Abstract
Background
Delirium is a neuropsychiatric syndrome frequently observed in elderly hospitalised patients and can be found in any medical condition. Due to the severe consequences, early recognition of delirium is important in order to start treatment in time. Despite the high incidence rate, the occurrence of delirium is not always identified as such. Knowledge of potential risk factors is important. The aim of the current study is to determine factors associated with the occurrence of a prevalent delirium among elderly patients acutely admitted to an internal medicine ward.
Methods
All consecutive patients of 65 years and over acutely admitted to the Department of Internal Medicine of the Academic Medical Centre, Amsterdam, a university hospital, were asked to participate. The presence of delirium was determined within 48 hrs after admission by an experienced geriatrician.
Results
In total, 126 patients were included, 29% had a prevalent delirium after acute admission. Compared to patients without delirium, patients with delirium were older, more often were cognitively and physically impaired, more often were admitted due to water and electrolyte disturbances, and were less often admitted due to malignancy or gastrointestinal bleeding. Independent risk factors for having a prevalent delirium after acute admission were premorbid cognitive impairment, functional impairment, an elevated urea nitrogen level, and the number of leucocytes.
Conclusions
In this study, the most important independent risk factors for a prevalent delirium after acute admission were cognitive and physical impairment, and a high serum urea nitrogen concentration. These observations might contribute to an earlier identification and treatment of delirium in acutely admitted elderly patients.
Similar content being viewed by others
Background
Delirium is a complex neuropsychiatric syndrome with an acute onset, characterized by disturbances of consciousness, attention, cognition, and perception. Delirium can be found in any medical condition and is the most common reason for acute cognitive dysfunction in hospitalised elderly patients [1–3]. This syndrome occurs in about 10 to 25% of all acute admissions to a general hospital. The frequency in older patients is higher, 20% to 40% [4]. Due to the aging of the population, the absolute number may increase in the future.
Delirium has been associated with a poor outcome: prolonged hospitalisation, decreased cognitive and physical functioning, increased nursing home admission, and with a threefold higher morbidity and mortality risk [5, 6]. Due to the severe consequences, recognition of delirium is important to start treatment in time. Despite the high incidence rate, the occurrence of delirium is not always identified. Several studies reported that between 32% and 67% of delirious patients were not recognized by their physicians [7, 8]. There are a number of hypotheses for this lack of recognition. First, delirium is not always regarded as an important clinical syndrome, because it is varied and the multiple aetiology defies the classic disease model to look for a single cause of disease. In addition, delirium is often believed to present with agitation, hallucination, and inappropriate behaviour, whereas it also often presents with lethargy and decreased activity. Finally, the fluctuating course of the delirium may confound the diagnosis [9].
The patho-physiology of delirium is still poorly understood, although a number of mechanisms have been hypothesized. Delirium might be the result of changes in neurotransmitter systems, in cytokines, and in the lipid metabolism [10–16]. Delirium and Alzheimer's disease (AD) may share several patho-physiological features as they share several symptoms [17]. Moreover, preliminary results support the assumption that genetic variation plays a role [18].
Several studies have examined risk factors that might predispose, or influence the development of delirium. A systematic review identified 27 articles studying 61 different risk factors [19]. Results of these 27 studies were not conclusive. Most studies found an increased risk for delirium in dementia, medical illness, and alcohol abuse. For risk factors like medication, male gender, or serum concentrations, of e.g. urea, creatinine, sodium, potassium or glucose, some studies did find an increased risk for delirium, whereas other studies did not find an increased risk of these factors [20–23]. Finally, most of these studies determined risk factor for new-onset delirium in hospitalised patients [24, 25]. Yet, prevalent delirium can be a major problem as well, especially among acutely admitted patients. A prompt recognition of the syndrome is important to initiate appropriate treatment as soon as possible. Therefore, more knowledge of potential risk factors for acutely admitted patients is important.
The aim of the current study is to determine factors associated with a prevalent delirium among acutely admitted elderly patients to an internal medicine ward.
Methods
Patients
All consecutive patients of 65 years and over acutely admitted to the Department of Internal Medicine of the Academic Medical Centre, Amsterdam, a university teaching hospital, were invited. Patients admitted to our hospital are sometimes referred because of the university function, but about 60% are directly admitted to our hospital. Patients were excluded from the study if they were unable to speak or understand Dutch or English, if they or their relatives did not give permission for the study, if they came from or were transferred to another ward than Internal Medicine, or left the ward within 48 hours. Due to logistic limitations, a random sample of included patients was taken for the current study regarding risk factors and genetic variation. More detailed information regarding medication and DNA was collected of these selected patients. Inclusion period was between January 2003 and February 2004. Before enrolment, informed consent was obtained from the patient or substitute decision-maker. The hospital's Medical Ethics Committee approved the study.
Procedures
Members of the team completed an initial multidisciplinary evaluation for all study participants within 48 hrs after admission. The team was composed of a geriatric physician, a fellow in geriatric medicine, and two research nurses trained in geriatric medicine. Demographic and clinical data were collected. Severity and number of comorbidities were scored with the Charlson comorbidity index [26]. The final score was divided in 3 categories; mild (0 or 1 point), moderate (2 or 3 points) and severe (more than 3 points). Biochemistry values, i.e. urea nitrogen, creatinine, glucose, haemoglobin, natrium, and potassium concentrations, and leucocytes count were obtained from a serum blood taken within 48 hrs after admission.
Within 48 hrs after admission, the research nurses interviewed patients, medical and nursing staff. Cognitive impairment was recorded by two validated instruments (MMSE, IQCODE) at the time of hospital admission. The MMSE (Mini Mental State Examination) is the most widely used screening instrument for detection of cognitive impairment in the elderly [27]. Many studies have shown that the MMSE has got a high construct validity and test-retest reliability [28]. The MMSE measures cognitive functioning on a scale of 0 (poor) to 30 (excellent), with a score less than 24 indicating cognitive impairment. The IQCODE (Informant Questionnaire on COgnitive DEcline) assesses the possible presence of dementia before admission based on the response of an informant who had known the patient for at least ten years and could assess any decline in memory or cognition [29]. The informant was asked to recollect the situation 2 weeks before admission and to compare it with the situation 10 years before. The score is an average of the 16-item scores, each rated from 1 (much improved) to 5 (much worse). Patients with a mean score of 3.9 or more were considered to have dementia [30]. Final classification for having cognitive impairment was based on the MMSE score for patients without delirium, whereas for patients with delirium, the combination of both instruments (MMSE and IQCODE) was applied. In case of conflicting outcome, the score of the IQCODE was used.
The geriatric physician or the fellow scored the presence of delirium within 48 hrs after admission with the CAM (Confusion Assessment Method). The CAM is a structured interview of delirium symptoms based on the Diagnostic and Statistical Manual of Mental Disorders criteria (DSM-III-R). This instrument have been found reliable, sensitive and specific [31]. The delirium could have been present at admission, or developed within 48 hrs after admission.
The KATZ ADL scale is a 15-item scale for measuring functional status in a geriatric population. The KATZ-ADL consists of one scale for patients and one for their relative or informant [32]. KATZ-ADL as scored by the informant of a patient was taken as the final ADL score. In case this score was missing, the KATZ-ADL score of the patient was taken. Once more, the informant was asked to recall the situation 2 weeks before admission. The nurses that collected the risk scores were blinded to the presence or absence of delirium in the patient.
All medication before hospital admission was registered. The number of prescribed drugs was scored. Psychopharmaca included benzodiazepines, antidepressive medication such as selective serotonin reuptake inhibitors and tricyclic antidepressants, and antipsychotic medication.
Based on the literature and our clinical experience, we predefined five different types of drugs as suspected of being a high-risk drug for obtaining delirium [33–35]; namely anticholinergic medication, benzodiazepines, narcotic analgetics, corticosteroids and antihistaminics. Cholinergic drugs were classified according to the list of Han et al.[35], all drugs scored with 3 points were considered cholinergic drugs. We completed this list with parasympathicolytics. Benzodiazepines included sedative-hypnotics and anxiolytics. The antihistamincs group contains only H1 receptor blocking agents.
Statistical analysis
Standard descriptive statistics were used. Univariate and multivariate logistic regression analysis was performed to identify risk factors of delirium. All variables with a p-value <0.20 in the univariate analysis were used in the multivariate model. A backward elimination procedure was used to define the final risk factors. All variables with a p-value >0.10 were eliminated from the model. To confirm the final risk factors, the multiple logistic regression analysis was repeated with a forward selection procedure (all variables with a p-value <0.10 were included).
Results
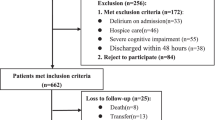
During the inclusion period 576 patients were admitted to the internal ward. Of these patients, 88 patients came from another ward, resulting in 488 eligible patients. 182 patients were not included because no informed consent was given or they were unable to speak or understand Dutch or English. In total, 306 patients were included, a random sample of 126 patients was selected for the current study. Non-selected and selected patients were similar regarding mean age, the percentages male, and the frequency of patients with a prevalent delirium. Mean age of the non-selected patients was 78.1 (SD: 8.5), 45% were male and 28% of these patients had a prevalent delirium after acute hospital admission. For the 126 selected patients mean age was 79.1 (7.8), 41% were male and 36 patients (29%) had a prevalent delirium after acute hospital admission.
Baseline characteristics of the 126 selected patients with and without a prevalent delirium are presented in Table 1. Patients with delirium were significantly older, had more often cognitive impairment, and were more impaired in daily activities compared to patients without delirium. Reason for admission was less frequently a malignancy, or a gastrointestinal bleeding, and more frequently water or electrolyte disturbances for patients with delirium. On average, delirious patients had a significantly higher level of serum urea nitrogen at admission.
Table 2 presents the type of medication prescribed to more than 20% of the patients. The majority of the most frequently prescribed drugs are similar for patients with and without delirium, except for psychopharmaca. This type of drugs is prescribed to 31% of the patients with delirium, whereas 17% of the patients without delirium were taking these drugs. Patients without a prevalent delirium were on nearly 5 different prescribed drugs before admission, whereas delirious patients were taking on average 4.4 different drugs before admission. This difference was not statistically significant.
Information on the number of patients taking one or more of the predefined high-risk medications is presented in Table 3. Delirious patients obtained more often drugs suspected of being a drug with a high risk, especially benzodiazepines, 17% versus 10%, and narcotic analgetics (14% versus 7%). Yet these differences were not significant.
Based on univariate logistic regression analysis, risk factors for a prevalent delirium after acute admission are higher age, cognitive impairment, impaired physical functioning, admission reason, and urea nitrogen level (Table 4). No increased risk was observed for mean number of prescribed drugs, or the use of drugs suspected of being a high-risk drug. Results of the multivariate logistics regression analysis are presented in Table 5. Independent predictors for an increased risk for a prevalent delirium after acute admission were cognitive impairment, impaired physical functioning, increased urea nitrogen level, and the number of leucocytes. The backward and the forward selection procedure resulted in the same final risk factors (data not shown).
Discussion
In this prospective cohort study, nearly 30% of acutely admitted elderly patients had delirium within 48 hrs after admission. Increased risk for developing delirium was found for cognitive and physical impairment, elevated urea nitrogen level, and the number of leucocytes. No increased risk for developing delirium was noticed for comorbidity or type or number of medication.
A possible reason for not finding an increased risk of comorbidity could be the limited number of included patients. The use of a more liberal inclusion criteria in the multivariate logistic regression analysis, elimination of all variables with a p-value >0.15, resulted into the same final model. In the literature, inconclusive results can be found regarding the impact of the severity of the disease on the risk of delirium [20, 23–25]. So, the limited number of included patients does not seem to be the sole reason for no association between comorbidity and the risk of delirium. Another possible explanation could be the balancing relationship of comorbidity with cognitive impairment. The more cognitive impaired, the less physical illness might be needed to become delirious.
No effect of type or number of drugs prescribed on the risk of delirium was observed. In the current literature, results on the association between anticholinergic drugs and delirium are conflicting. Both in patients with an incident as in patients with a prevalent delirium, some studies did find an increased risk [33, 34, 36], whereas other studies did not find an effect of anticholinergic drugs [22, 23, 37, 38]. In addition, it could be possible that not just the medication type itself is associated with the risk of delirium, but rather the dosage of the medication, or a recent change in type or dosage of prescribed medication. We did not collect data on these detailed topics, nor did we collect the compliance of the patient to the prescribed medication.
Most studies report an increased risk associated with older age. A reason for not confirming this finding is the strong correlation between age and impaired physical functioning in our study. Indeed, if we excluded the KATZ ADL score, higher age is an independent risk factor for having delirium within 48 hrs after admission.
Our results could have been obscured due to selectively inclusion of patients, as not all patients gave informed consent. However, we found that nearly 30% of the acutely admitted patients had a prevalent delirium after acute admission. This finding is in concordance with the literature; a frequency between 20% and 40% is usually found. Moreover, the frequency in demented patients was much higher, 46% of these patients had delirium. This finding is supported by the literature as well.
Cognitive impairment was the strongest risk factor for a prevalent delirium; we found a ninefold increased risk. This effect is also reported in other studies for the development of delirium after admission. The amount of reported increased risk varies between 2.8 and 9.0 [20, 23, 24]. An increased urea nitrogen level was associated with an increased risk of a prevalent delirium. A most likely explanation for this finding is that an increased urea nitrogen concentration is, among others, an indication of dehydration. The effect of dehydration on risk of delirium was found in other studies as well [7, 24, 39]. Moreover, if we did not take urea nitrogen level in the multivariate analysis, we find a significant increased risk for the admission reason water and electrolyte disturbances (data not shown). Finally, we found that a higher number of leucocytes was associated with a lower risk of delirium. We cannot explain this finding, we speculate that this might be due to the higher percentages of non-delirious patients with infectious diseases and malignancies, both associated with a higher level of leucocytes. Indeed, the highest leucocytes counts were found in the non-delirious patients with reason of admission malignancy or infectious disease.
Conclusions
In this study the independent risk factors for a prevalent delirium after acute admission are premorbid cognitive and physical impairment, and a high urea nitrogen level. These observations might contribute to an earlier identification and treatment of delirium in acutely admitted elderly patients.
Role of the funding source
Funding source was our own hospital, it was an unrestricted grant.
References
Liptzin B, Levkoff SE: An empirical study of delirium subtypes. Br J Psychiatry. 1992, 161: 843-845.
Sandberg O, Gustafson Y, Brannstrom B, Bucht G: Clinical profile of delirium in older patients. J Am Geriatr Soc. 1999, 47: 1300-1306.
Meagher DJ, O'Hanlon D, O'Mahony E, Casey PR, Trzepacz PT: Relationship between etiology and phenomenologic profile in delirium. J Geriatr Psychiatry Neurol. 1998, 11: 146-149.
Fick DM, Agostini JV, Inouye SK: Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002, 50: 1723-1732. 10.1046/j.1532-5415.2002.50468.x.
Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK: The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001, 27: 1892-1900. 10.1007/s00134-001-1132-2.
Francis J, Kapoor WN: Prognosis after hospital discharge of older medical patients with delirium. J Am Geriatr Soc. 1992, 40: 601-606.
Inouye SK, Bogardus ST, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM: A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999, 340: 669-676. 10.1056/NEJM199903043400901.
Armstrong SC, Cozza KL, Watanabe KS: The misdiagnosis of delirium. Psychosomatics. 1997, 38: 433-439.
Inouye SK: The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994, 97: 278-288. 10.1016/0002-9343(94)90011-6.
Flacker JM, Lipsitz LA: Neural mechanisms of delirium: current hypotheses and evolving concepts. J Gerontol A Biol Sci Med Sci. 1999, 54: B239-B246.
van der Mast RC: Pathophysiology of delirium. J Geriatr Psychiatry Neurol. 1998, 11: 138-145.
Roche V: Southwestern Internal Medicine Conference. Etiology and management of delirium. Am J Med Sci. 2003, 325: 20-30.
van der Mast RC, van den Broek WW, Fekkes D, Pepplinkhuizen L, Habbema JD: Is delirium after cardiac surgery related to plasma amino acids and physical condition?. J Neuropsychiatry Clin Neurosci. 2000, 12: 57-63.
van der Mast RC, Fekkes D, Moleman P, Pepplinkhuizen L: Is postoperative delirium related to reduced plasma tryptophan?. Lancet. 1991, 338: 851-852. 10.1016/0140-6736(91)91504-N.
Mortazavi S, Thompson J, Baghdoyan HA, Lydic R: Fentanyl and morphine, but not remifentanil, inhibit acetylcholine release in pontine regions modulating arousal. Anesthesiology. 1999, 90: 1070-1077. 10.1097/00000542-199904000-00021.
Wang JC, Kwon JM, Shah P, Morris JC, Goate A: Effect of APOE genotype and promoter polymorphism on risk of Alzheimer's disease. Neurology. 2000, 55: 1644-1649.
Eikelenboom P, Hoogendijk WJ: Do delirium and Alzheimer's dementia share specific pathogenetic mechanisms?. Dement Geriatr Cogn Disord. 1999, 10: 319-324. 10.1159/000017162.
Gorwood P, Limosin F, Batel P, Hamon M, Ades J, Boni C: The A9 allele of the dopamine transporter gene is associated with delirium tremens and alcohol-withdrawal seizure. Biol Psychiatry. 2003, 53: 85-92. 10.1016/S0006-3223(02)01440-3.
Elie M, Cole MG, Primeau FJ, Bellavance F: Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998, 13: 204-212. 10.1046/j.1525-1497.1998.00047.x.
Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM, Donaldson MC, Whittemore AD, Sugarbaker DJ, Poss R: A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994, 271: 134-139. 10.1001/jama.271.2.134.
Dyer CB, Ashton CM, Teasdale TA: Postoperative delirium. A review of 80 primary data-collection studies. Arch Intern Med. 1995, 155: 461-465. 10.1001/archinte.155.5.461.
Francis J, Martin D, Kapoor WN: A prospective study of delirium in hospitalized elderly. JAMA. 1990, 263: 1097-1101. 10.1001/jama.263.8.1097.
Schor JD, Levkoff SE, Lipsitz LA, Reilly CH, Cleary PD, Rowe JW, Evans DA: Risk factors for delirium in hospitalized elderly. JAMA. 1992, 267: 827-831. 10.1001/jama.267.6.827.
Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME: A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993, 119: 474-481.
Inouye SK, Charpentier PA: Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996, 275: 852-857. 10.1001/jama.275.11.852.
Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987, 40: 373-383. 10.1016/0021-9681(87)90171-8.
Folstein MF, Folstein SE, McHugh PR: "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975, 12: 189-198. 10.1016/0022-3956(75)90026-6.
Tombaugh TN, McIntyre NJ: The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992, 40: 922-935.
Jorm AF, Jacomb PA: The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med. 1989, 19: 1015-1022.
de Jonghe JF: Differentiating between demented and psychiatric patients with the Dutch version of the IQCODE. Int J Geriatr Psychiatry. 1997, 12: 462-465. 10.1002/(SICI)1099-1166(199704)12:4<462::AID-GPS510>3.0.CO;2-Q.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI: Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990, 113: 941-948.
Weinberger M, Samsa GP, Schmader K, Greenberg SM, Carr DB, Wildman DS: Comparing proxy and patients' perceptions of patients' functional status: results from an outpatient geriatric clinic. J Am Geriatr Soc. 1992, 40: 585-588.
Tune LE, Damlouji NF, Holland A, Gardner TJ, Folstein MF, Coyle JT: Association of postoperative delirium with raised serum levels of anticholinergic drugs. Lancet. 1981, 2: 651-653. 10.1016/S0140-6736(81)90994-6.
Tune LE, Bylsma FW: Benzodiazepine-induced and anticholinergic-induced delirium in the elderly. Int Psychogeriatr. 1991, 3: 397-408. 10.1017/S1041610291000832.
Han L, McCusker J, Cole M, Abrahamowicz M, Primeau F, Elie M: Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. 2001, 161: 1099-1105. 10.1001/archinte.161.8.1099.
Trzepacz PT: Anticholinergic Model For Delirium. Semin Clin Neuropsychiatry. 1996, 1: 294-303.
Marcantonio ER, Juarez G, Goldman L, Mangione CM, Ludwig LE, Lind L, Katz N, Cook EF, Orav EJ, Lee TH.: The relationship of postoperative delirium with psychoactive medications. JAMA. 1994, 272: 1518-1522. 10.1001/jama.272.19.1518.
Kolbeinsson H, Jonsson A: Delirium and dementia in acute medical admissions of elderly patients in Iceland. Acta Psychiatr Scand. 1993, 87: 123-127.
Cook DJ, Rooke GA: Priorities in perioperative geriatrics. Anesth Analg. 2003, 96: 1823-1836. 10.1213/01.ANE.0000063822.02757.41.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2318/5/6/prepub
Acknowledgements
The authors wish to thank the research nurses of the department of internal medicine for their assistance in the logistics and data collection of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The author(s) declare that they have no competing interests.
Authors' contributions
SR is the principal investigator of the study; she designed the protocol, supervised its progress, and was involved in the acquisition of the data. BM was involved in the planning of the study and the acquisition of the data. JK was responsible for the statistical analysis. JK and BM drafted the manuscript. All authors contributed to the interpretation of the data, revisions of the paper, and read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Korevaar, J.C., van Munster, B.C. & de Rooij, S.E. Risk factors for delirium in acutely admitted elderly patients: a prospective cohort study. BMC Geriatr 5, 6 (2005). https://doi.org/10.1186/1471-2318-5-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2318-5-6