Abstract
Background
In Mexico, guidelines for fasting periods, or any audits on this topic are unavailable, and therefore the attitudes of anesthesiologists for recommending preoperative fasting periods are unknown.
Material and methods
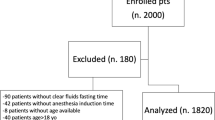
The study was a cross-sectional survey of anesthesiologists subscribed to the Annual Updated Course, organized by the Sociedad Mexicana de Anestesiologia in 2000. The response rate was 31.4%.
Results
Most respondents were general anesthesiologists, with 5 or more years experience in a clinical post, were working in both public and private hospitals, and were performing anesthetic procedures on both pediatric and adult patients and in both ambulatory and hospitalized patients. Approximately 23% of the respondents considered natural fruit juices to be clear liquids. For a pediatric patient ingesting breast milk 1 h before undergoing a surgical procedure, 45% thought that surgery should be delayed for 3h, followed by those delaying the surgical procedure for 6 to 8 h. Our results show that more than 50% of the anesthesiologists had better defined attitudes for fasting milk and clear liquids in patients of 6 month or under than for older children and adults. However, due to the poor definition or pre-operative fasting, using clear liquids, in all other patient groups, several patients are allowed to go without oral clear liquids administration for prolonged periods.
Conclusion
Preoperative fasting periods recommended by Mexican anesthesiologists differ from international guidelines.
Similar content being viewed by others
Background
A preoperative fasting period is always required in any patient undergoing an elective surgery, and guidelines have emerged in order to recommend a minimum fasting period required for adult and pediatric patients [1, 2]. Shorter fasting periods than that currently recommended could result in the increased risk of pulmonary aspiration of gastric content, whereas prolonged fasting has been related to discomfort, thirst, hunger, irritability in adult patients, and dehydration, hypovolemia and hypoglycemia in children. In Mexico guidelines for fasting periods or audits on this topic are not available, and therefore the attitudes of anesthesiologists for recommending preoperative fasting periods are ignored. In order to have any evidence in relation to the fasting periods recommended by anesthesiologists in our country, we performed the present study.
Material and methods
The study was a cross-sectional survey. The survey was developed and validated by consensus by a group of anesthesiologists and clinical epidemiologists, and tested thereafter in a small group of anesthesiologists. It was printed on both sides of a sheet of paper, and attached to the documents delivered to each of the 825 anesthesiologists subscribed to the Annual Updated Course organized by the Sociedad Mexicana de Anestesiologia in 2000. This course, traditionally carried out in Mexico City, was selected due to the fact that it is the major national course of anesthesia, and therefore colleagues from all over the country attend the course. This gives the course a national representation. Voluntary participation was mentioned verbally at the moment the printed survey was provided to the anesthesiologists. Negation to answer the survey was not penalized in any form.
The survey included the following four sections:
Section 1. General information
1. Your current maximal specialty training is: anesthesiologist, anesthesiologist with subspecialty training, or anesthesiology resident
2. Have you been practicing anesthesia for <5, 5 to 10, or >10 years?
3. Have you been working at a public, private or both types of health services?
4. Are your anesthetic procedures performed in pediatric, adult, or mixed patients? If mixed patients was selected, then the proportion representing the pediatric patients was asked (<25, 25 to 50, 50 to 75 or >75%).
5. Are your anesthetic procedures performed on ambulatory, hospitalized, or mixed patients? If a mixed setting was selected, then the proportion representing the pediatric patients was asked (<25, 25 to 50, 50 to 75 or >75%).
Section 2. The availability of guidelines at work
6. Do you have fasting guidelines at your work? If so, how long have they been available at you private or public health service?
Section 3. Knowledge of guidelines
7. Have you read the guidelines for fasting periods elaborated by the American Society of Anesthesia (ASA) Task Force on Preoperative Fasting published in 1999?
8. Have you read the guidelines for preoperative fasting periods published by the Sociedad Mexicana de Anestesiología in 1999? (This question in relation to non-existent guidelines was included in order to evaluate whether the anesthesiologists were answering automatically positive).
Section 4. Clinical practices. For this section, we considered a clear liquid to be any aqueous solution which is liquid at 37°C [3], non clear fluids to be suspensions and emulsions, breast milk whether it was directly provided by the mother or obtained from her and thereafter provided by means of a nursing bottle, and solid food to be any kind of meat.
9. A list of eight drinks was provided and anesthesiologists had to answer whether they were clear liquids or not. The following drinks were included: clear water, industrialized fruit juice, natural fruit juice, black coffee, breast milk and infant formula, milk-based jelly, concentrated industrialized fruit juice, and liquid food supplement (e.g. Ensure®)
10. What is your attitude for a male patient, 2 yr. old undergoing surgical repair of a hiatal hernia who ingested breast milk 1 h before surgery: to avoid the surgery, to delay the surgery for 2, 3 or 6 to 8 h, or to continue with the surgical plan?
11. What is your attitude for a patient 62 yr. old receiving ranitidine and cisapride, and undergoing surgical repair of hiatal hernia: to avoid the surgery, to modify the dose of ranitidine and cisapride, no modification in dosage and continuation of surgical plan, or you do not know?
12. What duration of pre-operative fasting using breast milk or infant formula do you recommend for patients age <6 mo., 6 mo. to 3 yr., or children >3 yr. undergoing a surgical procedure?
13. What duration of pre-operative fasting for using clear liquids do you recommend for patients aged <6 mo., 6 mo. to 3 yr., children >3 yr., adolescents and adults, or old patients undergoing a surgical procedure?
14. What duration of pre-operative fasting for solids do you recommend for patients aged <6 mo., 6 mo. to 3 yr., children >3 yr., adolescents and adults, or old patients undergoing a surgical procedure?
Invitation to return the survey was performed during the resting periods of the course. Because the course did not include any topic on fasting, no follow-up questionnaire was performed. The response rate was 31.4%, and data were summarized by means of descriptive statistics as number and proportions (%) with the corresponding 95% confidence of intervals (CI95%), the two latter computed from respondents for each question. When answers were analyzed as a set, comparisons between children and adults were performed by means of the x2 test at a significant limit of p < 0.05, and CI95% were not computed.
Results
Of the 259 respondents, approximately 70% were general anesthesiologists, had a clinical practice of 5 years or longer and were working in both public and private hospitals (Table 1). Most of them, n = 212, were performing anesthetic procedures in both pediatric and adult patients as following. Children represented <25% of their patients for 56.3% (CI95% 49.6 to 63.0%), between 25 to 50% for 15.8% (CI95% 10.9 to 20.7%), between 50 to 75% for 6.3% (CI95% 3.0 to 9.6%), and 75% for 3.3% (CI95% 0.9 to 5.7%).
Most of the anesthesiologists (n = 220) performed both ambulatory and hospitalized procedures (Table 1). Ambulatory procedures were performed in <25% of their patients by 50% (CI95% 43.4 to 56.6%) of them, in 25 to 50% for 30.4% (CI95% 24.3 to 36.5%), in 50 to 75% for 9.6% (CI95% 5.7 to 13.5%), and in >75% for only 1.3% (CI95% -0.2 to 2.8%).
Of 259, 90.4% (CI95% 86.8 to 94.0%) recognized the availability of guidelines at work setting. Of 198, 72.7% (CI95% 66.5 to 78.9%) answered the guidelines have been available for >5 yr. in public hospitals. While of 224, 67.4% (CI95% 61.3 to 73.5%) answered the guidelines have been available for >5 yr. in private hospitals. Furthermore, of 230, 39.6% (CI95% 33.3 to 45.9%) have not read the guidelines published by the ASA Task Force on Preoperative Fasting. However, 58.3% (CI95% 51.9 to 64.7%) accepted having read the guidelines published in a national journal.
From the list of drinks, industrialized clear juices and black coffee were considered clear liquids by a small proportion of respondents (Table 2), whereas approximately one fifth of anesthesiologists considered as clear liquid the natural fruit juices. Attitudes of the anesthesiologists for a pediatric patient ingesting breast milk 1 h before undergoing a surgical procedure were as following. The 44.6% (CI95% 38.2 to 51.0%) out of 229 delayed the surgery for 3 h, 28.3 % (CI95% 22.5 to 34.1%) delayed it for 6 to 8 h, 17.1% (CI95% 12.2 to 22.0%) delayed it for 2 h, 2.9% (CI95% 0.7 to 5.1%) avoided the surgery, 2.5% (CI95% 0.5 to 4.5%) continued with the surgical plan, and finally 3.8% (CI95% 1.3 to 6.3%) recognized they do not know what to do.
For the adult patient receiving ranitidine and cisapride, 73.3% (CI95% 67.6 to 79.0%) did not modify treatment or the surgical schedule, 16.3% (CI95% 11.6 to 21.1%) recommended to modify the dose of any or both drugs, 3.3% (CI95% 1.0 to 5.6%) stopped administration of these drugs, and 3.8% (CI95% 1.3 to 6.3%) recognized they do not know what to do.
Furthermore, anesthesiologists recommended shorter fasting periods for breast or infant formula in pediatric patients <6 mo. and between 6 mo. to 3 yr. than for children > 3 yr. (Figure 1). For clear liquids, most preferred a fasting period of 2 h in patients <6 mo. while 4 to 6 h was recommended for patients between 6 mo. to 3 yr. and longer fasting periods were preferred for children >3 yr., adolescents and adults, and older patients (Figure 2). Even more, when fasting periods for clear liquids were specified by direct answers anesthesiologists also preferred shorter fasting periods for children than for adult patients (Table 3). Finally, fasting periods ranging from 6 to 8 h for solids were recommended for all groups (Figure 3).
Discussion
The low response rate is a major deficiency of the present study. In surveys also related to fasting, applied to British, German and American anesthesiologists, a response rate ranging between 67 to 80% was reported [4–6]. Furthermore, in two previous surveys applied during the same course, we obtained a response rate of approximately 40% [7, 8]. However, despite the general low response rate makes our results likely not representative, they can be supported by previous experiences or by national patterns. Similar demographic data have been observed in other two surveys performed at the same course in two different years [7, 8]. Furthermore, the low rate of residents attending the course was also reflected into the low rate of residents replying the survey (Table 1).
Among the clear liquids, our colleagues identified only water as a clear one, while a high rate identified a natural juice also as a clear liquid. Furthermore, they preferred shorter fasting periods for infants than for children >3 yr., adolescents, adults or old patients. This attitude was expressed both when answering a specific question (Table 3), and when freely giving the fasting time (Figures 1,2,3). According to the ASA Task Force, a preoperative fasting period for breast milk of 4 hours for both neonates and infants has been recommended [1]. For infants and children it is appropriate to fast from intake of infant formula for 6 or more hours. For patients of all ages requiring general anesthesia, regional anesthesia or sedation/analgesia, the Task Force supported a fasting period for a light meal (e.g. toast and clear liquid) or non-human milk of 6 hours before elective procedures [1]. Furthermore, oral administration of clear liquids in order to avoid dehydration, discomfort and other potential complications has been recommended for many years [9–14]. Even more, it was recently demonstrated that oral administration of an electrolyte solution 2–3 h before surgery in order to interrupt a prolonged fasting period results in clear benefits for the pediatric patients [15].
Our results support that >50% of the anesthesiologists had better defined attitudes for fasting milk and clear liquids in patients <6 mo. than for older children and adults. However, attitudes for fasting for clear liquids were poorly defined in all the other groups, in some instances allowing patients without oral clear liquids administration for prolonged periods. Whereas fasting for solids was defined between 6 to 8 in all groups. In a national survey performed in the United States [16], the anesthesiologists were more likely to allow clear liquids before elective surgeries for children than for adults. Patient compliance by avoiding some uncomfortable procedures including prolonged fasting periods that prone patients to dehydration must be counterbalanced with risk of aspiration [17]. However, this concept could allow the individual prescription of fasting periods according to each anesthesiology criteria. In fact, more than a decade ago the Canadian Society of Anaesthesia allowed each Department of Anesthesia in Canada to dictate its own guidelines for fasting [2].
Preoperative fasting guidelines have been available in several countries for many years [18, 19], whereas in Mexico they have not been established by neither regional nor national groups of anesthesiologists. However, most anesthesiologists answered that preoperative fasting guidelines have been available at public and private hospitals for > 5 yr. It is probable that respondents were considering department criteria or attitudes traditionally performed as established guidelines. Even more, most anesthesiologists answered they had not read the guidelines published by the ASA Task Force for Preoperative Fasting while answered they had read the unavailable Mexican guidelines. Probably our colleagues were biased to recognize that they knew the guidelines published in Spanish by a national journal of anesthesia even if the guidelines did not exist. Finally, despite guidelines are not normative, it is expected that anesthesiologists adhering to them will have an improvement of their own clinical practice [19–21].
According to experience in other centers, efforts to correct some adverse attitudes in relation to the fasting periods have not been completely successful [17, 19, 22, 23]. If we are facing a more complex problem not limited to fasting periods, the contribution of the different groups of Mexican anesthesiologists to extend basic information in courses will result of major importance. The problem will certainly also require the participation of different centers forming general anesthesiologists in order to review their contribution to topics requiring an urgent attention as they were identified as problematic by the different surveys performed in Mexico, i.e. blood transfusion [7, 8] and fasting periods (current study). We therefore consider to plan and to promote audits at different hospitals, and to include intensive educational programs addressed to bring practice into line with published information as urgent measures.
References
American Society of Anesthesiologists Task Force on Preoperative Fasting: Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. Anesthesiology. 1999, 90: 896-905.
Goresky GV, Maltby R: Fasting guidelines for elective surgical patients. Can J Anaesth. 1990, 37: 493-495.
American Dietetic Association: Manual of Clinical Dietetics Chicago. Chicago. 1998
Steeds C, Mather SJ: Fasting regimens for regional ophtalmic anaesthesia. A survey of members of the British Ophtalmic Anaesthesia Society. Anaesthesia. 2001, 56: 638-642. 10.1046/j.1365-2044.2001.02116.x.
Haas U, Motsch J, Schreckenberger R, Bardenheuer HJ, Martin E: Premedication and preoperative fasting in pediatric anesthesia. Results of a survey (in German). Anaesthesist. 1998, 47: 838-843. 10.1007/s001010050633.
McKinley AC, James RL, Mims GR: NPO after midnight is no longer common practice for the majority of anesthesiologists. Am J Anesthesiol. 1995, 22: 88-92.
Moyao-García D, Nava-Ocampo AA: Survey of transfusional practices among anesthesiologists. I. Results of two different years of survey application, 1996 and 1998 (in Spanish). Rev Mex Anest. 1999, 22: 76-84.
Nava-Ocampo AA, Moyao-García D: Survey of transfusional practices among anesthesiologists. II. Qualitative comparison between preferences of Mexican anesthesiologists and international recommendations (in Spanish). Rev Mex Anest. 1999, 22: 85-90.
Splinter WM, Schaefer JD: Unlimited clear fluid ingestion two hours before surgery in children does no affect volume or pH stomach contents. Anaesth Intensive Care. 1990, 18: 522-526.
Splinter WM, Shaefer JD: Clear fluids three hours before surgery do not affect the gastric fluid contents of children. Can J Anaesth. 1990, 37: 498-501.
Splinter WM, Stewart JA, Muir JG: Large volumes of apple juice preoperatively do not affect gastric pH and volume in children. Can J Anaesth. 1990, 37: 36-39.
Splinter WM, Schneider ME, Shaefer JD: Unrestricted clear fluids ingestion 3-hours before anesthesia is safe for adolescents. Anesth Analg. 1990, 70: S387-
Phillips S, Daborn AK, Hatch DJ: Preoperative fasting for paediatric anaesthesia. Br J Anaesth. 1994, 73: 529-536.
Coté CJ: Preoperative preparation and premedication. Br J Anaesth. 1999, 83: 16-28.
Moyao-García D, Corrales-Fernández MA, Blanco-Rodríguez G, Sánchez-Hernández E, Nava-Ocampo AA: Benefits of oral administration of an electrolyte solution interrupting a prolonged preoperatory fasting period in pediatric patients. J Pediatr Surg. 2001, 36: 457-459. 10.1053/jpsu.2001.21614.
Green CR, Pandit SK, Schork MA: Preoperative fasting time: Is the traditional policy changing? Results of a national survey. Anesth Analg. 1996, 83: 123-128.
Veall GRQ, Dorman T: Prolonged starvation in paediatric surgery. Anaesthesia. 1995, 50: 458-460.
Ericksson LI, Sandin R: Fasting guidelines in different countries. Acta Anaesthesiol Scand. 1996, 40: 971-974.
Fasting S, Søreide E, Ræder JC: Changing preoperative fasting policies: Impact of a national consensus. Acta Anaesthesiol Scand. 1998, 42: 1188-1191.
Emerson BM, Wrigley SR, Newton M: Pre-operative fasting for paediatric anaesthesia. A survey of current practice. Anaesthesia. 1998, 53: 326-330. 10.1046/j.1365-2044.1998.00317.x.
Wilson MC, Hayward RSA, Tunis SR, Bass EB, Guyatt G: User's guides to the medical literature. VIII. How to use clinical practice guidelines. B. What are the recommendations and will they help you in caring for your patients?. JAMA. 1995, 274: 1630-1632. 10.1001/jama.274.20.1630.
Ferrari LR, Rooney FM, Rockoff MA: Preoperative fasting practices in pediatrics. Anesthesiology. 1999, 90: 978-980. 10.1097/00000542-199904000-00008.
Maclean AR, Renwick C: Audit of pre-operative starvation. Anaesthesia. 1993, 48: 164-166.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2253/2/3/prepub
Acknowledgments
Authors thank the heads of the Sociedad Mexicana de Anestesiología in 2000 for giving permission to apply the survey during the course. We also thank to Miss Arely Venancio Mondragón for his helpful technical computing assistance, to Mr. Victor Manuel Vázquez for his assistance in preparing the manuscript in the English language, and to the journal's reviewer for the insightful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors contribution
JCR participated in the study design, carried out the survey and participated in the data interpretation. DMG participated in the study design, data interpretation and drafted the manuscript. AANO participated in the study design, data interpretation, statistical analysis and drafted the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ramírez-Mora, J.C., Moyao-García, D. & Nava-Ocampo, A.A. Attitudes of Mexican anesthesiologists to indicate preoperative fasting periods: A cross-sectional survey. BMC Anesthesiol 2, 3 (2002). https://doi.org/10.1186/1471-2253-2-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2253-2-3