Abstract
Background
FibroTest (FT) is the most frequently used serum fibrosis marker and consists of an algorithm of five fibrosis markers (alfa2-macroglobulin, apolipoproteinA1, haptoglobin, GGT, bilirubin). The Enhanced Liver Fibrosis (ELF) test consists of an algorithm of three fibrosis markers (hyaluronic acid, amino-terminal propeptide-of-type-III-collagen, tissue-inhibitor of matrix-metaloproteinase-1). While a systematic review has shown comparable results for both individual markers, there has been no direct comparison of both markers.
Methods
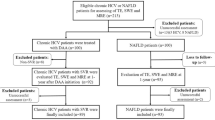
In the present study, the ELF-test was analyzed retrospectively in patients with chronic liver disease, who received a liver biopsy, transient elastography (TE) and the FibroTest using histology as the reference method. Histology was classified according to METAVIR and the Ludwig's classification (F0-F4) for patients with chronic hepatitis C and B virus (HCV, HBV) infection and primary biliary cirrhosis (PBC), respectively.
Results
Seventy-four patients were analysed: 36 with HCV, 10 with HBV, and 28 with PBC. The accuracy (AUROC) for the diagnosis of significant fibrosis (F≥2) for ELF and FibroTest was 0.78 (95%CI:0.67-0.89) and 0.69 (95%-CI:0.57-0.82), respectively (difference not statistically significant, n.s.). The AUROC for the diagnosis of liver cirrhosis was 0.92 (95%CI:0.83-1,00), and 0.91 (95%CI:0.83-0.99), respectively (n.s.). For 66 patients with reliable TE measurements the AUROC for the diagnosis of significant fibrosis (cirrhosis) for TE, ELF and FT were 0.80 (0.94), 0.76 (0.92), and 0.67 (0.91), respectively (n.s.).
Conclusion
FibroTest and ELF can be performed with comparable diagnostic accuracy for the non-invasive staging of liver fibrosis. Serum tests are informative in a higher proportion of patients than transient elastography.
Similar content being viewed by others
Background
For different causes of chronic liver disease assessment of liver fibrosis is important to estimate the prognosis and to determine surveillance strategies for liver cancer. In addition, for chronic viral hepatitis the degree of liver fibrosis is one important parameter for decision on antiviral therapy [1]. At present, liver biopsy is still most commonly used as reference standard for the assessment of liver fibrosis. However, it is an invasive method associated with patient discomfort and in rare cases with serious complications [2]. In addition, the accuracy of liver biopsy is limited due to sampling error and significant intra- and inter-observer variability in histological staging [3, 4]. Therefore, research has focused on the evaluation of non-invasive methods for the assessment of liver fibrosis. Transient elastography (FibroScan, Echosens, France, [TE]) [5, 6] and the serological fibrosis marker FibroTest (Biopredictive, France, [FT]) [7, 8] have been evaluated most frequently. FibroTest consists of an algorithm of five fibrosis markers (alfa2-macroglobulin, apolipoproteinA1, haptoglobin, GGT, bilirubin). The Enhanced Liver Fibrosis Test (ELF, Siemens Diagnostics) [9, 10] consists of an algorithm of three fibrosis markers (hyaluronic acid, amino-terminal propeptide of type III collagen, tissue inhibitor of matrix metaloproteinase 1). The aim of the present study was to analyze the ELF test using frozen serum samples from patients with chronic liver disease that received a liver biopsy, transient elastography (TE) and the FibroTest and to compare the results of the non-invasive tests using histology as reference method.
Methods
The study period for sample acquisition was from September 2005 to June 2008. The Serum bank of the J.W. Goethe-University Hospital was checked for serum of patients with chronic liver disease, who received a liver biopsy, transient elastography and FibroTest. The patients were included in the present study, if frozen serum was available dated around the time of the performance of FibroTest. The time interval between sample acquisition for the FibroTest and ELF was up to one week without any therapeutic interventions between the performances of the two tests. As the mean progression rate of liver fibrosis in untreated patients was estimated 0.085-0.120 fibrosis stages on the Metavir scoring system per year [11] a time interval between liver biopsy and the performance of the non-invasive methods of up to 12 months was accepted for enrollment in the present study. The time interval between liver biopsy and study inclusion ranged from 0 to 10 months (mean 10 ± 10 weeks, median 3 weeks). The indication for liver biopsy was the determination of histological fibrosis and inflammation. Written informed consents were obtained from all patients and the study was conducted in agreement with the Declaration of Helsinki and Good Clinical Practice guidelines (ethics committee of Johann Wolfgang Goethe-University).
Liver Histology
Liver biopsy specimens were fixed in 4%-buffered formalin and embedded in paraffin. Two-micrometer-thick sections were stained with hematoxylin-eosin, Perls-iron-stain, dPAS (periodic-acid-Schiff after digestion with diastase), Masson-Trichrome. All biopsy specimens were analyzed by an experienced pathologist blinded to the clinical results of the patients. Liver fibrosis stages were evaluated semi-quantitatively according to the Metavir scoring-system [12] for patients infected with chronic hepatitis B or C. Liver fibrosis was staged on a F0-F4 scale: F0-no fibrosis, F1-portal fibrosis without septa, F2- portal fibrosis with few septa, F3- numerous septa without cirrhosis, F4-cirrhosis. In patients with PBC histological-stage was determined according to the Ludwig's classification[13]: stage I = inflammation and/or abnormal connective tissue is confined to portal triads; stage II = the number of normal bile ducts is reduced, the inflammation and/or fibrosis is confined to portal and periportal areas; stage III = fibrous septa link adjacent portal triads (bridging fibrosis); stage IV = cirrhosis with regenerative nodules. No stage 0 = no inflammation/fibrosis exists in the Ludwig's classification, since stage I is part of the diagnosis of PBC. The biopsies were judged as adequate, if the number of portal tracts was at least 6 and the length of liver biopsy at least 1 cm. The mean length of the included liver biopsies was 22.3 ± 9.3 mm (median 20 mm, range 10-54 mm).
Blood Markers
The following blood parameters were determined after overnight fasting in the same laboratory on the same day as transient elastography in all patients: aspartate aminotransaminase (AST), alanine aminotransaminase (ALT), γ-glutamyl transpeptidase, alkaline phosphatase, total bilirubin, platelet count, α2-macroglobulin, apolipoprotein A1, and haptoglobin. Enzymatic activity was measured at 37°C according to International Federation of Clinical Chemistry standards.
The laboratory followed the pre-analytical and analytical recommendations required to obtain the fibrosis marker score FibroTest® (Biopredictive, France) [14]. The FibroTest was computed on the Biopredictive website http://www.biopredictive.com. The security algorithms on the industrial website permitting to exclude patients with high risk profile of false positive/negative were respected [15].
Frozen serum of the above patients taken around the same time (stored at -80°C) was send to an independent reference laboratory (iQur Limited, Southampton, UK). Serum samples were analyzed for levels of tissue inhibitor of matrix metalloproteinase 1 (TIMP-1), hyaluronic acid (HA), and amino-terminal propeptide of type III collagen (P3NP) using the proprietary assays developed for ELF test by Siemens Healthcare Diagnostics Inc. (Tarrytown, New York USA). Assays were performed on an Immuno-1 auto-analyser (Siemens Healthcare Diagnostics Inc, Tarrytown, New York, USA). Results were entered into the established algorithm [10] and expressed as discriminant scores (DS) = -7.412 + (ln(HA)*0.681) + (ln(P3NP)*0.775) + (ln(TIMP1)*0.494) +10 for comparison to Metavir and Ludwig's histological staging.
Transient Elastography
Transient Elastography (TE) was performed using FibroScan® (Echosens, France). This machine is equipped with a probe including an ultrasonic transducer mounted on the axis of a vibrator. A vibration transmitted from the vibrator towards the tissue induces an elastic shear wave that propagates through the tissue. These propagations are followed by pulse-echo ultrasound acquisitions and their velocity is measured which is directly related to tissue stiffness. Results are expressed in kilopascal. Details have been described in previous studies [16]. The examination was performed on the right lobe of the liver through the intercostal space. After the area of measurement was located, the examiner pressed the button of the probe to start the acquisition. The measurement depth was between 25 and 65 mm. As suggested by the manufacturer ten successful acquisitions were performed on each patient. Only TE-results obtained with 10 valid measurements, with a success-rate of at least 60% and an interquartile range ≤30% were considered reliable. FibroScan failure is defined when less than 10 valid measurements are obtained.
Statistical Analysis
Statistical analysis was performed using BiAS for Windows (version 9.04, epsilon 2009, Frankfurt, Germany). Correlations were assessed by Spearmans correlation coefficient. The diagnostic performance of ELF, FibroTest and TE was assessed using receiver-operating-characteristic (ROC)-curves. The ROC-curve represents a plot of sensitivity versus 1-specificity for all possible cut-off values for prediction of the different fibrosis stages, respectively. The areas-under-the-ROC-curves (AUROC) as well as 95%-CI of AUROC were calculated. AUROC values for different diagnostic criteria for the same data set were compared with the non-parametric DeLong-test. Note that AUROC values for the different methods are correlated and that this test accounts for such correlations. Therefore, it may find significant differences in diagnostic accuracy even when confidence intervals of the single AUROC values, which ignore these correlations, are overlapping. Since two different fibrosis staging systems (Metavir and Ludwig's) were used to classify histology, and both systems use scores ranging from 0 to 4, the scoring systems were pooled for the overall calculation of the mean-AUROC. In case of diagnosing fibrosis stages greater than or equal 2 versus stages less than 2, we also calculated the differences between mean advanced, versus mean non-advanced fibrosis stages (DANA)-adjusted AUROC according to Poynard et al. [17] for a standardized DANA value of 2.5. Note that this adjustment was only validated for HCV patients and for FibroTest only. Assuming that, using other methods (TE and ELF) and in other pathologies, the spectrum bias has the same profile as for FT in HCV, we extrapolated the algorithm to adjust all the AUROCs in the present study.
Using cut-off values defined for the prediction of fibrosis in previous studies, sensitivity, specificity, positive- and negative-predictive-values positive- and negative likelihood ratios were calculated for the present study.
Results
Seventy-four patients were included in the analysis: 36 patients with HCV infection, 10 with HBV infection, and 28 with PBC. Patients' characteristics are shown in table 1.
The Spearman correlation coefficient of FibroTest and ELF with the different histological stages were 0.44, and 0.61, respectively (all p < 0.0001). The correlation coefficient between FibroTest and ELF was 0.62 (p < 0.0001).
The diagnostic accuracy (AUROC) for the diagnosis of significant fibrosis (F≥2) for ELF and FibroTest was 0.78 (95%-CI: 0.67-0.89) and 0.69 (95%-CI: 0.57-0.82), respectively (s. figure 1). The difference was not statistically significant (p = 0.20). The AUROC for the diagnosis of severe fibrosis (F≥3) was 0.79 (95%-CI: 0.67-0.91) and 0.72 (95%-CI: 0.60-0.84), respectively (p = 0.22). The AUROC for the diagnosis of liver cirrhosis was 0.92 (95%-CI: 0.83-1.00) and 0.91 (95%-CI: 0.82-0.99), respectively (p = 0.91) (s. figure 2). Details are shown in table 2.
Eight patients were excluded because of unreliable TE-measurements (less than 10 valid measurements, success rate <60%, or IQR >30%). Therefore only 66 patients were available for the comparison of TE with FT and ELF. For these 66 patients the Spearman correlation coefficient between TE, FibroTest and ELF with the different histological stages were 0.58, 0.42, and 0.58, respectively (p < 0.001). The correlation coefficient between TE and FibroTest was 0.67 (p < 0.0001), between TE and ELF 0.65 (p < 0.0001), and between FibroTest and ELF 0.62 (p < 0.0001), respectively. For these 66 patients the AUROC for the diagnosis of significant fibrosis for TE, ELF and FT was 0.80, 0.76, and 0.67, respectively (p = 0.42 for TE vs ELF, p = 0.08 for TE vs FT, p = 0.23 for ELF vs FT). The AUROC for the diagnosis of severe fibrosis (F≥3) was 0.66, 0.69 and 0.63, respectively (p = 0.60 for TE vs ELF, p = 0.68 for TE vs FT, p = 0.35 for ELF vs FT). And the AUROC for the diagnosis of liver cirrhosis was 0.94, 0.92, and 0.91, respectively (p = 0.60 for TE vs ELF, p = 0.42 for TE vs FT, p = 0.66 for ELF vs FT). Details are shown in table 2.
The diagnostic performance of FibroTest, ELF and transient elastography in the prediction of significant fibrosis (F≥2), severe fibrosis (F≥3), and cirrhosis using cut-offs defined in previous studies are shown in table 3.
Discussion
At present, transient elastography and the serum marker FibroTest are the most intensively evaluated non-invasive methods for the assessment of liver fibrosis. The results of the present study for transient elastography, FibroTest and ELF are in accordance with the results of previous studies [5–8, 10, 18]. However, the latter is of more clinical importance for estimation of prognosis, surveillance and treatment decisions before patients develop liver cirrhosis [1]. Furthermore inter and intra-observer discrepancies in histological classification of lesser stages of fibrosis are more prevalent than for higher stages and this may account for the observed under performance of non-invasive tests when compared to histology as a reference standard.
A systematic review has shown comparable results for ELF and FibroTest but no direct comparison of both markers had been performed before [19]. This is the first study, comparing transient elastography, FibroTest and ELF in the same study population. The results of the three non-invasive methods using different approaches were comparable for the diagnosis of significant fibrosis and cirrhosis in the present study.
The ELF test was developed in an international multicenter cohort study with 1021 subjects with chronic liver disease using discriminant analysis to identify the above mentioned algorithm having investigated specific markers of matrix turnover as well as indirect markers of liver function [10]. The ELF test was validated in Non-Alcoholic Liver Disease in adults [20] and in children [21], in PBC and hepatitis C [9, 22]
One study [23] has compared the FibroTest with ELF in a subgroup of patients infected with chronic hepatitis C. In this study, instead of using the ELF assays for HA, PIIINP and TIMP-1 that have been developed by Siemens Healthcare Diagnostics specifically for use in the ELF test; and instead of performing the assays on the Immuno-1 auto-analyser on which the ELF test is currently validated and CE marked, the investigators used alternative assays and performed manual testing. Thus the method used by Cales et al. to measure the analytes prior to incorporating results into the ELF algorithm cannot be considered to be analogous with the present study.
In the study of Cales et al. Fibrometer, an algorithm of direct and indirect markers was evaluated and compared with other non-invasive markers in a validation group. The authors suggest that the combination of both markers might increase certain advantages and limit other disadvantages. However, no significant difference was found between the Fibrometer, FibroTest and ELF as performed by the authors in this study. Similar results were found comparing ELF and TE in 80 patients with hepatitis C with the same diagnostic accuracy for both methods (AUROC 0.91, 0.90 for cirrhosis and 0.82 for >stage 2 fibrosis) [24].
Recently, a series of algorithms based on sequential combination of non-invasive serum markers showed 93-95% accuracy in the detection or exclusion of significant liver fibrosis and a reduction of 50% of liver biopsies in this subset of patients with HCV infection [25]. However, the combination of FibroTest and ELF has not been evaluated yet. Further studies are needed to evaluate the advantages and disadvantages of both markers and in which situations they may substitute each other.
Using liver biopsy as a reference standard for the evaluation of non-invasive methods and markers has methodological limitations which may influence the performance of these tests. The accuracy of liver biopsy is limited due to intra- and inter-observer variability and sampling errors [3]. In a study on more than 10,000 virtual biopsies Bedossa et al. [3] showed that liver fibrosis stage is correctly diagnosed in only 65% of cases, if the biopsy is at least 15 mm long, in 75% if it is at least 25 mm long and, that the optimal size should be 40 mm. However, most biopsies even at specialist Hepatology centers do not fulfill these optimal criteria [26].
Data analyzing the discordance of liver biopsy and the panel marker FibroTest showed that this discordance was highly attributable to biopsy in 5% and to the panel marker in 2% (p = 0.03) [26]. The authors concluded that these shortcomings of liver biopsy lead to underestimation of the diagnostic accuracy of non-invasive markers. A recent study has demonstrated that error in the liver biopsy result itself makes it impossible to distinguish a perfect non-invasive marker from less valid assays [27]. This supports the assumption that non-invasive markers might be underestimated using liver biopsy as reference method. The ultimate validation of liver fibrosis as a marker of liver injury is its prognostic value in terms of morbidity and mortality. In a study in patients infected with chronic hepatitis C, FibroTest was shown to have a 5-year prognostic value similar to that of liver biopsy [15]. In addition, the FibroTest was shown to accurately define 4-year prognosis in patients infected with hepatitis B [28] and 10-year prognosis in patients with alcoholic liver disease [29]. A study in patients with PBC demonstrated a highly significant relationship between the baseline ELF score and the likelihood of developing a clinical complication over the next 6 years [22], which was also shown in a mixed etiology cohort of 500 patients [30].
For ultrasound based methods to measure liver fibrosis (transient elastography [FibroScan], and acoustic radiation force impulse imaging [ARFI]) long-term follow-up studies are not available yet [5, 31]. Large, well-conducted randomized trials with clearly defined endpoints, i.e. assessing 5-year survival without complications related to liver disease (liver related death, liver transplantation, hepatic decompensation, variceal bleeding, hepatocellular carcinoma) are needed to compare the non-invasive methods with each other and with liver biopsy.
A limitation of the present study is its retrospective analysis and the small study population, however, this is the first study comparing an algorithm of indirect fibrosis markers (FibroTest), an algorithm of direct fibrosis markers (ELF) using the approved and validated ELF assay and analyzer and an ultrasound-based elastography method in one and the same study population. Larger prospective studies are necessary to confirm these results. Another limitation of our analysis is the inclusion of biopsies which are shorter than the usual standard of 15 mm, if at least 6 portal tracts were present. Nevertheless, the exclusion of such short biopsies had no significant effect on our results. In addition, the present study was a comparative study between the different non-invasive methods, where the quality of liver biopsy affected all methods equally.
Conclusion
FibroTest and ELF can be performed with comparable diagnostic accuracy for the non-invasive staging of liver fibrosis.
Funding
none
References
National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C 2002 (June 10-12, 2002). Hepatology. 2002, 36: S3-S20.
Castera L, Negre I, Samii K, Buffet C: Pain experienced during percutaneous liver biopsy. Hepatology. 1999, 30: 1529-1530. 10.1002/hep.510300624.
Bedossa P, Dargere D, Paradise V: Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003, 38: 1449-1457.
Maharaj B, Maharaj RJ, Leary WP, Cooppan RM, Naran AD, Pirie D, et al: Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Lancet. 1986, 1: 523-525. 10.1016/S0140-6736(86)90883-4.
Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E: Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008, 134: 960-974. 10.1053/j.gastro.2008.01.034.
Talwalkar JA, Kurtz DM, Schoenleber SJ, West CP, Montori VM: Ultrasound-based transient elastography for the detection of hepatic fibrosis: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2007, 5: 1214-1220. 10.1016/j.cgh.2007.07.020.
Poynard T, Imbert-Bismut F, Munteanu M, Messous D, Myers RP, Thabut D, Ratziu V, Mercadier A, Benhamou Y, Hainque B: Overview of the diagnostic value of biochemical markers of liver fibrosis (FibroTest, HCV FibroSure) and necrosis (ActiTest) in patients with chronic hepatitis C. Comp Hepatol. 2004, 23: 8-10.1186/1476-5926-3-8.
Shaheen AA, Wan AF, Myers RP: FibroTest and FibroScan for the Prediction of Hepatitis C-Related Fibrosis: A Systematic Review of Diagnostic Test Accuracy. Am J Gastroenterol. 2007, 102: 2589-2600. 10.1111/j.1572-0241.2007.01466.x.
Parkes J, Guha IN, Roderick P, Harris S, Cross R, Manos MM, Irving W, Zaitoun A, Wheatley M, Ryder S, Rosenberg W: Enhanced Liver Fibrosis (ELF) test accurately identifies liver fibrosis in patients with chronic hepatitis C. J Viral Hepatitis. 2010,
Rosenberg WM, Voelker M, Thiel R, Becka M, Burt A, Schuppan D, Hubscher S, Roskams T, Pinzani M, Arthur MJ: Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004, 127: 1704-1713. 10.1053/j.gastro.2004.08.052.
Thein HH, Yi Q, Dore GJ, Krahn MD: Estimation of stage-specific fibrosis progression rates in chronic hepatitis C virus infection: a meta-analysis and meta-regression. Hepatology. 2008, 48: 418-431. 10.1002/hep.22375.
Bedossa P, Poynard T: An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996, 24: 289-293. 10.1002/hep.510240201.
Ludwig J, Dickson ER, McDonald GS: Staging of chronic nonsuppurative destructive cholangitis (syndrome of primary biliary cirrhosis). Virchows Arch A Pathol Anat Histol. 1978, 379: 103-112. 10.1007/BF00432479.
Imbert-Bismut F, Messous D, Thibault V, Myers RB, Piton A, Thabut D, Devers L, Hainque B, Mercadier A, Poynard T: Intra-laboratory analytical variability of biochemical markers of fibrosis (Fibrotest) and activity (Actitest) and reference ranges in healthy blood donors. Clin Chem Lab Med. 2004, 42: 323-333. 10.1515/CCLM.2004.058.
Ngo Y, Munteanu M, Messous D, Charlotte F, Imbert-Bismut F, Thabut D, Lebray P, Thibault V, Benhamou Y, Moussalli J, Ratziu V, Poynard T: A prospective analysis of the prognostic value of biomarkers (FibroTest) in patients with chronic hepatitis C. Clin Chem. 2006, 52: 1887-1896. 10.1373/clinchem.2006.070961.
Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, et al: Transient elastography: a new non-invasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003, 29: 1705-1713. 10.1016/j.ultrasmedbio.2003.07.001.
Poynard T, Halfon P, Castera L, Munteanu M, Imbert-Bismut F, Ratziu V, Benhamou Y, Bourliere M, de LV: Standardization of ROC Curve Areas for Diagnostic Evaluation of Liver Fibrosis Markers Based on Prevalences of Fibrosis Stages. Clin Chem. 2007, 53: 1615-1622. 10.1373/clinchem.2007.085795.
Halfon P, Munteanu M, Poynard T: FibroTest-ActiTest as a non-invasive marker of liver fibrosis. Gastroenterol Clin Biol. 2008, 32: 22-39. 10.1016/S0399-8320(08)73991-5.
Parkes J, Guha IN, Roderick P, Rosenberg W: Performance of serum marker panels for liver fibrosis in chronic hepatitis C. J Hepatol. 2006, 44: 462-474. 10.1016/j.jhep.2005.10.019.
Guha IN, Parkes J, Roderick P, Chattopadhyay D, Cross R, Harris S, Kaye P, Burt AD, Ryder SD, Aithal GP, Day CP, Rosenberg WM: Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: Validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology. 2008, 47: 455-460. 10.1002/hep.21984.
Nobili V, Parkes J, Bottazzo G, Marcellini M, Cross R, Newman D, Vizzutti F, Pinzani M, Rosenberg WM: Performance of ELF serum markers in predicting fibrosis stage in pediatric non-alcoholic fatty liver disease. Gastroenterology. 2009, 136: 160-167. 10.1053/j.gastro.2008.09.013.
Mayo MJ, Parkes J, Adams-Huet B, Combes B, Mills AS, Markin RS, Rubin R, Wheeler D, Contos M, West AB, Saldana S, Getachew Y, Butsch R, Luketic V, Peters M, Di BA, Bass N, Lake J, Boyer T, Martinez E, Boyer J, Garcia-Tsao G, Barnes D, Rosenberg WM: Prediction of clinical outcomes in primary biliary cirrhosis by serum enhanced liver fibrosis assay. Hepatology. 2008, 48: 1549-1557. 10.1002/hep.22517.
Cales P, Oberti F, Michalak S, Hubert-Fouchard I, Rousselet MC, Konate A, Gallois Y, Ternisien C, Chevailler A, Lunel F: A novel panel of blood markers to assess the degree of liver fibrosis. Hepatology. 2005, 42: 1373-1381. 10.1002/hep.20935.
Cobbold JF, Crossey MM, Colman P, Goldin RD, Murphy PS, Patel N, Fitzpatrick J, Vennart W, Thomas HC, Cox IJ, Taylor-Robinson SD: Optimal combinations of ultrasound-based and serum markers of disease severity in patients with chronic hepatitis C. J Viral Hepat. 2010, 17: 537-545. 10.1111/j.1365-2893.2009.01209.x.
Sebastiani G, Alberti A: Non invasive fibrosis biomarkers reduce but not substitute the need for liver biopsy. World J Gastroenterol. 2006, 12: 3682-3694.
Poynard T, Munteanu M, Imbert-Bismut F, Charlotte F, Thabut D, Le Calvez S, Messous D, Thibault V, Benhamou Y, Moussalli J, Ratziu V: Prospective analysis of discordant results between biochemical markers and biopsy in patients with chronic hepatitis C. Clin Chem. 2004, 50: 1344-1355. 10.1373/clinchem.2004.032227.
Mehta SH, Lau B, Afdhal NH, Thomas DL: Exceeding the limits of liver histology markers. J Hepatol. 2009, 50: 36-41. 10.1016/j.jhep.2008.07.039.
Ngo Y, Benhamou Y, Thibault V, Ingiliz P, Munteanu M, Lebray P, Thabut D, Morra R, Messous D, Charlotte F, Imbert-Bismut F, Bonnefont-Rousselot D, Moussalli J, Ratziu V, Poynard T: An accurate definition of the status of inactive hepatitis B virus carrier by a combination of biomarkers (FibroTest-ActiTest) and viral load. PLoS One. 2008, 3: e2573-10.1371/journal.pone.0002573.
Naveau S, Gaude G, Asnacios A, Agostini H, Abella A, Barri-Ova N, Dauvois B, Prevot S, Ngo Y, Munteanu M, Balian A, Njike-Nakseu M, Perlemuter G, Poynard T: Diagnostic and prognostic values of noninvasive biomarkers of fibrosis in patients with alcoholic liver disease. Hepatology. 2009, 49: 97-105. 10.1002/hep.22576.
Parkes J, Roderick P, Harris S, Gough C, Wheatley M, Day C, Mutimer D, Collier J, Alexander G, Lombard M, Ramage J, Dusheiko G, Burt A, Sampson E, Rosenberg W: European Liver Fibrosis (ELF) panel of serum markers can predict clinical outcome in a cohort of patients from England with mixed aetiology chronic liver disease. Hepatology. 2007, 46: S1-
Friedrich-Rust M, Wunder K, Kriener S, Sotoudeh F, Richter S, Bojunga J, Herrmann E, Poynard T, Dietrich CF, Vermehren J, Zeuzem S, Sarrazin C: Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009, 252: 595-604. 10.1148/radiol.2523081928.
Foucher J, Chanteloup E, Vergniol J, Castera L, Le Bail B, Adhoute X, Bertet J, Couzigou P, de Lédinghen V: Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut. 2006, 55: 403-408. 10.1136/gut.2005.069153.
Castera L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, Haaser M, Darriet M, Couzigou P, de Ledinghen V: Prospective comparison of transient elastography, fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005, 128: 343-350. 10.1053/j.gastro.2004.11.018.
Corpechot C, El Naggar A, Poujol-Robert A, Ziol M, Wendum D, Chazouilleres O, De Ledinghen V, Dhumeaux D, Marcellin P, Beaugrand M, Poupon R: Assessment of biliary fibrosis by transient elastography in patients with PBC and PSC. Hepatology. 2006, 43: 1118-1124. 10.1002/hep.21151.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-230X/10/103/prepub
Acknowledgements
The authors are indebted to Dr. Hanns Ackermann for providing us with easy to use software for the specific statistical analysis of this study. WMR is a member of the UCLH/UCL Comprehensive Biomedical Research Centre supported by the National Institute for Health Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The manuscript (including the article-processing charge) is not financed by any organization. The performance of the ELF-marker was supported by the National Institute for Health Research through the University College London Hospital Comprehensive Biomedical Research Centre. William Rosenberg has been paid for providing lectures by Siemens on the topic of the ELF marker. He is named inventor on a patent wholly owned by Siemens. He has no financial or non-financial competing interests of relevance to declare. In addition, the following authors have no competing interests or funding: Mireen Friedrich-Rust, Julie Parkes, Eva Herrmann, Stefan Zeuzem, Christoph Sarrazin.
Authors' contributions
MFR participated in the study design, data analysis and writing. WR participated in the study design, ELF testing, data analysis and writing. JP participated in the data analysis and writing. EH participated in the study design and performed the statistical analysis. SZ participated in the study design and coordination. CS conceived the study and participated in the study design and coordination. All authors collected and analyzed data, contributed to preparing the manuscript, and read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Friedrich-Rust, M., Rosenberg, W., Parkes, J. et al. Comparison of ELF, FibroTest and FibroScan for the non-invasive assessment of liver fibrosis. BMC Gastroenterol 10, 103 (2010). https://doi.org/10.1186/1471-230X-10-103
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-230X-10-103