Abstract
Background
Interferon-alpha monotherapy is effective in less than one-third patients with chronic hepatitis C. The dose-effect, tolerability and durability of interferon-alpha treatment and its long-term effect on the prevention of cirrhosis and hepatocellular carcinoma in naïve Taiwanese patients with chronic hepatitis C have not been well investigated. We conducted the present cohort study treated with high and standard interferon-alpha to illustrate the issues.
Methods
We performed a long-term virologic and histological follow-up of 214 chronic hepatitis C patients treated with interferon-alpha, 3 million units (3-MU, n = 80) or 6-MU (n = 134) thrice weekly for 24 weeks, in Taiwan between 1992 and 2001.
Results
There was no difference in the incidence of discontinuation between 3-MU and 6-MU groups (4/80, 5.0% versus 10/134. 7.5%). The 6-MU group had similar incidence of adverse events with the 3-MU group, except that 6-MU group had significantly higher incidence of psychological manifestations, mainly presented as irritability. The rates of sustained virological response (SVR) were significantly higher in 6-MU regimen (37.1%) than in 3-MU regimen (23.7%, p < 0.05) in per protocol analysis. Based on multivariate analysis, baseline viral load was strongly associated with SVR, followed by hepatitis C virus genotype, interferon-alpha regimen, and liver fibrosis. A histological improvement in necroinflammatory activity, but not in fibrosis was observed in the follow-up biopsy performed 0.5–5.5 years (mean: 1.9 years, n = 51) after end-of-treatment. Among patients without SVR, there was more activity improvement in 6-MU group. The durability of SVR was 100% (18/18) and 97.8% (45/46) for 3-MU and 6-MU group, respectively, in a mean follow-up period of 6.81 years (5.25–9.18 years). For 163 baseline non-cirrhotic patients, 9 of 84 (10.7%) non-responders and 3 of 79 (3.8%) sustained responders progressed to cirrhosis during a mean follow-up period of 5.52 and 5.74 years, respectively (p = 0.067, Kaplan-Meier survival analysis, log-rank test). For all 200 patients, hepatocellular carcinoma was detected in 12 of 113 (10.6%) non-responders and one of 87 (1.1%) sustained responders during a mean follow-up period of 5.67 and 5.73 years, respectively (p < 0.01, Kaplan-Meier survival analysis, log-rank test).
Conclusion
We confirm the dose effect of interferon-alpha in chronic hepatitis C. Six-MU regimen had better efficacy than 3-MU regimen in virologic and histological responses. Both regimens had good tolerability and durability in Taiwan. Sustained response could reduce the incidence of cirrhotic change and hepatocarcinogenesis.
Similar content being viewed by others
Background
Hepatitis C virus (HCV) is the major etiologic agent in parenterally transmitted non-A non-B hepatitis and frequently causes persistent infection leading to chronic liver disease and primary hepatocellular carcinoma (HCC)[1, 2]. Interferon-alpha (IFN-α) was the first approved therapy in the 1980s but resulted in a sustained virological response in only 8–20% of chronic hepatitis C patients treated with a standard regimen of IFN-α monotherapy, 3 million units (MU) thrice weekly for 24 weeks [3–8]. A number of factors have been considered in terms of their potential to predict the response to IFN-α therapy. These include infection with non-genotype 1b, lower levels of viremia and the absence of cirrhosis, which have been currently reported to be associated with a better response[2, 9, 10]. Several studies in Japan and Western countries have shown that higher dose (5–10 MU) of IFN could improve the efficacy on chronic hepatitis C[5, 9, 11]. Reviewing the Medline, however, only one limited study on the efficacy of IFN therapy for naïve patients of chronic hepatitis C has been reported before 1997 in Taiwan[4]. Furthermore, the dose effect, tolerability and durability of high-dose IFN therapy for naïve Taiwanese chronic hepatitis C patients have never been reported.
Since 1992, we have treated a number of Taiwanese patients with chronic hepatitis C with a standard IFN regimen, 3 MU thrice weekly for 24 weeks, and since 1995, with 6 MU thrice weekly for 24 weeks. We have followed these patients closely for 5–10 years, and we report herein the end-of-treatment and sustained response, and results of long-term follow-up to both regimens, as well as the dose effect, tolerability and durability of high-dose IFN therapy.
Methods
Patients
Two hundred and fourteen naïve chronic hepatitis C patients were enrolled in the study. All were positive for HCV antibodies (second-generation, enzyme-linked immunosorbent assay, Abbott, North Chicago, IL) and serum HCV RNA for at least 6 months. Patients with a concurrent hepatitis B virus, alcohol abuse (≧80 mL ethanol per day), overt hepatic failure, a current or past history of psychiatric condition, pregnancy, or with evidence of hepatocellular carcinoma were excluded. Two pathologists assessed all biopsy results, which were taken before IFN treatment, without knowledge of patients' clinical or laboratory data. Disease activity grade and fibrosis stage were quantitatively scored according to the histological activity index described by Knodell et al[12] Cirrhosis was diagnosed histologically in the presence of a stage 4 of fibrosis or in the absence of a liver biopsy, by a compatible ultrasonographic and clinical picture. A follow-up liver biopsy was performed in 51 patients. The present study was approved by the ethics committee of Kaohsiung Medical University Hospital. After they had given their informed consent, all patients were treated with recombinant IFN-α 2a (n = 40), IFN-α 2b (n = 102) or lymphoblastoid IFN-α n1 (n = 72), given intramuscularly, in a dose of 3-or 6-MU thrice weekly for 24 weeks. Group allocation was chronological and consecutive rather than randomized, because, before 1994, all patients were given a 3-MU and then a 6-MU IFN-α regimen. Fourteen patients (4 in 3-MU group, 5.0% and 10 in 6-MU group, 7.5%), who received IFN-α therapy less than 12 weeks, were excluded from the present study (Table 1). The presence of HCV RNA in the serum was assessed every three months for 12 months, and then every 12 months. End-of-treatment virological responder (ETVR) was defined as patients showing clearance of HCV RNA at the end of treatment. Others were defined as non-ETVR. Sustained virological responder (SVR) was defined as patients showing clearance of HCV RNA by at the end-of-treatment and 6 months after end-of-treatment. The others were classified as non-SVR. Histological improvement and worsening was defined as a ≧2-point decrease and increase in the total necroinflammatory scores between paired biopsies, respectively.
Detection/quantification of serum HCV RNA and genotyping
Detection of serum HCV RNA was performed using a standardized automated qualitative reverse transcription polymerase chain reaction assay (RT-PCR, COBAS AMPLICOR Hepatitis C Virus Test, version 2.0; Roche, Branchburg, NJ, USA). The detection limit was 50 IU/mL. HCV genotypes 1a, 1b, 2a, 2b and 3a were determined by amplification of the core region using genotype-specific primers described by Okamoto et al[13]. Serum HCV RNA levels were measured by using the branched DNA assay (Quantiplex HCV RNA 2.0, Bayer, Emeryville, CA), performed strictly in accordance with the manufacturer's instructions. The quantification range was 0.2 to 120 million equivalents (Meq) of HCV RNA per ml.
Statistical analyses
Frequency was compared between groups using the chi-square test with Yate's correction or Fisher's exact test. Group means were compared using the Student t-test. Serum HCV RNA levels were expressed as the mean ± standard deviation after logarithmic transformation of original values. Stepwise logistic regression was used to analyze factors associated with IFN-α response. Comparisons of paired liver histology were carried out with two-sample Wilcoxon's signed rank test. Preventive effects of antiviral therapy on progression of chronic HCV infection to liver cirrhosis (LC) and HCC were analyzed by using Kaplan-Meier survival analysis.
Results
Adverse effect
There was no difference of incidence of discontinuation of treatment between 3-MU and 6-MU groups (Table 1). The incidence of adverse events was similar between two groups in the presentation of flu-like symptoms, gastrointestinal and dermatological manifestations, and alopecia. However, patients in 6-MU group had significantly higher rate of psychological manifestation than those in 3-MU group did (74/134, 55.2% versus 34/80, 41.0%, p = 0.028, Table 1).
SVR and factors predicting SVR
Seventy-six patients received 3-MU IFN-α and 124 received 6-MU, thrice weekly for 24 weeks. All were followed-up for at least 6 months after end of treatment. Baseline clinical and laboratory data were not different in the two groups (Table 2). At the end of IFN-α therapy, 36 patients (47.4%) in 3-MU group and 103 (83.1%) had ETVR, the difference being highly significant (P < 0.0001). Of those with ETVR, 50% (18/36) in 3-MU group and 55.3% (57/103) in 6-MU group had reappearance of serum HCV RNA within 6 months after end-of-treatment. The difference was not significant. The SVR was significantly higher in 6-MU group (37.1%, 46/124) than in 3-MU group (23.7%, 18/76, P < 0.05).
In univariate analysis, SVR was not related gender, age, history of transfusion, the necroinflammatory activity of liver histopathology, or preparations of IFN-α (Table 3). A significant positive association for SVR was found for pretreatment alanine aminotransferase value and IFN-α dose, and a negative association with severe fibrosis (score 3 or 4), infected with HCV genotype 1b and pretreatment serum levels of HCV RNA. Based on multivariate logistic regression analysis, pretreatment HCV RNA level was strongly associated with SVR, followed by infected HCV genotype, IFN-α regimen, and severity of liver fibrosis (table 4).
Dose effect on SVR according to virological risk factors
Since HCV genotype and baseline viral loads were important predictors for SVR to IFN-α, we divided 200 patients into three virological unfavorable risk groups according to the infected HCV genotype and pretreatment HCV RNA levels[14]: low-risk group, absence of both virological risk factors (genotype 1b and pretreatment HCV RNA levels > 0.65 Meq/mL); medium-risk group, presence of only one virological risk factor; and high-risk group, presence of both two virological risk factors. The 6-MU group had significantly higher ETVR than the 3-MU group in all of the three risk groups (p < 0.01, <0.001, and <0.01 for low-, medium-, and high-risk group, respectively, Table 5). The relapsed rate did not differ between 3-MU and 6-MU groups whatever the risk groups. In medium-risk group, patients treated with 6-MU had significantly higher SVR than those with 3-MU (29.5% vs. 7.7%, p < 0.05). However, SVR did not differ between 3-MU and 6-MU groups both in low- and high-risk groups.
Paired histological examination
A follow-up liver biopsy was performed 0.5–5.5 years (mean ± SD, 1.9 ± 1.4 years) after end of treatment in 51 patients. A histological improvement with a significant decrease in the mean scores for all necroinflammatory activity (periportal, intralobular, portal inflammation and total necroinflammatory score), but not for fibrosis was observed in the follow-up biopsy (Table 6). The necroinflammatory activity improved in 68.2%, remained stable in 27.3%, and worsened in 4.6% for patients achieved a SVR, in contrast to 37.9%, 34.5%, and 27.6%, respectively, for those with non-SVR (P < 0.05, Fig. 1). Among patients achieving a SVR, there was no difference in histological response between 3-MU and 6-MU groups. Among patients without SVR, there was less frequently worsening of necroinflammatory activity (17.4%) and more activity improvement (47.8%) in 6-MU group, when compared with 3-MU group (66.7% and 0%, respectively, P < 0.01).
Impact of sustained virological response (SVR) to interferon-alpha therapy on necroinflammatory activity of liver histology. Impact of SVR to interferon-alpha therapy (left side) and of interferon regimens (3-MU versus. 6-MU groups, middle and right side) on necroinflammatory activity progression between paired liver histology.
Long-term follow-up for viral status and the development of LC and HCC
During the follow-up period, reappearance of serum HCV RNA was found in one patient, who has achieved SVR in 6-MU group, at the 57th month. The durability of SVR was 100% and 97.8% for 3-MU and 6MU group, respectively, in a mean follow-up period of 6.81 years (5.25–9.18 years). The SVR remained similar among three IFN preparations at the end of the 10 years.
Of 136 non-responders in the present study, 50 received a second course of IFN-based treatment. Three of 11 (27.3%) with IFN-α monotherapy and 20 of 39 (51.3%) with IFN-α/ribavirin combination therapy achieved a second SVR. Clinical evaluation, liver biochemistry, α-fetoprotein, and abdominal sonography were performed every 3–6 months for patients without baseline cirrhosis, and every 2–3 months for those with baseline cirrhosis during the follow-up period.
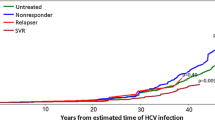
For 163 baseline non-cirrhotic patients, 9 of 84 (10.7%) non-responders and 3 of 79 (3.8%) sustained responders progressed to cirrhosis during a mean follow-up period of 5.52 and 5.74 years, respectively. The difference was borderline significant by using Kaplan-Meier survival analysis (p = 0.067, figure 2, left side). For all 200 patients, HCC was detected in 12 of 113 (10.6%) non-responders and one of 87 (1.1%) sustained responders during a mean follow-up period of 5.67 and 5.73 years, respectively. The difference was significant by using Kaplan-Meier survival analysis (p < 0.01, figure 2, right side).
Cumulative incidence of liver cirrhosis (LC) and hepatocellular carcinoma (HCC) among patients treated with interferon-alpha. Left side, cumulative incidence of LC among 163 baseline non-cirrhotic patients with sustained virological response (SVR, solid line) and without SVR (dotted line) to interferon-alpha therapy. P = 0.067 by the log-rank test. The number of LC events and patients at risk at each time point are shown below the graph. Right side, cumulative incidence of HCC among 200 patients with SVR (solid line) and without SVR (dotted line) to interferon-alpha therapy. P < 0.01 by the log-rank test. The number of HCC events and patients at risk at each time point are shown below the graph.
Discussion
In the present study, we have investigated the dose effect of IFN-α therapy on a group of Taiwanese patients with chronic hepatitis C in a 10-year follow-up. Our results demonstrated that 6 MU IFN-α, thrice weekly for 24 weeks, had better efficacy (2.3-fold) than 3 MU, thrice weekly for 24 weeks, in both virological and histological responses. Improved efficacy was mainly seen in subgroups of patients with one of the two unfavorable virologic factors, the medium-risk group, in the current study. The 6-MU regimen was as tolerable as standard 3-MU regimen for Taiwanese patients. Both regimens had good durability of SVR.
Treatment with IFN-α was the first approved therapy but a SVR could be achieved in only 8–20% of chronic hepatitis C patients treated with a standard regimen of IFN-α monotherapy (3 MU thrice weekly for 24 weeks) [3–8]. Therefore, how to improve the efficacy of IFN-α therapy is the concern of many studies. Until recently, 48 weeks of IFN-α, 3 MU thrice weekly was recommended for the treatment of chronic hepatitis C[5]. Concerning the suffering from long-term IFN therapy, we conducted higher dose of IFN regimen, 6 MU thrice weekly for 24 weeks, which total dosage was equal to that of 3 MU, thrice weekly for 48 weeks. In the present study, 6-MU regimen was observed to achieve significantly higher rates of ETVR and SVR than 3-MU regimen, but had no benefit on reducing the relapse rate. In contrast to the duration effect on improvement of SVR by reducing the relapse rate after end-of-treatment, our results implicated the dose effect on the initial response of HCV to IFN therapy[5, 7, 8]. High dose regimen as well as induction therapy could result in early clearance of HCV viremia, which is very important in the prediction of IFN response[10, 15, 16].
In the present study, the incidence of discontinuation and most of the major adverse events were similar between standard dose and higher dose of IFN therapy, despite that the higher dose of IFN regimen had significantly higher incidence of psychological manifestations. However, the psychological manifestations, mainly presented as irritability, could be controlled well with minor tranquillizers.
Consistent with previous reports[2, 3, 9, 10, 14], we confirmed the associations of pretreatment serum HCV RNA levels, HCV genotype 1b and presence of cirrhosis with response to IFN-α treatment in chronic hepatitis C patients by using stepwise logistic regression model. According to previous studies for Taiwanese patients, we divided our patients into three virological risk groups based on the presence/absence of HCV genotype 1b and the baseline viral loads greater than the cut-off point, 0.65 Meq/mL, or not[14]. As observed in the present study, 6-MU regimen could achieve significantly higher rate of ETVR but could not decrease the relapse rate in all of the three risk groups. Although our logistic regression model predicted a 2.3-times increase in probability for a SVR to occur in the 6-MU regimen versus the 3-MU regimen, the significantly better efficacy of 6-MU regimen on SVR was only observed in patients with one virological risk factor. Therefore, how to enhance the ETVR for the medium- and high-risk groups and to reduce the relapse rates for all of the three risk groups will be the key to improve SVR. Extended therapy and/or combination with ribavirin might be considered to overcome the unfavorable virological risk factors[16, 17]. Since the unfavorable virological risk factors are unchangeable, tailored regimens of IFN with or without ribavirin combination therapy according to the virological status are the only way to improve the efficiency of HCV eradication, as recommended in recent consensus on management of chronic hepatitis C[18, 19].
In accordance with previous studies [20–22], a significant decrease in necroinflammatory activity of liver histology was observed in the current study. However, our material was unable to show whether the IFN treatment resulted in cessation of fibrogenesis, regardless of IFN regimen and virological response (data not shown). Indeed, no firm conclusion can be drawn about whether the fibrosis remaining at long-term follow-up was irreversible and established or whether it will diminish with even longer follow-up[22]. Further analysis of histological response, stratified by IFN regimen and SVR, we found that 6-MU regimen could achieve histological improvement not only in SVR but also in non-SVR. By contrast, most of non-SVR treated with 3-MU regimen had histological worsening. These results presumed the prominent benefit of high dose IFN on the treatment of chronic hepatitis C.
Similar to other reports[23, 24], the long-term prognosis was excellent in this well-defined material of SVR. Serum HCV RNA was persistently undetectable in 63 of 64 patients with SVR. The only one patient, who had reappearance of serum HCV RNA concomitant with abnormal ALT level at the 57th month of follow-up, is a resident of an HCV hyperendemic area, Tzukuan[25]. Whether this is reinfection[26] or recurrence[23, 24] of HCV remains to be clarified by phylogenetic analysis of viral genome. Also our results confirm that IFN therapy, when associated with response, reduces the incidence of LC and HCC among chronic hepatitis C patients[27].
A greater efficacy in treatment of chronic hepatitis C was observed in combination with IFN-α and ribavirin[24], which has been available in Taiwan since August 1998 and becomes to be the recommendations for chronic hepatitis C patients[18, 19]. More recently, combination of pegylated IFN-α plus ribavirin shows more effective and convenient and may replace the current standard of IFN-α plus ribavirin[28, 29]. The results of current study could provide decision-making information for future therapeutic strategies of individualizing dose and duration of standard or pegylated IFN-α treatment in combination with ribavirin according to the baseline virological predictors to improve the efficiency of HCV eradication. However, pegylated IFN-α and ribavirin combination therapy is expensive and might carry potential side effects. The present higher dose regimen of IFN monotherapy might be suggested for patients who are contraindicated to ribavirin and/or pegylated IFN-α therapy[30].
Conclusion
We confirm the dose effect of IFN in chronic hepatitis C. Six-MU regimen had better efficacy than standard 3-MU regimen in both of virological and histological responses, and was as tolerable as 3-MU regimen. Nearly all sustained virological responders had a durable response and the sustained response had a preventive effect on the development of HCV-associated LC and HCC. Since the unfavorable predictors, high pretreatment HCV RNA levels, infected with genotype 1b, and presence of cirrhosis, are unchangeable, adjustment of IFN dose and duration according to the unfavorable factors is important to achieve a better efficacy/risk ratio. Our results could provide decision-making information for future therapeutic strategies of individualizing dose and duration of standard or pegylated IFN-α treatment in combination with ribavirin according to baseline predictors.
Abbreviations
- Hepatitis C virus:
-
HCV
- interferon-alpha:
-
IFN-α
- million units:
-
MU
- liver cirrhosis:
-
LC, hepatocellular carcinoma: HCC, end-of-treatment virologic responder: ETVR, sustained virologic responder: SVR
- reverse transcription polymerase chain reaction assay:
-
RT-PCR
- million equivalent:
-
Meq.
References
Alter MJ, Margolis HS, Krawczynski K, Judson FN, Mares A, Alexander WJ, Hu PY, Miller JK, Gerber MA, Sampliner RE: The natural history of community-acquired hepatitis C in the United States. The Sentinel Counties Chronic non-A, non-B Hepatitis Study Team. N Engl J Med. 1992, 327 (27): 1899-1905.
Lauer GM, Walker BD: Hepatitis C virus infection. N Engl J Med. 2001, 345 (1): 41-52. 10.1056/NEJM200107053450107.
Martinot-Peignoux M, Boyer N, Pouteau M, Castelnau C, Giuily N, Duchatelle V, Auperin A, Degott C, Benhamou JP, Erlinger S: Predictors of sustained response to alpha interferon therapy in chronic hepatitis C. J Hepatol. 1998, 29 (2): 214-223. 10.1016/S0168-8278(98)80006-8.
Hwang SJ, Chan CY, Lu RH, Wu JC, Lee SD: Randomized controlled trial of recombinant interferon-alpha 2b in the treatment of Chinese patients with chronic hepatitis C. J Interferon Cytokine Res. 1995, 15 (7): 611-616.
Poynard T, Leroy V, Cohard M, Thevenot T, Mathurin P, Opolon P, Zarski JP: Meta-analysis of interferon randomized trials in the treatment of viral hepatitis C: effects of dose and duration. Hepatology. 1996, 24 (4): 778-789.
Lindsay KL: Therapy of hepatitis C: overview. Hepatology. 1997, 26 (3 Suppl 1): 71S-77S. 10.1002/hep.510260713.
Carithers RLJ, Emerson SS: Therapy of hepatitis C: meta-analysis of interferon alfa-2b trials. Hepatology. 1997, 26 (3 Suppl 1): 83S-88S. 10.1002/hep.510260715.
Thevenot T, Regimbeau C, Ratziu V, Leroy V, Opolon P, Poynard T: Meta-analysis of interferon randomized trials in the treatment of viral hepatitis C in naive patients: 1999 update. J Viral Hepat. 2001, 8 (1): 48-62. 10.1046/j.1365-2893.2001.00271.x.
Shiratori Y, Kato N, Yokosuka O, Imazeki F, Hashimoto E, Hayashi N, Nakamura A, Asada M, Kuroda H, Tanaka N, Arakawa Y, Omata M: Predictors of the efficacy of interferon therapy in chronic hepatitis C virus infection. Tokyo-Chiba Hepatitis Research Group. Gastroenterology. 1997, 113 (2): 558-566.
Yu ML, Chuang WL, Dai CY, Chen SC, Lin ZY, Hsieh MY, Wang LY, Chang WY: Clinical evaluation of the automated COBAS AMPLICOR HCV MONITOR test version 2.0 for quantifying serum hepatitis C virus RNA and comparison to the quantiplex HCV version 2.0 test. Journal Of Clinical Microbiology. 2000, 38 (8): 2933-2939.
Hakozaki Y, Shirahama T, Katou M, Nakagawa K, Oba K, Mitamura K: A controlled study to determine the optimal dose regimen of interferon-alpha 2b in chronic hepatitis C. Am J Gastroenterol. 1995, 90 (8): 1246-1249.
Knodell RG, Ishak KG, Black WC, Chen TS, Craig R, Kaplowitz N, Kiernan TW, Wollman J: Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981, 1 (5): 431-435.
Okamoto H, Tokita H, Sakamoto M, Horikita M, Kojima M, Iizuka H, Mishiro S: Characterization of the genomic sequence of type V (or 3a) hepatitis C virus isolates and PCR primers for specific detection. J Gen Virol. 1993, 74 ( Pt 11): 2385-2390.
Yu ML, Chuang WL, Chen SC, Lin ZY, Hsieh MY, Wang LY, Chang WY: Clinical application of the Quantiplex HCV RNA 2.0 and Amplicor HCV Monitor assays for quantifying serum hepatitis C virus RNA. Journal Of Clinical Pathology. 1999, 52 (11): 807-811.
Neumann AU, Lam NP, Dahari H, Gretch DR, Wiley TE, Layden TJ, Perelson AS: Hepatitis C viral dynamics in vivo and the antiviral efficacy of interferon-alpha therapy. Science. 1998, 282 (5386): 103-107. 10.1126/science.282.5386.103.
Layden TJ: Principles of interferon induction therapy. Am J Med. 1999, 107 (6B): 71S-73S. 10.1016/S0002-9343(99)00387-3.
Chemello L, Bonetti P, Cavalletto L, Talato F, Donadon V, Casarin P, Belussi F, Frezza M, Noventa F, Pontisso P, et al: Randomized trial comparing three different regimens of alpha-2a-interferon in chronic hepatitis C. The TriVeneto Viral Hepatitis Group. Hepatology. 1995, 22 (3): 700-706. 10.1016/0270-9139(95)90286-4.
Consensus statements on the prevention and management of hepatitis B and hepatitis C in the Asia-Pacific region. Core Working Party for Asia-Pacific Consensus on Hepatitis B and C. J Gastroenterol Hepatol. 2000, 15 (8): 825-841. 10.1046/j.1440-1746.2000.02324.x.
EASL International Consensus Conference on hepatitis C. Paris, 26-27 February 1999. Consensus statement. J Hepatol. 1999, 31 Suppl 1: 3-8. 10.1016/S0168-8278(99)80367-5.
Poynard T, Bedossa P, Chevallier M, Mathurin P, Lemonnier C, Trepo C, Couzigou P, Payen JL, Sajus M, Costa JM: A comparison of three interferon alfa-2b regimens for the long-term treatment of chronic non-A, non-B hepatitis. Multicenter Study Group. N Engl J Med. 1995, 332 (22): 1457-1462. 10.1056/NEJM199506013322201.
Marcellin P, Boyer N, Gervais A, Martinot M, Pouteau M, Castelnau C, Kilani A, Areias J, Auperin A, Benhamou JP, Degott C, Erlinger S: Long-term histologic improvement and loss of detectable intrahepatic HCV RNA in patients with chronic hepatitis C and sustained response to interferon-alpha therapy. Ann Intern Med. 1997, 127 (10): 875-881.
Shiratori Y, Imazeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, Kuroki T, Nishiguchi S, Sata M, Yamada G, Fujiyama S, Yoshida H, Omata M: Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000, 132 (7): 517-524.
Larghi A, Tagger A, Crosignani A, Ribero ML, Bruno S, Portera G, Battezzati PM, Maggioni M, Fasola M, Zuin M, Podda M: Clinical significance of hepatic HCV RNA in patients with chronic hepatitis C demonstrating long-term sustained response to interferon-alpha therapy. J Med Virol. 1998, 55 (1): 7-11. 10.1002/(SICI)1096-9071(199805)55:1<7::AID-JMV2>3.0.CO;2-7.
McHutchison JG, Gordon SC, Schiff ER, Shiffman ML, Lee WM, Rustgi VK, Goodman ZD, Ling MH, Cort S, Albrecht JK: Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. Hepatitis Interventional Therapy Group. N Engl J Med. 1998, 339 (21): 1485-1492. 10.1056/NEJM199811193392101.
Yu ML, Chuang WL, Chen SC, Dai CY, Hou C, Wang JH, Lu SN, Huang JF, Lin ZY, Hsieh MY, Tsai JF, Wang LY, Chang WY: Changing prevalence of hepatitis C virus genotypes: Molecular epidemiology and clinical implications in the hepatitis C virus hyperendemic areas and a Tertiary Referral Center in Taiwan. Journal of Medical Virology. 2001, 65 (1): 58-65. 10.1002/jmv.2001.
Kao JH, Lai MY, Chen PJ, Chen DS: Probable reinfection with hepatitis C virus in a chronic hepatitis C patient with a sustained response to combination therapy. J Formos Med Assoc. 2001, 100 (12): 824-828.
Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, Inoue O, Yano M, Tanaka M, Fujiyama S, Nishiguchi S, Kuroki T, Imazeki F, Yokosuka O, Kinoyama S, Yamada G, Omata M: Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med. 1999, 131 (3): 174-181.
Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, Goodman ZD, Koury K, Ling M, Albrecht JK: Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001, 358 (9286): 958-965. 10.1016/S0140-6736(01)06102-5.
Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Goncales FLJ, Haussinger D, Diago M, Carosi G, Dhumeaux D, Craxi A, Lin A, Hoffman J, Yu J: Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002, 347 (13): 975-982. 10.1056/NEJMoa020047.
Keating GM, Curran MP: Peginterferon-alpha-2a (40kD) plus ribavirin: a review of its use in the management of chronic hepatitis C. Drugs. 2003, 63 (7): 701-730.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/5/27/prepub
Acknowledgements
This study was supported by the Taiwan Liver Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
MLY carried out the laboratory work and molecular virologic studies, participated in the collection and clinical evaluation of patients, performed the statistical analysis, and drafted the manuscript. CYD, SCC and LPL participated in the laboratory work and molecular virologic studies, and in the collection and clinical evaluation of patients. MYH, ZYL, MYH, JFT and LYW, participated in the collection and clinical evaluation of patients. WYC participated in the design of the study. WLC conceived of the study, and participated in its design and coordination. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yu, ML., Dai, CY., Chen, SC. et al. High versus standard doses interferon-alpha in the treatment of naïve chronic hepatitis C patients in Taiwan: a 10-year cohort study. BMC Infect Dis 5, 27 (2005). https://doi.org/10.1186/1471-2334-5-27
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-5-27