Abstract
Background
Studies have demonstrated that the use of implantable cardioverter defibrillators (ICDs) is effective for the primary prevention of arrhythmic events but due to imposing costs, there remains a need to identify which patients will derive the greatest benefit. Microvolt T-wave alternans (MTWA) has been proposed to assist in this stratification.
Methods
We systematically searched the literature using MEDLINE, EMBASE, Current Contents, the Cochrane Library, INAHTA, and the Web of Science to identify all primary prevention randomized controlled trials and prospective cohort studies with at least 12 months of follow-up examining MTWA as a predictor of mortality and severe arrhythmic events in patients with severe left-ventricular dysfunction. The search was limited to full-text English publications between January 1990 and May 2007. The primary outcome was a composite of mortality and severe arrhythmias. Data were synthesized using Bayesian hierarchical models.
Results
We identified no trials and 8 published cohort studies involving a total of 1,946 patients, including 332 positive, 656 negative, 84 indeterminate, and 874 non-negative (which includes both positive and indeterminate tests) MTWA test results. The risk of mortality or severe arrhythmic events was higher in patients with a positive MTWA compared to a negative test (RR = 2.7, 95% credible interval (CrI) = 1.4, 6.1). Similar results were obtained when comparing non-negative MTWA to a negative test.
Conclusion
A positive MTWA test predicts mortality or severe arrhythmic events in a population of individuals with severe left ventricular dysfunction. However, the wide credible interval suggests the clinical utility of this test remains incompletely defined, ranging from very modest to substantial. Additional high quality studies are required to better refine the role of MTWA in the decision making process for ICD implantation.
Similar content being viewed by others
Background
Implantable cardioverter defibrillators (ICDs) decrease mortality principally by detecting and treating tachyarrhythmias, the most common cause of sudden cardiac death (SCD)[1]. Although ICDs were originally used for secondary prevention among survivors of cardiac arrest or malignant arrhythmias, they have also been effective for primary prevention in high-risk patients without a history of malignant arrhythmias or SCD [2, 3]. Consequently, prophylactic ICD therapy has been recommended for patients with reduced ejection fractions, resulting in a large number of potentially eligible patients [2, 4, 5]. Due to the substantial costs, as well as potential physical and psychological adverse effects, there is a need for better patient selection [6]. Novel diagnostic tests may have a role in improving risk stratification for ICD implantation [4].
Microvolt T-wave alternans (MTWA) represents a promising candidate test to stratify the risk among a primary prevention population [7, 8]. MTWA, which usually involves an exercise treadmill test, is non-invasive and relatively inexpensive. Some studies have suggested that patients with negative MTWA tests have an extremely low risk for SCD or cardiac arrest [7] but conflicting opinions exists [9–12]. We therefore undertook a systematic review and meta-analysis to determine the utility of MTWA for risk stratification for primary prevention of patients with severe left ventricular dysfunction. Our objectives were to systematically review the existing medical literature and quantitatively summarize the utility of MTWA in performing primary prevention risk stratification.
Methods
Search Criteria
We performed a systematic literature search for all randomized controlled trials and prospective cohort studies published in English between January 1990, 4 years before the publication of the first clinical application of MTWA [13], and May 2007. Using the terms "MTWA" or "T wave alternans", we searched the following databases: MEDLINE, EMBASE, Current Contents, and the Web of Science, restricting our search to full text articles involving human subjects. We also hand-searched The Cochrane Library, INAHTA, and references of relevant articles, reviews, and previous meta-analyses for additional studies. Since only observational studies were identified, all elements of this meta-analysis strictly followed the guidelines described in the Meta-analysis of Observational Studies in Epidemiology (MOOSE) proposal [14].
Inclusion Criteria
We downloaded all identified articles to Reference Manager (Version 11), and study eligibility was assessed first by examining titles and abstracts (CJA). We restricted our meta-analysis to studies examining MTWA in primary prevention. We excluded studies with patient populations involving a history of (resuscitated) cardiac death or malignant arrhythmias, Brugada Syndrome, or Long QT Syndrome. The inclusion criteria were: 1) original full length research article; 2) randomized controlled trial or prospective cohort study design; 3) exercise-induced application of MTWA; 4) human participants with left-ventricular dysfunction and no history of previous arrhythmic event; 5) reported meaningful clinical endpoints including all-cause mortality (ACM), SCD, severe arrhythmias, ventricular tachycardia (VT), ventricular fibrillation (VF), or ICD shock as a function of MTWA results. We contacted study authors to resolve important ambiguities (n = 2). Duplicate publications, studies with a follow-up of less than 12 months, and studies in patients without severe left ventricular dysfunction (due to their underlying low arrhythmic risk and fundamental differences from patients with established cardiovascular disease) were excluded. We defined patients with severe left ventricular dysfunction as those with an ejection fraction of ≤ 35%.
Data Extraction
Two investigators (CJA and KBF) independently extracted data using a structured and pilot-tested extraction form, with discrepancies resolved by consensus. Abstracted data included: study design, study funding, inclusion and exclusion criteria, details regarding MTWA testing and classification of results, baseline demographic and clinical characteristics of participants, duration of follow-up, endpoints evaluated, multivariable analyses, and main conclusions.
We assessed study quality with a modified 7-item list based on QUADAS [15], a quality assessment tool used for diagnostic accuracy studies [see Additional file 1]. We could not use QUADAS directly as no standard reference test was available. Briefly, studies received one point for each item they reported, for a maximum score of 7. We then classified studies as having good (≥ 6), moderate (≤ 4 and < 6), or poor (< 4) quality. This quality assessment was not used to assess study inclusion or exclusion, but was included as a study characteristic.
Statistical Analyses
Our primary analysis examined MTWA as a predictor of a composite of mortality or severe arrhythmic events in primary prevention of patients with severe left-ventricular dysfunction. In secondary analyses, we examined the use of MTWA uniquely as a predictor of mortality (all-cause mortality, cardiac death, and/or arrhythmic death). For each study, we determined: the percentage of patients tested as positive, negative, or indeterminate, and the percentage of patients who had the endpoint in each of these MTWA categories. Since some studies did not report outcomes for patients in the indeterminate category, the sensitivity and specificity reported in these studies are not valid measures. In studies with available data, we re-calculated sensitivity, specificity, and positive and negative predictive values by comparing non-negative and negative MTWA. For each MTWA category, we calculated the probability of the outcome given a positive test result (positive predictive value) and the probability of the absence of the outcome given a negative test result (negative predictive value). Given the variability in disease prevalence and duration across studies and the effect of these variables on predictive values, we decided that only the ratios comparing predictive values between categories (i.e., the relative risk) could reasonably be pooled across studies [16].
We carried out separate meta-analyses comparing each pair of MTWA categories in terms of risk ratios for each endpoint. We used a Bayesian hierarchical model with non-informative prior distributions to estimate the overall risk ratios using the WinBUGS software package [17]. We reported the posterior median and 95% credible intervals (CrI) for the parameters of interest. All plots were made using the R software package.
We also carried out two sensitivity analyses. In the first, we examined the effect of follow-up time by restricting our analysis to studies with between 1 and 2 years of follow-up. In the second, we excluded studies that included ICD shocks as part of their composite endpoint.
Results
Study and Participant Characteristics
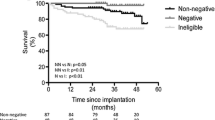
No randomized controlled trials examining MTWA in primary prevention were identified. We identified 8 prospective cohort studies involving a total of 1,946 participants (Figure 1) [6, 18–24]. All studies were identified in MEDLINE, although some were also found in other databases.
The characteristics of included studies are presented in Table 1. The underlying cardiac pathology varied between studies but the age and sex distributions were relatively similar. Studies also varied in sample size and duration of follow-up. Four studies were classified as being of good quality [6, 18, 19, 22], and 4 were of moderate quality [20, 21, 23, 24].
Differences existed in the categorization schemes of MTWA test results and in the percentage of patients in the different MTWA categories (Table 2). Of the 1,946 patients, 332 had a positive MTWA test, 656 had a negative test, 84 had an indeterminate test, and 874 were classified as non-negative. Three studies excluded indeterminate patients, preventing the calculation of valid measures of sensitivity, specificity, and positive and negative predictive values. In the remaining 5 studies, MTWA sensitivity and negative predictive values were high (Table 2). However, MTWA specificity and positive predictive values were relatively modest.
Results of the Meta-Analyses
In our primary analysis of the composite endpoint of mortality and severe arrhythmia, we pooled data across studies to investigate the predictive ability of MTWA (Figures 2 and 3). Different numbers of studies were used in each meta-analysis, reflecting the variability in reporting of outcomes as a function of MTWA categories. The risk of mortality or severe arrhythmic events with positive MTWA was increased compared to negative test results (RR = 2.7, 95%CrI = 1.4, 6.1) (Figure 2). Similar results were obtained when comparing non-negative to negative MTWA (RR = 2.6, 95%CrI = 1.4, 5.8) (Figure 3). There were insufficient data to make any statements regarding the predictive utility of the indeterminate group (positive vs indeterminate: RR = 1.1, 95%CrI = 0.4, 3.9; indeterminate vs negative: 2.5, 95%CrI = 0.8, 5.4). In secondary analyses, we examined MTWA as a predictor of mortality. However, with only 3 studies [18, 21, 24] reporting all-cause mortality, cardiac death, or arrhythmic death, this analysis provided inconclusive results (positive vs negative: RR = 1.94, 95%CrI = 0.6, 10.3; non-negative vs negative: RR = 1.94, 95%CrI = 0.4, 11.8).
We also conducted two sensitivity analyses. In the first, we restricted our analysis to the 7 studies that had follow-up durations between 1 and 2 years. In this analysis, we found that patients with a non-negative MTWA had three-times the risk of experiencing an arrhythmic event or death in the 1–2 years following MTWA testing than patients with a negative MTWA result (RR = 3.1; 95%CrI = 1.3, 9.5). These results are consistent with those obtained in our primary analysis. In the second, we excluded the study by Bloomfield and colleagues [6], which included ICD shocks as part of their composite endpoint. The inclusion of this trial appears to have had a minimal effect on our estimates (non-negative vs negative without Bloomfield: RR = 2.2, 95% CI = 1.2, 5.5).
Discussion
This systematic review and meta-analysis examined MTWA as a predictor of mortality and severe arrhythmic events for primary prevention in patients with left-ventricular dysfunction. We were unable to identify any randomized trials investigating this diagnostic modality. Consequently, our conclusions are based on less rigorous cohort studies, which are further weakened by a lack of standardization. Nevertheless, a positive MTWA test result cumulatively predicted an increased risk of mortality and severe arrhythmic events compared with a negative test. MTWA may therefore possess some clinical utility as a stratification tool to assess short- to moderate-term risk in high-risk primary prevention populations. This is important as the majority of the economic burden associated with the prevention of arrhythmic events by ICD implantation occurs in this population [25, 26]. However, the wide credible interval suggests the clinical utility may range from very modest to substantial and highlights the need for additional high-quality studies to better refine these estimates. Furthermore, our review identified a dearth of data examining the utility of MTWA for long-term risk stratification; only 1 study to date has examined the ability of MTWA to predict events after 2 years of follow-up.
MTWA as a predictor of cardiac events has been examined in several non-systematic, narrative reviews [7, 8, 27–31] and one systematic review. This systematic review included a meta-analysis and also concluded that MTWA predicted an increased risk of mortality and arrhythmic events [32]. Compared to the previous meta-analysis [32], which included more heterogeneous studies, we have avoided duplicate publications, added several more recent publications, and included only patient populations with significant left ventricular dysfunction. Our study is therefore more homogenous and specifically addresses the utility of MTWA in high-risk primary prevention. In addition, we have concentrated on comparing ratios of predictive values and avoided summarizing predictive values as these results are heavily dependent on study disease prevalence and follow-up time. Despite these important differences, the results of this previous study [32] are generally consistent with those of the present meta-analysis.
The utility of MTWA for predicting severe arrhythmic events in patients with left ventricular dysfunction also has been examined in 3 trials that have been recently presented at scientific meetings but not included in this meta-analysis. In the MASTER-I trial, which was presented at the Late Breaking Clinical Trial Session of the American Heart Association 2007 Scientific Sessions, 575 post-MI patients with left ventricular ejection fractions ≤ 30% and no history of severe arrhythmic events from 50 U.S. hospitals were followed for at least 2 years [33]. All patients received an ICD. The primary endpoint of the MASTER I trial was life-threatening ventricular tachyarrhythmic event, defined as either arrhythmic death or appropriate ICD discharge, and the secondary endpoints were total and cause-specific mortality. Non-negative MTWA did not appear to predict life-threatening ventricular tachyarrhythmias (hazard ratio (HR): 1.26, 95% confidence interval (CI): 0.76, 2.09), although with a wide 95% CI, we are unable to rule out a clinical difference of the same magnitude as that reported in the current meta-analysis. The MASTER I investigators did find an increase in all-cause mortality among patients with non-negative MTWA (HR: 2.04, 95%CI: 1.10, 3.78). In the MASTER II trial, the utility of MTWA was examined in 303 patients with moderate ventricular dysfunction (i.e., left ventricular ejection fraction between 31% and 40%), 48% of whom received an ICD [34]. The MASTER II trial, which excluded patients with indeterminate test results, provided inconclusive results due to a lower event rate than expected (positive MTWA vs negative MTWA: unadjusted stratified HR: 1.22, 95% CI: 0.34, 4.39; adjusted stratified HR: 1.20, 95% CI = 0.33, 4.31). In the ABCD trial, Costantini and colleagues examined the utility of MTWA and electrophysiological testing to predict different arrhythmic outcomes [35]. This study involved 566 patients with ischemic cardiomyopathy, an ejection fraction < 40%, and documented non-sustained VT, and patients were followed for 2 years. The investigators found that, at 1 year, non-negative MTWA was an important predictor of polymorphic VT, VF, and SCD (2.7% vs 0%, p = 0.04) but not of monomorphic VT (data not provided). At 2 years, non-negative MTWA was not associated with either outcome.
Although these studies provide important information regarding the utility of MTWA, we have not included them in our meta-analysis for a number of reasons. First, they have not yet undergone the rigorous peer-review associated with publication of a full manuscript. Second, in the MASTER-I trial, all patients received an ICD regardless of MTWA test. This trial therefore examines an inherently different question than the one posed in our meta-analysis. Finally, only limited information is available for each study, rending it difficult to assess the eligibility of each study relative to the inclusion/exclusion criteria of our meta-analysis. This limited information available also prevents the inclusion of these data in the analyses, particularly in the case of the ABCD trial. Despite these limitations, it is unlikely that the inclusion of these results would alter the conclusions drawn in the present study, particularly given the consistency of the point estimates obtained in these studies with our results.
Our study has a number of strengths. This is the first systematic review and meta-analysis that focuses on the use of MTWA in the setting of primary prevention in patients with left-ventricular dysfunction. By excluding studies of healthy individuals, we provide a more valid measure of MTWA specificity and negative predictive value as it pertains to clinical practice. Second, our meta-analysis included patients with indeterminate test results, avoiding a potentially important selection bias. Third, our systematic review and meta-analysis was conducted using a pre-specified protocol and in accordance with the MOOSE criteria [14]. Finally, this is the first meta-analysis to compare the different MTWA categories (i.e., positive vs negative, positive vs indeterminate, negative vs indeterminate), rather than simply grouping test results as negative and non-negative. Furthermore, our comparison of negative and non-negative MTWA was restricted to studies that reported indeterminate tests results, resulting in a more valid estimate of the effect of MTWA.
Our meta-analysis also has some potential limitations. First, we restricted our search to full-text studies published in English and thus may be affected by language and/or publication bias. Although our decision to not include studies recently published as abstracts may affect the precision of our estimates, it is unlikely to bias our results. These 3 studies have not been published because they are recently completed; the publication status is not due to the positive or negative nature of their results. Second, despite recommendations from the manufacturer strongly encouraging retesting following an indeterminate result [36], none of the studies identified in our systematic review conducted retesting. Retesting could decrease the number of patients with indeterminate test results and could potentially alter the sensitivity and specificity of MTWA. Thus, we may possibly be underestimating the potential benefits of MTWA testing. Third, there was some heterogeneity present in the individual studies included in our systematic review and meta-analysis. Studies varied in patient characteristics, duration of follow-up, study endpoints, and distribution of MTWA categories. Heterogeneity was also present in test classification, with some studies grouping patients into 3 categories (positive, negative, and indeterminate), some grouping patients into negative and non-negative, and the remaining studies excluding indeterminate tests. However, our results, although inconclusive due to wide CrIs that include both no effect and clinical important differences, suggest that there is no difference in risk of mortality or severe arrhythmic events between patients with positive MTWA and those with indeterminate results. Consequently, grouping patients as negative and non-negative is likely a valid approach. Fourth, some studies excluded indeterminate tests when calculating sensitivities and specificities. Where possible, we re-calculated the sensitivity, specificity, and positive and negative predictive values comparing non-negative and negative MTWA. However, we were unable to re-calculate these test characteristics for all studies. We also examined MTWA using the ratio of positive predictive values, which is not affected by the underlying disease prevalence. Fifth, we were limited to aggregate data and thus were unable to compare the predictive ability of MTWA to those of other tests, including New York Heart Association Class and left ventricular ejection fraction. Sixth, the ability of MTWA to predict events occurring 2 or more years after testing remains unclear. Finally, all studies included in our meta-analysis were observational studies. The potential effects of selection bias and confounding must be considered when interpreting their results.
Conclusion
Although the body of evidence is far from ideal, MTWA appears to predict mortality and severe arrhythmias occurring within one to two years in patients with left-ventricular dysfunction and no previous history of ventricular arrhythmias. Patients with positive or indeterminate tests are at higher risk of mortality and severe arrhythmic events than patients with negative MTWA, potentially aiding the identification of patients most likely to benefit from prophylactic ICD implantation and thereby perhaps improving the cost-effectiveness of this therapy. There remains a need to examine MTWA in well-conducted randomized controlled trials as well as the ability of MTWA to predict long-term outcomes. While awaiting further quality studies, physicians and policy makers may wish to consider MTWA to help identify patients in the greatest need of aggressive primary prevention and ICD implantation.
References
Connolly SJ, Hallstrom AP, Cappato R, Schron EB, Kuck KH, Zipes DP, et al: Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg. Canadian Implantable Defibrillator Study. Eur Heart J. 2000, 21 (24): 2071-2078. 10.1053/euhj.2000.2476.
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al: Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002, 346 (12): 877-883. 10.1056/NEJMoa013474.
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al: Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005, 352 (3): 225-237. 10.1056/NEJMoa043399.
Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al: ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006, 48 (5): e247-e346. 10.1016/j.jacc.2006.07.010.
Al-Khatib SM, Anstrom KJ, Eisenstein EL, Peterson ED, Jollis JG, Mark DB, et al: Clinical and economic implications of the Multicenter Automatic Defibrillator Implantation Trial-II. Ann Intern Med. 2005, 142 (8): 593-600.
Bloomfield DM, Bigger JT, Steinman RC, Namerow PB, Parides MK, Curtis AB, et al: Microvolt T-wave alternans and the risk of death or sustained ventricular arrhythmias in patients with left ventricular dysfunction. J Am Coll Cardiol. 2006, 47 (2): 456-463. 10.1016/j.jacc.2005.11.026.
Cohen RJ: Enhancing specificity without sacrificing sensitivity: potential benefits of using microvolt T-wave alternans testing to risk stratify the MADIT-II population. Card Electrophysiol Rev. 2003, 7 (4): 438-442. 10.1023/B:CEPR.0000023161.35685.68.
Klingenheben T, Ptaszynski P: Clinical significance of microvolt T-wave alternans. Herzschrittmacherther Elektrophysiol. 2007, 18 (1): 39-44. 10.1007/s00399-007-0553-1.
Myles RC, Jackson CE, Tsorlalis I, Petrie MC, McMurray JJ, Cobbe SM: Is microvolt T-wave alternans the answer to risk stratification in heart failure?. Circulation. 2007, 116 (25): 2984-2991. 10.1161/CIRCULATIONAHA.107.699918.
Verrier RL, Kumar K, Josephson ME: The frustrating search for arrhythmia risk stratifiers in heart failure due to nonischemic cardiomyopathy: does T-wave alternans testing help?. J Am Coll Cardiol. 2007, 50 (19): 1905-1906. 10.1016/j.jacc.2007.09.005.
Cantillon DJ, Stein KM, Markowitz SM, Mittal S, Shah BK, Morin DP, et al: Predictive value of microvolt T-wave alternans in patients with left ventricular dysfunction. J Am Coll Cardiol. 2007, 50 (2): 166-173. 10.1016/j.jacc.2007.02.069.
Klingenheben T, Hohnloser SH: Clinical value of T-wave alternans assessment. Card Electrophysiol Rev. 2002, 6 (3): 323-328. 10.1023/A:1016305831211.
Rosenbaum DS, Jackson LE, Smith JM, Garan H, Ruskin JN, Cohen RJ: Electrical alternans and vulnerability to ventricular arrhythmias. N Engl J Med. 1994, 330 (4): 235-241. 10.1056/NEJM199401273300402.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al: Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000, 283 (15): 2008-2012. 10.1001/jama.283.15.2008.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J: The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003, 3: 25-10.1186/1471-2288-3-25.
Dendukuri N, Chiu K, Brophy JM: Validity of electron beam computed tomography for coronary artery disease: asystematic review and meta-analysis. BMC Med. 2007, 5: 35-10.1186/1741-7015-5-35.
Warn DE, Thompson SG, Spiegelhalter DJ: Bayesian random effects meta-analysis of trials with binary outcomes: methods for the absolute risk difference and relative risk scales. Stat Med. 2002, 21 (11): 1601-1623. 10.1002/sim.1189.
Chow T, Kereiakes DJ, Bartone C, Booth T, Schloss EJ, Waller T, et al: Prognostic utility of microvolt T-wave alternans in risk stratification of patients with ischemic cardiomyopathy. J Am Coll Cardiol. 2006, 47 (9): 1820-1827. 10.1016/j.jacc.2005.11.079.
Grimm W, Christ M, Bach J, Muller HH, Maisch B: Noninvasive arrhythmia risk stratification in idiopathic dilated cardiomyopathy: results of the Marburg Cardiomyopathy Study. Circulation. 2003, 108 (23): 2883-2891. 10.1161/01.CIR.0000100721.52503.85.
Ikeda T, Sakata T, Takami M, Kondo N, Tezuka N, Nakae T, et al: Combined assessment of T-wave alternans and late potentials used to predict arrhythmic events after myocardial infarction. A prospective study. J Am Coll Cardiol. 2000, 35 (3): 722-730. 10.1016/S0735-1097(99)00590-2.
Kitamura H, Ohnishi Y, Okajima K, Ishida A, Galeano E, Adachi K, et al: Onset heart rate of microvolt-level T-wave alternans provides clinical and prognostic value in nonischemic dilated cardiomyopathy. J Am Coll Cardiol. 2002, 39 (2): 295-300. 10.1016/S0735-1097(01)01718-1.
Klingenheben T, Zabel M, D'Agostino RB, Cohen RJ, Hohnloser SH: Predictive value of T-wave alternans for arrhythmic events in patients with congestive heart failure. Lancet. 2000, 356 (9230): 651-652. 10.1016/S0140-6736(00)02609-X.
Sakabe K, Ikeda T, Sakata T, Kawase A, Kumagai K, Tezuka N, et al: Comparison of T-wave alternans and QT interval dispersion to predict ventricular tachyarrhythmia in patients with dilated cardiomyopathy and without antiarrhythmic drugs: a prospective study. Jpn Heart J. 2001, 42 (4): 451-457. 10.1536/jhj.42.451.
Sarzi BS, Vaninetti R, Laporta A, Picozzi A, Pedretti RF: T wave alternans is a predictor of death in patients with congestive heart failure. Int J Cardiol. 2004, 93 (1): 31-38. 10.1016/S0167-5273(03)00119-0.
Hreybe H, Bedi M, Ezzeddine R, Barrington W, Jain S, Ngwu O, et al: Indications for internal cardioverter defibrillator implantation predict time to first shock and the modulating effect of beta-blockers. Am Heart J. 2005, 150 (5): 1064-10.1016/j.ahj.2005.07.019.
Wilkoff BL, Hess M, Young J, Abraham WT: Differences in tachyarrhythmia detection and implantable cardioverter defibrillator therapy by primary or secondary prevention indication in cardiac resynchronization therapy patients. J Cardiovasc Electrophysiol. 2004, 15 (9): 1002-1009. 10.1046/j.1540-8167.2004.03625.x.
Armoundas AA, Cohen RJ: Clinical utility of T-wave alternans. Card Electrophysiol Rev. 1997, 1 (3): 390-394. 10.1023/A:1009902030340.
Armoundas AA, Tomaselli GF, Esperer HD: Pathophysiological basis and clinical application of T-wave alternans. J Am Coll Cardiol. 2002, 40 (2): 207-217. 10.1016/S0735-1097(02)01960-5.
Armoundas AA, Hohnloser SH, Ikeda T, Cohen RJ: Can microvolt T-wave alternans testing reduce unnecessary defibrillator implantation?. Nat Clin Pract Cardiovasc Med. 2005, 2 (10): 522-528. 10.1038/ncpcardio0323.
Haghjoo M, Arya A, Sadr-Ameli MA: Value of microvolt T-wave alternans for predicting patients who would benefit from implantable cardioverter-defibrillator therapy. Cardiol Rev. 2006, 14 (4): 173-179. 10.1097/01.crd.0000184454.56306.d6.
Takagi M, Yoshikawa J: T wave alternans and ventricular tachyarrhythmia risk stratification: a review. Indian Pacing Electrophysiol J. 2003, 3 (2): 67-73.
Gehi AK, Stein RH, Metz LD, Gomes JA: Microvolt T-wave alternans for the risk stratification of ventricular tachyarrhythmic events: a meta-analysis. J Am Coll Cardiol. 2005, 46 (1): 75-82. 10.1016/j.jacc.2005.03.059.
Late-Breaking Clinical Trial News Release 12a. Date accessed: May 26, 2008, [http://scientificsessions.americanheart.org/portal/scientificsessions/ss/lbctnr12a.2007]
Chow T, Kereiakes DJ, Onufer J, Woelfel A, Gursoy S, Peterson BJ, et al: Prognostic value of microvolt T-wave alternans in patients with moderate ischemic left ventricular dysfunction: results from the MASTER II trial. J Am Coll Cardiol. 2008, 51 (10): A17-10.1016/j.jacc.2008.02.017.
Costantini O, Rosenbaum DS, Hohnloser SH, Kirk M, Lerman B, Baker J, et al: The alternans before cardioverter defibrillator (ABCD) trial: A noninvasive strategy for primary prevention of sudden cardiac death using T-wave alternans. Circulation. 2006, 114 (22): 2426-
Cambridge Heart: Microvolt T-Wave Alternans (MTWA). Date accessed: November 29, 2007, [http://www.cambridgeheart.com/content/Clinicians/MTWA_Indepth.shtml]
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2261/9/5/prepub
Acknowledgements
Mr. Filion, Dr. Dendukuri, and Dr. Brophy receive financial support from le Fonds de la Recherche en Santé du Québec. Ms. van der Avoort received financial support from the Foundation of the University of Nijmegen and from the Faculty of Medicine of the Radboud University Nijmegen Medical Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JMB conceived of the study idea, and CJA, KBF, and JMB contributed to the study design. CJA conducted the literature review. CJA and KBF performed the data extraction and drafted the manuscript. ND designed and conducted the statistical analyses. All authors were involved in revising the article for important intellectual content, interpreting the data, and approved the final version to be published.
Electronic supplementary material
12872_2008_226_MOESM1_ESM.pdf
Additional file 1: Quality assessment scale. This scale, based on QUADAS [15], was used to assess the quality of studies included in the meta-analysis. (PDF 56 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
van der Avoort, C.J., Filion, K.B., Dendukuri, N. et al. Microvolt T-wave alternans as a predictor of mortality and severe arrhythmias in patients with left-ventricular dysfunction: a systematic review and meta-analysis. BMC Cardiovasc Disord 9, 5 (2009). https://doi.org/10.1186/1471-2261-9-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2261-9-5