Abstract
Background
The National Cardiovascular Disease (NCVD) Database Registry represents one of the first prospective, multi-center registries to treat and prevent coronary artery disease (CAD) in Malaysia. Since ethnicity is an important consideration in the occurrence of acute coronary syndrome (ACS) globally, therefore, we aimed to identify the role of ethnicity in the occurrence of ACS among high-risk groups in the Malaysian population.
Methods
The NCVD involves more than 15 Ministry of Health (MOH) hospitals nationwide, universities and the National Heart Institute and enrolls patients presenting with ACS [ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI) and unstable angina (UA)]. We analyzed ethnic differences across socio-demographic characteristics, hospital medications and invasive therapeutic procedures, treatment of STEMI and in-hospital clinical outcomes.
Results
We enrolled 13,591 patients. The distribution of the NCVD population was as follows: 49.0% Malays, 22.5% Chinese, 23.1% Indians and 5.3% Others (representing other indigenous groups and non-Malaysian nationals). The mean age (SD) of ACS patients at presentation was 59.1 (12.0) years. More than 70% were males. A higher proportion of patients within each ethnic group had more than two coronary risk factors. Malays had higher body mass index (BMI). Chinese had highest rate of hypertension and hyperlipidemia. Indians had higher rate of diabetes mellitus (DM) and family history of premature CAD. Overall, more patients had STEMI than NSTEMI or UA among all ethnic groups. The use of aspirin was more than 94% among all ethnic groups. Utilization rates for elective and emergency percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) were low among all ethnic groups. In STEMI, fibrinolysis (streptokinase) appeared to be the dominant treatment options (>70%) for all ethnic groups. In-hospital mortality rates for STEMI across ethnicity ranges from 8.1% to 10.1% (p = 0.35). Among NSTEMI/UA patients, the rate of in-hospital mortality ranges from 3.7% to 6.5% and Malays recorded the highest in-hospital mortality rate compared to other ethnic groups (p = 0.000). In binary multiple logistic regression analysis, differences across ethnicity in the age and sex-adjusted ORs for in-hospital mortality among STEMI patients was not significant; for NSTEMI/UA patients, Chinese [OR 0.71 (95% CI 0.55, 0.91)] and Indians [OR 0.57 (95% CI 0.43, 0.76)] showed significantly lower risk of in-hospital mortality compared to Malays (reference group).
Conclusions
Risk factor profiles and ACS stratum were significantly different across ethnicity. Despite disparities in risk factors, clinical presentation, medical treatment and invasive management, ethnic differences in the risk of in-hospital mortality was not significant among STEMI patients. However, Chinese and Indians showed significantly lower risk of in-hospital mortality compared to Malays among NSTEMI and UA patients.
Similar content being viewed by others
Background
Acute coronary syndrome (ACS) encompasses a spectrum of clinical entities, ranging from unstable angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI) to ST-elevation myocardial infarction (STEMI) [1]. In the Western world, ACS is the most common cause of death [2]. Cardiovascular disease (CVD) mortality is on the rise in the Asia Pacific countries (including Malaysia) that were undergoing rapid urbanization, industrialization and lifestyle changes [3]. According to the Global Burden of Disease Study (GBD), ischemic heart disease (IHD) is ranked first among the leading causes of mortality for eight regions in the world [4]. The World Health Organization (WHO) estimated that CAD will be the single largest cause of disease burden in many countries world-wide by the year 2020 [5]. Similarly, in Malaysia, CVD accounted for 147,843 admissions or about 6.91% of total admissions in Ministry of Health (MOH) hospitals in year 2009 [6]. CVD accounted for approximately 24.5% of death in government hospitals in year 2010 and is the leading cause of death in Malaysia [7].
Established coronary risk factors such as cigarette smoking, diabetes mellitus (DM), hypertension, obesity, sedentary life style and dyslipidemias still play major roles in CAD [8]. While conventional cardiovascular risk factors such as smoking, blood pressure and total cholesterol predict risk within these ethnic groups, they do not fully account for the differences in risk between ethnic groups, suggesting that alternative explanations might exist [9]. Epidemiological evidence that includes cross-sectional studies, coronary angiographic studies, and registry data showed significant differences between ethnic groups who were diagnosed with ACS in terms of presentations, risk factors, coronary vessel diameters, prognoses and outcomes [10–14].
With CVD accounting for most deaths globally, eliminating ethnic disparities in cardiac care has become a new challenge in the practice of cardiology [15]. Studies have shown that CVDs present differently in between ethnic groups [16, 17]. Ethnicity has been shown to be an independent predictor of adverse cardiovascular outcomes in patients with atherothrombotic disease [18] and CAD [19].
ACS registries are important tools for analyzing disease management [20, 21]. Exploration of registries data may lead to changes in disease management strategies and the national health care policies [22]. The National Cardiovascular Disease (NCVD) Database Registry is one of the pioneer projects to treat and prevent CAD in Malaysia. The project is a joint effort of doctors and nurses in public, private and academic medical institutions supported by the National Heart Association, National Heart Foundation, Clinical Research Centre and the MOH, Malaysia [23].
The aim of this study is, therefore, to identify the role of ethnicity in relation to the occurrence of ACS among high-risk groups in the Malaysian population using the Malaysian NCVD.
Methods
A detailed description of NCVD has been reported elsewhere [23, 24]. In brief, the NCVD for ACS is the first prospective, multi-center registry involving more than 15 MOH hospitals nationwide, universities and the National Heart Institute (IJN: Institut Jantung Negara). Since its establishment in 2006, all registry centers attempt to ensure the enrollment of an unbiased population. The NCVD is an observational prospective registry that collects data on ‘real-life’ ACS patients comprising STEMI, NSTEMI and UA according to demographic, epidemiological, management and outcome characteristics. The registry enrolls inpatients presented with ACS from January 2006 onwards and is still on-going at the time of writing.
Entry criteria of ACS include risk stratum of patients presenting with clinical features consistent with an ACS (chest pain or overwhelming shortness of breath) and defined by accompanying clinical, electrocardiographic and biochemical features. The final diagnosis of ACS was made by the attending physician using the following criteria: STEMI was diagnosed on the basis of the presence of acute chest pain with new or presumably new ST segment elevations more than 1 mm in two consecutive leads or the presence of a new left bundle branch block on the index or subsequent ECG with positive cardiac markers of necrosis [25]. NSTEMI was defined by ECG ST-segment depression or prominent T-wave inversion and/or positive biomarkers of necrosis in the absence of ST-segment elevation and in an appropriate clinical setting (chest discomfort or angina equivalent). UA was defined as angina pectoris (or equivalent type of ischemic discomfort) with any one of the three following features: a) angina occurring at rest and prolonged, usually more than 20 min; b) new-onset angina of at least Canadian Cardiovascular Society (CCS) classification III severity; c) recent acceleration of angina reflected by an increase in severity of at least one CCS class to at least CCS class III. The patient must also have normal cardiac biomarkers [26].
Demographic, significant risk factors or past medical history, anthropometric, ACS stratum, treatment, length of hospitalization, outcome (alive, dead) and complications (such as bleeding) data were obtained from the medical records and recorded on a standardized clinical research form by trained coordinators. Standardized definitions for all patient-related variables and clinical diagnoses were used [24]. Precise definition and quantification for risk factors, past medical history and ways of treatments were described in earlier publications [23, 24].
Collected data were subsequently entered into a web-based centralized database with security password encryption according to individual centers. Regular data checks were performed and queries were generated for correction to ensure accuracy. Ethnicity that includes Malays, Chinese, Indians (major ethnic groups), Indigenous (Orang Asli), Kadazan, Melanau, Murut, Bajau, Bidayuh, Iban (minor ethnic groups) and other Malaysians were recorded. Ethnicity was self-reported and coded as mutually exclusive categories. We excluded 17 patients with missing ethnic information. A total of 13,591 patients were included in the analysis. The current study included ACS patients from March 2006 to February 2010 over a period of 4 years. All patients were enrolled in Malaysia at different centers as listed in Figure 1.
Statistical analysis
Data were examined for normality distribution using the stem-and-leaf plot and Kolmogorov-Smirnov test. Descriptive statistics and baseline variables were presented as numbers and percentages, means and standard deviations, or medians and interquartile ranges. A chi square test was used to assess differences between categorical variables; a one-way ANOVA with post-hoc multiple comparisons (parametric analysis) or Kruskal-Wallis test (non-parametric analysis) was used to test differences across the four ethnic groups (Malays, Chinese, Indians, Others). For multivariate analysis, binary simple and multiple logistic regressions were used to model the dichotomous outcome of STEMI and NSTEMI/UA mortality among ethnic groups with adjustment for age and sex. We checked for significant interaction between age and sex and possible multicollinearity by examining the standard errors of the b coefficients. Any significant interaction should be included in the final model. Standard errors of the b coefficients that were less than 2 indicate the absence of multicollinearity. The results were reported as crude and adjusted odds ratio (OR) with 95% confidence interval for ethnicity. A p value of <0.05 was considered statistically significant. All statistical calculations were performed using the IBM SPSS Statistics 20.
Ethics approval
This NCVD study was approved by the Medical Review & Ethics Committee (MREC), MOH Malaysia in 2007 (Approval Code: NMRR-07-20-250). MREC waived informed consent for NCVD.
Results
Socio-demographic characteristics
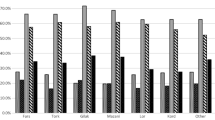
Socio-demographic characteristics and risk factors of the NCVD population are listed in Table 1. The distribution of the NCVD population was as follows: 49.0% Malays, 22.5% Chinese, 23.1% Indians, 5.3% Others (representing other indigenous groups and non-Malaysian nationals) and 0.1% missing data (Figure 2). The mean age of ACS patients at presentation was 59.1 (SD 12.0) years. More than 70% were males (p = 0.000). A large proportion of individuals within each ethnic group had more than two coronary risk factors including hypertension, DM and hyperlipidemia. Majority of patients were overweight [Body mass index (BMI) of more than 23 kg/m2] in accordance with the BMI for Asian populations [27]. Malays had the highest BMI (26.0 kg/m2) (p = 0.000). Indian had the biggest waist circumference (WC) (90.6 cm), the highest rate of DM (65.2%) and family history of premature CAD (22.2%) as compared to other ethnic groups (p = 0.000). Despite having the lowest BMI (24.8 kg/m2), Chinese had the highest rate of hypertension (76.1%) and dyslipidemia (51.8%) (p = 0.000). Others had the highest proportion of current or former smokers (65.7%) (p = 0.000).
Table 2 shows the ethnic distribution of ACS and clearly indicated that Others (58.3%) had significantly higher STEMI (p = 0.000). Overall, more patients had STEMI than NSTEMI or UA among all the ethnic groups.
Table 3 shows that Malays had significantly higher mean total cholesterol (TC) and low density lipoprotein cholesterol (LDL) (5.5 mmol/l, 3.5 mmol/l, respectively) (p = 0.000). Indians had significantly higher mean fasting blood glucose (FBG) (8.4 mmol/l) (p = 0.000). Troponin T level was higher among Chinese (1.6 ng/ml). The level of CK is significantly higher in Others (1242 unit/l) (p = 0.000).
Hospital medications
Medication use at the time of admission is listed in Table 4. Aspirin, adenosine diphosphate antagonist, β-blockers, angiotensin-converting enzyme inhibitors, and statins were commonly prescribed to all ACS patients. The use of antiplatelet therapies, such as aspirin, was similar among all ethnic groups; more than 94% of patients in each group were taking aspirin at baseline. Malays received significantly lower proportion of low molecular weight heparin (LMWH) than other ethnic groups (p = 0.000).
Invasive therapeutic procedures
Majority of patients in the registry were recorded in centers with on-site cardiac catheterization facilities and teaching hospitals (Figure 1). For ACS patients, utilization rates for elective and emergency percutaneous coronary intervention (PCI) (13.1-16.5%) and coronary artery bypass graft (CABG) (0.7-1.8%) were generally low among all ethnic groups (Table 5). The overall rates of invasive therapeutic procedures such as PCI and CABG were slightly different across the ethnic groups. Indians and Others (16.5%, 16.5%) were likely to receive PCI than Chinese and Malays (16.0%, 13.1%) (p = 0 · 000). CABG rate was slightly higher in Others (1.8%) compared to Malays (1.4%), Chinese (1.3%) and Indians (0.7%), respectively (p = 0.006). Left anterior descending (LAD) artery was the commonest culprit artery involved in ACS among all ethnic groups followed by right coronary artery (RCA) and left circumflex (LCX) artery. However, the difference across the ethnic groups was not significant (p = 0.359).
Treatment of STEMI
Table 6 shows the reperfusion strategy for STEMI including subgroup analysis for the fibrinolytic group, door-to-needle time and door-to-balloon time. Majority of STEMI patients (≥80%) received some form of reperfusion therapy either by primary PCI or fibrinolysis. Fibrinolysis appeared to be the dominant treatment options (≥70%) for all ethnic groups. Overall, significant higher proportion of Malays (78.1%) received reperfusion therapy either by primary PCI or fibrinolysis as compared with other ethnic groups (p = 0.000). Significant higher proportion of Chinese (9.0%) received primary PCI, at the same time, no reperfusion (21.5%) was higher in Chinese than other ethnic groups (P = 0.000).
In the subset analysis for fibrinolysis, a higher proportion of Malays (8.4%) managed to achieve less than 30 minutes of door-to-needle time compared to other ethnic groups (P = 0.000) as recommended by Clinical Practice Guidelines [25, 28]. Others reported higher door-to-needle time of 59 (IQR: 30–116) min compared to other ethnic groups (p = 0.013). On the other hand, in primary PCI, Others had the shortest door-to-balloon time of 81 (IQR: 48–124) min compared to other ethnic groups (p = 0.018). Overall, it is important to point out that we found a low percentage of patients achieving less than 30 minutes of door-to-needle time among all ethnic groups. Furthermore, door-to-needle and door-to-balloon time were longer than those recommended [25, 28].
In-hospital clinical outcomes
Indians reported significantly higher coronary care unit (CCU) days compared to Malays, Chinese and Others (3.6, 3.5, 3.2, and 2.5, respectively; p = 0.000) (Table 7). However, for total days, Malays reported significantly higher total days of admission compared to Others, Indians and Chinese (5.0, 4.9, 4.7, and 4.5, respectively; p = 0.000). Rates of major bleeding were low (≤ 0.7%) among all ethnic groups. There was no significant difference among the ethnic groups in the major or minor bleeding complication (p = 0.150) according to the Thrombolysis in Myocardial Infarction (TIMI) criteria for bleeding [29, 30].
In-hospital-mortality rate for STEMI was higher than NSTEMI and UA among all ethnic groups. STEMI mortality rate ranges from 8.1 to 10.1% which was statistically insignificant (p = 0.35) across all ethnic groups. In-hospital mortality was also not significantly different across ethnic groups in a risk adjusted multivariable model that controlled for age and sex.
For NSTEMI/UA, there was statistically significant higher in-hospital-mortality (p = 0.000) among Malays (6.5%) compared to Chinese (5.6%), Others (5.4%) and Indians (3.7%). These results were persisting after age and sex adjustment. Therefore, Malays remained a positive predictor for in-hospital mortality as compared to Chinese and Indians in the NSTEMI/UA group irrespective of age and sex.
Discussion
The study has shown important ethnic differences in the demographics, comorbid coronary risk factors, clinical presentation, baseline investigations, treatments and in-hospital outcomes.
Socio-demographics and coronary risk factors
Malaysia is a multiracial South East Asian country, consisting of 28.3 million people that include 67.4% Malays, 24.6% Chinese, 7.3% Indians, and 0.7% other ethnic groups [31]. However, the percentage of Indians (majority have their origins in Southern India) captured in this registry was 23.4% which indicates an over representation of the Indian population in the NCVD.
It seems that a relatively higher proportion of Indians was being captured in the NCVD Registry. However, the causal link between ethnicity and ACS is difficult to evaluate based on cross-sectional data as the NCVD Registry consists of a well-defined population diagnosed with ACS. Therefore, based on the NCVD Registry, one cannot possibly draw any conclusion as to the higher incidence of ACS among Indians compared to other ethnic groups. The finding of over-representation of Indians in the NCVD Registry was an interesting fact that serves as a basis for a prospective cohort study to reveal the association between ethnicity and ACS. Nevertheless, people of South Asian origin such as India, Pakistan, Bangladesh, Sri Lanka and Nepal represents one of the largest ethnic groups in the world and also one of the regions with the highest burden of CVDs [32]. Studies on South Asian migrants in Western countries such as Canada, United Kingdom (UK) and the United States of America (USA) documented significantly higher risks of CVDs with higher morbidity and mortality than other ethnic groups [10, 14, 33, 34]. Previous mortality statistics and cross-sectional surveys had confirmed that Indians have an increased risk of CAD compared to other ethnic groups [11, 35]. A cardiovascular cohort study showed that ethnicity plays a major role in CAD with Indian males found to have three times the risk of CAD as compared to Malays and Chinese in Singapore [36].
The mean age at presentation was 59.1 years among all ethnic groups. In contrast to earlier registries from developed countries, such as National Registry of Myocardial Infarction (NRMI) (mean age 68 years) [37], Global Registry of Acute Coronary Event (GRACE) registry (53% aged ≥ 65 years) [38, 39] and the Euro Heart Survey I (EHS-ACS-I) (mean age 63.4 years) [40, 41], our cohort was characterized by a younger age at presentation. The mean age was similar to the CREATE registry (58 years) [42] and Saudi Project for Assessment of Coronary Events (SPACE) registry (57 years) [43] that were conducted in India and Saudi Arabia, respectively. The age at presentation discrepancy observed between the European and Asian Registries should be investigated further to establish risk factors that possibly contributed toward the age difference.
Similar to ACS registries world-wide, the predominant sex was male (more than two thirds) among all ethnic groups. There were substantial differences between male and female in the presentation, diagnosis, management and outcome of CADs [44–47]. Most clinical trials have enrolled primarily men and the women have been under-represented in CAD clinical trials; further research involving larger female cohorts is required. Further, at participating centers, a lower proportion of women were found to have ischemia during the course of routine clinical care, and screening tests for ischemia were less predictive of CAD in women than those in men [48].
The patients’ risk factor profiles differed significantly among the ethnic groups. For example, Malays showed significantly highest mean BMI. Chinese patients had the highest proportion of hypertension and hyperlipidemia. On the other hand, Indians had the highest mean for WC and the highest proportion for DM and family history of premature CAD. Others had significantly highest proportion of smokers. The WC recorded among all ethnic groups was generally higher than the mean WC of Malaysians [49]. The finding of high WC among Indians was similar to those previously reported in the Malaysian National Health and Morbidity Survey III [49]. The finding of high prevalence of BMI among all ethnic groups with ACS was similar to another Malaysian prevalence study on overweight and obesity among non ACS population [50]. Higher BMI among Malays with ACS was also consistent with the national study on obesity among Malaysians according to ethnicity [51]. This explains the relationship between high BMI and higher occurrence of ACS in the general population [52]. The results suggest that a higher proportion of patients with ACS also have metabolic syndrome as compared to the general population [53, 54]. DM has been found to be more common in Indians. This finding was consistent with previous multi-center registries and studies in Singapore [55], Trinidad [35], Fiji [56], USA [57] and UK [33, 58]. A study in Canada by the Study of Health Assessment and Risk in Ethnic Groups (SHARE) investigators also found that Indians had more plasma glucose and lipid abnormalities compared to Europeans and Chinese [16]. Indians also have higher past history of CVDs and family history of MI compared to other ethnic groups [57]. Generally, our patients had high prevalence of coronary risk factors at presentation among all ethnic groups. These findings were similar to an earlier publication using NCVD [59], Singapore population [60], Iranian population [61], Saudi Arabia population [62], and in developing countries [63].
ACS
The proportion of STEMI among all ethnic groups (38.8–58.3%) was higher compared to earlier ACS registries in developed countries: GRACE (30.0%) [38], EHS-ACS-I (42.3%) [40], NRMI (40.0%) [64], Euro Heart Survey II (EHS-ACS-II) (34.5%) [65] and Canadian Acute Coronary Syndrome Registry (27.7%) [66]. Higher proportion of STEMI compared to NSTEMI and UA in NCVD was similar to those in the CREATE registry (47.3–71.4%) [42]. In the CREATE registry, poorer socio-economic group of patients recorded a higher proportion of STEMI in India. This finding could possibly explain why Others (indigenous ethnic groups), who generally belong to the lower socioeconomic status, recorded a higher proportion of STEMI.
Lipid profile, fasting blood glucose
Our findings on serum lipid were consistent with previous studies on Indian populations living in UK and USA. Generally, Indians have lower HDL cholesterol than whites or Afro-Caribbean populations but do not have higher total or LDL cholesterol than other races [67–69].
Hospital medications
Results indicated high use of Aspirin, Beta-blockers, LMWH and Statins among all ethnic groups was in line with the Clinical Practice Guidelines [26, 28, 70] and comparable to those in developed countries. Religious practice could be a factor to explain the lower use of LMWH (containing porcine-related material) among Malays as the overwhelming majorities are Muslims compared to other ethnic groups.
Invasive therapeutic procedures and culprit artery
On invasive therapeutic procedures, the rate of PCI and CABG in our registry was lower than those reported in developed countries [38, 40, 65, 66]. Our results showed disparities existed in the use of medications, PCI and CABG among ethnic groups. The finding of LAD artery as the most common culprit artery was similar to those of Yadav et al. [71] and Deshpandey and Dixit [72].
Treatment of STEMI
In STEMI, timely delivery of reperfusion therapy can reduce mortality; therefore, guidelines recommend fibrinolysis within 30 min (door-to-needle time) and primary PCI within 90 minutes (door-to-balloon-time) [25, 28]. Primary PCI has been proven better than fibrinolysis in treating STEMI [73, 74] and timely administration of fibrinolytic therapy significantly reduces mortality [75]. In STEMI, despite majority of patients who received reperfusion therapy, the rate of primary PCI was lower and the use of fibrinolytics was higher among all ethnic groups as compared to ACS registries in developed countries such as GRACE [38], EHS-ACS-I [40] and EHS-ACS-II [65]. In the fibrinolysis subgroup, door-to-needle time among all ethnic groups was longer than those recommended by the American and European Guidelines [25, 28] and the proportion of patients achieving less than 30 minutes of door-to-needle time was low. This is one of the main concerns of our study that illustrated suboptimal care in treating STEMI. Streptokinase, the less-fibrin specific (less effective) fibrinolytic agent as compared with fibrin-selective fibrinolytic agents [76] was commonly used among all ethnic groups. Higher proportion of Chinese received less reperfusion therapy than other ethnic groups; however, the reasons for these discrepancies were unclear.
In the implementation of evidence-based reperfusion strategies, doctors have to make the best decision to allocate limited resources to patients who are at highest risk and hope to obtain the largest benefit. Many studies have found differences in the delivery of cardiac care and reperfusion procedure among different ethnic groups in ACS [77–79]. Earlier studies of ethnic variation in the treatment and outcome of ACS in USA showed that non-whites had longer door-to-needle time in the treatment of AMI [80] and were less likely to undergo invasive cardiac procedures [81, 82]. However, this finding was controversial in other clinical trials [83]. Research has shown that by implementing a national quality improvement program, it is possible to reduce or eliminate the differences in care by ethnicity [84]. Considerably more effort and resources will be granted to improve the reperfusion strategies in developing countries like Malaysia for all patients regardless of their ethnic origin. Adherence to clinical practice guidelines has shown to improve quality of care and associated with significant reduction in in-hospital mortality rates [85].
In-hospital clinical outcomes
In developed countries, STEMI mortality rates were reported as 4.3–4.4% in NRMI [86], 7.0% in the GRACE Registry [38], 7.0% in the EHS-ACS-I [40] and 2.4% in the Canadian Acute Coronary Syndrome Registry [66]. In the NCVD, higher STEMI mortality rate (8.1–10.1%) in comparison with developed countries could be explained by lower use of primary PCI, higher use of less effective fibrinolytic agent (Streptokinase) and delay in door-to-needle time among all ethnic groups. In addition, LAD artery involvement as the main culprit vessel (>56%) among all ethnic groups could have contributed towards a less favorable outcome as reported earlier by Thanavaro et al. [87].
Interestingly, despite the fact that disparities exist in risk factors, clinical presentation, medical treatments and invasive management, there was no statistically significant difference in STEMI mortality among all ethnic groups. However, there are limitations in the analysis of mortality outcome comparing different ethnic groups and we advise caution in its interpretation. Firstly, it was an in-hospital mortality of STEMI and NSTEMI/UA of both genders and all age groups. As for ACS, many studies had shown higher mortality in women [88, 89] and older patients [39, 41, 90]. Hence, the mortality outcome analyzed in this method may have over or underestimated the differences between age groups and across genders. Secondly, we used in-hospital all-cause mortality as an end point in order to minimize event misclassification. Results for cardiac-specific mortality may be different for present results. Caution should, therefore, be observed in comparing results with those from other national registries or clinical trials.
On the basis of the risk factor profiles across all ethnic groups, it would seem unreasonable for Malays to have higher NSTEMI and UA mortality. It would seem that higher mortality in Malays can be partly explained by the higher proportion of Malays receiving lower rates of PCI compared to other ethnic groups. Other possible explanations include greater cigarette consumption and higher BMI among Malays.
Earlier observational studies locally and elsewhere have shown a higher proportion of deaths in Indians with IHD compared to other ethnic groups [11, 35, 91]. The finding of lower in-hospital mortality in NSTEMI/UA among Indians in our study contradicted with previous studies for unexplained reasons.
There were evidences that bleeding risk in ACS differs in different type of ACS, reperfusion therapy and ethnic groups [92]. Registry data [92], prospective study [93] and randomized controlled trials (RCT) [94] of developed countries in ACS patients reported that the major bleeding risk was between 4.6–10.9%. Compared to developed countries, major bleeding in NCVD was generally low among all ethnic groups (0.2–0.7%) and this finding was similar to those in the ACS Registry in India (0.2–0.3%) (CREATE) and Middle Eastern countries (0.83%) [95]. The finding of a lower risk of major bleeding is intriguing and possibly could be explained by the lower use of invasive cardiac procedures among all ethnic groups as compared to those in developed countries.
Strengths and limitations
The main strength of this study is the collection of data from multi centers to represent a complete and unselected group of patients in a real-world setting. Unlike restricted populations recruited in RCTs which tend to exclude high risk patients, the NCVD collects data on the full spectrum of ACS patients from a nationwide perspective. We gain insight into ACS patients that were not included in RCTs. We use a standard method across all ethnic groups in collecting data to avoid bias.
Several limitations of our study should be noted. Firstly, misclassification of ethnicity can occur as ethnicity was self-reported and mutually-exclusive. Secondly, the possibility of selection bias despite our attempt to include hospitals in different regions of the country. Many private hospitals with significant number of ACS admissions possibly with a different ethnic distribution did not participate in this registry. Ethnic minorities living in remote areas had difficulty accessing the health facilities and therefore could have been under-represented in this study. Thirdly, there may have been underreporting of risk factors such as cigarette smoking and past medical history as these measures were self-reported and this may subject to bias.
Furthermore, statistical differences are frequently observed in a large number of subjects but may not be clinically meaningful. In studies with large patient enrolment, small differences between groups will be highly significant by conventional use of the p values, and the clinical importance of these differences can only be judged with clinical insight.
Conclusions
There are two major implications of our study. First, we have shown interesting facts about the differences and similarities of demographic, risk profile, ACS stratum, treatment and outcome among different ethnic groups. Second, our study establishes a critical understanding of disease spectrum, drug usage, invasive procedures, clinical outcomes, and the overall quality of care provided to ACS patients in Malaysia. In addition, the NCVD provides insights and forms the basis for clinical investigators to design future clinical trials. The NCVD also enables clinicians and health care administrators to compare disease-specific patterns, management and outcomes which might lead to changes in national health priorities or strategies of disease management.
Abbreviations
- ACS:
-
Acute coronary syndrome
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass graft
- CCU:
-
Coronary care unit
- CREATE:
-
Treatment and outcomes of ACS in India
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- GRACE:
-
Global Registry of Acute Coronary Events
- IHD:
-
Ischemic heart disease
- LAD:
-
Left anterior descending
- LCX:
-
Left circumflex
- LM:
-
Left main
- LMWH:
-
Low molecular weight heparin
- LVEF:
-
Left ventricular ejection fraction
- MOH:
-
Ministry of Health
- NCVD:
-
National Cardiovascular Disease Database Registry
- NRMI:
-
National Registry of Myocardial Infarction
- NSTEMI:
-
Non ST-segment elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- RCA:
-
Right coronary artery
- RCT:
-
Randomized controlled trial
- SPACE:
-
Saudi Project for Assessment of Coronary Events
- STEMI:
-
ST-elevation myocardial infarction
- UA:
-
Unstable angina
- WHO:
-
World Health Organization
- TIMI:
-
Thrombolysis in myocardial infarction
- WC:
-
Waist circumference.
References
Herzog E, Saint-Jacques H, Rozanki A: The pain pathway as a tool to bridge the gap between evidence and management of acute coronary syndrome. Critic Path in Cardiology. 2004, 3: 20-24. 10.1097/01.hpc.0000116583.24833.ce.
Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Donald L-J, Mary MD, James M, Claudia M, Nichol G, Donnell CO, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y: Heart Disease and Stroke Statistics 2008 Update. A report from the American Heart Association statistics committee and Stroke Statistics subcommittee. Circulation. 2008, 117: 25-146.
Khor GL: Cardiovascular epidemiology in the Asia-Pacific region. Asia Pac J Clin Nutr. 2001, 10 (2): 76-80. 10.1046/j.1440-6047.2001.00230.x.
Murray CJ, Lopez AD: Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997, 349: 1269-1276. 10.1016/S0140-6736(96)07493-4.
WHO: The World Health Statistic. 2012, [http://www.who.int/gho/publications/world_health_statistics/EN_WHS2012_Full.pdf] (Accessed 15 August 2013)
Ministry of Health, Malaysia: Annual Report. 2009, [http://www.moh.gov.my/images/gallery/publications/md/ar/2009-2.pdf] (Accessed 15 August 2013)
Health Informatics Centre, Planning and Development Division, Ministry of Health Malaysia, July 2010: Number of discharges and deaths in government hospitals. [http://www.moh.gov.my/images/gallery/stats/heal_fact/health_facts_2010.pdf] (Accessed 15 August 2013)
Kuulasmaa K, Tunstall-Pedoe H, Dobson A, et al: Estimation of contribution of changes in classic risk factors to trends in coronary event rates across the WHO MONICA project populations. Lancet. 2000, 355: 675-687. 10.1016/S0140-6736(99)11180-2.
Forouhi NG, Sattar N: CVD risk factors and ethnicity-A homogeneous relationship?. Atherosclerosis Suppl. 2006, S7 (1): 11-19.
Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KGMM, Harland J, Patel S, Ahmad N, Turner C: Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999, 319 (24): 215-220.
Hughes K, Yeo PPB, Lun KC, Thai AC, Sothy SP, Wang KW, Cheah JS, Phoon WO, Lim P: Cardiovascular diseases in Chinese, Malays, and Indians in Singapore. I. Differences in mortality. J Epid and Comm Hlth. 1990, 44: 24-28. 10.1136/jech.44.1.24.
Mak KH, Chia KS, Kark JD, Chua T, Tan C, Foong BH, Lim YL, Chew SK, et al: Ethnic differences in acute myocardial infarction in Singapore. Eur Heart J. 2003, 24: 151-160.
Makaryus AN, Dhama B, Raince J, Raince A, Garyali S, Labana SS, Kaplan BM, Park C, Jauhar R: Coronary artery diameter as a risk factor for acute coronary syndromes in Asian-Indians. Am J Cardiol. 2005, 96: 778-780. 10.1016/j.amjcard.2005.05.018.
Nijjar APK, Wang H, Quan H, Khan NA: Ethnic and sex differences in the incidence of hospitalized acute myocardial infarction: British Columbia, Canada 1995–2002. BMC Cardio Dis. 2010, 10 (38): 1471-2261.
Peterson E, Yancy CW: Eliminating racial and ethnic disparities in cardiac care. N Engl J Med. 2009, 360: 1172-1174. 10.1056/NEJMp0810121.
Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo K, Montague P, Kelemen L, Yi C, Lonn E, Gerstein H: Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic Groups (SHARE). Lancet. 2000, 356: 279-284. 10.1016/S0140-6736(00)02502-2.
Lanza GA: Editorial. Ethnic variations in acute coronary syndromes. Heart. 2004, 90: 595-597. 10.1136/hrt.2003.026476.
Mak KH, Bhatt DL, Shao M, Hankey GJ, Easton JD, Fox KAA, Topol EJ: Ethnic variation in adverse cardiovascular outcomes and bleeding complications in the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) study. Am Heart J. 2009, 157 (4): 658-665. 10.1016/j.ahj.2008.08.031.
Shaw LJ, Shaw RS, Merz NB, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKAy CR, Block PC, Hewitt K, Weintraub WS, Peterson ED on behalf of the American College of Cardiology (ACC)-National Cardiovascular Data Registry Investigators (NCDR): Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the ACC-NCDR. Circulation. 2008, 117: 1787-1801. 10.1161/CIRCULATIONAHA.107.726562.
Fox KAA: Registries and surveys in acute coronary syndrome. Eur Heart J. 2006, 27: 2260-2262. 10.1093/eurheartj/ehl240.
Alpert JS: Editorial. Are data from clinical registries of any value?. Eur Heart J. 2000, 21: 1399-1401. 10.1053/euhj.2000.2265.
Pillay MS, Noor Hisham A, Zaki M, Lim TO, Jamaiyah H, Purany SPJ: Patient registries in Malaysia and the role of the Clinical Research Centre of the Ministry of Health. Med J Malaysia. 2008, 63 (Suppl C): 1-4.
Chin SP, Jeyaindran S, Azhari R, Wan Azman WA, Omar I, Robaayah Z, Sim KH: Acute coronary syndrome (ACS) Registry -Leading the charge for National Cardiovascular Disease (NCVD) Database. Med J Malaysia. 2008, 63 (Suppl C): 29-36.
Wan Ahmad WA, Sim KH: National Cardiovascular Disease Database (NCVD). Inaugural Report of the Acute Coronary Syndrome (ACS) Registry. 2007, [http://www.acrm.org.my/ncvd/acsReport_07-08.php] (Accessed 15 August 2013), &2008
Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC: 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the Canadian Cardiovascular Society Endorsed by the American Academy of Family Physicians. J Am Coll Cardiol. 2008, 51: 200-247.
Jneid H, Anderson JL, Wright RS, Adams CD, Bridges CR, Casey DE, Ettinger JSM, Fesmire FM, Ganiats TG, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP: ACCF/AHA Focused Update of the Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction (Updating the 2007 Guidelines and Replacing the 2011 Focused Update): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012, 2012 (126): 875-910.
WHO Expert Consultation: Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004, 363: 157-163.
Steg G, James SK, Atar D, Badano LP, Blo¨mstrom-Lundqvist C, Borger MA, Mario CD, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, Hof AV, Widimsky P, Zahger D, The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC): ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012, 33: 2569-2619.
Chesebro JH, Knatterud G, Roberts R, et al: Thrombolysis in Myocardial Infarction (TIMI) Trial. Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987, 76: 142-154. 10.1161/01.CIR.76.1.142.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, Serebruany V, Valgimigli M, Vranckx P, Taggart D, Sabik JF, Cutlip DE, Krucoff MW, Ohman EM, Steg PG, White H: Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011, 123: 2736-2747. 10.1161/CIRCULATIONAHA.110.009449.
Department of Statistics, Malaysia: Population and Demography. 5-[http://www.statistics.gov.my/portal/index.php?option=com_content%26view=article%26id=1465%26lang=en] (Accessed 15 August 2013)
Goyal A, Yusuf S: The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006, 124: 235-244.
Cappuccio FP, Cook DG, Atkinson RW: Prevalence, detection and management of cardiovascular risk factors in different ethnic groups in South London. Heart. 1997, 78: 553-563.
Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S, Yusuf S: Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007, 297: 286-294. 10.1001/jama.297.3.286.
Beckles GLA, Miller GJ, Kirkwood BR, Alexis SD, Carson DC, Byam NTA: High total and cardiovascular disease mortality in adults of Indian descent in Trinidad, unexplained by major cardiovascular risk factors. Lancet. 1986, 327: 1298-1301. 10.1016/S0140-6736(86)91221-3.
Lee J, Heng D, Chia KS, Chew SK, Tan BY, Hughes K: Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore Cardiovascular Cohort Study. Intern J Epidem. 2001, 30: 983-988. 10.1093/ije/30.5.983.
Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N, for the Investigators in the National Registry of Myocardial Infarction 1, 2, 3: Temporal trend in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999. J Am Coll Cardiol. 2000, 36: 2056-2063. 10.1016/S0735-1097(00)00996-7.
Steg PG, Goldberg RJ, Gore JM, Fox KAA, Eagle KA, Sadiq I, Kasper R, Rushton-Mellor SK, Anderson FA: Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE). Am J of Cardiol. 2002, 90 (4): 358-363. 10.1016/S0002-9149(02)02489-X.
Avezum A, Makdisse M, Spencer F, Gore JM, Fox KAA, Montalescot G, Eagle KA, White K, Mehta RH, Knobel E, Collet JP: Impact of age on management and outcome of acute coronary syndrome: observation from Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005, 149: 67-73. 10.1016/j.ahj.2004.06.003.
Hasdai D, Behar S, Wallentin L, et al: A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J. 2002, 23: 1190-1201. 10.1053/euhj.2002.3193.
Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, Hasdai D: Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006, 27: 789-795. 10.1093/eurheartj/ehi774.
Xavier D, Pais P, Devereaux PJ, Xie CC, Prabhakaran D, Reddy KS, Gupta R, Joshi P, Kerkar P, Thanikachalam S, Haridas KK, Jaison TM, Naik S, Maity AK, Yusuf S, on behalf of the CREATE registry investigators: Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008, 371: 1435-1442. 10.1016/S0140-6736(08)60623-6.
AlHabib KF, Hersi A, AlFaleh H, Kurdi M, Arafah M, Youssef M, AlNemer K, Bakheet A, AlQarni A, Soomro T, Taraben A, Malik A, Ahmed WH: The Saudi Project for Assessment of Coronary Events (SPACE) registry: design and results of a phase I pilot study. Can J of Cardiol. 2009, 25 (7): 255-258. 10.1016/S0828-282X(09)70513-6.
Leuzzi C, Modena MG: Coronary artery disease: clinical presentation, diagnosis and prognosis in women. Nutr, Metab & Cardiovascular Diseases. 2010, 20: 426-435. 10.1016/j.numecd.2010.02.013.
Laskey WK: Editorial. Gender differences in the management of coronary artery disease; bias or good clinical judgment?. Ann Intern Med. 1992, 116: 869-871. 10.7326/0003-4819-116-10-869.
Steingart RM, Packer M, Hamm P, Coglianee ME, Gersh B, Geltman E, Josephine S, et al: Sex differences in the management of coronary artery disease. N Engl J Med. 1991, 325: 226-230. 10.1056/NEJM199107253250402.
Hochman JS, Tamis JE, Thompson TD, Weaver WD, White HD, Van De Werf F, Aylward P, Topol EJ, Califf RM, For the Global USe of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndrome. IIb. Investigator: Sex, clinical presentation and outcome in patients with acute coronary syndromes. N Eng J Med. 1999, 341: 226-232. 10.1056/NEJM199907223410402.
Steingart RM, Forman S, Coglianese M, Bittner V, Mueller H, Frishman W, Handberg E, Gambino A, Knatterud G, Conti CR: Factors Limiting the Enrollment of Women in a Randomized Coronary Artery Disease Trial. For the ASYMPTOMATIC CARDIAC ISCHEMIA PILOT STUDY (ACIP) investigator. Clin Cardiology. 1996, 19: 614-618. 10.1002/clc.4960190807.
Kee CC, Jamaiyah H, Noor Safiza MN, Geeta A, Khor GL, Suzana S, Jamalludin AR, Rahmah R, Ahmad AZ, Ruzita AT, Wong NF, Ahmad Faudzi Y: Abdominal obesity in Malaysian adults: National Health and Morbidity Survey III (NHMS III, 2006). Malaysian J Nutr. 2008, 14 (2): 125-135.
Ismail MN, Chee SS, Nawawi H, Yusof K, Lim TO, James WPT: Obesity in Malaysia. Obes Rev. 2002, 3: 203-208. 10.1046/j.1467-789X.2002.00074.x.
Rampal L, Rampal S, Geok LK, Zain AM, Ooyub S, Rahmat R, Ghani SN, Krishnan J: A national study on the prevalence of obesity among 16,127 Malaysians. Asia Pacific J Clin Nutrition. 2007, 16 (3): 561-566.
Wilson P, D’Agostino R, Sullivan L, Parise H, Kannel WB: Overweight and obesity as determinants of cardiovscular risk. The Framingham Experience. Arch Intern Med. 2002, 162 (16): 1867-1872. 10.1001/archinte.162.16.1867.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, Rinfret S, Schiffrin EL, Eisenberg MJ: The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol. 2010, 56 (14): 1113-1132. 10.1016/j.jacc.2010.05.034.
Shehab A, Al-Dabbagh B, Almahmeed W, Bustani N, Nagelkerke N, Alnaeemi A, Alsheikh-Ali AA: Prevalence, characteristics, and in-hospital outcomes of metabolic syndrome among patients with acute coronary syndrome in the United Arab Emirates. Open Cardiovasc Med J. 2012, 6: 81-87. 10.2174/1874192401206010081.
Hughes K, Yeo PPB, Lun KC, Thai AC, Sothy SP, Wang KW, Cheah JS, Phoon WO, Lim P: Cardiovascular diseases in Chinese, Malays, and Indians in Singapore. II. Differences in risk factor levels. J Epid and Comm Health. 1990, 44: 29-35. 10.1136/jech.44.1.29.
Collins VR, Dowse GK, Cabealawa S, Ram P, Zimmet PZ: High mortality from cardiovascular disease and analysis of risk factors in Indian and Melanesian Fijians. Int J Epidemiol. 1996, 25 (1): 59-69. 10.1093/ije/25.1.59.
Meadows TA, Bhatt DL, Cannon CP, Gersh BJ, Röther J, Goto S, Liau C-S, Wilson PWF, Salette G, Smith SC, Steg G: Ethnic differences in cardiovascular risks and mortality in atherothrombotic disease: Insights from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Mayo Clin Proc. 2011, 86 (10): 960-967. 10.4065/mcp.2011.0010.
Mather HM, Keen H: The Southall Diabetes Survey: prevalence of known diabetes in Asians and Europeans. BMJ. 1985, 291: 1081-1084. 10.1136/bmj.291.6502.1081.
Wan Ahmad WA, Zambahari R, Ismail O, Sinnadurai J, Rosman A, Chin SP, Zainal Abidin I, Sim KH: Malaysian National Cardiovascular Disease Database (NCVD) – Acute Coronary Syndrome (ACS) registry: How are we different?. CVD Prevent and Control. 2011, 6 (3): 81-89. 10.1016/j.cvdpc.2011.04.004.
Tan CE, Tan BY, Emmanuel SC, Jacob E: Prevalence of diabetes and ethnic differences in cardiovascular risk factors, The 1992 Singapore National Health Survey. Diabetes Care. 1999, 22: 241-247. 10.2337/diacare.22.2.241.
Esteghamati A, Abbasi M, Nakhjavani M, Yousefizadeh A, Basa AP, Afshar H: Prevalence of diabetes and other cardiovascular risk factors in an Iranian population with acute coronary syndrome. Cardiovas Diabetol. 2006, 5: 15-10.1186/1475-2840-5-15.
Al-Nuaim R: High prevalence of metabolic risk factors for cardiovascular diseases among Saudi population, aged 30–64 years. Int J Cardiol. 1997, 62 (3): 227-235. 10.1016/S0167-5273(97)00268-4.
Li N, Tuomilehto J, Dowse G, Virtala E, Zimmet P: Prevalence of coronary heart disease indicated by electrocardiogram abnormalities and risk factors in developing countries. J Clin Epid. 1994, 47 (6): 599-611. 10.1016/0895-4356(94)90208-9.
Rogers W, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, Pollack CV, Gore JM, for the National Registry of Myocardial Infarction Investigators: Trends in presenting characteristics and hospital mortality among patients with STEMI and NSTEMI in National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008, 156: 1026-1034. 10.1016/j.ahj.2008.07.030.
Mandelzweig L, Battler A, Boyko V, et al: The second Euro Heart Survey on acute coronary syndromes: Characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006, 27: 2285-2293. 10.1093/eurheartj/ehl196.
Yan AT, Tan M, Fitchett D, Chow CM, Fowlis RA, McAvinue TG, Roe MT, Peterson ED, Tu JV, Langer A, Goodman SG, Canadian Acute Coronary Syndromes Registry Investigators: One-year outcome of patients after acute coronary syndrome (from the Canadian Acute Coronary Syndromes Registry). Am J Cardiol. 2004, 94 (1): 25-29. 10.1016/j.amjcard.2004.03.024.
McKeigue PM, Adelstein AM, Shipley MJ, Riemersma RA, Marmot MG, Hunt SP, Butler SM, Turner PR, et al: Diet and risk factors for CHD in Asian Indians in Northwest London. Lancet. 1985, 326 (8464): 1086-1090. 10.1016/S0140-6736(85)90684-1.
Miller GJ, Kotecha S, Wilkinson WH, Wilkes H, Stirling Y, Sanders TAB, Broadhurst A, Allison J, Meade TW: Dietary and other characteristics relevant for CHD in men of Indian, West Indian and European descent in London. Atherosclerosis. 1988, 70: 63-72. 10.1016/0021-9150(88)90100-1.
Thomas I, Gupta S, Sempos C, Cooper R: Serum lipids in Indian physicians living in the US compared to US born physicians. Atherosclerosis. 1986, 61: 99-106. 10.1016/0021-9150(86)90068-7.
Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger D, The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC): ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2011, 32: 2999-3054.
Yadav P, Joseph D, Joshi P, Sakhi P, Jha RK, Gupta J: Clinical profile & risk factors in acute coronary syndrome. National J Comm Med. 2010, 1 (2): 150-151.
Deshpandey JD, Dixit JV: Hospital based study of clinical profile and risk factors for acute myocardial infarction. Indian Med Gazette. 2009, Oct: 380-382.
Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O’Keefe J, Everlie P, Donohue B, Chelliah N, Timmis GC: A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993, 328: 673-679. 10.1056/NEJM199303113281001.
Keeley EC, Boura JA, Grines CL: Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet. 2003, 361 (9351): 13-20. 10.1016/S0140-6736(03)12113-7.
McNamara RL, Herrin J, Wang Y, Curtis JP, Bradley EH, Magid DJ, Rathore SS, Nallamothu BK, Peterson ED, Blaney ME, Frederick P, Krumholz HM: Impact of delay in door-to-needle time on mortality in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2007, 100: 1227-1232. 10.1016/j.amjcard.2007.05.043.
The GUSTO investigator groups: An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993, 329: 673-682.
Sonel AF, Good CB, Mulgund J, Roe MT, Gibler WB, Smith SC, Cohen MG, Pollack CV, Ohman EM, Peterson ED, for the CRUSADE Investigators: Racial variations in treatment and outcomes of Black and White patients with high-risk Non–ST-elevation acute coronary syndromes insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005, 111: 1225-1232. 10.1161/01.CIR.0000157732.03358.64.
Feder G, Crook AM, Magee P, Banerjee S, Timmis AD, Hemingway H: Ethnic differences in invasive management of coronary disease: prospective cohort study of patients undergoing angiography. BMJ. 2002, 324: 511-516. 10.1136/bmj.324.7336.511.
Ford E, Newman J, Deosaransingh K: Racial and ethnic differences in the use of cardiovascular procedures: findings from the California Cooperative Cardiovascular Project. Am J Public Health. 2000, 90 (7): 1128-1134.
Bradley EH, Herrin J, Wang YF, McNamara RL, Webster TR, Magid DJ, Blaney M, Peterson ED, Canto JG, Pollack CV, Krumholz HM: Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004, 292 (13): 1563-1572. 10.1001/jama.292.13.1563.
Peterson ED, Shaw LK, De Long ER, Pryor DB, Califf RM, Mark DB: Racial variation in the use of coronary-revascularization procedures: are the differences real? Do they matter?. N Eng J Med. 1997, 336: 480-486. 10.1056/NEJM199702133360706.
Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM: Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Eng J Med. 2001, 344: 1443-1449. 10.1056/NEJM200105103441906.
Leape LL, Hilborne LH, Bell R, Kamberg C, Brook RH: Underuse of cardiac procedures: Do women, ethnic minorities and the uninsured fail to receive needed revascularization?. Ann Intern Med. 1999, 130: 183-192. 10.7326/0003-4819-130-3-199902020-00003.
Cohen MG, Fonarow GC, Peterson ED, Moscucci M, Dai D, Hernandez AF, Bonow RO, Smith SC: Racial and ethnic differences in the treatment of acute myocardial infarction. Findings from the Get With The Guidelines–Coronary Artery Disease Program. Circulation. 2010, 121: 2294-2301. 10.1161/CIRCULATIONAHA.109.922286.
Peterson ED, Shah BR, Parsons L, Pollack CV, French WJ, Canto JG, Gibson CM, Rogers WJ, for the NRMI Investigators: Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008, 156: 1045-1055. 10.1016/j.ahj.2008.07.028.
Gibson CM: NRMI and current treatment patterns for ST-elevation myocardial infarction. Am Heart J. 2004, 148: 29-33. 10.1016/j.ahj.2004.09.012.
Thanavaro S, Kleiger RE, Province MA, Hubert JW, Miller JP, Krone RJ, Oliver GC: Effect of infarct location on the in-hospital prognosis of patients with first transmural myocardial infarction. Circulation. 1982, 66 (4): 742-747. 10.1161/01.CIR.66.4.742.
Weintraub WS, Vaccarino V: Explaining racial disparities in coronary in women. Circulation. 2003, 108: 1041-1043. 10.1161/01.CIR.0000083529.48474.4F.
Zhang Z, Fanf J, Gillespie C, Wang G, Hong Y, Yoon PW: Age-specific gender differences in in-hospital mortality by type of AMI. Cardiol. 2012, 109: 1097-1103. 10.1016/j.amjcard.2011.12.001.
Ahmed E, El-Menyar A, Singh R, Al Binali HA, Al Suwaidi J: Effect of age on clinical presentation and outcome of patients hospitalized with acute coronary syndrome: a 20-year registry in a middle eastern country. The Open Cardiovasc Med J. 2012, 6: 60-67. 10.2174/1874192401206010060.
Jeyamalar R: Coronary artery disease in Malaysia: a perspective. Med J Malaysia. 1991, 46 (1): 1-6.
Mehta R, Parson L, Rao S, Peterson ED, on behalf of National Registry of Myocardial Infarction (NRMI) Investigators: Association of bleeding and In-hospital mortality in black and white patients with ST-segment-elevation myocardial infarction receiving reperfusion. Circulation. 2012, 125: 1727-1734. 10.1161/CIRCULATIONAHA.111.068668.
Yan AT, Huynh RTYT, DeYoung P, Weeks A, Fitchett DH, Langer A, Goodman SG, for the INTERACT Investigators: Bleeding and outcome in acute coronary syndrome: Insights from continuous electrocardiogram monitoring in the Integrilin and Enoxaparin Randomized Assessment of Acute Coronary Syndrome Treatment (INTERACT) trial. Am Heart J. 2008, 156 (4): 769-775. 10.1016/j.ahj.2008.05.022.
Mortensen J, Thygesen SS, Johnsen SP, Vinther PM, Kristensen SD, Refsgaard J: Incidence of bleeding in ‘real-life’ acute coronary syndrome patients treated with antithrombotic therapy. Cardiology. 2008, 111: 41-46. 10.1159/000113426.
Shakir DK, Zubaid M, Al Mallah MH, Mahmeed WL, Alsheikhali AA, Singh R, Amin H, Rao N, Suwaidi JA: Bleeding complications with acute coronary syndrome in six Middle Eastern countries. Acta Cardiol. 2011, 66 (2): 203-211.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2261/13/97/prepub
Acknowledgements
The authors would like to acknowledge the Chairperson of the NCVD Governance Board for permission to use the data for this paper. We would like to thank all doctors and nurses participating in the NCVD.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Both authors declare that they have no competing interests.
Authors’ contributions
LHT and RBN collated and analyzed the data. LHT prepared the first draft of the paper and RBN vetted the final manuscript. Both authors interpreted the results, revised the paper, and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lu, H.T., Nordin, R.B. Ethnic differences in the occurrence of acute coronary syndrome: results of the Malaysian National Cardiovascular Disease (NCVD) Database Registry (March 2006 - February 2010). BMC Cardiovasc Disord 13, 97 (2013). https://doi.org/10.1186/1471-2261-13-97
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2261-13-97