Abstract
Background
M.tuberculosis (M.tb) is associated with enhanced T helper cell type 1 (Th1) immune responses while helminth infection is associated with T helper cell type 2 (Th2) immune responses. Our aim was to investigate whether helminth infection could influence the ability to generate an appropriate Th1 immune response that is characterized by a positive tuberculin skin test (TST), in M.tb exposed children.
Methods
We completed a community-based, cross sectional household contact tracing study, using matched enrolment of HIV negative children with and without documented household M.tb exposure. We documented demographics, clinical characteristics, HIV status, M.tb exposure (using a standard contact score) and M.tb infection status (TST > = 10 mm). Ascaris lumbricoides-specific IgE was used as proxy for Ascaris infection/exposure.
Results
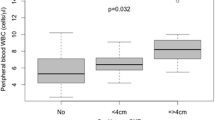
Of 271 children (median age 4 years (range: 4 months to 15 years)) enrolled, 65 participants (24%) were serum positive for Ascaris IgE. There were 168 (62%) children with a documented household tuberculosis contact and 107 (40%) were (TST) positive overall.
A positive TST was associated with increasing age (Odds Ratio (OR) =1.17, p < 0.001), increasing M.tb contact score (OR = 1.17, p < 0.001), previous tuberculosis treatment (OR = 4.8, p = 0.06) and previous isoniazid preventive treatment (OR = 3.16, p = 0.01). A visible bacillus Calmette-Guérin (BCG) scar was associated with reduced odds of being TST positive (OR = 0.42, p = 0.01).
Ascaris IgE was not associated with TST status in univariate analysis (OR = 0.9, p = 0.6), but multivariable logistic regression analysis suggested an inverse association between Ascaris IgE status and a positive TST (OR = 0.6, p = 0.08), when adjusted for age, and M.tb contact score. The addition of an age interaction term to the model suggested that the age effect was stronger among Ascaris IgE positive children; the effect of being Ascaris IgE positive significantly reduced the odds of being TST positive amongst younger children while this effect weakened with increasing age.
Conclusions
Our preliminary findings highlight a high prevalence of both Ascaris exposure/infection and M.tb infection in children in an urban setting. Helminth exposure/infection may reduce the immune response following M.tb exposure when controlling for epidemiological and clinical covariates. These findings might be relevant to the interpretation of immunological tests of M.tb infection in children.
Similar content being viewed by others
Background
Infectious diseases are important causes of morbidity and mortality in children living in the developing world. Tuberculosis is a major global threat with an estimated 9.4 million incident cases reported globally in 2009 [1], with South Africa ranked third with an estimated annual notification rate of 971 per 100 000 per year [1]. Paediatric tuberculosis contributes an estimated 15-20% of the overall global caseload, with >80% cases notified from the 22 so-called “high-burden” countries, including South Africa [2]. Young children exposed to and infected with Mycobacterium tuberculosis (M.tb) are at high risk for disease progression in the absence of effective chemoprophylaxis [3].
Poor socio-economic circumstances, prevalent in many settings with a high burden of tuberculosis, also predispose to poor living conditions, overcrowding and increased risk of helminth exposure and infection [4, 5]. Helminth infection in children is often chronic and is associated with anaemia, growth retardation, impaired cognitive functioning and chronic inflammatory diseases [6–8]. The World Health Organization (WHO) classifies South Africa as one of the 130 helminth-endemic countries (prevalence of infection > 20% - 50%) [9]. The WHO Integrated Management of Childhood Illness (IMCI) guidelines therefore routinely recommend regular deworming in children older than 1 year [10]; however, this is not consistently practiced and the constant risk of re-infection remains high in helminth-prevalent settings [4, 5].
M.tb exposure involves complex immune processes and leads to a spectrum of infection and clinical disease outcomes in children, including M.tb-exposed but uninfected, infected non-diseased and diseased [11, 12]. In addition to innate host immunity, protection against M.tb requires an effective adaptive cellular immune response characterized by robust T helper cell type 1 (Th1) T-cell immunity and relative weaker T helper cell type 2 (Th2) T-cell immune responses [13–17]. The tuberculin skin test (TST), the most established clinical-epidemiological immune measure of M.tb infection, is a marker of a Th1-type delayed type hypersensitivity reaction. Previously M.tb-sensitized circulating lymphocytes are attracted to the intra-dermal tuberculin injection site, followed by monocyte, macrophage, CD4 + − and CD8+ T-lymphocyte accumulation and release of inflammatory mediators that causes clinical erythema and oedema [12].
Th2 cells produce cytokines which play a role in protection against extracellular organisms and are increased in the presence of helminth infection [18–21], specifically Ascaris lumbricoides [20] and hookworm species [20, 21]. Data regarding the role of Th2 cells in the presence of Trichiuris trichiura infection are inconsistent [15, 22]. Th2 cell types impair signal transduction and induce anergy of immune cells, which might decrease the ability to generate protective cellular immunity to protect against common infections, like M.tb and to routine vaccinations [19]. Helminth infection is further associated with suppressive T-cell population induction and inhibitory cytokine production which can suppress Th1-type responses and interfere with effector T-cell activation, potentially resulting in altered memory immune responses against M.tb [15].
The current limited evidence supports a potential immune modulating effect of helminths on mycobacterial immune responses in humans [15, 21, 23], although contradictory evidence also exists [24, 25]. We therefore investigated the effect of an Ascaris-specific IgE positive status on a commonly used marker of M.tb infection (TST), in children in a setting with a high burden of tuberculosis. We hypothesized primarily that helminth infection in children, while controlling for M.tb exposure and other relevant covariates, would decrease the ability to generate an appropriate Th1 immune response characterized by a positive TST in children.
Methods
This was a prospective cross-sectional community-based study. Study participants were recruited from three high burden tuberculosis communities: Ravensmead, Uitsig (R/U) and Site C, Khayelitsha (Site C), in Cape Town, Western Cape Province, South Africa. The communities are demographically heterogeneous, and respectively represent ethnic groups that are predominantly of South African Mixed (R/U) and Xhosa African ancestry (Site C).
The tuberculosis notification rate in the province was 994 per 100 000 in adults and 671 per 100 000 in children aged 0 – 14 years in 2008 (Western Cape Department of Health, unpublished data). There is near universal infant bacille Calmette-Guérin (BCG) vaccination.
Prior surveys from school-going children in R/U found that 25% were stool positive for Ascaris lumbricoides and 51% for Trichuris trichiura [26]. Routine clinic and school-based deworming has since become standard of care in local health care centres. There are currently no published data on the prevalence of helminth infection in children in Khayelitsha.
Participants were recruited following identification of consenting adults (≥ 18 years of age), who routinely started tuberculosis treatment in the preceding 3 months (“source case”) at the local clinic. Participants were eligible for enrolment if they were a household child contact between 3 months and 15 years of age. Households were identified through TB source cases (“tuberculosis households”), and matched neighbouring households without known tuberculosis exposure (“neighbouring households”). The ratio between tuberculosis and neighbouring households was approximately 1:1.
We identified tuberculosis households within 2–4 weeks following the adult source case identification, then completed a home visit and collected data on M.tb exposure and demographic characteristics. In addition, all adult household members were screened for symptoms of tuberculosis followed by sputum collection, if they were symptomatic.
Following written informed consent from the parents/caregivers, children aged 3 months – 15 years who were not currently on tuberculosis therapy, were enrolled in the study. Children were deferred for enrolment if there was a) prior TST administration in the preceding 3 months, b) live measles or polio vaccine within the past 6 weeks or c) recent acute illness requiring hospitalization (preceding 6 weeks). Children on isoniazid preventive therapy (IPT) were not excluded, whereas HIV-infected children were.
All children were investigated for M.tb infection and disease using standard protocols [27, 28], including TST, a standard symptom questionnaire , blinded independent dual expert review of chest radiographs (postero-anterior and lateral), sputum or gastric washing for mycobacterial culture (Mycobacterial Growth Indicator Tubes; Becton Dickinson, Sparks, USA), a TST, and clinical examination.
The TST (Mantoux method; 2 tuberculin units purified protein derivative; Statens Serum Institute, Copenhagen) was administered intra-dermally on the volar aspect of the left forearm by trained standardized study nurses, and read within 48–72 hours using the ball-point and ruler method and callipers. The TST was regarded as positive if measuring ≥10 mm in HIV-negative children for clinical care. Unless already known to be HIV-infected, participants were tested for HIV (Abbott Determine Rapid HIV test), followed by a confirmatory laboratory based ELISA/PCR test if positive or indeterminate.
Data were collected to quantify the degree of M.tb exposure (M.tb contact score) [29]. In the absence of a gold standard of infection, we used this score to quantify the degree of exposure in children as a surrogate reference standard for M.tb infection [29–31] [Table 1. The score includes measures of source case infectivity, the average reported duration of exposure to the source case, and the child’s reported proximity to the source case. TST results in children from the study communities were previously shown to be well correlated with this score [29, 30].
We also recorded information on BCG vaccination history and scar presence, previous and current isoniazid preventive therapy, previous tuberculosis treatment, nutritional status (z-scores), household composition, measures of socio-economic status (household assets), and reported history of deworming during the preceding 6 months. Z-scores were calculated with reference to the 2006 World Health Organization Child Growth Standards for children up to five years of age and the 2000 Centres for Disease Control and Prevention growth charts reference population for children that were older than 5 years [32]. Reported socio-economic indicators were based on surveys in our study communities and were used in the absence of reliable data on reported income, given high unemployment rates in these impoverished urban communities.
Sensitization to Ascaris lumbricoides was determined by the ImmunoCAP specific-IgE testing which measures circulating Ascaris-specific IgE concentration in serum. This method was developed for clinical diagnosis and laboratory use where reagins belonging to the IgE antibody class, which develop shortly after exposure, are measured by a fluoroenzymeimmunoassay [33]. Results are expressed as kU/L and are typically categorised in 6 groups (Table 2) or interpreted as positive or negative based on a binary classification (25).
Data analysis
Data analysis was performed using STATA/SE version 12.0 (StataCorp LP, StataCorp, 4905 Lakeway Drive, College Station, Texas 77845 USA). An alpha level of less than or equal to 0.05 was regarded as statistically significant. The main outcome of interest was M.tb infection, measured by a positive TST (≥10 mm). The main exposure of interest, Ascaris IgE, was categorised according to RAST categories and dichotomized (positive if ≥0.35kU/L). This measure, consistent with previous work (25) was used as a measure of Ascaris infection or sensitization.
We assessed the effect of predictors of M.tb infection in univariate analysis, with the primary determinant being Ascaris IgE status in 271 enrolled participants. Child baseline characteristics were described overall, and stratified according to Ascaris IgE status for baseline characteristics. Continuous data were described using mean and standard deviations and median and inter-quartile ranges, dependent on data distribution. Categorical variables were described using frequencies and percentages.
We developed logistic regression models that included Ascaris IgE status, age and the M.tb contact score. These measures were significant during univariate analysis or were clinically or epidemiologically relevant as covariates. Additionally, the developed model was examined for interactions between the explanatory and environmental variables in order to establish if possible effect modification is present. Results of the regression model are presented as adjusted odds ratios (aORs) and corresponding 95 percent confidence intervals (95% CIs).
We complied with the Helsinki Declaration and the study was approved by the Health Research Ethics Committee of the Stellenbosch University (reference number N05/07/129 and N08/08/207).
Results
Of 337 total child participants enrolled, 271 HIV-negative children were included in the analysis (n = 66, 20% were HIV infected and excluded). The median age was 4 years (range: 4 months to 15 years).
Few children (2%) were receiving IPT at the time of enrolment despite the fact that 67% of children were household contacts of a tuberculosis index case currently on therapy. Of children with a documented contact (n = 181), 121 were below 5 years of age and were referred for IPT. Previous IPT use was reported in 9% and 3% had previously received tuberculosis treatment.
Housing and socio-economic indicators indicate the poor living conditions prevalent in these communities: almost 20% of participants did not have access to a fridge or radio at home while almost 5% relied occasionally on selling household assets. Only 68% of children lived in a house with a flushing toilet and 83% had access to piped water in the household. The majority of children resided in formal brick housing (77%) [Table 3].
Ascaris IgE results are described in Table 2. A total of 65 (24%) children were Ascaris IgE positive. Of these, 37% were also TST positive. Most Ascaris IgE positive participants were within RAST range 2 (moderate level of allergen specific IgE) followed by ranges 1 (low level of allergen specific IgE) and 3 (high level of allergen specific IgE) [Table 2]. Of the 8% of children in whom the caregiver reported that the child had passed a worm in the preceding 3 months, most (86%) had been dewormed. Anthropometric measures were not associated with either positive Ascaris or TST status.
Overall, 40% of children were TST positive at enrolment. Children were more likely to have a positive TST if they were older (OR 1.2, p < 0.001), had a higher M.tb contact score (OR 1.2, p < 0.001), had received previous TB treatment (OR 4.8, p = 0.06) or previous IPT (OR 3.2, p = 0.01). A visible BCG scar (OR 0.4, p = 0.01) was associated with reduced odds of infection [Table 4]. There was no significant association between positive Ascaris IgE and positive TST status (OR = 0.9, 95% CI 0.5– 1.6, p = 0.63).
Based on the univariate analysis, we included age, M.tb contact score and binary Ascaris IgE status in a regression model that demonstrated an increased risk for a positive TST in older children (aOR 1.2, 95% CI 1.1 – 1.3) and those with a higher M.tb contact score (aOR 1.2, 95% CI 1.1 – 1.3). This model also showed an inverse association between TST and Ascaris IgE positivity (aOR 0.6, 95% CI 0.1 – 1.1).
A second model including M.tb contact score, age, Ascaris IgE and an age interaction term showed that the effect of age was stronger among those children with a positive Ascaris IgE status. Being Ascaris IgE positive significantly reduced the odds of being TST positive amongst younger children, while this effect weakened as age increased (Table 5).
Discussion
We demonstrate a high prevalence of M.tb and Ascaris lumbricoides infection in children from households with and without documented tuberculosis exposure living in poor urban South African communities. Our results suggest an inverse relationship between Ascaris IgE and TST positive status, which is consistent with our hypothesis.
False-negative TST results might be due to technical factors or a suppressed immune status while false-positive tests may be attributed to BCG vaccination and the effect of non-tuberculous mycobacteria [12]. In our study, a positive TST was associated with increasing age and an increasing M.tb contact score, which is biologically plausible and consistent with other data [30, 34]. The presence of a BCG vaccination scar [35–37] and indicators of higher socio-economic household status [38] protected against having a positive M.tb infection phenotype.
Our multivariable logistic regression adjusting for age, degree of M.tb exposure and previous TB therapy, supports this hypothesis; children with a positive Ascaris IgE appeared to be less likely to mount a positive TST response, especially if they were younger.
In the absence of stool samples, as in this study, serum Ascaris-induced specific IgE is widely used as proxy for Ascaris infection. Ascaris IgE however cannot differentiate previous infection from new infection and/or previous sensitization, and therefore assumes Ascaris infection and Th2 polarization without information regarding the time of infection [39], similar to measures of M.tb infection. Additionally potential cross-reactivity due to Trichiuris trichiura infection cannot be excluded [40]. Despite these limitations, Ascaris IgE responses remain a useful proxy for immunological and epidemiological studies, and are a standard and widely used indication of Ascaris exposure/infections.
Despite universal clinic access to deworming and school- based deworming programs, the positive Ascaris IgE levels of 24%, although lower than previously reported from these communities [26], are high and consistent with WHO definitions for a helminth endemic country [9]. Deworming may not be practised as regularly as required (at least once a year), as indicated by the low proportion of caregivers (7%) who had reported deworming of the child in the preceding 3 months. On the other hand, helminth re-exposure and infection, given the poor socio-economic circumstances is also possible [9, 38]. These factors should be investigated in longitudinal studies with repeat measures of infection.
Older children (OR 1.2, p < 0.001) were more likely to be Ascaris positive which we attribute to the age-related risk of infection and immune system responsiveness, and possibly due to behavioural patterns (i.e. more outdoor activities in shared environments like schools and sports fields).
Few children were on IPT at enrolment which could reflect the active contact tracing strategy used by the study; however previous studies from these communities indicate poor IPT uptake and adherence in young children under routine programmatic conditions [41–43].
This study is limited by its cross-sectional nature, the limited sample size and the exclusion of HIV-infected children, due to small numbers. The enrolment strategy was purposeful to ensure a high proportion of children with recent M.tb exposure and included children from neighbouring “control” households as a measure of background M.tb transmission. Finally, the proxy used for Ascaris in our study does not apply to all potential helminth species, and might underestimate the general and differential effect of helminth infection. Deworming was only reported on a questionnaire basis and its impact on mycobacterial and other immune responses could therefore not be rigorously evaluated.
In light of these limitations, these results need to be verified in paediatric cohort studies, preferably with additional measures of helminth infection including stool samples and the standard evaluation of the effect of deworming on mycobacterial immune responses.
Conclusions
The results support our hypothesis that helminth infection may change immune responses in children. This may play a clinically measureable role in widely used immune diagnostic tests that measures M.tb infection, especially in high prevalence tuberculosis and helminth infection settings.
Abbreviations
- 95% CI:
-
95 percent confidence interval
- aOR:
-
Adjusted odds ratio
- BCG:
-
Bacillus Calmette-Guérin
- IMCI:
-
Integrated Management of Childhood Illness
- IPT:
-
Isoniazid preventive therapy
- M.tb :
-
Mycobacterium tuberculosis
- OR:
-
Odds ratio
- R/U:
-
Ravensmead and Uitsig
- Site C:
-
Site C, Khayelitsha
- TB:
-
Tuberculosis
- Th1:
-
T helper cell type 1
- Th2:
-
T helper cell type 2
- TST:
-
Tuberculin skin test
- WHO:
-
World Health Organisation.
References
WHO: Global tuberculosis control: WHO report 2010. 2010, Geneva, Switzerland: World Health Organization
Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, Dye C: The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003, 163 (9): 1009-1021. 10.1001/archinte.163.9.1009.
Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Starke JJ, Enarson DA, Donald PR, Beyers N: The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004, 8 (4): 392-402.
Appleton CC, Mosala TI, Levin J, Olsen A: Geohelminth infection and re-infection after chemotherapy among slum-dwelling children in Durban, South Africa. Ann Trop Med Parasitol. 2009, 103 (3): 249-261. 10.1179/136485909X398212.
Saathoff E, Olsen A, Kvalsvig JD, Appleton CC: Patterns of geohelminth infection, impact of albendazole treatment and re-infection after treatment in schoolchildren from rural KwaZulu-Natal/South-Africa. BMC Infect Dis. 2004, 4: 27-10.1186/1471-2334-4-27.
Albonico M, Allen H, Chitsulo L, Engels D, Gabrielli AF, Savioli L: Controlling soil-transmitted helminthiasis in pre-school-age children through preventive chemotherapy. PLoS Negl Trop Dis. 2008, 2 (3): e126-10.1371/journal.pntd.0000126.
Ezeamama AE, Friedman JF, Acosta LP, Bellinger DC, Langdon GC, Manalo DL, Olveda RM, Kurtis JD, McGarvey ST: Helminth infection and cognitive impairment among Filipino children. AmJTrop Med Hyg. 2005, 72 (5): 540-548.
Jardim-Botelho A, Raff S, Rodrigues Rde A, Hoffman HJ, Diemert DJ, Correa-Oliveira R, Bethony JM, Gazzinelli MF: Hookworm, Ascaris lumbricoides infection and polyparasitism associated with poor cognitive performance in Brazilian schoolchildren. Trop Med Int Health. 2008, 13 (8): 994-1004. 10.1111/j.1365-3156.2008.02103.x.
WHO: Weekly epidemiological record. 2010, 141-148. 85
WHO: Integrated Management of Childhood Illness. 2008
Young DB, Gideon HP, Wilkinson RJ: Eliminating latent tuberculosis. Trends Microbiol. 2009, 17 (5): 183-188. 10.1016/j.tim.2009.02.005.
Tuberculosis: A Comprehensive Clinical Reference. Edited by: Schaaf HS, Zumla A. 2009
Lewinsohn DA, Gennaro ML, Scholvinck L, Lewinsohn DM: Tuberculosis immunology in children: diagnostic and therapeutic challenges and opportunities. Int J Tuberc Lung Dis. 2004, 8 (5): 658-674.
Winek J, Demkow U, Rowinska-Zakrzewska E, Szolkowska M, Filewska M, Jagodzinski J, Roszkowski-Sliz K: Comparison of Th1 and Th2 response in the blood of tuberculous patients and healthy contacts. Pneumonol Alergol Pol. 2009, 77 (5): 446-452.
Elias D, Mengistu G, Akuffo H, Britton S: Are intestinal helminths risk factors for developing active tuberculosis?. Trop Med Int Health. 2006, 11 (4): 551-558. 10.1111/j.1365-3156.2006.01578.x.
Demissie A, Abebe M, Aseffa A, Rook G, Fletcher H, Zumla A, Weldingh K, Brock I, Andersen P, Doherty TM: Healthy Individuals That Control a Latent Infection with Mycobacterium tuberculosis Express High Levels of Th1 Cytokines and the IL-4 Antagonist IL-4{delta}2. J Immunol. 2004, 172 (11): 6938-6943.
Wigginton JE, Kirschner D: A model to predict cell-mediated immune regulatory mechanisms during human infection with Mycobacterium tuberculosis. J Immunol. 2001, 166 (3): 1951-1967.
Yazdanbakhsh M, van den Biggelaar A, Maizels RM: Th2 responses without atopy: immunoregulation in chronic helminth infections and reduced allergic disease. Trends Immunol. 2001, 22 (7): 372-377. 10.1016/S1471-4906(01)01958-5.
Borkow G, Leng Q, Weisman Z, Stein M, Galai N, Kalinkovich A, Bentwich Z: Chronic immune activation associated with intestinal helminth infections results in impaired signal transduction and anergy. J Clin Invest. 2000, 106 (8): 1053-1060. 10.1172/JCI10182.
Cooper PJ, Chico ME, Sandoval C, Espinel I, Guevara A, Kennedy MW, Urban JF, Griffin GE, Nutman TB: Human infection with Ascaris lumbricoides is associated with a polarized cytokine response. J Infect Dis. 2000, 182 (4): 1207-1213. 10.1086/315830.
Resende Co T, Hirsch CS, Toossi Z, Dietze R, Ribeiro-Rodrigues R: Intestinal helminth co-infection has a negative impact on both anti-Mycobacterium tuberculosis immunity and clinical response to tuberculosis therapy. Clin Exp Immunol. 2007, 147 (1): 45-52.
Wright VJ, Ame SM, Haji HS, Weir RE, Goodman D, Pritchard DI, Mohamed MR, Haji HJ, Tielsch JM, Stoltzfus RJ, et al: Early exposure of infants to GI nematodes induces Th2 dominant immune responses which are unaffected by periodic anthelminthic treatment. PLoS Negl Trop Dis. 2009, 3 (5): e433-10.1371/journal.pntd.0000433.
Tristao-Sa R, Ribeiro-Rodrigues R, Johnson LT, Pereira FE, Dietze R: Intestinal nematodes and pulmonary tuberculosis. Rev Soc Bras Med Trop. 2002, 35 (5): 533-535. 10.1590/S0037-86822002000500020.
Potian JA, Rafi W, Bhatt K, McBride A, Gause WC, Salgame P: Preexisting helminth infection induces inhibition of innate pulmonary anti-tuberculosis defense by engaging the IL-4 receptor pathway. The Journal of Experimental Medicine. 2011, 208 (9): 1863-1874. 10.1084/jem.20091473.
Neto LM, Oliveira Rde V, Totino PR, Sant'Anna FM, Coelho Vde O, Rolla VC, Zanini GM: Enteroparasitosis prevalence and parasitism influence in clinical outcomes of tuberculosis patients with or without HIV co-infection in a reference hospital in Rio de Janeiro (2000–2006). Braz J Infect Dis. 2009, 13 (6): 427-432.
Adams VJ, Markus MB, Adams JF, Jordaan E, Curtis B, Dhansay MA, Obihara CC, Fincham JE: Paradoxical helminthiasis and giardiasis in Cape Town, South Africa: epidemiology and control. Afr Health Sci. 2005, 5 (3): 276-280.
Marais BJ, Gie RP, Hesseling AC, Schaaf HS, Enarson DA, Beyers N: Radiographic signs and symptoms in children treated for tuberculosis: possible implications for symptom-based screening in resource-limited settings. Pediatr Infect Dis J. 2006, 25 (3): 237-240. 10.1097/01.inf.0000202140.76368.74.
Marais BJ, Gie RP, Hesseling AC, Schaaf HS, Lombard C, Enarson DA, Beyers N: A refined symptom-based approach to diagnose pulmonary tuberculosis in children. Pediatrics. 2006, 118 (5): e1350-1359. 10.1542/peds.2006-0519.
Mandalakas AM, Kirchner HL, Lombard C, Walzl G, Grewal HMS, Gie RP, Hesseling AC: Well-quantified tuberculosis exposure is a reliable surrogate measure for tuberculosis infection. Int J Tuberc Lung Dis. 2012, 16 (7):
Hesseling AC, Mandalakas AM, Kirchner HL, Chegou NN, Marais BJ, Stanley K, Zhu X, Black G, Beyers N, Walzl G: Highly discordant T cell responses in individuals with recent exposure to household tuberculosis. Thorax. 2009, 64 (10): 840-846. 10.1136/thx.2007.085340.
Shams H, Weis SE, Klucar P, Lalvani A, Moonan PK, Pogoda JM, Ewer K, Barnes PF: Enzyme-linked immunospot and tuberculin skin testing to detect latent tuberculosis infection. Am J Respir Crit Care Med. 2005, 172 (9): 1161-1168. 10.1164/rccm.200505-748OC.
Kuczmarski RJ, Ogden CL, Guo SS, et al: 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002, 11 (246):
ImmunoCAP Specific IgE Fluoroenzymeimmunoassay Calibration Range 0=100kU/l. 2008, Uppsala, Sweden: Phadia AB
Mandalakas AM, Detjen AK, Hesseling AC, Benedetti A, Menzies D: Interferon-gamma Release Assays and Childhood Tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2011, 15 (8): 1018-32. 10.5588/ijtld.10.0631.
Lalvani A, Bakir M, Millington KA, Dosanjh D, Soysal A: BCG and protection against Mycobacterium tuberculosis infection. Lancet. 2006, 367 (9508): 391-392.
Jeremiah K, Praygod G, Faurholt-Jepsen D, Range N, Andersen AB, Grewal HM, Friis H: BCG vaccination status may predict sputum conversion in patients with pulmonary tuberculosis: a new consideration for an old vaccine?. Thorax. 2010, 65 (12): 1072-1076. 10.1136/thx.2010.134767.
Soysal A, Millington KA, Bakir M, Dosanjh D, Aslan Y, Deeks JJ, Efe S, Staveley I, Ewer K, Lalvani A: Effect of BCG vaccination on risk of Mycobacterium tuberculosis infection in children with household tuberculosis contact: a prospective community-based study. Lancet. 2005, 366 (9495): 1443-1451. 10.1016/S0140-6736(05)67534-4.
Mahomed H, Hawkridge T, Verver S, Geiter L, Hatherill M, Abrahams DA, Ehrlich R, Hanekom WA, Hussey GD: SATVI Adolescent Study Team: Predictive factors for latent tuberculosis infection among adolescents in a high-burden area in South Africa. Int J Tuberc Lung Dis. 2011, 15: 331-336.
Haswell-Elkins MR, Leonard H, Kennedy MW, Elkins DB, Maizels RM: Immunoepidemiology of Ascaris lumbricoides: relationships between antibody specificities, exposure and infection in a human community. Parasitology. 1992, 104 (Pt 1): 153-159.
Figueiredo CA, Barreto ML, Rodrigues LC, Cooper PJ, Silva NB, Amorim LD, Alcantara-Neves NM: Chronic Intestinal Helminth Infections Are Associated with Immune Hyporesponsiveness and Induction of a Regulatory Network. Infect Immun. 2010, 78 (no 7): 3160-3167. 10.1128/IAI.01228-09.
van Zyl S, Marais BJ, Hesseling AC, Gie RP, Beyers N, Schaaf HS: Adherence to anti-tuberculosis chemoprophylaxis and treatment in children. Int J Tuberc Lung Dis. 2006, 10 (1): 13-18.
Marais BJ, van Zyl S, Schaaf HS, van Aardt M, Gie RP, Beyers N: Adherence to isoniazid preventive chemotherapy: a prospective community based study. Arch Dis Child. 2006, 91 (9): 762-765. 10.1136/adc.2006.097220.
Van Wyk SS, Hamade H, Hesseling AC, Beyers N, Enarson DA, Mandalakas AM: Recording isoniazid preventive therapy delivery to children: operational challenges. Int J Tuberc Lung Dis. 2010, 14 (5): 650-653.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/12/211/prepub
Acknowledgements
We would like to thank all study participants from the study communities, the health care personnel from City of Cape Town Health Directorate and the clinical, data and laboratory team at the Desmond Tutu TB Centre. This study was made possible by generous grants from the Norwegian Cooperation for Higher Education (NUFUPRO-2007/10183), National Institute of Allergy and Infectious Disease at the National Institutes of Health [R01A076199] and the German Research Foundation (DFG) (JA 1479/3-1).
During this period NVS was supported through an operational research course, which was jointly developed and run by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease, and the Operational Research Unit, Medecins sans Frontieres, Brussels as well as through an operational research fellowship from the Centre for Operational Research.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
All authors declare that they have no competing interests.
Authors’ contributions
NVS was involved in study design, data analysis, interpretation and manuscript preparation and primarily responsible for manuscript writing. AMM participated in design, implementation, analysis and writing. HLK participated in analysis, interpretation and writing. GW participated in design, writing and interpretation. HMSG was involved in study design and interpretation. MJ participated in writing and interpretation. ACH participated as academic supervisor in all phases of the study and manuscript preparation including design, implementation, analysis and writing. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
van Soelen, N., Mandalakas, A.M., Kirchner, H.L. et al. Effect of Ascaris Lumbricoides specific IgE on tuberculin skin test responses in children in a high-burden setting: a cross-sectional community-based study. BMC Infect Dis 12, 211 (2012). https://doi.org/10.1186/1471-2334-12-211
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-12-211