Abstract
Background
This study was conducted to elucidate if nitric oxide is released by the porcine jejunal mucosa upon selective stimulation of AT2 receptors and the possible involvement of iNOS, and to investigate the presence of jejunal AT1 and AT2 receptors. Young landrace pigs were anaesthetized with ketamine and α-chloralose. Jejunal luminal NO output was assessed by intraluminal tonometry and analysed by chemiluminescense. Western blot analysis quantified mucosal iNOS and detected AT1 and AT2 receptor protein expression. AT1 and AT2 receptor RNA expression was detected by rtPCR.
Results
Baseline luminal NO output correlated significantly to baseline mucosal iNOS-protein content. In animals treated with the AT2-receptor agonist CGP42112A (n = 11) luminal NO output increased significantly (at 0.1 micrograms kg-1 min-1 and 1.0 micrograms kg-1 min-1), but not in animals simultaneously treated with the AT2-receptor antagonist PD123319 (bolus 0.3 mgkg-1, infusion 0.03 mg kg-1 h-1) (n = 7). No differences in iNOS protein expression were found between groups or before/after the administration of drugs. Western blot and rtPCR recognised expression of the AT1 and AT2 receptors in jejunal tissue.
Conclusion
The results suggest that activation of AT2 receptors increases jejunal luminal NO output. This response was not due to an increase in the expression of the iNOS protein in the mucosa.
Similar content being viewed by others
Background
The overall function of the renin-angiotensin system (RAS) and its key mediator angiotensin II (Ang II) is to maintain extracellular fluid volume and the electrolyte homeostasis, as well as to regulate vascular tone and blood pressure. Traditionally, the RAS is regarded as an endocrine system, but components of the RAS can be found in several tissues eg kidney, brain, adrenals and the reproductive organs, suggesting paracrine/autocrine functions [1, 2]. Most of the effects of Ang II, including cardiovascular, are mediated by activation of angiotensin II receptor type 1 (AT1 receptor)[2]. Efforts have recently been made to correlate biological functions to the angiotensin II receptor type 2 (AT2 receptor). Involvement in cell differentiation and inhibition of cell proliferation, particularly in fetal development, has been demonstrated [2]. In the adult organism the AT2 receptor has been shown to be present in eg ovaries, adrenal medulla and pancreas. It has also been identified in the gut [3–5] where it is suggested to influence jejunal sodium and water absorption and secretion, probably involving the release of nitric oxide (NO) and the generation of cyclic guanosine 3, 5-monophosphate (cGMP) [6, 7]. Johansson et al [4] demonstrated that rat duodenal mucosal bicarbonate secretion increased upon administration of the AT2-receptor agonist CGP42112A (0.1 μg kg-1 min-1). Furthermore, rat duodenal mucosal bicarbonate secretion has been shown to be regulated partly by NO [8].
The present study aimed to investigate if nitric oxide is released by the porcine jejunal mucosa upon the pharmacological activation (CGP42112A) of intestinal AT2 receptors and if a dynamic iNOS-protein expression is involved. Additionally, the study aimed to investigate the existence and expression of the AT1 and AT2 receptors in the porcine jejunum.
Results
NO output and iNOS expression
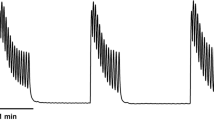
Baseline NO output varied considerably between individuals; range: 46 to 1138 ppb, but exhibited a positive correlation to the baseline mucosal iNOS content (Rho 0.65, p < 0.01). No significant differences in NO output were detected between groups at baseline. Luminal NO output increased in all animals treated with only CGP42112A (group B) at the doses 0.1 μg kg-1 min-1 and1.0 μg kg-1 min-1, compared to controls (group A) and to animals treated with PD123319 and CGP42112A simultaneously (group C) (Figure 1). Acute administration of PD123319 did not alter the baseline NO levels, as tested in separate experiments (n = 5, data not shown).
NO output recordings, presented as values relative to baseline, during infusion of A: saline (150 mM NaCl) (n = 5), B: CGP 42112A at increasing infusion rates (0.01 μg kg -1 min-1, 0.1 μg kg -1 min-1,1.0 μg kg -1 min-1) each lasting 45 min (n = 11), C: CGP 42112A (as in B) in the presence of PD123319 (0.3 mg kg-1 iv bolus and 0.03 mg kg-1 h-1 iv infusion administration initiated at baseline) (n = 7). A p-value < 0.05 was concidered significant and is denoted by *.
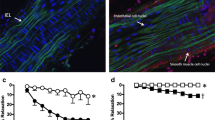
Western blot analysis did not detect any significant differences of iNOS expression between groups at baseline. The iNOS protein expression did not change significantly in any group and there were no significant differences between groups (ratio post-/pre-treatment) (Figure 2).
The ratio post- to pre-treatment iNOS protein expression (optical density). iNOS expression did not change significantly in any group and the change did not differ significantly between the groups: A: saline (150 mM NaCl) (n = 6), B: CGP 42112A at increasing infusion rates (0.01 μg kg-1 min-1, 0.1 μg kg-1 min-1,1.0 μg kg-1 min-1 iv) (n = 6), C: CGP 42112A (as in B) in the presence of PD123319 (0.3 mg kg-1 iv bolus and 0.03 mg kg-1h-1 iv infusion administration initiated at baseline) (n = 6).
AT1 and AT2 receptor expression
Western blot using antibodies specific for AT1 and AT2 receptor proteins recognised bands of the expected molecular weight 41 kDa and 44 kDa, respectively, in all samples (n = 11) (Figure 3).
Western blot experiments using specific antibodies to AT1 and AT2 receptors, respectively. Staining for AT1 receptor detect a single band at the size 41 kDa in all individuals (n = 11) and the PC12 cell lysate serving as a positive control. Staining for AT2 receptor detect a single band at the size 44 kDa in all individuals (n = 11) and in the KNRK cell lysate serving as a positive control.
The rtPCR using specific primers for AT1, AT2 receptor and GAPDH, respectively, recognised expression of RNA in all samples (n = 11) (Figure 4). The median ratio AT1/GAPDH and AT2/GAPDH were 0.429 (range 0.167–2.117; n = 11) and 0.645 (range 0.429–1.556; n = 11), respectively.
Hemodynamics
The hemodynamic variables (portal venous flow, cardiac output, heart rate and mean arterial pressure) did not differ between groups at baseline and were stable throughout the protocol, except for a slight but significant decrease in mean arterial pressure in group C.
Discussion
The present study demonstrates that intravenous infusion of the AT2 receptor ligand CGP42112A [13, 14] stimulates jejunal luminal NO output. The effect was absent in presence of the AT2 receptor blocker PD123319 giving strong support to the assumption that AT2 receptors initiate intestinal luminal NO formation. Jejunal nitric oxide formation was assessed using intraluminal tonometry, a method previously described for intestinal use by Snygg et al [15]. By definition the tonometric approach allows determination of NO levels in the close vicinity to the gas-equilibrating balloon. The NO levels obtained by this technique therefore reflect mainly NO formation in the luminal compartment and the mucosa located close to the luminal compartment. Furthermore, immunohistochemistry has revealed that the source for NO as assessed by a luminal tonometer is iNOS situated in the surface epithelial layer of the mucosa [15]. Nitric oxide may also be synthetized by endothelial NOS (eNOS) and neuronal NOS (nNOS). These NOS isoforms are situated in deeper layers of the intestinal wall [15] and it is unlikely that NO produced in the submucosa can reach the luminal compartment due to the rapid elimination by hemoglobin in such a highly perfused tissue. Our study confirms that iNOS is present in the pig jejunal mucosal epithelium and demonstrates a significant positive correlation between enzyme expression and NO output during basal conditions. The results also suggest that baseline NO output is determined by the amount of available synthase. This observation gives additional support to the view that luminal tonometry reflects mucosal epithelial NO synthesis. It may also explain why the measured luminal output of NO by the pig jejunal mucosa varies between individuals. The factors regulating intestinal epithelial iNOS expression is not completely known. Luminal microbial factors may be involved [16] as well as nutrient and digestive factors. The present approach using systemic drug administration makes it impossible to evaluate if the AT2-receptor mediated point of action is situated in the mesenteric area or elsewhere. However, local actions in the gut are expected as the AT2 receptor is present in the intestine of the rat and particularly in the mucosa [3, 4]. Our current data supports this hypothesis as both RNA and protein expression of the AT2 receptor were detected in the jejunal wall of the pig. In the literature AT2-receptor mediated actions on vascular tone have been reported in terms of vasodilation and decrease of arterial pressure and particularly so during pathological conditions with increased AT2 receptor expression [2, 17] eg in hypertensive states [18]. It was thus not surprising that an effect on MAP was not obtained upon infusion of the AT2 receptor agonist in the present study on healthy young pigs.
Several studies performed in vivo have demonstrated that CGP42112A is an agonist and that PD123319 is an antagonist at the AT2 receptor [4, 6, 7, 13, 14]. The present study shows that CGP42112A stimulates jejunal mucosal NO output. The sensitivity to PD123319 of this response speaks in favour of a selective action via the AT2 receptor in turn activating NO synthesis. AT2-receptor mediated NO dependent functional alterations have been reported also in the gastrointestinal tract [6] but direct measurements of NO synthesis in response to AT2-receptor activation in the intestine have not until now been reported.
AngII has previously been shown to induce eNOS expression in the kidney [19] but the receptor involved was not evaluated. Furthermore, it has been reported that AngII can activate NFκB [20] and particularily via the AT2 receptor [21, 22]. This transcription factor regulates the expression of several inflammatory mediators and among these iNOS [23, 24]. It was found in the present study that epithelial iNOS expression did not increase in mucosal specimens from the CGP42112A-treated animals. These results indicate that AT2-receptor stimulation does not activate the intestinal iNOS enzyme expression, at least not in the short term perspective. Taken together, the present study shows that selective AT2 receptor stimulation activates mucosal NO output. This may involve facilitation of the L-Arginine/NO pathway on the enzymatic level. The functional significance of increased mucosal NO formation in response to AT2-receptor stimulation remains to be investigated. Interestingly, RAS plays a role as a regulator of various inflammatory conditions including NO synthesis [25]. Intestinal epithelial NO, on the other hand, is proposed to be a key mediator of intestinal mucosal barrier functions and of host defence mechanisms against potentially noxious luminal agents [26]. It can thus be speculated that the present study reveals a previously unknown regulatory link between the RAS and the barrier properties of the gastrointestinal mucosa.
Conclusions
The results suggest that activation of AT2 receptors increases jejunal luminal NO output. This response was not due to an increase in the expression of the iNOS protein in the mucosa.
Methods
34 healthy young landrace pigs of both sexes, weighing 21–29 kg were used for the experiments. Biopsies for studying AT1 and AT2 receptor expression were obtained in a subset of 11 animals. The animals were fasted over night with free access to water. The study was approved by the Ethics Committee of Experiments in Animals, Goteborg University.
Anesthesia and surgical procedures
Anesthesia was induced by ketamine (Ketalar™, Parke-Davis, Solna, Sweden) intramuscularly (15 mg per kg body weight), azaperon (Stresnil™, Jansen-Cilag, Vienna, Austria) intramuscularly (80 mg) and a bolus of α-chloralose (Kebo Lab, Spanga, Sweden) intravenously (100 mg per kg body weight). Anesthesia was maintained by intravenous infusion of α-chloralose (25 mg per hour and kg body weight). The lack of response to painful stimuli was controlled before any surgical procedures. Fentanyl (100–200 μg) (Fentanyl Alpharma™, Alpharma, Stockholm, Sweden) was given when needed. The animals were tracheotomized and mechanically ventilated with 30% oxygen in air (Servo 900, Siemens, Stockholm, Sweden) to normocapnia. Isotonic Rehydrex® solution (2,5% glucose) (Fresenius Kabi, Uppsala, Sweden) was infused at 20 ml per kg body weight during surgery and 10 ml per kg body weight during the rest of the protocol. Heating blankets kept the core body temperature at 38°C. The right femoral vein and artery were catheterized for infusions and monitoring of arterial blood pressure and heart rate (Datex, Helsinki, Finland). A 7F central venous catheter (Secalon®T, Ohmeda, Swindon, UK) was inserted into the left external jugular vein for infusions. A 7F Swan-Ganz catheter (Baxter Medical AB, Solna, Sweden) was inserted via the right external jugular vein for measurement of core body temperature and to determine cardiac output by thermodilution as the average of triplicate measurements within a 10% range (Datex, Helsinki, Finland). A midline laparotomy was performed. An ultrasonic transit-time flowmetry probe (inner diameter of 16 mm, Transonic Systems Inc, Ithaca, NY, USA) was positioned around the portal vein to measure mesenteric blood flow. Small antemesenteric jejunal incisions were made at 80 and 130 cm distal to the ligament of Treitz, and tonometry catheters (Tonometrics Inc, Datex-Engstom Div, Helsinki, Finland) were inserted and advanced 20 cm. Each incision was tightened by a purse string suture.
NO measurements
Each tonometer was inflated with 5 ml of room air and left to equilibrate for 15 minutes. The gas was aspirated into a gas tight syringe and immediately injected into the sample line of a chemiluminescence analyser (ECO Physics AG, Dürnten, Switzerland) displaying NO concentrations in parts per billion (ppb) as previously described [9]. Data were collected during the last 15 minutes during each period of the protocol and represent a mean of the values obtained from the two tonometry ballons in each individual.
Western blot iNOS
Antemesenteric jejunal specimens were collected at the insertion sites for tonometry catheters during the surgical preparation and immediately after the protocol was finished. The superficial mucosal layer was scraped off and immediately frozen in liquid nitrogen and subsequently stored at -70°C. The specimens were sonicated (Sonifier 450/250, Branson Ultrasonics Co, Danbury, USA) during 2 × 15 min in a PE-buffer (10 mM potassium Phosphate buffer, pH 6.8, and 1 mM EDTA) containing CHAPS (3-[(3-cholamidopropyl) dimethyl-ammanio] 1-propanesulfonate), aprotinin (1 μg/ml), leupeptin (10 μg/ml), pepstatin (10 μg/ml) and Pefablock (1 mg/ml) (Boeringer Mannheim, Mannheim, Germany). Centrifugation was performed at 10.000 g for 10 min at 4°C. The supernatant was analysed for protein content by the method of Bradford [10] and stored at -70°C for further analysis. Samples were diluted in SDS-buffer and heated at 70°C for 10 min before they were loaded on a NuPage 3–8 % Tris-Acetat gel (NOVEX, San Diego, California, USA). One lane of each gel was loaded with prestained molecular weight standards (SeeBlue™, NOVEX, San Diego, CA, USA). After the electrophoresis the proteins were transferred to a polyvinyldifluoride membrane (Amersham, Buckinghamshire, UK) which was incubated with a specific antibody directed against iNOS (a 21-kDa proteinfragment corresponding to amino acids 961–1144 of mouse macrophage NOS) (Transduction Laboratories, Lexington, Ky, USA). An alkaline phosphatase conjugated goat anti-rabbit antibody (Santa Cruz, CA, USA) and CDP-Star (Tropix, Bedford, MA, USA) as a substrate, were used to identify immunoreactive proteins by chemiluminescense. Images were captured by a LAS-100 cooled CCD-camera (Fujifilm, Tokyo, Japan) and semi-quanification was performed using the soft ware Gauge 3.3 (Fujifilm, Tokyo, Japan). Data were assessed as optical density per microgram of protein and represent a mean of the values obtained from tissue sampled from the positions of the two tonometry ballons in each individual.
Western blot AT1 and AT2 receptors
Antemesenteric jejunal specimens (50–80 cm below the ligament of Treitz) of full wall thickness were collected immediately after the abdominal incision and snap frozen in liquid nitrogen and subsequently stored at -70°C. The specimens were homogenized on ice (Polytron, Kinematica AG, Switzerland) in buffer A (10% glycerol, 20 mM Tris-HCl pH 7,3, 100 mM NaCl, 2 mM phenylmethylsulfonyl fluoride, 2 mM EDTA, 2 mM EGTA, 10 mM sodium orthovanadate, 10 μg/mL leupeptin, and 10 μg/mL aprotinin) [11]. Centrifugation was performed at 30.000 g for 30 min at 4°C. The pellet was resuspended in buffer B (1 % NP-40 (Sigma-Aldrich, Stockholm, Sweden) in buffer A) and subsequently stirred at 4°C for one hour before centrifugation at 30.000 g for 30 min at 4°C. The supernatant was analysed for protein content by the method of Bradford [10] and stored at -70°C for further analysis. Loading on gels, electrophoresis and blotting procedures were performed as described above. NuPage 10% Bis-Tris gels and an electrophoresis running MOPS buffer (Invitrogen AB, Sweden) were used. KNRK (for AT2) and PC-12 (for AT1) whole cell lysates serving as positive controls (Santa Cruz, CA, USA), respectively. Polyvinyldifluoride membranes were incubated with polyclonal specific antibodies of rabbit origin directed to the AT1 and AT2 receptors, respectively (Santa Cruz, CA, USA). Identification of immunoreactive proteins and capturing of images were performed as described above.
rtPCR AT1 and AT2 receptors
Antemesenteric jejunal specimens (50 and 80 cm below the ligament of Treitz) of full wall thickness were collected immediately after the abdominal incision, placed in extraction solution RNAStat60 (TEL-TEST Inc, Friendswood, USA) and snap frozen in liquid nitrogen and stored at -70°C. The tissue was homogenized on ice (Polytron, Kinematica AG, Switzerland) and total RNA was extracted according to the methods supplied by the manufacturer following phenol-chloroform extraction and ethanol precipitation. The RNA concentration was quantified by absorbance measurement at 260 nm and the integrity was assessed by absorbance measurement at 280 nm. Reverse transcription was carried out using the SUPERSCRIPT™ First-Strand Synthesis System (Invitrogen AB, Sweden) according to the manufacturers instructions. Resulting cDNA was stored at -20°C until use. Amplification of cDNA was performed by usage of the PCR Reagent System (Invitrogen AB, Sweden) in a final volume of 25 μl and according to the manufacturers instructions. Primers specific for human AT1 and AT2 receptors and GAPDH (glyceraldehyde-3-phosphate dehydrogenase) [12] (Table 1) were added at a concentration of 500 nM. The amplification was performed using cycles as follows: 94°C for 5 min followed by 35 cycles (AT1 and AT2) or 28 cycles (GAPDH) at 94°C for 1 min for denaturation, 55°C (AT1) or 58°C (AT2 and GAPDH) for 1 min for annealing, 72°C for 1 min for elongation, followed by one cycle of 72°C for 7 min for final elongation and then samples were cooled. Cycles were optimized to represent the linear phase of the PCR reaction. The resulting products were electrophoresed on a 1,5% agarose-0.5 TBE gel containing 0.5 μg/ml etidium bromide. Visualisation of PCR products was achieved using ultraviolet light and images were captured by a LAS-100 cooled CCD-camera (Fujifilm, Tokyo, Japan).
Drugs
CGP 42112A (peptidergic AT2 receptor agonist) (Neosystem, Strasbourg, France) and PD123319 (non-peptidergic AT2 receptor antagonist) (Research Biochemicals International, Natick, MA, USA) were freshly dissolved in 150 mM sodium chloride solution.
Experimental protocol
All animals were left to stabilise for at least 30 minutes after surgery. After a baseline period of 45 min the animals received either saline vehicle (A, n = 5) or CGP 42112A (B, n = 11). In a third group the AT2-receptor antagonist PD123319 was administered (0.3 mg kg-1 iv. bolus and 0.03 mg kg-1 h-1 iv. infusion) during baseline and CGP 42112A administered subsequently as in B (C, n = 7). CGP 42112A was administered at three consecutive infusion rates, each lasting 45 min, starting at 0.01 μg kg-1 min-1 followed by 0.1 μg kg-1 min-1 and 1.0 μg kg-1 min-1. Hemodynamic variables were recorded continously with the exception for CO which was determined at the end of each 45 min period of the protocol.
Statistical analysis
NO output and iNOS protein content were analysed as calculated individual means. Spearman rank correlation test was used to test the relation between luminal NO output and iNOS content in basal conditions. Differences between pre- and post-treatment iNOS protein expression were analysed by Wilcoxon signed rank test. Differences between groups and post- to pre-treatment ratios of iNOS protein content, as well as relative changes in NO output, were analysed by the Kruskal-Wallis and the Mann-Whitney U test. Hemodynamic variables were analysed by ANOVA and the Bonferroni post-hoc test. A p-value less than 0.05 was considered statistically significant.
References
Zimmerman BG, Dunham EW: Tissue renin-angiotensin system: a site of drug action?. Annu Rev Pharmacol Toxicol. 1997, 37: 53-69. 10.1146/annurev.pharmtox.37.1.53.
de Gasparo M, Catt KJ, Inagami T, Wright JW, Unger T: International union of pharmacology. XXIII. The angiotensin II receptors. Pharmacol Rev. 2000, 52: 415-472.
Sechi LA, Valentin JP, Griffin CA, Schambelan M: Autoradiographic characterization of angiotensin II receptor subtypes in rat intestine. Am J Physiol. 1993, 265: G21-27.
Johansson B, Holm M, Ewert S, Casselbrant A, Pettersson A, Fandriks L: Angiotensin II type 2 receptor-mediated duodenal mucosal alkaline secretion in the rat. Am J Physiol Gastrointest Liver Physiol. 2001, 280: G1254-1260.
Duggan KA, Mendelsohn FA, Levens NR: Angiotensin receptors and angiotensin I-converting enzyme in rat intestine. Am J Physiol. 1989, 257: G504-510.
Jin XH, Siragy HM, Guerrant RL, Carey RM: Compartmentalization of extracellular cGMP determines absorptive or secretory responses in the rat jejunum. J Clin Invest. 1999, 103: 167-174.
Jin XH, Wang ZQ, Siragy HM, Guerrant RL, Carey RM: Regulation of jejunal sodium and water absorption by angiotensin subtype receptors. Am J Physiol. 1998, 275: R515-523.
Holm M, Johansson B, von Bothmer C, Jonson C, Pettersson A, Fandriks L: Acid-induced increase in duodenal mucosal alkaline secretion in the rat involves the L-arginine/NO pathway. Acta Physiol Scand. 1997, 161: 527-532. 10.1046/j.1365-201X.1997.00239.x.
Snygg J, Casselbrant A, Pettersson A, Holm M, Fandriks L, Aneman A: Tonometric assessment of jejunal mucosal nitric oxide formation in anaesthetized pigs. Acta Physiol Scand. 2000, 169: 39-45. 10.1046/j.1365-201x.2000.00678.x.
Bradford MM: A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976, 72: 248-254. 10.1006/abio.1976.9999.
Ozono R, Wang ZQ, Moore AF, Inagami T, Siragy HM, Carey RM: Expression of the subtype 2 angiotensin (AT2) receptor protein in rat kidney. Hypertension. 1997, 30: 1238-1246.
Okamura A, Rakugi H, Ohishi M, Yanagitani Y, Takiuchi S, Moriguchi K, Fennessy PA, Higaki J, Ogihara T: Upregulation of renin-angiotensin system during differentiation of monocytes to macrophages. J Hypertens. 1999, 17: 537-545. 10.1097/00004872-199917040-00012.
Macari D, Bottari S, Whitebread S, De Gasparo M, Levens N: Renal actions of the selective angiotensin AT2 receptor ligands CGP 42112B and PD 123319 in the sodium-depleted rat. Eur J Pharmacol. 1993, 249: 85-93. 10.1016/0014-2999(93)90665-5.
Macari D, Whitebread S, Cumin F, De Gasparo M, Levens N: Renal actions of the angiotensin AT2 receptor ligands CGP 42112 and PD 123319 after blockade of the renin-angiotensin system. Eur J Pharmacol. 1994, 259: 27-36. 10.1016/0014-2999(94)90153-8.
Snygg J, Aneman A, Pettersson A, Fandriks L: Jejunal mucosal nitric oxide production and substrate dependency during acute mesenteric hypoperfusion in pigs. Crit Care Med. 2000, 28: 2563-2566.
Lamarque D, Kiss J, Tankovic J, Flejou JF, Delchier JC, Whittle BJ: Induction of nitric oxide synthase in vivo and cell injury in rat duodenal epithelium by a water soluble extract of Helicobacter pylori. Br J Pharmacol. 1998, 123: 1073-1078.
Tsutsumi Y, Matsubara H, Masaki H, Kurihara H, Murasawa S, Takai S, Miyazaki M, Nozawa Y, Ozono R, Nakagawa K, Miwa T, Kawada N, Mori Y, Shibasaki Y, Tanaka Y, Fujiyama S, Koyama Y, Fujiyama A, Takahashi H, Iwasaka T: Angiotensin II type 2 receptor overexpression activates the vascular kinin system and causes vasodilation. J Clin Invest. 1999, 104: 925-935.
Siragy HM, Carey RM: Protective role of the angiotensin AT2 receptor in a renal wrap hypertension model. Hypertension. 1999, 33: 1237-1242.
Chin SY, Pandey KN, Shi SJ, Kobori H, Moreno C, Navar LG: Increased activity and expression of Ca(2+)-dependent NOS in renal cortex of ANG II-infused hypertensive rats. Am J Physiol. 1999, 277: F797-804.
Pueyo ME, Gonzalez W, Nicoletti A, Savoie F, Arnal JF, Michel JB: Angiotensin II stimulates endothelial vascular cell adhesion molecule-1 via nuclear factor-kappaB activation induced by intracellular oxidative stress. Arterioscler Thromb Vasc Biol. 2000, 20: 645-651.
Ruiz-Ortega M, Lorenzo O, Ruperez M, Blanco J, Egido J: Systemic infusion of angiotensin II into normal rats activates nuclear factor-kappaB and AP-1 in the kidney: role of AT(1) and AT(2) receptors. Am J Pathol. 2001, 158: 1743-1756.
Ruiz-Ortega M, Lorenzo O, Ruperez M, Suzuki Y, Egido J: Angiotensin II activates nuclear transcription factor-kappaB in aorta of normal rats and in vascular smooth muscle cells of AT1 knockout mice. Nephrol Dial Transplant. 2001, 16 (Suppl 1): 27-33.
Wang Y, Marsden PA: Nitric oxide synthases: biochemical and molecular regulation. Curr Opin Nephrol Hypertens. 1995, 4: 12-22.
Zhang X, Ruiz B, Correa P, Miller MJ: Cellular dissociation of NF-kappaB and inducible nitric oxide synthase in Helicobacter pylori infection. Free Radic Biol Med. 2000, 29: 730-735. 10.1016/S0891-5849(00)00375-0.
Dzau VJ: Theodore Cooper Lecture: Tissue angiotensin and pathobiology of vascular disease: a unifying hypothesis. Hypertension. 2001, 37: 1047-1052.
Wallace JL, Miller MJ: Nitric oxide in mucosal defense: a little goes a long way. Gastroenterology. 2000, 119: 512-520.
Acknowledgements
We thank Christina Ek for excellent laboratory assistance. This investigation was supported financially by the Swedish Medical Research Council (grant no: 8663), the Gothenburg Medical Society and the Knut & Alice Wallenberg foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
SE carried out animal experiments, molecular genetic and protein analysis, performed the statistical analysis and drafted the manuscript. ML, BJ, MH, and AA carried out animal experiments and participated in study design. LF concieved and coordinated the study and drafted the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ewert, S., Laesser, M., Johansson, B. et al. The angiotensin II receptor type 2 agonist CGP 42112A stimulates NO production in the porcine jejunal mucosa. BMC Pharmacol 3, 2 (2003). https://doi.org/10.1186/1471-2210-3-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2210-3-2