Abstract
Background
Impairment in activities of daily living (ADL) is an important predictor of outcomes although many administrative databases lack information on ADL function. We evaluated the impact of ADL function on predicting postoperative mortality among older adults with hip fractures in Ontario, Canada.
Methods
Sociodemographic and medical correlates of ADL impairment were first identified in a population of older adults with hip fractures who had ADL information available prior to hip fracture. A logistic regression model was developed to predict 360-day postoperative mortality and the predictive ability of this model were compared when ADL impairment was included or omitted from the model.
Results
The study sample (N = 1,329) had a mean age of 85.2 years, were 72.8% female and the majority resided in long-term care (78.5%). Overall, 36.4% of individuals died within 360 days of surgery. After controlling for age, sex, medical comorbidity and medical conditions correlated with ADL impairment, addition of ADL measures improved the logistic regression model for predicting 360 day mortality (AIC = 1706.9 vs. 1695.0; c -statistic = 0.65 vs 0.67; difference in - 2 log likelihood ratios: χ2 = 16.9, p = 0.002).
Conclusions
Direct measures of ADL impairment provides additional prognostic information on mortality for older adults with hip fractures even after controlling for medical comorbidity. Observational studies using administrative databases without measures of ADLs may be potentially prone to confounding and bias and case-mix adjustment for hip fracture outcomes should include ADL measures where these are available.
Similar content being viewed by others
Background
Several disease processes can lead to functional impairments in basic activities of daily living (ADLs) [1] and impairments in ADLs are common among older adults living in community [2–4] and long-term care (LTC) [5, 6] settings. Measures of ADL impairment are important in observational studies as ADL may be a strong predictor of outcomes such as mortality [7–11] and long-term care (LTC) placement [12–15] and may act as a confounder if ADL impairment is imbalanced between comparison groups [16]. This potential confounding may be particularly problematic in observational studies of older adults with complex chronic diseases given that ADL impairment may be a stronger predictor of some outcomes such as LTC placement or mortality than some commonly used measures of medical comorbidity [17–19].
Comorbidity indices, such as the Charlson comorbidity score [20, 21], the Johns Hopkins Adjusted Clinical Groups (ACG) system [22], or measures based on prescription medications [23], can be constructed from information in many administrative databases to risk adjust outcomes and control for confounding. However, these databases and comorbidity measures do not contain direct information on ADL impairment and as such residual confounding due to ADL impairment may be present in these studies. To date, there have been only a few studies which have evaluated the impact of ADL impairment on predicting outcomes in administrative databases [19, 24, 25] and there is limited information available on strategies to minimize the potential bias that may result when direct measures of ADL impairment are not available.
One potential method to control for confounding due to ADL impairment is to control for variables that are available in most administrative databases such as demographics, medical conditions [1, 26–28], and measures of medical comorbidity which are correlated with ADL impairment. These proxy measures of ADL impairment may be more widely available in administrative data and may be able to minimize the effect of omitting information on direct measures of ADL impairment when such measures are not available. The goal of our study was to identify correlates of ADL impairment among older adults with hip fractures and to assess the impact of direct measures of ADL impairment on predicting mortality in the 360 days following hip fracture surgery.
Methods
Systematic review of factors associated with functional impairment
Electronic search strategy
To identify medical conditions and other correlates of functional impairment we searched electronic databases using key words and medical subject headings (Additional file 1). The databases Medline and EMBASE were searched from inception until November, 2010 to identify relevant articles. The abstracts and titles of retrieved citations were then reviewed for relevance and potentially relevant articles were reviewed for inclusion criteria. One author (D.S.) reviewed the titles and abstracts of all potentially included articles to identify potential correlates of ADL impairment.
Study selection
Observational studies that identified demographic variables, measures of medical comorbidity, medical conditions, or patterns of health service utilization that were correlated with impairment in basic ADLs were eligible for inclusion. We included a condition as a potential correlate of ADL impairment provided there was at least one study identified through our review process which identified a statistically significant relationship between the potential correlate and any clinically derived measure of impairment in ADLs. We restricted our selection of studies to those that that identified variables that are routinely collected in administrative data sources which typically include diagnoses associated with medical conditions (e.g. dementia) or clinical presentations (e.g. falls). For example, we excluded correlates of functional impairment that involved measurement of variables such as laboratory values and physiological measurements such as blood pressure which are not routinely available in administrative data. Activities of daily living are classified into basic activities of daily living (e.g. ability to walk, bath oneself, toilet, and eat) and instrumental activities of daily living (e.g. shopping, managing finances or medications, and completing housework) [29]. Impairment in activities of either basic or instrumental ADLs is commonly assessed by determining the amount of assistance that an individual requires to perform a given ADL. Commonly utilized measures of basic or instrumental ADL measures often provide summary scores of the degree of assistance required in component ADLs [30]. The final list of variables correlated with ADL impairment were summarized in a table along with the range of statistical association reported between that variable and ADL impairment (e.g. odds ratios or relative risks).
Definitions of medical conditions associated with functional impairment in administrative data
Methods for measuring each of the variables correlated with ADL impairment were identified using linked administrative healthcare databases situated at the Institute for Clinical Evaluative Sciences (ICES). These data sets were held securely in a linked, deidentified form and analysed at ICES. These datasets included the Registered Persons Database (RPDB) for demographic variables and date of death, the Canadian Institute for Health Information (CIHI) National Ambulatory Care Reporting System (NACRS) and Discharge Abstract Database (DAD) for emergency department visits and hospital admissions, respectively; the Ontario Health Insurance Plan (OHIP) claims database for outpatient and inpatient claims and assessments; and the Ontario Drug Benefits (ODB) database to identify claims for outpatient prescription medications; and the Ontario Mental Health Reporting System (OMHRS) for mental health inpatient admissions. These databases are routinely used for research purposes and the accuracy of these databases have been detailed in previous reports [31, 32].
Our study population included all adults aged 66 or older who underwent hip fracture surgery (admission diagnosis: ICD-9: 820, or ICD-10: S72) in Ontario between April 1, 2003 and March 31, 2009. The correlates of functional impairment were determined using hospital discharge diagnostic codes, diagnostic codes associated with outpatient physician visits, and prescribed medications (Additional file 2). Age was categorized as 66 – 75 years, 76–85 years, and 86 years or older. The number of outpatient physician visits in the year preceding hip fracture was categorized into 10 or fewer visits, 11 – 20 visits, or greater than 20 visits. Several measures of comorbidity were measured in the study sample. The Charlson Comorbidity Index is a commonly utilized comorbidity measure [33, 34] which has been adapted for use with administrative healthcare data [20, 35]. The Johns Hopkins Adjusted Clinical Groups classification to measure underlying medical severity [36]. In this system, individual medical conditions are assigned to categories referred to as Aggregated Diagnosis Groups (ADGs) [22]. Eight ADGs are considered major ADGs and the sum of major ADGs determined from hospital admissions, emergency room visits or outpatient physician contacts can be utilized as a measure of comorbidity to predict outcomes [37]. We also used the sum of the number of unique medications prescribed in the year preceding index as another measure of medical comorbidity [23]. This study was approved by the ethics review board at Sunnybrook Health Sciences Centre.
Correlates of functional impairment in study sample
We selected older adults with hip fractures as our study population because hip fractures are common among older adults [38] and functional impairment has been demonstrated to be a predictor of mortality in this population [39, 40]. Hip fractures are particularly common among frail older adults who receive home care or long-term care services [41]. To determine functional impairment in our study sample, we used information contained in the Resident Assessment Instrument (RAI) derived from assessments completed for individuals who had either received home care services or who were in long-term care (LTC) prior to their hip fracture. We only included those individuals in the final study sample who had either a RAI assessment associated with home care services [42] (RAI-HC) or a RAI assessment associated with long-term care Minimum Dataset (RAI-MDS) [43] within the 90 days preceding hospital admission for hip fracture. The RAI-MDS is completed at the time of admission and quarterly for residents in LTC, the RAI-HC is completed every 6 months for individuals receiving home care services. Within both RAI instruments are several measures of ADL function. Seven components of ADL function (dressing, personal hygiene, toilet use, locomotion, transfers, bed mobility, and eating) are used to create a composite measure of ADL function referred to as the ADL long-form [44]. Each ADL item is scored from 0 (independent) to 4 (total dependence) to derive the total ADL score (range 0 – 28, higher scores indicating greater ADL impairment). The ADL long-form total score was categorized as: 5 or less; 6 – 10; 11 – 15; 16 – 20; or greater than 20. The RAI-HC [42] and RAI-MDS [45] are both accurate and reliable instruments for the measurement of demographic and clinical information in populations of older adults and are routinely used for research purposes in Ontario [46, 47].
To determine whether medical conditions or other measures in administrative data were correlated with functional impairment, we performed a series of linear regression analyses with ADL long-form total scores as the dependent variable and each potential correlate as the independent variable. Variables associated with ADL impairment with a p-value of <0.05 were then retained for future models and the proportion of the variance of ADL impairment explained by the variable was assessed by the value of the R2 statistic. Finally, all variables that were significant in the bivariate analyses were combined in a multivariable model predicting ADL impairment, with the proportion explained variance for the model assessed by the adjusted R2 statistic. SAS version 9.3 (SAS Institute, Cary, North Carolina) was utilized for all analyses.
Effect of ADL impairment on postoperative mortality
We selected 360-day mortality following hip fracture surgery as death is common in the year following hip fracture surgery with approximately 30% of older adults experiencing this outcome [48]. Follow-up data for mortality were available until March 31, 2010, therefore all individuals in the study cohort contributed a minimum of 360 days of follow-up data in which to determine mortality. Information on mortality in our databases are highly accurate with error rates of 1 – 2% [49]. The probability of mortality in the 360 days following surgery was compared across the categories of ADL impairment using a χ2 statistic. Then, a multivariable logistic regression model was constructed to predict the probability of 360-day postoperative mortality. We first added age, sex, and residence in LTC in sequence to the model. Next, the measures of medical comorbidity and health service utilization that were significantly correlated with ADL impairment in the study sample were added to the model. Finally, all the medical conditions that were correlated with ADL impairment were included in the model. Direct measures of ADL impairment were then added to model using dummy variables for the previously defined categories of ADL impairment. The predictive ability of the model was assessed by the c-statistic and the maximum rescaled R2 values obtained for the models with and without ADL impairment. To assess whether ADL impairment improved the model fit, the change in the -2 log likelihood values for the models with and without ADL impairment were compared using a χ2 test for with a degrees of freedom equal to the number of additional variables in the models with ADL impairment compared to the models without ADL impairment. The AIC value for the models with and without ADL impairment were also compared as another method to assess improvement in model fit with a reduction in AIC indicating improved model fit. In all of our models, we ensured that the number of events (i.e. number of individuals who died within 360 days) were sufficient for the number of covariates in order to avoid over-fitting the model using a minimum of 10 events for each covariate included [50]. There were a total of 487 individuals who died within the 360 days following hip fracture surgery, therefore, our multivariable models could include up to 48 independent variables.
Results
Identification of correlates of ADL impairment
A total of 195 potentially relevant articles were identified from the electronic database search, 25 articles were identified through reference lists and 4 review articles were identified [1, 26, 28, 51]. A total of 37 articles reported on medical conditions or patient characteristics associated with basic ADL impairment (Additional file 3).
A total of 23 conditions were reported to be associated with impairment in basic ADLs (Additional file 2). These variables included demographic factors, general measures of medical comorbidity, general medical conditions, psychiatric conditions and conditions generally seen in older adult populations such as sensory impairment, falls, and incontinence. Cerebrovascular disease, cognitive impairment, and depression were the conditions most commonly reported to be associated with ADL impairment.
Information from physician outpatient visits, emergency room visits, hospital admissions and prescription drugs were identified to correspond to the medical conditions correlated with functional impairment. A medical condition was considered to be present if there was any outpatient physician visit code, emergency room, or hospitalization associated with the condition in the 5 year preceding cohort entry unless otherwise specified (Additional file 2).
Description of hip fracture study sample
A total of 1,329 individuals were included in the final study sample of older adults with hip fractures who had either a RAI-HC assessment (N = 286) or a RAI-MDS assessment (N = 1,043) in the 90 days preceding hospitalization for hip fracture surgery (Table 1). The mean age of the sample was 85.2 years (standard deviation (SD) = 6.9) and the majority were female (72.8%). Most of the study sample resided in LTC prior to hip fracture. The study population was in frequent contact with physicians and had a high number of emergency room visits and hospital admissions in the year preceding hip fracture. There was a high prevalence of several common chronic medical problems such as dementia (79%), ischemic heart disease (40%), and osteoarthritis (43%). Overall, medical comorbidity was common in the group as reflected by the 92% of individuals having a Charlson Comorbidity Index score of 1 or more and 98% of individuals having 1 or more major ADGs. Polypharmacy was also common in this group, with the average study participant prescribed a mean of 12.3 (SD = 6.2) unique medications in the year preceding cohort entry. Impairment in ADLs prior to hip fracture was substantial in the study sample with the mean ADL score of 11.9 (SD = 7.7) and a median ADL score of 12 (interquartile range = 5–18).
Correlates of functional impairment in older adults with hip fractures
In univariate linear regression analyses, several individual medical conditions or measures of medical comorbidity were associated with ADL impairment (Table 2). Variables associated with ADL impairment (p < 0.05) included residence in LTC, Charlson score (categorical), number of major ADGs (categorical), number of physician outpatient visits (continuous), congestive heart failure, COPD, dementia, hearing impairment, ischemic heart disease, number of emergency room visits for falls, osteoarthritis, Parkinson’s disease, stroke and pressure ulcers. The two variables that individually accounted for the greatest proportion of ADL impairment as assessed by the R2 statistic were residence in LTC (R2 = 0.11) and dementia (R2 = 0.05), while the other variables were associated with smaller R2 values.
A multivariable linear regression model was then constructed using the variables that were associated with ADL impairment in the preceding analysis. Age and sex were first entered into the model and accounted for a small proportion of ADL impairment (adjusted R2 = 0.005). Addition of LTC residence increased R2 value to 0.12. Further addition of Charlson score, number of major ADGs, and outpatient visits had a minimal effect on the adjusted R2 = 0.13. Addition of medical conditions associated with ADL impairment also only had a small effect on the overall adjusted R2 value, which was 0.16 for the final model (Table 3).
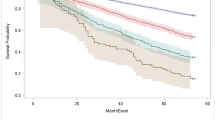
Effects of ADL impairment, medical comorbidity, and medical conditions on postoperative mortality
Overall, 487 individuals (36.6%) died within the 360 days of hip fracture. The severity of ADL impairment was positively correlated with mortality. Individuals with an ADL score of between 0 – 5 had a mortality risk of 25.8% when compared to a risk of mortality of 43.6% for individuals with an ADL score of > 20 with intermediate categories of ADL impairment associated with a gradation in the risk of mortality (Table 4).
Impairment in ADLs was strongly associated with mortality in a logistic regression model (OR = 2.22; 95% CI: 1.54 – 3.23; χ2 = 26.46, P <0.0001 for highest vs. lowest level of ADL impairment). However, this logistic regression model with only ADL impairment had a weak discriminative ability (c-statistic of 0.578) and only explained a low proportion of the variation in mortality (maximum rescaled R2 = 0.028) (Table 5). A multivariable logistic regression model including age (categorical), sex, LTC residence, Charlson score (categorical), number of major ADGs (categorical), total number of outpatient visits (continuous), and medical conditions identified as being correlated with ADL impairment (including congestive heart failure, COPD, dementia, hearing impairment, ischemic heart disease, number of emergency room visits for falls, osteoarthritis, Parkinson’s disease, stroke and pressure ulcers) was then created. The performance of this model to predict 360 day mortality was modest with a c-statistic of 0.653 and an R2 value of 0.09. The addition of ADL impairment to this model resulted in statistically significant improvement in the predictive ability fit of the model according to the difference in the – 2 log likelihoods for the models with and without ADL impairment. The p-value associated with the change in – 2 log likelihoods was p = 0.002 for ADL impairment as a categorical variable and p = 0.0002 for ADL impairment as a continuous variable. This improvement in model fit was also evident with a reduction in the AIC value from 1706.94 to 1695.95 with the inclusion of ADL impairment in the model as well as improvements in the c-statistic (0.668 vs. 0.653) and maximum rescaled R2 (0.11 vs. 0.09).
We also completed a sensitivity analysis to identify correlates of ADL impairment using backward selection in two models using P-values 0.1 and 0.05 to identify correlates. After identifying variables correlated with ADL using these models, the addition of direct measures of ADL impairment to the final model predicting mortality resulted in improved predictive ability of the model as determined changes in the AIC, -2 log likelihood ratio and c-statistic similar to the primary analysis.
Discussion
In the current study, a number of medical conditions that are routinely recorded in administrative data and other variables were identified as being correlated with functional impairment in older adults who underwent hip fracture surgery. Impairment in basic ADLs was significantly associated with an increased risk of mortality in the year following hip fracture with a 2-fold increase in the risk of death for individuals with greatest ADL impairment as compared to those with the least amount of impairment. Importantly, even after controlling for medical comorbidity and medical conditions correlated with ADL impairment, direct measures of ADL impairment added significantly to the prediction of postoperative mortality. This suggests that measures to control for the effects of ADL impairment through use of conditions associated with functional impairment and medical comorbidity may not be sufficient when direct measures of ADL impairment are not available potentially resulting in confounding or bias in observational studies.
These findings are consistent with previous research demonstrating that ADL impairment is a significant predictor of mortality and other poor health outcomes for populations of older adults with hip fractures [39, 40]. Several of the correlates of ADL impairment, such as residence in LTC, number of outpatient visits, measures of comorbidity such as the Charlson score, number of major ADGs and some medical conditions were correlated with ADL impairment in bivariate comparisons. However, in multivariable regression only residence in LTC, and certain medical conditions were correlated with ADL impairment. The association between residence in LTC and ADL impairment is predictable given that some degree of ADL impairment is required to be eligible for LTC admission in Ontario [52]. The association between dementia and ADL impairment is also anticipated given that the progressive nature of dementia results in ADL impairment especially as the disease reaches the moderate to severe stages [53]. Many of the medical conditions which were positively correlated with ADL impairment were associated with musculoskeletal dysfunction such as Parkinson’s disease and falls. These conditions, all of which have known relationships to impairment in mobility which would be expected to be reflected within our measure of ADL function. Pressure ulcers were also correlated with ADL impairment which is in keeping with immobility being the major risk factor for the development of pressure ulcers [54, 55]. Counter-intuitively, the presence of some conditions such as osteoarthritis, COPD and ischemic heart disease were significantly associated with decreased likelihood of ADL impairment. One potential reason for this observation likely related to how diagnoses are recorded in administrative data. Some chronic health conditions may appear to be protective against health outcomes when they actually may be markers of individuals being in relatively good health when compared to other individuals in the same population who have other unstable health conditions which become the focus of clinical encounters by physicians and are billed as such [56].
When the outcome of mortality in the 360 days following hip fracture surgery was examined, ADL function was significantly associated with mortality in a dose response relationship. Impairment in ADLs has been demonstrated to be a predictor of postoperative mortality in older adults with hip fractures, along with several other risk factors [39, 40]. While ADL impairment was a statistically significant predictor of postoperative mortality, the overall predictive value of ADL impairment was modest when considered in isolation. Addition of measures of ADL functioning to commonly used methods of risk adjustment in studies of older adults resulted in significant improvements in the predictive ability of this model although much of the variation in postoperative mortality was still unexplained by the model suggesting that some other prognostic variables were not captured in the model.
Prior studies have also demonstrated that studies utilizing administrative datasets with direct measures of functional status can significantly add to statistical models predicting outcomes such as death, institutionalization, or hospitalization [19]. A study of 6,465 participants enrolled in a cluster randomized controlled clinical trial examined the effects of usual methods of case-mix adjustment including measures of demographic variables, comorbidity scores, and measures of health service utilization to predict death, institutionalization or hospitalization. Addition of ADL measures to these models improved the predictive ability of the models although the effects of ADL measures on the overall predictive ability of the models were modest as measured by changes in the rescaled R2 and c-statistics. The importance of ADL impairment in predicting outcomes after adjusting for medical comorbidity has also been observed in observational studies of older adults undergoing cardiac surgery [24] and community-dwelling older adults [17]. Likewise, a modest improvement in the ability of our model to predict mortality following hip fracture surgery was also observed with the inclusion of ADL measures although the clinical significance of this is questionable.
There are some limitations to the current study. The first relates to the study population, the majority of which were in LTC prior to cohort entry along with community-dwelling older adults who received home care services. Given the high rates of functional impairment in these populations, the results observed in our study may not generalize well to other study populations with less severe levels of impairment such as community-dwelling older adults who are not receiving home care services. Some clinical variables associated with ADL impairment such as abnormal laboratory values or measures of strength were not available in our datasets and as such these could not be included in our statistical models. Finally, some conditions such as malnutrition are likely underreported in our administrative databases when compared to detailed chart review or clinical examination [57] and our methods for identifying these conditions in administrative data may also be subject to measurement error. The underreporting of some of the conditions that were identified as potential correlates of ADL impairment may have resulted in an overestimation of the relative contribution of direct measures of ADL impairment to predicting postoperative outcomes.
Conclusions
In summary, impairment in basic activities of daily living can be an important predictor of outcomes in observational studies using administrative databases. There is the potential for residual confounding due to ADL impairment when direct measures of ADL functioning are not available, even after controlling for demographics, medical comorbidity, and medical conditions correlated with ADL impairment. Additional studies of populations other than older adults with hip fractures will be useful to further understand the impact of ADL impairment on outcomes in observational studies using administrative healthcare datasets.
Author contribution
All authors made substantial contributions to the conception and design of the study. DS contributed to the analysis of data. DS drafted the manuscript and all authors revised it critically for content. The final manuscript was approved by all authors.
References
Naglie G, Gill SS: Review of risk factors associated with dependency in basic and instrumental activities of daily living. Can J Geriatr. 2009, 12: 160-176.
Schoeni RF, Freedman VA, Wallace RB: Persistent, consistent, widespread, and robust? Another look at recent trends in old-age disability. J Gerontol B Psychol Sci Soc Sci. 2001, 56 (4): S206-S218. 10.1093/geronb/56.4.S206.
Crimmins EM, Saito Y, Reynolds SL: Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: the LSOA and the NHIS. J Gerontol B Psychol Sci Soc Sci. 1997, 52 (2): S59-S71.
Wilkins K, Park E: Home care in Canada. Health Rep. 1998, 10: 29-37.
Manton KG, Corder L, Stallard E: Chronic disability trends in elderly United States populations: 1982–1994. Proc Natl Acad Sci USA. 1997, 94 (6): 2593-2598. 10.1073/pnas.94.6.2593.
Manton KG, Gu X: Changes in the prevalence of chronic disability in the United States black and non-black population above age 65 from 1982 to 1999. Proc Natl Acad Sci USA. 2001, 98: 6354-6359. 10.1073/pnas.111152298.
Narain P, Rubenstein LZ, Wieland GD, Rosbrook B, Strome LS, Pietruszka F, Morley JE: Predictors of immediate and 6-month outcomes in hospitalized elderly patients. The importance of functional status. J Am Geriatr Soc. 1988, 36 (9): 775-783.
Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J: Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998, 279 (15): 1187-1193. 10.1001/jama.279.15.1187.
Ponzetto M, Maero B, Maina P, Rosato R, Ciccone G, Merletti F, Rubenstein LZ, Fabris F, Ponzetto M, Maero B, et al: Risk factors for early and late mortality in hospitalized older patients: the continuing importance of functional status. J Gerontol A Biol Sci Med Sci. 2003, 58 (11): 1049-1054. 10.1093/gerona/58.11.M1049.
Reuben DB, Rubenstein LV, Hirsch SH, Hays RD: Value of functional status as a predictor of mortality: results of a prospective study. Am J Med. 1992, 93 (6): 663-669. 10.1016/0002-9343(92)90200-U.
Naeim A, Keeler EB, Reuben D: Perceived causes of disability added prognostic value beyond medical conditions and functional status. J Clin Epidemiol. 2007, 60 (1): 79-85. 10.1016/j.jclinepi.2005.11.026.
Coughlin TA, McBride TD, Liu K: Determinants of transitory and permanent nursing home admissions. Med Care. 1990, 29 (7): 616-631.
Greene VL, Ondrich JI: Risk factors for nursing home admissions and exits: a discrete-time hazard function approach. J Gerontology. 1990, 45 (6): S250-S258. 10.1093/geronj/45.6.S250.
Banaszak-Holl J, Fendrick A, Foster NL, Herzog A, Kabeto MU, Kent DM, Straus WL, Langa KM: Predicting nursing home admission: estimates from a 7-year follow-up of a nationally representative sample of older Americans. Alzheimer Dis Assoc Disord. 2004, 18 (2): 83-89. 10.1097/01.wad.0000126619.80941.91.
Ebly EM, Hogan DB, Rockwood K: Living alone with dementia. Dement Geriatr Cogn Dis. 1999, 10 (6): 541-548. 10.1159/000017202.
Jackson LA, Nelson JC, Benson P, Neuzil KM, Reid RJ, Psaty BM, Heckbert SR, Larson EB, Weiss NS: Functional status is a confounder of the association of influenza vaccine and risk of all cause mortality in seniors. Int J Epidemiol. 2006, 35 (2): 345-352.
Pressley JC, Patrick CH: Frailty bias in comorbidity risk adjustments of community-dwelling elderly populations. J Clin Epidemiol. 1999, 52 (8): 753-760. 10.1016/S0895-4356(99)00056-6.
Landi F, Bernabei R, Russo A, Zuccala G, Onder G, Carosella L, Cesari M, Cocchi A: Predictors of rehabilitation outcomes in frail patients treated in a geriatric hospital. J Am Geriatr Soc. 2002, 50 (4): 679-684. 10.1046/j.1532-5415.2002.50162.x.
Mayo NE, Nadeau L, Levesque L, Miller S, Poissant L, Tamblyn R, Mayo NE, Nadeau L, Levesque L, Miller S, et al: Does the addition of functional status indicators to case-mix adjustment indices improve prediction of hospitalization, institutionalization, and death in the elderly?. Med care. 2005, 43 (12): 1194-1202. 10.1097/01.mlr.0000185749.04875.cb.
Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992, 45 (6): 613-619. 10.1016/0895-4356(92)90133-8.
Southern DA, Quan H, Ghali WA: Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004, 42 (4): 355-360. 10.1097/01.mlr.0000118861.56848.ee.
Reid RJ, Roos NP, MacWilliams L, Frohlich N, Black C: Assessing population health care need using a claims-based ACG morbidity measure: a validation in the province of manitoba. Health Serv Res. 2002, 37: 1345-1364. 10.1111/1475-6773.01029.
Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ: Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol. 2001, 154 (9): 854-864. 10.1093/aje/154.9.854.
Afilalo J, Mottillo S, Eisenberg MJ, Alexander KP, Noiseux N, Perrault LP, Morin J-F, Langlois Y, Ohayon SM, Monette J, et al: Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Cardiovasc Qual Outcom. 2012, 5 (2): 222-228. 10.1161/CIRCOUTCOMES.111.963157.
Tan WS, Ding YY, Chong WF, Tay JC, Tan JT-L: Impact of data source and time reference of functional status on hospital mortality prediction. BMC Health Serv Res. 2012, 12: 115-10.1186/1472-6963-12-115.
Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC: Risk factors for functional decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999, 48: 445-469. 10.1016/S0277-9536(98)00370-0.
Boult C, Kane RL, Louis TA, Boult L, McCaffrey D: Chronic conditions that lead to functional limitation in the elderly. J Gerontol. 1994, 49: M28-M36. 10.1093/geronj/49.1.M28.
McCusker J, Kakuma R, Abrahamowicz M: Predictors of functional decline in hospitalized elderly patients: a systematic review. J Gerontol. 2002, 57A: M569-M577.
Katz S: Assesing self-maintenance: activities of daily living, mobility and instrumental activities of daily living. J Am Geriatr Soc. 1983, 31: 721-727.
Law M, Letts L: A critical review of scales of activities of daily living. Am J Occup Ther. 1989, 43: 522-528. 10.5014/ajot.43.8.522.
Williams JI, O’Brien BJ, Sellors C, Grootendorst P, Willison D: A summary of studies on the quality of health care administrative databases in Canada. Patterns of health care in Ontario The ICES practice atlas. Edited by: Goel V, Williams JI, Anderson GM, Blacksterin-Hirsch P, Fooks C, Naylor CD. 1996, Ottawa,ON: Canadian Medical Association, 339-345.
Levy AR, O’Brien BJ, Sellors C, Grootendorst P, Willison D: Coding accuracy of administrative drug claims in the Ontario drug benefit database. Can J Clin Pharmacol. 2003, 10 (2): 67-71.
Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987, 40: 373-383. 10.1016/0021-9681(87)90171-8.
Charlson M, Szatrowski TP, Peterson J, Gold J: Validation of a combined comorbidity index. J Clin Epidemiol. 1994, 47: 1245-1251. 10.1016/0895-4356(94)90129-5.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA: Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005, 43 (11): 1130-1139. 10.1097/01.mlr.0000182534.19832.83.
Starfield B, Weiner J, Murla P: Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res. 1991, 26: 53-74.
Baldwin L-M, Klabunde CN, Green P, Barlow W, Wright G: In search of the perfect comorbidity measure for Use with administrative claims data. Med Care. 2006, 44: 744-753.
Seitz DP, Adunuri N, Gill SS, Rochon PA: Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc. 2011, 12 (8): 556-564. 10.1016/j.jamda.2010.12.001.
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL: Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA. 2001, 285 (21): 2736-2742. 10.1001/jama.285.21.2736.
Bellelli G, Mazzola P, Corsi M, Zambon A, Corrao G, Castoldi G, Zatti G, Annoni G: The combined effect of ADL impairment and delay in time from fracture to surgery on 12-month mortality: an observational study in orthogeriatric patients. J Am Med Dir Assoc. 2012, 13 (7): 664-e9-664 doi:10.1016/jamda.2012.06.007
Rapp K, Becker C, Cameron ID, Klenk J, Kleiner A, Bleibler F, König H-H, Büchele G: Femoral fracture rates in people with and without disability. Age Ageing. 2012, 41 (5): 653-658. 10.1093/ageing/afs044.
Landi F, Tua E, Onder G, Carrara B, Sgadari A, Rinaldi C, Gambassi G, Lattanzio F, Bernabei R: Minimum data Set for home care: a valid instrument to assess frail older people living in the community. Med Care. 2000, 38 (12): 1184-1190. 10.1097/00005650-200012000-00005.
Canadian Institute of Health Information: Minimum dataset (2.0) Canadian version 2002: Canadian Institutes of Health Information. 2010, Ontario, Canada: Ottawa
Morris JN, Fries BE, Morris SA: Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999, 54 (11): M546-M553. 10.1093/gerona/54.11.M546.
Hirdes JP, Ljunggren G, Morris JN, Frijters DH, Soveri HF, Gray L, Björkgren M, Gilgen R: Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. 2008, 8 (1): 277-10.1186/1472-6963-8-277.
Gruneir A, Forrester J, Camacho X, Gill S, Bronskill S: Gender differences in home care clients and admission to long-term care in Ontario, Canada: a population-based retrospective cohort study. BMC Geriatr. 2012, 13: 48-
Daneman N, Gruneir A, Newman A, Fischer HD, Bronskill SE, Rochon PA, Anderson GM, Bell CM: Antibiotic use in long-term care facilities. J Antimicrob Chemothe. 2011, 66 (12): 2856-2863. 10.1093/jac/dkr395.
Jiang H, Majumdar S, Dick D, Moreau M, Raso J, Otto D, Johnston D: Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005, 20 (3): 494-
Iron K: Living and dying in Ontario: an opportunity for improved health information: institute for clinical evaluative sciences. 2008
Peduzzi P, Concato J, Kemper E, Holford T, Feinstein A: A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996, 49 (12): 1373-10.1016/S0895-4356(96)00236-3.
Miller EA, Weissert WG: Predicting elderly People’s risk for nursing home placement, hospitalization, functional impairment, and mortality: a synthesis. Med Care Res Rev. 2000, 57: 259-297. 10.1177/107755870005700301.
Understanding your options. http://healthcareathome.ca/#Long-Term Care Homes.
Njegovan V, Hing MM, Mitchell SL, Molnar FJ: The hierarchy of functional loss associated with cognitive decline in older persons. J Gerontol A Biol Sci Med Sci. 2001, 56 (10): M638-M643. 10.1093/gerona/56.10.M638.
Reddy M, Gill SS, Rochon PA: Preventing pressure ulcers: a systematic review. JAMA. 2006, 296 (8): 974-984. 10.1001/jama.296.8.974.
Brandeis GH, Ooi WL, Hossain M, Morris JN, Lipsitz LA: A longitudinal study of risk factors associated with the formation of pressure ulcers in nursing homes. J Am Geriatr Soc. 1994, 42 (4): 388-393.
Elixhauser A, Steiner C, Harris DR, Coffey RM: Comorbidity measures for use with administrative data. Med Care. 1998, 36 (1): 8-27. 10.1097/00005650-199801000-00004.
Humphries KH, Rankin JM, Carere RG, Buller CE, Kiely FM, Spinelli JJ: Co-morbidity data in outcomes research: are clinical data derived from administrative databases a reliable alternative to chart review?. J Clin Epidemiol. 2000, 53 (4): 343-349. 10.1016/S0895-4356(99)00188-2.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2318/14/9/prepub
Funding
Dr. Seitz is supported by a Clinician Scientist Development Program salary award from Queen’s University. Dr. Austin was funded in part by a Career Investigator award from the Heart and Stroke Foundation. Dr. Bell is supported by a Canadian Institutes of Health Research and Canadian Patient Safety Institute Chair in Patient Safety and Continuity of Care. Dr. Gruneir is partially supported in part by a Team Grant (OTG-88591) from the Canadian Institutes of Health Research (CIHR) Institute of Nutrition, Metabolism and Diabetes. This work was supported by an Interdisciplinary Capacity Enhancement Grant (HOA-80075) from the CIHR Institute of Gender and Health and the CIHR Institute of Aging and a Team Grant (OTG-88591) from the Canadian Institutes of Health Research (CIHR) Institute of Nutrition, Metabolism and Diabetes.
This study was conducted at the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors of this manuscript have no conflicts of interest to declare.
Electronic supplementary material
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited.
About this article
Cite this article
Seitz, D.P., Anderson, G.M., Austin, P.C. et al. Effects of impairment in activities of daily living on predicting mortality following hip fracture surgery in studies using administrative healthcare databases. BMC Geriatr 14, 9 (2014). https://doi.org/10.1186/1471-2318-14-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2318-14-9