskarzewski PM, Morrison JA, Khoury P, Kelly K, Wette R, Russell J, Glueck CJ: The Cincinnati Lipid Research Clinic family study: cultural and biological determinants of lipids and lipoprotein concentrations. AmJHumGenet. 1982, 34: 888-903.
Kathiresan S, Melander O, Guiducci C, Surti A, Burtt NP, Rieder MJ, Cooper GM, Roos C, Voight BF, Havulinna AS, et al: Six new loci associated with blood low-density lipoprotein cholesterol, high-density lipoprotein cholesterol or triglycerides in humans. Nat Genet. 2008, 40: 189-197. 10.1038/ng.75.
Willer CJ, Sanna S, Jackson AU, Scuteri A, Bonnycastle LL, Clarke R, Heath SC, Timpson NJ, Najjar SS, Stringham HM, et al: Newly identified loci that influence lipid concentrations and risk of coronary artery disease. Nat Genet. 2008, 40: 161-169. 10.1038/ng.76.
Herd JA, Ballantyne CM, Farmer JA, Ferguson JJ, Jones PH, West MS, Gould KL, Gotto AM: Effects of fluvastatin on coronary atherosclerosis in patients with mild to moderate cholesterol elevations (Lipoprotein and Coronary Atherosclerosis Study [LCAS]). AmJCardiol. 1997, 80: 278-286. 10.1016/S0002-9149(97)00346-9.
Martinez LO, Jacquet S, Esteve JP, Rolland C, Cabezon E, Champagne E, Pineau T, Georgeaud V, Walker JE, Terce F, et al: Ectopic beta-chain of ATP synthase is an apolipoprotein A-I receptor in hepatic HDL endocytosis. Nature. 2003, 421: 75-79. 10.1038/nature01250.
Rodriguez S, Gaunt TR, Day IN: Hardy-Weinberg equilibrium testing of biological ascertainment for Mendelian randomization studies. Am J Epidemiol. 2009, 169: 505-514. 10.1093/aje/kwn359.
Storey JD, Tibshirani R: Statistical significance for genomewide studies. ProcNatlAcadSci USA. 2003, 100: 9440-9445. 10.1073/pnas.1530509100.
de Grooth GJ, Zerba KE, Huang SP, Tsuchihashi Z, Kirchgessner T, Belder R, Vishnupad P, Hu B, Klerkx AHEM, Zwinderman AH: The cholesteryl ester transfer protein (CETP) TaqIB polymorphism in the cholesterol and recurrent events study: no interaction with the response to pravastatin therapy and no effects on cardiovascular outcome: A prospective analysis of the CETP TaqIB polymorphism on cardiovascular outcome and interaction with cholesterol-lowering therapy. Journal of the American College of Cardiology. 2004, 43: 854-857. 10.1016/j.jacc.2003.08.056.
Corbex M, Poirier O, Fumeron F, Betoulle D, Evans A, Ruidavets JB, Arveiler D, Luc G, Tiret L, Cambien F: Extensive association analysis between the CETP gene and coronary heart disease phenotypes reveals several putative functional polymorphisms and gene-environment interaction. GenetEpidemiol. 2000, 19: 64-80.
Yamada Y, Matsuo H, Warita S, Watanabe S, Kato K, Oguri M, Yokoi K, Metoki N, Yoshida H, Satoh K, et al: Prediction of genetic risk for dyslipidemia. Genomics. 2007, 90: 551-558. 10.1016/j.ygeno.2007.08.001.
Carr MC, Ayyobi AF, Murdoch SJ, Deeb SS, Brunzell JD: Contribution of hepatic lipase, lipoprotein lipase, and cholesteryl ester transfer protein to LDL and HDL heterogeneity in healthy women. ArteriosclerThrombVascBiol. 2002, 22: 667-673.
Couture P, Otvos JD, Cupples LA, Lahoz C, Wilson PW, Schaefer EJ, Ordovas JM: Association of the C-514T polymorphism in the hepatic lipase gene with variations in lipoprotein subclass profiles: The Framingham Offspring Study. ArteriosclerThrombVascBiol. 2000, 20: 815-822.
Deeb SS, Peng R: The C-514T polymorphism in the human hepatic lipase gene promoter diminishes its activity. J Lipid Res. 2000, 41: 155-158.
Dugi KA, Brandauer K, Schmidt N, Nau B, Schneider JG, Mentz S, Keiper T, Schaefer JR, Meissner C, Kather H, et al: Low hepatic lipase activity is a novel risk factor for coronary artery disease. Circulation. 2001, 104: 3057-3062. 10.1161/hc5001.100795.
Wang J, Ban MR, Kennedy BA, Anand S, Yusuf S, Huff MW, Pollex RL, Hegele RA: APOA5 genetic variants are markers for classic hyperlipoproteinemia phenotypes and hypertriglyceridemia. Nat Clin Pract Cardiovasc Med. 2008, 5: 730-737. 10.1038/ncpcardio1326.
Connelly PW, Maguire GF, Hofmann T, Little JA: Structure of apolipoprotein C-IIToronto, a nonfunctional human apolipoprotein. Proc Natl Acad Sci USA. 1987, 84: 270-273. 10.1073/pnas.84.1.270.
Kathiresan S, Melander O, Anevski D, Guiducci C, Burtt NP, Roos C, Hirschhorn JN, Berglund G, Hedblad B, Groop L, et al: Polymorphisms associated with cholesterol and risk of cardiovascular events. N Engl J Med. 2008, 358: 1240-1249. 10.1056/NEJMoa0706728.
Boekholdt SM, Sacks FM, Jukema JW, Shepherd J, Freeman DJ, McMahon AD, Cambien F, Nicaud V, de Grooth GJ, Talmud PJ, et al: Cholesteryl Ester Transfer Protein TaqIB Variant, High-Density Lipoprotein Cholesterol Levels, Cardiovascular Risk, and Efficacy of Pravastatin Treatment: Individual Patient Meta-Analysis of 13 677 Subjects. Circulation. 2005, 111: 278-287. 10.1161/01.CIR.0000153341.46271.40.
Goring HHH, Curran JE, Johnson MP, Dyer TD, Charlesworth J, Cole SA, Jowett JBM, Abraham LJ, Rainwater DL, Comuzzie AG, et al: Discovery of expression QTLs using large-scale transcriptional profiling in human lymphocytes. Nat Genet. 2007, 39: 1208-1216. 10.1038/ng2119.
Li X, Zhang S, Blander G, Tse JG, Krieger M, Guarente L: SIRT1 Deacetylates and Positively Regulates the Nuclear Receptor LXR. Molecular Cell. 2007, 28: 91-106. 10.1016/j.molcel.2007.07.032.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/10/111/prepub
Acknowledgements
Supported in part by grants from the TexGen Foundation and McDonald General Research Fund
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SNC carried out genotyping and assisted in data analysis, MC performed DNA sequencing and genotyping, JT carried out genotyping, RL also carried out genotyping and participated in phenotyping, JTW conceived and coordinated the TexGen study and recruited patients, AMG conceived, designed and coordinated the Lipoprotein and Coronary Atherosclerosis Study, CMB participated in the design of the study and phenotyping of the Lipoprotein and Coronary Atherosclerosis Study population and AJM conceived the genetic studies, analyzed the data and wrote the manuscript.
All authors read and approved the final manuscript.
Electronic supplementary material
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chen, S.N., Cilingiroglu, M., Todd, J. et al. Candidate genetic analysis of plasma high-density lipoprotein-cholesterol and severity of coronary atherosclerosis. BMC Med Genet 10, 111 (2009). https://doi.org/10.1186/1471-2350-10-111
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-10-111