Abstract
Background
Atrial fibrillation is a common serious cardiac arrhythmia. Knowing the prevalence of atrial fibrillation and documentation of medical management are important in the provision of primary care. This study sought to determine the prevalence of atrial fibrillation in a primary care population and to identify and quantify the treatments being used for stroke prevention in this group of patients.
Methods
A prevalence study through chart audit was conducted in the family medicine practice at the Sunnybrook campus of the Sunnybrook and Women's College Health Sciences Centre. The main outcome measures were the prevalence of atrial fibrillation in our primary care practice and the use of warfarin for stroke prevention in this population.
Results
261 patients in our practice have atrial fibrillation. The overall prevalence in our family practice unit is 3.9%. When considering patients aged 60 and over, the prevalence rises to 12.2%. 204 of our patients with atrial fibrillation (78.2%) are currently being treated with warfarin. Another 21 patients were previously treated and discontinued for a number of reasons. Of the 57 patients not currently treated with warfarin, 44 are treated with ASA, 2 with ticlopidine, and 11 are receiving no preventative treatment.
Conclusions
The prevalence of atrial fibrillation in our practice is higher than the range of prevalence reported in the general literature. However, our coverage with warfarin treatment exceeds previous reports in the literature.
Similar content being viewed by others
Background
Atrial fibrillation is an arrhythmia associated with serious morbidity, mortality and significant health services utilization. Atrial fibrillation is associated with 15% of cerebral vascular accidents [1, 2]. It has been conclusively shown that patients with non-valvular atrial fibrillation have five times the risk of stroke over the general population with an absolute risk of 2–6% per year in those without a previous CVA and 12–13% in those who have had a previous cerebrovascular event [3]. Despite its importance, atrial fibrillation frequently remains unrecognized in general practice.
Warfarin is an effective medical therapy for the prevention of stroke [4]. Prescribing of warfarin has increased as much as 4-fold over the last decade, likely as a result of the dissemination of clinical trials [5, 6], but evidence suggests that physicians are still treating anywhere from 10–50% of those patients with atrial fibrillation who would benefit from warfarin [7–11]. Furthermore, those who would benefit the most from treatment are elderly patients who are usually the group least likely to be treated [12]. The majority of medical care for this population is delivered in a primary care setting. Therefore, it is important to determine the number of patients in a practice with atrial fibrillation and to evaluate whether or not they are receiving optimum therapy.
The purpose of this study was twofold: to determine the prevalence of atrial fibrillation in an academic family practice setting and to document the treatments prescribed for this condition.
Methods
In this study, a complete detailed chart audit was performed to identify all patients with atrial fibrillation and the current treatment they are receiving. The audit comprised all patients registered in the practice who were seen at least once in the family practice unit during a 2 year period from January 1, 1999 to December 31, 2000 inclusive. The family practice unit consists of twelve full time equivalent physicians and six full-time equivalent nurses divided into three teams. These teams provide anticoagulation monitoring including venipuncture and warfarin dose adjustment. INR results are kept in a dedicated binder in the nursing stations for each team. There is an anticoagulation clinic also on site, but family practice provides anticoagulation to over 75% of patients receiving warfarin. The study was approved by the Research Ethics Board of the Sunnybrook and Women's College Health Sciences Centre.
Inclusion/Exclusion Criteria
Data was gathered on all patients identified as having chronic atrial fibrillation or at least one episode of paroxysmal atrial fibrillation during the two year period from January 1, 1999 to December 31, 2000. The presence of atrial fibrillation was based on documentation in the continuous patient profile, the clinic notes, consultant letters, emergency room or hospital discharge summaries, electrocardiograms, Holter monitors, echocardiograms, or stress test reports. Variables collected included age, sex, anti-coagulation treatment, and complications.
Analysis
Data was abstracted by a trained chart abstracter and verified by one of the study investigators (LC). All data was entered into a Microsoft database. Prevalence was calculated using the number of persons identified with atrial fibrillation divided by the number of patients in the 10 year age strata. Continuous variables are presented as mean (SD) and categorical variables as proportions with 95% confidence intervals. Statistical calculations were performed with EpiCalc 2000.
Results
Prevalence of atrial fibrillation
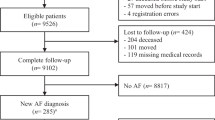
Two hundred and fifty-eight charts were identified as possible atrial fibrillation. Of these 258 charts, a more detailed audit excluded 22 of these patients with a remote history of atrial fibrillation (no recurrent episodes or persistent arrhythmia during the 2 year period from January 31, 1999 to December 31, 2000), 11 of these patients were misidentified and did not have atrial fibrillation, and 2 patients whose charts could not be found. In addition, 38 patients who were missed in the original chart audit were identified in the clinic anticoagulation record books. As a result of the audit, we identified a total of 261 patients (Table 1) in our family practice unit who have chronic atrial fibrillation or paroxysmal atrial fibrillation with at least one episode of arrhythmia during the 2 year period above.
The age range of our patients with atrial fibrillation is 40–97 years with an average age of 78.8 years and a standard deviation of 9.1 years (Table 2). There was no statistically significant difference in age between the sexes. The prevalence of atrial fibrillation in our population as a whole is 3.9 percent. When considering different age groups, the prevalence rises as high as 18.2 percent and 18.5 percent for patients aged 80–89 and 90–99 years respectively (Table 1).
Two hundred and nine of the 261 patients were identified by documentation of atrial fibrillation on the continuous patient profile (Table 3) at the front of the chart. Many charts had identifiable documentation in several of the areas described above. Seventeen patients had documentation in only one area. With regards to the type of atrial fibrillation in our 261 patients, 137 patients were classified as chronic, non-valvular, 113 as paroxysmal, and 11 as valvular.
Treatment
Two hundred and four of our 261 patients with atrial fibrillation are currently being treated with warfarin and another 21 patients had been previously treated (Table 4). This implies that 78.2 percent of our patients are treated with warfarin, and a total of 86.2 percent have been treated when including those who were previously treated and discontinued. There was an age relationship as the percentage of patients treated declined with each decade of age. Only 52% of patients over the age of 90 were treated with warfarin compared to 78–84% in the 60–89 age group (Table 5). With regard to treatment alternatives for anticoagulation, we found that 15 of our 204 patients currently treated with warfarin are taking ASA as well. Fifty-seven patients are not currently being treated with warfarin – of these, 44 are taking ASA, 2 are taking ticlopidine and 11 are receiving no anticoagulation.
As stated above, 21 patients who are not currently taking warfarin have been treated previously. The most common reason for stopping warfarin was successful electrical cardioversion, followed by bleeding complications and patient choice. The reason for discontinuing treatment was unclear in 4 patients. Thirty-six of our 261 patients have never been treated with warfarin. In the majority of patients, no reason was documented. The reasons that were documented include previous bleeding not on anticoagulation, fall risk, and patient choice. With regard to previous complications while taking warfarin, 26 episodes were documented. All of these were bleeding complications.
Discussion
The prevalence of atrial fibrillation in active patients at the family practice unit of Sunnybrook and Women's College Health Sciences Centre is 3.9 percent for all ages, and rises to 16 percent in patients aged 70 and over. This is higher than the prevalence suggested in previous reports [13].
Several factors may explain our high prevalence. The family physicians and residents at Sunnybrook may be more successful at identifying and documenting cases of atrial fibrillation than the physicians whose patients were used in previous studies. In addition, we may have more patients with atrial fibrillation as a result of being a tertiary care academic centre with cardiology services on site. Finally, a complete chart audit, which we performed, is the gold standard in a primary care setting, for identifying the most patients with a given condition. The use of a computer to search billing codes and prescriptions has been shown to miss as many as 30 percent of the patients in question [14].
Currently, 78.2 percent of our patients are being treated with warfarin for stroke prevention. Another 8 percent of our patients were previously treated with warfarin that was discontinued for a number of reasons described earlier. This implies a coverage rate of 86.2 percent of our atrial fibrillation patients treated with warfarin. When including alternatives to warfarin for anticoagulation, we find that 95.8 percent of our population are treated.
These results demonstrate that it is possible to achieve high coverage rates with warfarin in elderly patients with atrial fibrillation in the primary care setting. Our results compare favourably with the 10–50 percent coverage reported in previous studies [6–10].
What accounts for such high coverage levels? Our results may be attributable to our physicians', residents' and nurses' knowledge of atrial fibrillation due to having a large number of these patients, as well as being at an academic centre, with a close working relationship with our cardiologists. Patient-physician interactions may also play a role. Warfarin therapy may be framed by clinicians in a positive manner. It is unclear how the risks and benefits of warfarin are described to patients in clinical practice, but research evidence suggests that patients are sensitive to how risks are framed. Howitt and Armstrong found that health beliefs were important in determining choice of treatment and that those seeking a higher level of benefit were less likely to take warfarin [15]. Protheroe et al found that a shared decision-making approach led to fewer patients accepting warfarin therapy than would be expected by guidelines [16]. How patients in our practice view the risks and benefits of warfarin therapy, and how it was communicated to them, will be assessed by a survey and qualitative study.
One potential risk of our high levels of coverage is prophylaxis of younger patients. Currently, all of our patients under age 60 with atrial fibrillation are being treated with warfarin. The most influential set of guidelines for choice of therapy in atrial fibrillation suggests that patients with non-valvular atrial fibrillation under age 65 without any other risk factors for stroke are better treated with ASA since the bleeding risks on warfarin outweigh the preventive benefits [17].
Is this level of coverage appropriate? Guidelines on anticoagulation treatment for atrial fibrillation are highly variable. Thomson et al. showed that guidelines varied in terms of treatment advice. In their study, 13–100% of patients would be treated with warfarin [18] Placebo controlled trials favour warfarin treatment. A recently published systematic review of trials comparing antiplatelet treatment and anticoagulation suggested that warfarin may not be superior as a treatment option [19]. However, Cochrane Reviews support the use of warfarin for atrial fibrillation, with or without previous ischaemic events [20–22]. Thus, the evidence seems to favour warfarin treatment, and the goal for clinicians should be to achieve as high a coverage as appropriate given patient preferences. Identification of which patients are most likely to benefit from warfarin therapy is facilitated by the development of decision aids, as clinical practice guidelines are inconsistent or unclear [23].
With regard to our patients who are not currently treated with warfarin but who have previously been treated, most of the reasons for discontinuing the medication are identifiable and appropriate. There is greater uncertainty around those who have never been treated. In most cases no reason can be identified.
This study is limited by its potential lack of applicability in other community settings. However, the predominantly elderly population reflects future demographic trends. Also, potential cases of atrial fibrillation may have been missed had these patients not visited the clinic in the previous two years. Additionally, cases of atrial fibrillation may have been missed in the chart audit.
Conclusions
In conclusion, this study confirms that atrial fibrillation is a very common problem in primary care, affecting 18% of patients over 80. The high prevalence of atrial fibrillation and the availability of a safe and effective therapy suggests the utility of screening for atrial fibrillation in the elderly population. A prospective study to determine whether systematic screening for atrial fibrillation in the elderly reduces stroke morbidity and mortality is recommended. The study also shows that it is possible to achieve high coverage rates of warfarin therapy in primary care. This argues for the development of tools to enable primary care providers to ascertain the prevalence of atrial fibrillation in their practice, discover those patients not receiving optimal therapy and discuss treatment options with these patients.
References
Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT: Why do patients with atrial fibrillation not receive warfarin?. Arch Intern Med. 2000, 160: 41-46. 10.1001/archinte.160.1.41.
Antithrombotics and stroke in AF. Bandolier [Electronic]. 1999, 70 (2): [http://www.jr2.ox.ac.uk/Bandolier/bank70/b70-2.html]
Hart RG, Benavente O, McBride R, Pearce LA: Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann Intern Med. 1999, 131: 492-501.
Benavente O, Hart R, Koudstaal P, Laupacis A, McBride R: Oral anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks (Cochrane Review). In: The Cochrane Library, Issue 3. Oxford: Update Software. 2001
Thromboembolic prophylaxis in 3575 hospitalized patients with atrial fibrillation. The Clinical Quality Improvement Network (CQIN) Investigators. Can J Cardiol. 1998, 14: 695-702.
Li-Saw-Hee FL, Lip GY: Atrial fibrillation, thromboembolism and antithrombotic therapy. Int J Clin Pract. 1999, 53: 110-117.
Smith NL, Psaty BM, Furberg CD, White R, Lima JA, Newman AB, Manolio TA: Temporal trends in the use of anticoagulants among older adults with atrial fibrillation. Arch Intern Med. 1999, 159: 1574-1578. 10.1001/archinte.159.14.1574.
Mead GE, Wardlaw JM, Lewis SC, McDowall M, Dennis MS: The influence of randomized trials on the use of anticoagulants for atrial fibrillation. Age Ageing. 1999, 28: 441-446. 10.1093/ageing/28.5.441.
Hart RG: Warfarin in atrial fibrillation: underused in the elderly, often inappropriately used in the young. Heart. 1999, 82: 539-540.
Perez I, Melbourn A, Kalra L: Use of antithrombotic measures for stroke prevention in atrial fibrillation. Heart. 1999, 82: 570-574.
McCrory DC, Matchar DB, Samsa G, Sanders LL, Pritchett EL: Physician attitudes about anticoagulation for nonvalvular atrial fibrillation in the elderly. Arch Intern Med. 1995, 155: 277-281. 10.1001/archinte.155.3.277.
Tong DC, Albers GW: Antithrombotic management of atrial fibrillation for stroke prevention in older people. Clin Geriatr Med. 1999, 15: 645-662.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE: Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001, 285: 2370-2375. 10.1001/jama.285.18.2370.
Gray J, Majeed A, Kerry S, Rowlands G: Identifying patients with ischaemic heart disease in general practice: cross sectional study of paper and computerised medical records. BMJ. 2000, 321: 548-550. 10.1136/bmj.321.7260.548.
Howitt A, Armstrong D: Implementing evidence based medicine in general practice: audit and qualitative study of antithrombotic treatment for atrial fibrillation. BMJ. 1999, 318: 1324-1327.
Protheroe J, Fahey T, Montgomery AA, Peters TJ: The impact of patients' preferences on the treatment of atrial fibrillation: observational study of patient based decision analysis. BMJ. 2000, 320: 1380-1384. 10.1136/bmj.320.7246.1380.
Laupacis A, Albers G, Dalen J, Dunn MI, Jacobson AK, Singer DE: Antithrombotic therapy in atrial fibrillation. Chest. 1998, 114: 579S-589S.
Thomson R, McElroy H, Sudlow M: Guidelines on anticoagulant treatment in atrial fibrillation in Great Britain: variation in content and implications for treatment. BMJ. 1998, 316: 509-513.
Taylor FC, Cohen H, Ebrahim S: Systematic review of long term anticoagulation or antiplatelet treatment in patients with non-rheumatic atrial fibrillation. BMJ. 2001, 322: 321-326. 10.1136/bmj.322.7282.321.
Koudstaal P: Anticoagulants for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischemic attacks (Cochrane Review). In: The Cochrane Library, Issue 3. Oxford: Update Software. 2001
Segal J, McNamara R, Miller M, Powe N, Goodman S, Robinson K, Bass E: Anticoagulants or antiplatelet therapy for non-rheumatic atrial fibrillation and flutter (Cochrane Review). In: The Cochrane Library, Issue 3. Oxford: Update Software. 2001
Benavente O, Hart RG, Koudstaal P, Laupacis A, McBride R: Antiplatelet therapy for preventing stroke in patients with non-valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks (Cochrane Review). In: The Cochrane Library, Issue 3. Oxford: Update Software. 2001
Thomson R, Parkin D, Eccles M, Sudlow M, Robinson A: Decision analysis and guidelines for anticoagulant therapy to prevent stroke in patients with atrial' fibrillation. Lancet. 2000, 355: 956-962. 10.1016/S0140-6736(00)90012-6.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2296/3/11/prepub
Acknowledgements
The authors would like to thank Victoria Patchett for her assistance in abstracting the charts and Shari Gruman for help in preparing the manuscript. This study was funded by a resident research grant from Physicians' Services Incorporated. Dr Upshur is supported by a New Investigator Award from the Canadian Institutes of Health Research and a Research Scholar Award from the Department of Family and Community Medicine at the University of Toronto.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
LC and RU jointly conceived and designed the project. LC supervised and participated in the chart audit. RU conducted the statistical analysis. Both authors contributed to the writing of the drafts and read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ceresne, L., Upshur, R.E. Atrial fibrillation in a primary care practice: prevalence and management. BMC Fam Pract 3, 11 (2002). https://doi.org/10.1186/1471-2296-3-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2296-3-11