Abstract
Background
Most evidence on chronic diseases has been collected for single diseases whereas in reality, patients often suffer from more than one condition. There is a growing need for evidence-based answers to multimorbidity, especially in primary care settings where family doctors (FD’s) provide comprehensive care for a high variety of chronic conditions. This study aimed to define which disease and problem combinations would be most relevant and useful for the development of guidelines to manage multimorbidity in primary care.
Methods
A practice-based cross sectional analysis of clinicians’ chart reviews in 543 patients aged over 65 registered within two family practices in Ghent, Belgium. Main outcome measures were prevalence of disease and problem combinations and association strengths.
Results
The prevalence of multimorbidity (Cumulative Illness Rating Scale >1) in the study sample is 82.6%. The most prevalent combination is hypertension-osteoarthritis (132/543). Moderate to strong associations (Yules Q > 0.50) are reported for 14 combinations but the corresponding prevalences are mostly below 5%. More than half of these associations show a contribution of a psychiatric problem or a social problem.
Conclusions
This study confirms the high prevalence of multimorbidity in patients aged over 65 in primary care. Hypertension-osteoarthritis is defined as a frequent combination however 94% of these patients have more than two disorders. The low prevalence of specific combinations, the high prevalence of psychiatric and social problems and the general complexity of multimorbidity will hamper the usefulness of randomized trials or guidelines at practice level. There is a need to explore new paradigms for addressing multimorbidity.
Similar content being viewed by others
Background
Multimorbidity is clearly on the rise [1, 2] and a challenge for clinical practice [3, 4]. In family practice, patients with multimorbidity are the rule rather than the exception [5]. Yet, most available evidence to treat chronic diseases has been collected in single disease trials, often excluding patients with comorbid diseases. Clinicians feel a growing need for evidence that can be applied to patients with multiple diseases [6, 7]. A possible solution to tackle this evidence gap may be to look for specific disease combinations with a high prevalence and to engage in the development of randomized clinical trials or guidelines on patients with these combinations of diseases [8, 9]. Few studies have focused on how diseases co-occur. Mostof these studies assess comorbidity instead of multimorbidity. Comorbidity implies an index disease (e.g. Chronic Obstructive Pulmonary Disease (COPD) and comorbidity) whereas multimorbidity is defined as any co-occurrence of medical conditions within a person. From the perspective of primary health care multimorbidity is more relevant because general practitioners deal with the broad spectrum of the morbidity of the patient without prioritizing specific disease categories. In order to fill the evidence-gap for multimorbidity we need to focus on those problems that influence clinical management at the patient level [3, 4]. However, most studies use large databases from population surveys or automated extraction of disease codes out of medical records or insurance claims. Datasets based on automatized extraction of disease codes do not necessarily identify the problems that are relevant at the point of care [3]. They might also lead to over- or underestimation of diseases. For example, a disease code on low back pain might relate to a patient that only consulted for advice but the same disease code could also relate to a patient with severe impairment, decreased quality of life or intensive need for physiotherapy. This study aims to identify the problems that influence clinical management at the patient level in primary care in order to identify combinations of problems that could be a relevant focus for trials or guidelines for patients with multimorbidity.
Methods
Subjects
We conducted a practice-based cross sectional analysis of the patient records of all patients aged 65 or older who were registered in two community health centers (CHC) in Ghent, Belgium. CHC’s provide interdisciplinary comprehensive primary health care using a capitation payment system accessible for all people residing in the area covered by the CHC. The choice for CHC’s was based on the fact that the capitation based system enhances continuity of care and consequently leads to more complete information in patients’ medical records. The CHCs with the largest patient lists were chosen for inclusion of patients.
Chart review
Medical records in the participating practices are based on the problem-oriented medical record model as proposed by Weed (1968) [10] in which the patient's history, physical findings, laboratory results, etc. are organized around patient’s problems. These medical records include a list of all the problems of the patient including both clearly established diagnoses (such as diabetes II or COPD) and other problems relevant for patient management in primary care (such as “symptom diagnoses”, social problems,…). The underlying classification used in these records is the International Classification of Primary Care (ICPC) [11] For each problem presented by the patient, information is registered in the SOAP-format (subjective (S), objective (O) assessment (A) diagnostic and treatment plans (P). Three family doctors (PB, GG and SG), who were part of the medical staff of the participating practices, performed a detailed clinical review of each electronic patient record (EPR) and its additional paper file. They assessed whether or not a problem was of influence on the management for that patient. For each patient this resulted in a list of all problems with clinically relevant impact, including social problems and relevant medical history. To provide an estimation of the prevalence of multimorbidity in the study sample all patients were allocated a Cumulative Illness Rating Scale (CIRS) score based on the scoring guidelines published by Hudon [12–14]. To harmonize the clinical assessment, data extraction and allocation of the multimorbidity scores, 30 patient records were independently reviewed by the three family doctors who performed the assessment and results were compared and discussed in a meeting to attune the assessment approach. Every patient’s problem list was anonymized and transferred into a separate database for analysis. In order to find a reasonable way for including all relevant but often low prevalent problems into a sensible analysis of combinations a process of summarization was performed in which the research team constructed a list of 23 problems (Table 1). In this list different levels of detail were used: some disorders like COPD, diabetes and depression were analyzed at disease level, disorders like osteoarthritis and cardiac rhythm disorders were considered as “diagnostic group” and other disorders were summarized at the level of a body system (eg the EENT (Eye Ear Nose and Troat) system and the neurological system). Although they are not considered in the CIRS social problems were also included because of their possible relevance to the patients’ clinical management at the point of care.
Analysis of combinations
To reveal the combinations which occur most frequently, prevalences were calculated for all possible combinations of these 23 problems. Next to the prevalence, Yules Q was used to measure the strength of the association for each possible combination. Yule’s Q is a symmetric measure taking on values between −1 and +1. One implies perfect negative or positive association, 0 (zero) no association. Yules Q measures > 0,70 represent strong associations and Yules Q measures < 0,70 and > 0,50 represent moderate associations [15]. A percentile bootstrap [12] procedure with 1000 data sets was used to estimate the 95% confidence interval for the Yules Q coefficients. All analyses were supported by SPSS version 19.0.
Ethical approval
Ethical approval was provided by the Ethics Committee of Ghent University Hospital. The Belgian registration number of the approval for the data collection performed by GG and PB is B67020108605 and for the data collection of SG is B67020108596.
Results
Study population
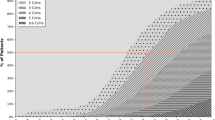
On 1st of October 2009, the practices under study listed 543 patients aged 65 or older. The mean age of patients in the study sample is 73 years (range 65–97), 47,3% of patients are male and 4,4% have no chronic disease (CIRS =0). The prevalence of multimorbidity (CIRS > 1) is 82.6% and 64.2% of the patients included have a CIRS score >2 (Figure 1). The most frequently affected CIRS domains are the endocrine (47,4%) and the musculoskeletal system (47%) followed by the cardiac system (30,4%). The most frequent disorders are hypertension (48,4%), osteoarthritis (48,4%), COPD (14,2%), ischemic heart disease (14,2%) and diabetes (14,2%). Table 1 reports the prevalence for the 23 problems which were used for further analysis of combinations.
Combinations with a prevalence >5%
Table 2 shows all 39 problem pairs which occur frequently (prevalence > 5%). The most prevalent combination is hypertension-osteoarthritis (n = 132 Yules Q 0.11 CI : −0.06-0.28). More than 2 out of 3 of these combinations include hypertension or osteoarthritis and only 4 of these combinations are moderately or strongly associated (Yules Q > 0.50) : hypertension-renal system (Yules Q 0,52), osteoarthritis –lower gastro-intestinal system (Yules Q 0,54), psychiatric system – social problem (Yules Q 0,66) and diabetes –overweight (Yules Q 0,74).
Combinations with a strong or moderate association
Table 3 shows all 14 combinations with a strong or moderate association (Yules Q > 50). Diabetes-overweight (Yules Q : 0,74; CI : 0,57-0,84; n = 28) and nicotine abuse-alcohol abuse (Yules Q : 0,73; CI : 0,48-0,98; n = 6) emerged as the most strongly associated combinations (Yules Q >0,7). Social problems, psychiatric issues and locomotor problems (osteoarthritis and osteoporosis) are well represented within the list of combinations with a moderate association (Yules’ Q 0,5-0,7). Most of these associations (9/14) have prevalences below 5%.
Discussion
This study aimed to include those disorders that influence the clinical management of patients and used clinician chart review to do so. By means of a practice-based analysis of individual patient records it was able to assess which combinations would be most relevant for the development of guidelines useful at practice level in primary care. Hypertension-osteoarthritis was identified as a most prevalent combination of diseases (24,3% of the study sample) but the association was not significant. The significant associations described in Table 3 generally show very low prevalence. In general this study indicates that the usefulness of RCT’s on disease combinations will be hampered by low prevalence at practice level, low association strengths and the fact that many patients present with more than 2 problems (64.2% of the study sample has a CIRS score > 2).
The combination hypertension-osteoarthritis has been described previously as the most prevalent combination in older persons [14]. Building evidence to manage patients with this combination could be useful because non-steroidal-anti-inflammatory-drugs (NSAIDs) might interfere with blood pressure control and keeping up an active life style can be difficult when suffering from osteoarthritis. Most other combinations with a considerable prevalence (which we have set at >5%) often include diagnostic groups (e.g. rhythm disorders) or body systems (e.g. neurological system) to which guidelines are not directly applicable. The combinations hypertension-diabetes, hypertension-lipid disorder, hypertension-overweight, hypertension-ischemic heart disease, hypertension-heart failure and diabetes-overweight are quite well covered within disease-specific guidelines because these combinations concern well established comorbid conditions based on causal associations [16, 17]. Many of the other combinations include osteoarthritis. Despite the existence of osteoarthritis guidelines [18], a standardized approach of the disorder is hampered due to the differing localization and the varying impact of the disorder on functional limitations and quality of life. Other combinations with considerable prevalence include mental health problems and social problems which is not only related to the high prevalence of both problems in this sample (psychiatric disorders (20,6%) and social problems (14,0%)) because remarkably, these problems are also highly represented in the associations with a moderate to strong correlation (Table 3). The importance of psychiatric comorbidity has been described previously [19] but to our knowledge there were no studies including social problems. From the perspective of clinical care psychosocial problems are very relevant as they can hamper compliance to disease specific guidelines for diabetes, heart failure,… [6,25] both in patients and providers. Qualitative inquiries in family doctors have also described them to be the main challenges within the management of multimorbidity [7].
Multimorbidity is not limited to a specific set of chronic conditions
Our study confirms the low prevalence of specific combinations described in earlier studies and highlights the heterogeneity of multimorbidity described in other populations [19–22]. The study of Van Oostrom et al. [19] selected 9 chronic diseases for analysis of disease pairs with 29 other disease codes. Only one combination (depression-anxiety) was found to have a prevalence over 5% and 70% of patients had a comorbid disease which was not included within the nine most common chronic conditions. Despite the fact that Van Oostrom et al. included a younger population (patients aged over 55) and provided a less comprehensive assessment of multimorbidity, their main results are in line with our findings showing a wide variety in multimorbidity which is not limited to a specific list of chronic conditions.
Tailored instead of standardized care
Our results have also clearly indicated that the usefulness of guidelines on disease combinations will not only be hampered by the low prevalence of the combinations, but even more by the fact that 94% of the patients with hypertension and osteoarthritis had additional problems and 64.2% of the patients in this sample had a CIRS > 2. Van den Bussche et al. [21] have described that 64% of patients with three or more diseases (out of a list of 64) were defined with a triade within the six most prevalent conditions (hypertension, lipid disorder, diabetes, low back pain, osteoarthritis, ischemic heart disease). They suggested that an adjustment and alignment of clinical guidelines for these six conditions would constitute a big step towards an adaptation of guidelines for multimorbid patients. However, these six problems include conditions which might have a very differing impact at patient level (for example low back pain and osteoarthritis) which may hamper the use of standardized guidelines. Moreover, our study has indicated a considerable prevalence of mental health problems and social problems which will also be less easily included in standardized guidelines and programs because they often require tailored and individualized instead of programmed and standardized care.
Strengths and limitations
The main strength of this study is that the morbidity estimates are derived from chart review rather than automated diagnostic codes [22]. This enabled a comprehensive assessment of multimorbidity including merely problems that were significant for the clinical management of the patient and enabling the inclusion of all problems whereas most studies are obliged to a pre-selection of chronic diseases [21–23]. This practice-based individualized assessment by family doctors provides a comprehensive insight in the day to day presentation of multimorbidity in primary care. The individualized assessment by clinicians may hamper validity of data but first, chart review within primary care has been validated for the assessment of multimorbidity [24] and second, the assessment approach has been harmonized. The results of this study require cautious interpretation mostly because prevalence figures on multimorbidity are highly determined by study design and datasources [20, 21]. Fortin et al. have indicated that prevalence estimates are higher in the primary care setting than in the general population [21, 22]. Moreover, because we were able to include every condition instead of a limited list higher prevalence figures are to be expected [21]. Because the aim of this specific study included an assessment of multimorbidity the way it presents to family doctors we believe our results indicate that the usefulness of guidelines on guidelines for disease combinations will be hampered at the level of clinical practice. A main disadvantage of our method is that detailed clinical review is not feasible for larger samples. The analysis of only 543 patients in two family practices in Belgium should be considered a limitation as is the fact that we only assessed combinations whereas many patients have more than two problems. The generalizability of our results may also be hampered due to the particularly deprived population within the CHC’s and the inclusion of older patients. However, the high morbidity load and complexity of this population should have been suitable to retrieve the combinations which in the end are relevant at practice level in primary care.
Conclusion
Our results show that patients with multimorbidity often have complex and unique combinations of problems. Low prevalence of disease combinations at practice level and the fact that many patients have more than two problems which influence clinical management make it unlikely that performing trials or developing guidelines for people with specific combinations will ever be useful at the level of clinical practice. The need for an individual approach is further emphasized by the high prevalence of social and psychiatric problems. We need to explore new generic ways and paradigms to approach patients with multimorbidity which allow to tailor care to each individual patient [19].
Abbreviations
- FD:
-
Family doctor
- (E)PR:
-
(Electronic) Patient record
- SOAP-format:
-
Subjective (S), objective (O) assessment (A) and diagnostic and treatment plans (P)
- CIRS:
-
Cumulative illness rating scale
- EENT:
-
Eye, ear, nose and throat system
- COPD:
-
Chronic obstructive pulmonary disease
- NSAIDs:
-
Non steroidal anti-inflammatory drugs
- TIA:
-
Transient ischemic attack
- CVA:
-
Cerebrovascular accident.
References
Anderson G: Chronic Conditions: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation, 08543-2316
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B: Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012, 380 (9836): 37-43. 10.1016/S0140-6736(12)60240-2.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M: Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009, 7 (4): 357-363. 10.1370/afm.983.
Starfield B: Threads and yarns: weaving the tapestry of comorbidity. Ann Fam Med. 2006, 4 (2): 101-103. 10.1370/afm.524.
Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L: Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005, 3 (3): 223-228. 10.1370/afm.272.
Boyd CMDJ, Boult C, Fried LP, Boult L, Wu AW: Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases. JAMA. 2005, 294: 716-724. 10.1001/jama.294.6.716.
Luijks HD, Loeffen MJ, Lagro-Janssen AL, van Weel C, Lucassen PL, Schermer TR: GPs’ considerations in multimorbidity management: a qualitative study. Br J Gen Pract. 2012, 62 (600): e503-e510. 10.3399/bjgp12X652373.
Fabbri LM, Luppi F, Beghe B, Rabe KF: Complex chronic comorbidities of COPD. Eur Respir J. 2008, 31 (1): 204-212. 10.1183/09031936.00114307.
Schafer I, von Leitner EC, Schon G, Koller D, Hansen H, Kolonko T, Kaduszkiewicz H, Wegscheider K, Glaeske G, van den Bussche H: Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One. 2010, 5 (12): e15941-10.1371/journal.pone.0015941.
Weed LL: What physicians worry about: how to organize care of multiple-problem patients. Mod Hosp. 1968, 110 (6): 90-94.
Prepared by the International Classification Committee of WONCA: ICPC-2 International Classification of Primary Care. 1998, Oxford: Oxford University Press, 2
Hudon C, Fortin M, Soubhi H: Abbreviated guidelines for scoring the Cumulative Illness Rating Scale (CIRS) in family practice. J Clin Epidemiol. 2007, 60 (2): 212-Epub 2006 Nov 13
Lewis-Beck MS, Bryman A, Liao TF: Encyclopedia of Social Science Research Methods. 2004, Thousand Oaks, CA: SAGE Publications, Inc, 1-3: http://dx.doi.org/10.4135/9781412950589,
Knoke D, Bohrnstedt W: Basic Social Statistics. 1991, Itasca, IL: F.E. Peacock Publishers
Mooney CZ DR: Bootstrapping: A Nonparametric Approach to Statistical Inference. 1993, Thousand Oaks, CA: Sage Publications
Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, Peters A, Ladwig KH, Doring A: Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PloS one. 2012, 7 (1): e30556-10.1371/journal.pone.0030556.
Jaques H, National Institute for clinical excellence (NICE): NICE guideline on hypertension. Eur Heart J. 2013, 34 (6): 406-408.
Sibal L, Home PD: Management of type 2 diabetes: NICE guidelines. Clin Med. 2009, 9 (4): 353-357. 10.7861/clinmedicine.9-4-353.
Conaghan PG, Dickson J, Grant RL: Guideline Development Group.Care and management of osteoarthritis in adults: summary of NICE guidance. BMJ. 2008, 336 (7642): 502-503. 10.1136/bmj.39490.608009.AD. doi:10.1136/bmj.39490.608009.AD
Dawes M: Co-morbidity: we need a guideline for each patient not a guideline for each disease. Family Practice. 2010, 27 (1): 1-2. 10.1093/fampra/cmp106.
van den Bussche H, Schafer I, Wiese B, Dahlhaus A, Fuchs A, Gensichen J, Hofels S, Hansen H, Leicht H, Koller D, Luppa M, Nutzel A, Werle J, Scherer M, Wegscheider K, Glaeske G, Schon G: A comparative study demonstrated that prevalence figures on multimorbidity require cautious interpretation when drawn from a single database. J Clin Epidemiol. 2013, 66 (2): 209-217. 10.1016/j.jclinepi.2012.07.019.
Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H: A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012, 10 (2): 142-151. 10.1370/afm.1337.
van Oostrom SH, Picavet HS, van Gelder BM, Lemmens LC, Hoeymans N, van Dijk CE, Verheij RA, Schellevis FG, Baan CA: Multimorbidity and comorbidity in the Dutch population - data from general practices. BMC Public Health. 2012, 12: 715-10.1186/1471-2458-12-715.
Hudon C, Fortin M, Vanasse A: Cumulative Illness Rating Scale was a reliable and valid index in a family practice context. J Clin Epidemiol. 2005, 58 (6): 603-608. 10.1016/j.jclinepi.2004.10.017.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2296/15/159/prepub
Acknowledgements
We want to gratefully acknowledge the Family Doctors of the participating Community Health Care Centers for their cooperation on the problem lists of the patients included in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
PB has performed detailed clinical review of the patient records in community health centre Botermarkt and has continuously supervised and coordinated the assessment of SG and GG. SG has performed detailed clinical review of the patient records in community health centre De Sleep and GG has performed detailed clinical review of the patient records in community health centre Botermarkt. PB has performed all data analyses and has written the manuscript. JDM has provided continuous input and support on the study method, data analysis and writing of the manuscript. WP provided methodological advice and has supported the statistical analysis of the data. GB has assisted in the set up of the study. ADS has supervised the whole study including all research team meetings, data collection, data analysis and the writing of the manuscript. All authors had full access to the data and can take responsibility for the integrity of the data and the accuracy of the analyses. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Boeckxstaens, P., Peersman, W., Goubin, G. et al. A practice-based analysis of combinations of diseases in patients aged 65 or older in primary care. BMC Fam Pract 15, 159 (2014). https://doi.org/10.1186/1471-2296-15-159
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2296-15-159