Abstract
Background
Extensive use of antibiotics as growth promoters in the livestock industry constitutes strong selection pressure for evolution and selection of antibiotic resistant bacterial strains. Unfortunately, the microbial ecology and spread of these bacteria in the agricultural, urban, and suburban environments are poorly understood. Insects such as house flies (Musca domestica) and German cockroaches (Blattella germanica) can move freely between animal waste and food and may play a significant role in the dissemination of antibiotic resistant bacteria within and between animal production farms and from farms to residential settings.
Results
Enterococci from the digestive tract of house flies (n = 162), and feces of German cockroaches (n = 83) and pigs (n = 119), collected from two commercial swine farms were isolated, quantified, identified, and screened for antibiotic resistance and virulence. The majority of samples (93.7%) were positive for enterococci with concentrations 4.2 ± 0.7 × 104 CFU/house fly, 5.5 ± 1.1 × 106 CFU/g of cockroach feces, and 3.2 ± 0.8 × 105 CFU/g of pig feces. Among all the identified isolates (n = 639) Enterococcus faecalis was the most common (55.5%), followed by E. hirae (24.9%), E. faecium (12.8%), and E. casseliflavus (6.7%). E. faecalis was most prevalent in house flies and cockroaches, and E. hirae was most common in pig feces. Our data showed that multi-drug (mainly tetracycline and erythromycin) resistant enterococci were common from all three sources and frequently carried antibiotic resistance genes including tet(M) and erm(B) and Tn916/1545 transposon family. E. faecalis frequently harbored virulence factors gelE, esp, and asa1. PFGE analysis of selected E. faecalis and E. faecium isolates demonstrated that cockroaches and house flies shared some of the same enterococcal clones that were detected in the swine manure indicating that insects acquired enterococci from swine manure.
Conclusions
This study shows that house flies and German cockroaches in the confined swine production environment likely serve as vectors and/or reservoirs of antibiotic resistant and potentially virulent enterococci and consequently may play an important role in animal and public health.
Similar content being viewed by others
Background
Antibiotic resistance is a serious public-health problem; reduced effectiveness of antibiotics results in greater patient mortality rates, prolonged hospitalization and increased healthcare costs. The economic impact of antibiotic resistance has been estimated between $5 and $24 billion annually in the United States alone [1]. Extensive use of antibiotics, especially as growth promoters, in the animal industry has resulted in strong selective pressure for the emergence of antibiotic-resistant bacteria in food animals [2–5]. In turn, animals and animal production environments have become reservoirs for antibiotic-resistant bacteria [6]. Many of these feed additive antibiotics are identical or related to those used in human medicine [7, 8]. The largest fraction of medically important antibiotics as feed additives in the USA is used in hogs (69%), compared to 19% in broiler chickens and 12% in beef cattle [9]. Antibiotic resistant bacteria are released into the environment in animal feces and can then spread to other ecological habitats, including humans [6, 10, 11]. A connection between antibiotic resistance in bacterial isolates from healthy food animals and clinical isolates of human and animal origins has been suggested; however, this is a controversial issue because the ecology of these bacteria and their genes in the agricultural and urban environment is not well understood [10, 12–16].
Insects associated with food animals, especially house flies (Musca domestica) and German cockroaches (Blattella germanica) are not only important nuisance pests but also potential vectors of animal and human pathogens [17, 18]. Organic waste in and around animal production facilities provide excellent habitats for the growth and development of these insects. Because of their habitat preferences, unrestricted movement, mode of feeding, and attraction to residential areas, house flies and cockroaches have a great potential to disseminate fecal bacteria, including human and animal pathogens and antibiotic resistant strains [17, 18]. With continuing urban expansion in agriculturally zoned areas in the last two decades, there is an increasing concern in the medical and public health community about insect pests directly associated with the spread of bacterial pathogens and antibiotic resistant microorganisms within animal production systems and to residential settings.
Enterococci are ubiquitous Gram-positive, lactic acid bacteria found in various habitats, including the intestinal tract of animals, from insects (102 to 104 CFU per house fly) to humans (104 to 106 CFU per gram of stool/feces), and environments contaminated by animal or human fecal material as well as in food and feed products derived from animals [19–25]. While some enterococci are used as probiotics, other Enterococcus species are important opportunistic and nosocomial pathogens of humans, causing urinary tract infections, bacteremia, intra-abdominal and pelvic infections, wound and tissue infections, and endocarditis [26]. The genus Enterococcus presently comprises over 30 species; however, E. faecalis and E. faecium are the two major species of clinical importance [20]. Enterococci are considered a reservoir of antibiotic resistance genes to a wide range of antibiotics (including beta-lactams and high concentration aminoglycosides) frequently used to treat infections of Gram-positive cocci. Enterococci have been implicated in dissemination of antibiotic resistance and virulence genes both intra- and interspecifically because of their ability to acquire and transfer antibiotic resistance through transfer of plasmids and transposons. In addition, enterococcal acquisition of vancomycin resistance leaves few options for therapeutic management [26–31]. Several studies have highlighted the importance of enterococci as a reservoir of antibiotic resistance genes in the environment [22, 26, 27, 32, 33]. However, little information is available about the role of insects in the ecology and dissemination of antibiotic resistant enterococci in the animal production environment and consequently in animal and public health.
The objective of this study was to determine the prevalence of antibiotic resistant and potentially virulent enterococci in house flies and German cockroaches collected from two commercial swine farms and to compare these to enterococci isolated from swine feces. This is the first comprehensive analysis of antibiotic resistance and virulence of enterococci associated with insect pests in swine farms, and it will enhance our understanding of the role of insects in the ecology of antibiotic resistant and virulent bacteria and in the public health and pre-harvest food safety and security.
Results
Prevalence, concentration, and diversity of enterococci
Enterococci from pig fecal samples (n = 119), German cockroaches fecal samples (n = 83), and digestive tract of house flies (n = 162), collected from two commercial swine farms, were isolated, quantified, identified, and screened for antibiotic resistance and virulence by a polyphasic approach (phenotypic and genotypic analysis). Enterococci were detected in 106 (89.1%) pig fecal samples, 78 (94.0%) cockroach fecal samples, and the digestive tracts of 159 (98.1%) house flies collected from swine farms. The concentration of enterococci (mean ± SEM) was 4.2 ± 0.7 × 104 CFU/house fly, 5.5 ± 1.1 × 106 CFU/g of cockroach feces, and 3.2 ± 0.8 × 105 CFU/g of pig feces. A total of 639 out of 932 (68.6%) enterococcal isolates from all sources (house flies, cockroaches, and pigs) were successfully identified by multiplex or single PCR to species level. The unidentified isolates (31.4%) were not included in the additional analysis in this study. Although differences in species prevalence varied by sources, E. faecalis was the common enterococcal species in all samples (55.5%), followed by E. hirae (24.9%), E. faecium (12.8%), E. casseliflavus (6.7%). The largest number of E. faecalis and E. casseliflavus isolates was detected in flies and cockroach feces and the highest number of E. faecium and E. hirae was found in pig feces (Figure 1). Concentration of E. faecalis from the digestive tract of house flies was significantly higher compared to that from feces of German cockroaches and pigs and E. hirae was significantly more prevalent in pig feces than in roach feces and house flies (Figure 1).
Prevalence and diversity of antibiotic resistance by phenotype and genotype
The prevalence of antibiotic resistance (expressed as percentages) within each Enterococcus spp. isolated from pig and cockroach feces and the digestive tract of house flies is shown in Figure 2. Among the isolates tested, no vancomycin resistance was observed and only a few isolates of E. faecalis and E. faecium were resistant to ampicillin. The majority of identified isolates from all samples showed high prevalence of tetracycline resistance (Tetr) followed by resistance to erythromycin (Eryr)) (Figure 2). High-level resistance to the aminoglycosides streptomycin and kanamycin was also detected in E. faecalis, E. faecium, E. hirae and E. casseliflavus from all samples (Figure 2). In general, the antibiotic resistance profiles of enterococci isolated from pig feces, cockroach feces, and the digestive tract of house flies were similar and no significant differences were observed within the same bacterial species (Figure 2). However, significant differences in resistance to ciprofloxacin and streptomycin were detected in E. faecalis (Figure 2A). Likewise, the incidence of ciprofloxacin resistance in E. faecium from the digestive tract of house flies was significantly higher compared to E. faecium from feces of German cockroaches and pigs (Figure 2B).
Phenotypic antibiotic resistance profiles (%) of (A) E. faecalis , (B) E. faecium , (C) E. hirae and (D) E. casseliflavus isolated from pig feces, German cockroach feces, and the digestive tract of house flies collected on two swine farms. AMP = ampicillin, VAN = vancomycin, TET = tetracycline, CHL = chloramphenicol, CIP = ciprofloxacin, ERY = erythromycin, STR = streptomycin, KAN = kanamycin.
The most common combination or resistance traits was Tetr and Eryr (E. faecalis, 65.8%; E. faecium, 52.0%; E. hirae, 34.5%; E. casseliflavus, 51.1%), followed by the combination of Tetr, Eryr, Strr, and Kanr (E. faecalis, 6.4%; E. faecium, 17.6%; E. hirae, 8.8%; E. casseliflavus, 17.0%). Further, the prevalence of the most common two-antibiotic-resistant isolates (Tetr and Eryr) was not significantly different in the feces of pigs and cockroaches and in the digestive tract of house flies (P = 0.0816). Similarly, no significant differences (P = 0.0596) in the prevalence of multiple-antibiotic-resistant isolates (Tetr, Eryr, Strr, and Kanr) were observed among all samples (pig feces, 11.9%; cockroach feces, 10.7%; house flies, 7.5%).
The prevalence of resistance genes (expressed as percentages) within each Enterococcus spp. is presented in Figure 3. The results revealed that the tet(M) and erm(B) determinants were widespread, tet(S), tet(O) and tet(K) were rare, and tet(A), tet(C), tet(Q) and tet(W) were not detected from the isolates tested based on our PCR approach. Irrespective of their origin, the majority of identified isolates contained the tet(M) determinant followed by the erm(B) determinant (Figure 3). Significant differences in prevalence of the tet(M) determinant were detected in enterococci isolated from pig and cockroach feces and the digestive tract of house flies (Figure 3). In contrast, the erm(B) determinant was equally prevalent in enterococci isolated from these three sources and no significant differences were observed within the same bacterial species (Figure 3).
The distribution and combination of resistance genes in phenotypically resistant enterococci are shown in Tables 1, 2, and Additional files 1-3). Many E. faecalis (93.4%), E. faecium (81.2%), and E. casseliflavus (90.9%) carried at least one resistance determinant. Among the isolates tested, the most common determinant was the ribosomal protection protein mechanism encoded by tet(M), alone or in combination with other determinants (Tables 1, 2, and Additional files 1-2). No significant differences were found in the prevalence of the tet(M) gene alone in E. faecium (P = 0.2837), E. hirae (P = 0.0823) and E. casseliflavus (P = 0.1223) isolated from pig feces, cockroach feces and the digestive tract of house flies (Tables 1, 2, and Additional file 1). The prevalence of tet(M) alone in E. casseliflavus from pig and cockroach feces was significantly higher (P = 0.0012) compared to that from digestive tracts of house flies (Additional file 2).
Multiple resistance determinants, specifically tet(M) and erm(B), were detected in E. faecalis, E. faecium, E. hirae, and E. casseliflavus (Tables 1, 2, Additional files 1-2). In general, the levels of prevalence of multiple resistance determinants tet(M) and erm(B) were similar and no significant differences were observed in E. faecalis (P = 0.4151), E. faecium (P = 0.0864), E. hirae (P = 0.5873) and E. casseliflavus (P = 0.5760) isolated from the digestive tract of house flies and feces of German cockroaches and pigs (Tables 1, 2, Additional files 1-2).
Since most of the tetracycline resistant isolates were also resistant to erythromycin, and the tet(M) gene is frequently linked with the erm(B) gene on the highly mobile conjugative transposon Tn1545, tests for the detection of int genes were also performed for the presence of conjugative transposons of the Tn1545/Tn916 family. The results revealed that the Tn1545/Tn916 conjugative transposon family was found in 219/639 (34.3%) identified isolates from all samples. The Tn1545/Tn916 family determinant was commonly detected in E. faecalis followed by E. hirae, E. casseliflavus, and E. faecium (Additional file 3). The most common E. faecalis genotypes based on a combination of antibiotic resistance and Tn1545/Tn916 family determinants were tet(M) plus erm(B) plus Tn916/1545 followed by tet(M) plus Tn916/1545 (Additional file 3). In addition, many (23.3%) E. faecalis isolates from pig feces also carried frequently resistance determinants including tet(M), tet(K) and erm(B) in combination with the Tn1545/Tn916 family (Additional file 3).
Prevalence and diversity of virulence factors by phenotype and genotype
The overall prevalence of putative virulence factors (gelatinase, haemolysin and aggregation substance production) for all identified isolates is listed in Figure 4. Gelatinase production on skimmed milk agar was the most common virulence factor among all identified isolates, with significantly higher incidence in E. faecalis than in E. casseliflavus, E. faecium, and E. hirae (Figure 4). No significant differences were detected in prevalence of gelatinase production among E. faecalis and E. faecium isolated from the digestive tract of house flies and feces of German cockroaches and pigs (Figure 4).
The prevalence of β-hemolysis on human blood agar in E. faecalis was higher than that observed in E. faecium, E. casseliflavus, and E. hirae (Figure 4). In general, the prevalence of β-hemolysis among identified enterococci isolated from pig feces, German cockroach feces and the digestive tract of house flies were similar and no significant differences were observed within the same species (Figure 4).
The clumping/aggregation assay revealed that the prevalence of the clumping phenotype among E. faecalis was low as only 6 of the 631 E. faecalis (1.95%) isolates aggregated in vitro. However, no significant differences were found in the prevalence of this virulence factor among E. faecalis isolated from pig feces, German cockroach feces and the digestive tract of house flies (Figure 4A).
PCR amplifications of enterococcal DNA with the specific primers for asa1, esp, cylA, and gelE revealed significantly higher prevalence of virulence determinants in E. faecalis than in other enterococcal species irrespective of the origin of the isolates (Figure 5). E. faecium and E. hirae isolates were generally without virulence determinants. No significant differences were detected in the prevalence of virulence determinants gelE and cylA among E. faecalis isolated from pig feces, German cockroach feces and the digestive tract of house flies (Figure 5A). However, the prevalence of asa1 and esp genes in E. faecalis from pig feces was significantly higher compared to E. faecalis from the digestive tract of house flies and feces of German cockroaches (Figure 5A).
Phenotypic tests showed that the 63.0% of E. faecalis that carried gelE were gelatinolytic. The test for detection of β-hemolysis in E. faecalis revealed there was a 100% (pig feces and cockroach feces) and 92.9% (house flies) correlation between cylA and β-hemolysis on human blood. In addition, 8.1% of the E. faecalis from house flies was β-hemolytic but negative for cylA.
Genotyping by pulsed-field gel electrophoresis (PFGE)
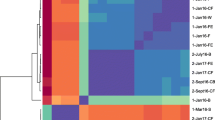
Genotyping of randomly selected E. faecalis and E. faecium isolated from swine manure, house flies, and German cockroaches from one of the farms revealed that insects and swine manure shared some of the same enterococcal clones. For example, the same genotype of E. faecalis was detected from the house fly (strain R1F-6-1) and swine manure (strains R1M-1-3, 1-6, 1-9, 4-2, 4-3) (Figure 6A). Another identical PFGE profile of E. faecalis was found in the German cockroach (R1C-13-1, 18-3, 20-3) and in the house fly (R1F-30-3) (Figure 6A). The same clone of E. faecium was detected in the German cockroach (R2C-12-3), in the house fly (R2F-4-6), and in swine manure (R2M-1-6, 3-4, 5-3, 6-1) (Figure 6B).
Dendrograms based on Apa I restriction pattern resolved by pulsed-field gel electrophoresis (PFGE) depicting the relationships of A) 27 E. faecalis strains and B) 19 E. faecium strains isolated from swine manure (SM), house flies (HF), and German cockroaches (GC) from one commercial swine farm. The scale indicates the level of pattern similarity.
Discussion
The worldwide increase in the emergence and spread of antibiotic resistance has become a major public health concern, with economic, social and political ramifications. Clearly, the prevalence of antibiotic resistant bacteria in the gastro-intestinal microbial communities of domestic food animals and their feces/manure has become high in the United States likely due to extensive use of antibiotics in food animal production [3, 6, 10, 34–36]. Although a connection between antibiotic resistance in bacterial isolates from healthy food animals and clinical isolates of human and animal origins has been suggested, this is a controversial issue because little is known about the amplification and spread of antibiotic resistant bacteria and genes in the environment [12–14, 16, 37–41].
The two groups of insects most frequently screened for food borne-pathogens are house flies and cockroaches. These insects have been implicated as mechanical or biological vectors for bacterial pathogens including Salmonella spp., Campylobacter spp; Pseudomonas aeruginosa, Listeria spp., Shigella spp., Aeromonas spp., Yersinia pseudotuberculosis, Escherichia coli O157:H7, and E. coli F18 that can cause diseases in humans and/or animals [17, 18]. Multi-antibiotic resistant enterococci have been reported from house flies collected from fast-food restaurants [19]. In addition, the horizontal transfer of tet(M) among E. faecalis in the house fly digestive tract as well as the great capacity of house flies to contaminate human food with enterococci have been demonstrated [42, 43]. Organic wastes in and around animal production facilities including swine farms provide excellent habitats for house flies and German cockroaches. Several features of house flies and cockroaches, including their dependence on live microbial communities, active dispersal ability and human-mediated transport, attraction to places where food is prepared and stored, developmental sites, and mode of feeding/digestion make these insects an important "delivery vehicle" for transport of bacteria including antibiotic resistant enterococci from reservoirs (animal manure), where they pose minimal hazard to people, to places where they pose substantial risk (food) [17, 18, 44]. Several reports showed a positive correlation between the incidence of food-borne diarrhea and the density of house fly or cockroach populations. For example, suppression of flies in military camps in the Persian Gulf resulted in an 85% decrease in Shigellosis and a 42% reduction in the incidence of other diarrheal disease [45]. Esrey [46] reported a 40% reduction in the incidence of diarrheal infections in children after suppression of a fly population. Another study showed that fly control could reduce trachoma and diarrhoea among children in Gambia [47]. An outbreak of gastro-enteritis caused by S. typhimurium in the children's ward of a Belgian hospital dropped as soon as the German cockroach infestation had been controlled [48]. Tarshis [49] recorded that control of cockroaches was accompanied by a decrease in the incidence of endemic infectious hepatitis. The German cockroach was also shown as a potential mechanical vector of the piglet pathogen Escherichia coli F18 [50].
To our knowledge, surveillance for resistance to antibiotics in enterococci from insects associated with swine production environments has not been previously conducted. Recently, Graham et al. [51] reported that flies may be involved in the transmission of drug resistant enterococci and staphylococci from confined poultry farms. In our study, enterococci were detected in the digestive tracts of house flies, cockroach fecal samples and pig fecal samples collected from two different swine farms with enterococci recovered from 93.7% of 364 samples analyzed. High concentrations of enterococci in the digestive tract of house flies and cockroaches suggest that enterococci are common commensals of these insects intestinal microbiota. Among the four most frequently identified species, E. faecalis and E. faecium are the most important enterococcal species from a clinical perspective [20, 22, 27]. However, infections caused by E. hirae and E. casseliflavus may also occur and warrant attention [52]. In addition, enterococci are regarded as important reservoirs of antibiotic resistance and virulence genes that are often found on mobile genetic elements [22, 27, 30, 52].
The most frequently encountered enterococcal species in the intestines of farm animals are E. faecalis, E. faecium, E. hirae, and E. durans; however, culture methods may influence the recovery and selection of enterococcal species [36, 53]. The dominance of E. hirae in pig feces in our study is consistent with studies of the enterococcal community of swine [32, 33]. E. faecalis was observed more frequently from the digestive tract of insects and these results are also in agreement with previous studies [19, 54]. The favorable conditions in the fly and cockroach digestive tract may serve to select and amplify environmentally acquired E. faecalis, including those carrying antibiotic resistance genes.
High frequency of resistance to tetracycline, erythromycin, streptomycin, kanamycin, and ciprofloxacin in our study likely reflects use of tetracyclines, macrolides, aminoglycosides and fluoroquinolones for swine in the USA [55]. Unfortunately, we were unable to obtain any specific information on the use of antibiotics in the two commercial farms in this study. Similar results were reported on antimicrobial resistant phenotypes and resistance genes in enterococci from animals and insects [10, 19, 51]. The patterns of antibiotic resistance observed in Enterococcus spp. recovered from the pig fecal samples were similar to those observed in isolates recovered from digestive tracts of house flies and cockroach fecal samples indicating that insects acquired enterococci from the pig manure. PFGE analysis of selected E. faecalis and E. faecium isolates confirmed that both insect species carried some of the same clones that were detected in the swine manure. This supports our data indicating that insects acquired the drug-resistant and potentially virulent enterococci from the swine feces although the opposite route cannot be ruled out. However, our previous study [56] showed that the prevalence of antibiotic resistant enterococci in house flies decreases with increasing distance from the likely source (cattle feedlot). This indicates that the source of antibiotic resistant enterococci in house flies and cockroaches in this study was the swine manure due to very high prevalence of antibiotic resistant enterococci in all three sources. The absence of VRE in this study is in agreement with previous findings and reflects a relationship between extensive use of specific antibiotics as growth promoters and presence of VRE [32, 35, 57]. Since avoparcin has not been used as a growth promoter in the United States, and VRE are rarely isolated from US food animal production environments. In contrast, VRE have been frequently isolated from food animal production environments in Europe where vancomycin was extensively used for farm animals [58].
Our findings are in agreement with the results of other studies which showed that tet(M) and erm(B) are the most widespread resistance genes among enterococci from food animals or foods [10, 15, 19, 24, 59, 60]. Furthermore, a strong association of the tet(M) and erm(B) genes with the conjugative transposon family Tn1545/Tn916 was also detected in many isolates in our study, indicating that antibiotic resistant enterococci associated with the confined swine environment could be a reservoir of transferable tetracycline and erythromycin resistance. The similar prevalence of resistance determinants and Tn1545/Tn916 transposons among isolates from pig feces, house flies and cockroach feces indicates exchange of resistant strains or their resistance genes. This is important because the Tn1545/Tn916 family has a very broad host range and members of this family of transposons can be transferred by conjugation to numerous bacterial species in the human gastrointestinal microbial community [61–63].
The highest incidence of multiple virulence factors was detected in E. faecalis with similar virulence profiles from the digestive tract of house flies, cockroach feces and pig feces. The gelE gene was detected frequently in E. faecalis (63.0%) and was the most common of the virulence factors. Prevalence of the gelE gene has been frequently documented in E. faecalis, and rarely in E. faecium and E. durans [12, 27]. The presence of gelE was, however, not strictly correlated with the phenotype suggesting that some gelE genes are silent which is likely due to a 23.9-kb chromosomal deletion involving the fsr locus that regulates gelE expression [64, 65]. We found little correlation between the clumping phenotype in vitro and the presence of the asa1 gene in E. faecalis showing that asa1 is not commonly expressed under these in vitro conditions. The phenotypic test for β-hemolysis (cytolysin production) with E. faecalis, E. faecium and E. casseliflavus showed a strong correlation between cylA and β-hemolysis on human blood. However, 8.1% of the E. faecalis from house flies were positive for β-hemolysis but negative for cylA, suggesting the presence of unknown determinant(s). Some of the genes encoding virulence determinants, including cytolysin and aggregation substance, are known to be present on pheromone-responsive plasmids, such as pAD1 and therefore transferable to other E. faecalis strains [27].
The data presented in this study offer evidence that should be helpful for future research initiatives aimed at reducing the dissemination of antibiotic resistant and virulent bacteria. It is likely that the high prevalence of resistant and potentially virulent enterococci in house flies and German cockroaches associated with confined swine environments reflects an extensive use of antibiotics by the swine industry. However, the degree to which these resistant and virulent enterococci hamper the efficacy of medically important antibiotics and thus pose risks to humans is unknown. The gastrointestinal tracts of mini-pigs, humans, and mice provide favorable environments for intra- and interspecies transfer of antibiotic resistance genes, but these processes have not been investigated in the digestive tract of insects and related arthropods with few exceptions [42, 66–71]. Knowing the sources of enterococci harboring in house flies and German cockroaches is also important to accurately assess risk, to identify and implement management plans for fecal waste, and to establish insect management practices that prevent the spread of antibiotic resistant strains and other potential human and animal pathogens. Further studies are warranted to pinpoint the potential sources of fecal contamination of insects, their subsequent contamination of food and feed, and for a detailed understanding gene transfer in the digestive tract of insects.
Conclusion
In summary, our study showed that multi-antibiotic resistant and potentially virulent enterococci are prevalent in confined swine production (in pig feces, house flies and German cockroaches). House flies and German cockroaches likely serve as vectors and/or reservoirs for antibiotic resistance and virulence genes in the confined swine production environment and consequently they present animal and public health risks. Therefore, effective management strategies aimed at reducing insect pest populations should be an important component of pre-harvest food safety efforts in the future, with increasing recognition of enterococci as human opportunistic pathogens.
Methods
Sample collection and isolation of enterococci
All samples were collected from two commercial farms, one in Duplin county, North Carolina and one in Ottawa county, Kansas. House flies (Musca domestica) were collected using a sweep net. Individual house flies were surface sterilized with sodium hypochlorite and ethanol [44], homogenized in 1 ml of phosphate buffered saline (PBS), serially diluted, and drop-plated onto modified Enterococcus agar (mENT, Becton Dickinson, MA, USA). German cockroaches (Blattella germanica) were collected by brushing them into sterile plastic bags. Cockroaches were randomly divided among sterile plastic petri dishes (20 per petri dish) and allowed to produce feces overnight at room temperature. Fecal material (10 mg) from each petri dish was aseptically collected and processed as below. Pig feces were aseptically collected in sterile 50 ml Falcon tubes. One gram of feces was suspended in 9 ml of PBS and vortexed. An aliquot of 1 ml from each suspension was serially diluted in PBS and drop-plated onto mENT agar. All inoculated mENT agar plates were incubated at 37°C for 48 h. Purple/red bacterial colonies with a morphology characteristic of enterococci were counted, and up to four presumptive enterococcal colonies per sample were sub-cultured on trypticase soy agar (TSA; Becton Dickinson, MA, USA) incubated at 37°C for 24 h. Presumptive enterococcal colonies were identified at the genus level with the esculin hydrolysis test using Enterococcossel broth (Becton Dickinson, MA, USA) incubated for 24 h at 44°C [72]. Isolates confirmed as enterococci were streaked on TSA and incubated for 24 h at 37°C and stored at 4°C for further analysis.
Enterococcal species identification
Species-level identification was performed using multiplex PCR for four common species: E. faecalis, E. faecium, E. casseliflavus and E. gallinarum and single PCR for E. hirae [73–75]. Control strains consisting of E. faecalis ATCC 19433, E. faecium ATCC 19434, E. gallinarum ATCC 49579, E. casseliflavus ATCC 25788, and E. hirae ATCC 8043 were included with each PCR assay. E. mundtii ATCC 43186 was used as negative control.
Phenotypic screening for antibiotic resistance and virulence factors
All identified isolates were tested for sensitivity to six antibiotics using standard disc diffusion method. Antibiotic discs of ampicillin (AMP, 15 μg/ml), vancomycin (VAN 30 μg/ml), tetracycline (TET, 30 μg/ml), chloramphenicol (CHL, 30 μg/ml), ciprofloxacin (CIP, 5 μg/ml), and erythromycin (ERY, 15 μg/ml) (all Oxoid) were used. High levels resistance to streptomycin (STR) and kanamycin (KAN) were assessed by the agar dilution technique using 2,000 μg/ml of streptomycin or kanamycin in brain heart infusion agar (Becton Dickinson, MA, USA). The protocols followed the guidelines of the National Committee for Clinical Laboratory Standards [76]. E. faecalis ATCC 19433, E. faecium ATCC 19434, E. gallinarum ATCC 49579 and E. casseliflavus ATCC 25788 were used as quality control strains.
Gelatinase activity was detected by streaking all identified isolates on TSA containing 1.5% (v/v) skim milk [27]. E. faecalis MMH594 was used as a positive control and E. faecalis FA2-2 as a negative control.
For detection of hemolytic activity, E. faecalis and E. faecium were streaked on Columbia agar base supplemented with 5% (v/v) fresh sterile human blood and grown for 24-48 h at 37°C. Isolates showing a complete clearance zone around the colonies indicated β-hemolysin production [27]. E. faecalis MMH594 was used as a positive control and E. faecalis FA2-2 as a negative control.
Production of aggregation substance was determined by the clumping assay [77]. E. faecalis OG1RF:pCF10 and JH2-2 were used as positive and negative controls, respectively.
Genotypic screening for antibiotic resistance, virulence and integrase genes
Multiplex or single PCR were used to screen all identified isolates for tetracycline and erythromycin resistance genes including, tet(S), tet(M), tet(O), tet(K), tet(A), tet(C), tet(Q), tet(W)] and erm(B) and for four putative virulence determinants gelE , cylA, esp, and asa1 [78–81]. Integrase gene (int) was used for detection of the conjugative transposon family Tn1545/Tn916 [19, 82]. To confirm the identity of our PCR products, one randomly selected PCR product for each resistance, virulence, and transposon determinant was purified with GFX PCR DNA and Gel Band Purification Kit (Amersham Bioscience, UK) and sequences were determined on an ABI 3700 DNA Analyzer at the K-State DNA Sequencing Facility using the same PCR primers. Sequences were analyzed for similarity to known sequences in the GenBank database using BLAST (Basic Local Alignment Search Tool) [83]. Manual sequence alignment was done with CodonCode Aligner (Version 1,3,4) (CodonCode Corporation, Dedham, MA) (data not shown).
Genotyping of selected isolates with pulsed-field gel electrophoresis (PFGE)
PFGE protocol of Amachawadi et al. [84] was used with minor modifications. Agarose plugs were digested with 40 U of ApaI (Promega, Madison, WI) for 4 h at 37°C. The digested plugs were run on to a 1% SeaKem Gold Agarose (Lonza, Rockland, MI) gel using CHEF Mapper (Bio-Rad, Hercules, CA) with initial pulse time for 1 s and final time for 20 s at 200 V for 21 h. Cluster analysis was performed with BioNumerics software (Applied Maths, Korrijk, Belgium) using the band-based Dice correlation coefficient and the unweighted pair group mathematical average algorithm (UPGMA).
Data analysis
Differences in the prevalence of antibiotic resistance and virulence factors (genotype and phenotype) among enterococcal isolates from pig feces, house flies and roach feces were analyzed using chi-square analysis of contingency tables and Fisher's exact test (α = 0.05). Species with zero prevalence of antibiotic resistance and virulence factors (genotype and phenotype) were not included in the analysis.
References
Hall BG: Predicting the evolution of antibiotic resistance genes. Nat Rev Microbiol. 2004, 2: 430-435. 10.1038/nrmicro888.
Cohen ML: Changing patterns of infectious disease. Nature. 2000, 406: 762-767. 10.1038/35021206.
Hardy B: The issue of antibiotic use in the livestock industry: What have we learned?. Animal Biotechnology, Proceedings of the Conference on Antibiotics Use in Animal Agriculture. 2002, 13: 129-147.
Levy SB: Factors impacting on the problem of antibiotic resistance. J Antimicrob Chemother. 2002, 49: 25-30. 10.1093/jac/49.1.25.
Kummerer K: Resistance in the environment. J Antimicrob Chemother. 2004, 54: 311-320. 10.1093/jac/dkh325.
Aarestrup FM: The origin, evolution, and local and global dissemination of antimicrobial resistance. Antimicrobial resistance in bacteria of animal origin. Edited by: Aarestrup FM. 2006, Washington DC, ASM Press, 339-360.
Mellon M, Benbrook C, Benbrook KL: Hogging It: Estimates of Antimicrobial Abuse in Livestock. Union of Concerned Scientists. 2000, Cambridge MA, [http://www.ucsusa.org/assets/documents/food_and_agriculture/hog_front.pdf]
Guardabassi L, Courvalin P: Modes of antimicrobial action and mechanisms of bacterial resistance. Antimicrobial Resistance in Bacteria of Animal Origin. Edited by: Aarestrup FM. 2006, Washington D.C., ASM Press, 1-18.
Florini K, Denison R, Stiffler T, Fitzerald T, Goldburg R: Resistant bugs and antibiotic drugs: State and County estimates of antibiotics in animal feed and animal waste. 2005, [http://www.environmentaldefense.org/documents/4301_AgEstimates.pdf]
Aarestrup FM, Agersø Y, Smith PG, Madsen M, Jensen LB: Comparison of antimicrobial resistance phenotypes and resistance genes in Enterococcus faecalis and Enterococcus faecium from humans in the community, broilers and pigs in Denmark. Diagn Microbiol Infect Dis. 2000, 37: 127-137. 10.1016/S0732-8893(00)00130-9.
Garcia-Migura L, Pleydell E, Barnes S, Davies RH, Liebana E: Characterization of vancomycin-resistant Enterococcus faecium isolates from broiler poultry and pig farms in England and Wales. J Clin Microbiol. 2005, 43: 3283-3289. 10.1128/JCM.43.7.3283-3289.2005.
Eaton TJ, Gasson MJ: Molecular screening of enterococcus virulence determinants and potential for genetic exchange between food and medical isolates. Appl Environ Microbiol. 2001, 67: 1628-1635. 10.1128/AEM.67.4.1628-1635.2001.
Smith DL, Harris AD, Johnson JA, Silbergeld EK, Morris JG: Animal antibiotic use has an early but important impact on the emergence of antibiotic resistance in human commensal bacteria. Proc Natl Acad Sci USA. 2002, 99: 6434-6439. 10.1073/pnas.082188899.
Iversen A, Kühn I, Rahman M, Franklin A, Burman LG, Ollson-Liljequist B, Torrel E, Möllby R: Evidence for transmission between humans and the environment of nosocomial strain of Enterococcus faecium. Environ Microbiol. 2004, 6: 55-59. 10.1046/j.1462-2920.2003.00534.x.
De Leener E, Martel A, Decostere A, Haesebrouck F: Distribution of the erm(B) gene, tetracycline resistance genes, and Tn1545-like transposons in macrolide- and lincosamide-resistant enterococci from pigs and humans. Microb Drug Resist. 2004, 10: 341-345. 10.1089/mdr.2004.10.341.
Heuer OE, Hammerum AM, Collignon P, Wegener HC: Human health hazard from antimicrobial-resistant enterococci in animals and food. Clin Inf Dis. 2006, 43: 911-916. 10.1086/507534.
Graczyk TK, Knight R, Gilman R, Cranfield M: The role of non-biting flies in the epidemiology of human infectious diseases. Microbes Infect. 2001, 3: 231-235. 10.1016/S1286-4579(01)01371-5.
Zurek L, Gorham JR: Insects as vectors of foodborne pathogens. Wiley Handbook of Science and Technology for Homeland Security. Edited by: Voeller JG. Hoboken, N.J. 2008, John Wiley and Sons, 1-16.
Macovei L, Zurek L: Ecology of antibiotic resistance genes: characterization of enterococci from houseflies collected in food settings. Appl Environ Microbiol. 2006, 72: 4028-4035. 10.1128/AEM.00034-06.
Willems RJL, van Schalk W: Transition of Enterococcus faecium from commensal organism to nosicomial pathogen. Future Microbiol. 2009, 4: 1125-1135. 10.2217/fmb.09.82.
Franz CAMP, Holzapfel WH, Stiles ME: Enterococci at the crossroads of food safety?. Int J Food Microb. 1999, 47: 1-24. 10.1016/S0168-1605(99)00007-0.
Klein G: Taxonomy, ecology and antibiotic resistance of enterococci from food and the gastro-intestinal tract. Int J Food Microbiol. 2003, 88: 123-131. 10.1016/S0168-1605(03)00175-2.
Hayes JR, Enghish LL, Carter PJ, Proescholt T, Lee KY, Wagner DD, White DG: Prevalence and antimicrobial resistance of Enterococcus species isolated from retail meats. Appl Environ Microbiol. 2003, 69: 7153-7160. 10.1128/AEM.69.12.7153-7160.2003.
Macovei L, Zurek L: Influx of enterococci and associated antibiotic resistance and virulence genes from ready-to-eat food to the human digestive tract. Appl Environ Microbiol. 2007, 73: 6740-6747. 10.1128/AEM.01444-07.
Macovei L, Ghosh A, Thomas V, Hancock L, Mahmood S, Zurek L: Enterococcus faecalis with the gelatinase phenotype regulated by the fsr-operon and with biofilm forming capacity are common in the agricultural environment. Environ Microbiol. 2009, 11: 154-1547. 10.1111/j.1462-2920.2009.01881.x.
Kayser FH: Safety aspects of enterococci from the medical point of view. Int J Food Microbiol. 2003, 88: 255-262. 10.1016/S0168-1605(03)00188-0.
Gilmore MS, Coburn S, Nallapareddy SR, Murray BE: Enterococcal virulence. The Enterococci: Pathogenesis, Molecular Biology, and Antibiotic Resistance. Edited by: Gilmore MS. 2002, Washington DC, ASM Press, 301-354.
Klare I, Konstabel C, Badstubner D, Werner G, Witte W: Occurrence and spread of antibiotic resistances in Enterococcus faecium. Int J Food Microbiol. 2003, 88: 269-290. 10.1016/S0168-1605(03)00190-9.
Weigel LM, Clewell DB, Gill SR, Clark NC, McDougal JK, Flannagan SE, Kolonay JF, Shetty J, Killgore GE, Tenover FC: Genetic analysis of a high-level vancomycin resistant isolate of Staphylococcus aureus. Science. 2003, 302: 1569-1571. 10.1126/science.1090956.
Nallapareddy SR, Wenxiang H, Weinstock GM, Murray E: Molecular characterization of a widespread, pathogenic, and antibiotic resistance receptive Enterococcus faecalis lineage and dissemination of its putative pathogenicity island. J Bacterial. 2005, 187: 5709-5718. 10.1128/JB.187.16.5709-5718.2005.
Mundy LM, Sahm DF, Gilmore MS: Relationship between enterococcal virulence and antimicrobial resistance. Clin Microbiol Rev. 2000, 13: 513-522. 10.1128/CMR.13.4.513-522.2000.
Knudtson JM, Hartman PA: Antibiotic resistance among enterococcal isolates from environmental and clinical sources. J Food Prot. 1993, 56: 489-492.
Kühn I, Iversen A, Burman LG, Olsson-Liljequist B, Franklin A, Finn M, Aarestrup F, Seyfarth AM, Franklin A, Finn M, Blanch AR, Vilanova X, Taylor H, Caplin J, Moreno MA, Dominguez L, Herrero IA, Möllby R: Comparison of enterococcal populations in animals, humans, and the environment - A European study. Inter J Food Microbiol. 2003, 88: 133-145.
Nikolich MP, Hong G, Shoemaker NB, Salyers AA: Evidence for natural horizontal transfer of tetQ between bacteria that normally colonize humans and bacteria that normally colonize livestock. Appl Environ Microbiol. 1994, 60: 3255-3260.
Thal LA, Chow JW, Mahayni R, Bonilla H, Perri MB, Donabedian SA, Silverman J, Taber S, Zervos MJ: Characterization of antimicrobial resistance in enterococci of animal origin. Antimicrob Agents Chemother. 1995, 39: 2112-2115.
Aarestrup FM, Butaye P, Witte W: Non-human reservoirs of enterococci. The Enterococci: Pathogenesis, Molecular Biology, and Antibiotic Resistance. Edited by: Gilmore MS. 2002, Washington DC, ASM Press, 55-99.
Silbergeld EK, Graham J, Price LB: Industrial food animal production, antimicrobial resistance, and human health. Annu Rev. Public Health. 2008, 29: 151-169. 10.1146/annurev.publhealth.29.020907.090904.
Phillips I, Casewell M, Cox T, De Groot B, Friis C, Jones R, Nightingale C, Preston R, Waddell J: Antibiotic use in animals. J Antimicrob Chemother. 2004, 53: 885-10.1093/jac/dkh149.
Phillips I, Casewell M, Cox T, De Groot B, Friis C, Jones R, Nightingale C, Preston R, Waddell J: Does the use of antibiotics in food animals pose a risk to human health? A critical review of published data. J Antimicrob Chemother. 2004, 53: 28-52. 10.1093/jac/dkg483.
Phillips I, Casewell M, Cox T, De Groot B, Friis C, Jones R, Nightingale C, Preston R, Waddell J: Does the use of antibiotics in food animals pose a risk to human health? A reply to critics. J Antimicrob Chemother. 2004, 54: 276-278. 10.1093/jac/dkh262.
Turnidge J: Antibiotic use in animals--prejudices, perceptions and realities. J Antimicrob Chemother. 2004, 53: 26-27. 10.1093/jac/dkg493.
Akhtar M, Hirt H, Zurek L: Horizontal transfer of the tetracycline resistance gene tetM mediated by pCF10 among Enterococcus faecalis in the house fly (Musca domestica L.) alimentary canal. Microb Ecol. 2009, 58: 509-518. 10.1007/s00248-009-9533-9.
Macovei L, Miles B, Zurek L: The potential of house flies to contaminate ready-to-eat food with antibiotic resistant enterococci. J Food Protect. 2008, 71: 432-439.
Zurek L, Schal C, Watson DW: Diversity and contribution of the gastrointestinal bacterial community to the development of Musca domestica (Diptera: Muscidae) larvae. J Med Entomol. 2000, 37: 924-928. 10.1603/0022-2585-37.6.924.
Cohen D, Green M, Block C, Slepon R, Ambar R, Wasserman S, Levine MM: Reduction of transmission of shigellosis by control of houseflies (Musca domestica). Lancet. 1991, 337: 993-997. 10.1016/0140-6736(91)92657-N.
Esrey SA: Effects of improved water supply and sanitation on ascariasis, diarrhoea, dracunculiasis, hookworm infection, schistosomiasis and trachoma. Bulletin of World Health Organisation. 1991, 69: 609-621.
Emerson PM, Lindsay SW, Walraven GEL, Faal H, Bogh C, Lowe K: Effect of fly control on trachoma and diarrhoea. Lancet. 1999, 353: 1401-1403. 10.1016/S0140-6736(98)09158-2.
Graffar M, Mertens S: Le role des blattes dans la transmission des salmonelloses. Ann Inst Past. 1950, 79: 654-660.
Tarshis IB: The cockroach - A new suspect in the spread of infectious hepatitis. Am J Trop Med Hyg. 1962, 11: 705-711.
Zurek L, Schal C: Evaluation of the German cockroach (Blattella germanica) as a vector for verotoxigenic Escherichia coli F18 in confined swine production. Vet Microbiol. 2004, 101: 263-267. 10.1016/j.vetmic.2004.04.011.
Graham JP, Price LB, Evans SL, Graczyk TK, Silbergeld EK: Antibiotic resistant Enterococci and staphylococci isolated from flies collected near confined feeding operations. Sci Tot Environ. 2009, 407: 2701-2710. 10.1016/j.scitotenv.2008.11.056.
Murray BE: The life and times of the Enterococcus. Clin Microbiol Rev. 1990, 3: 46-65.
Butaye P, Devriese LA, Goosens H, Leven M, Haesebrousk F: Enterococci with acquired vancomycin resistance in pigs and chickens of different age groups. Antimicrob Agents Chemother. 1999, 43: 365-366.
Martin JD, Mundt JO: Enterococci in insects. Appl Microbiol. 1972, 24: 575-580.
FDA (U.S. Food and Drug Administration): FDA Approved Animal Drug Products (Green Book). 2004, Blacksburg, VA Drug Information Laboratory Virginia/Maryland Regional College of Veterinary Medicine
Chakrabarti S, Kambhaampati Zurek L: Assessment of house fly dispersal between rural and urban habitats in Kansas, USA. J Kans Entomol Soc. 2010, 83: 172-188. 10.2317/JKES0809.15.1.
Coque TM, Tomayko JF, Ricke SC, Okhyusen PC, Murray BE: Vancomycin-resistant enterococci from nosocomial, community and animal sources in the United States. Antimicrob Agents Chemother. 1996, 40: 2605-2609.
Van den Bogaard AE, Stobberingh EE: Epidemiology of resistance to antibiotics: Links between animals and humans. Int J Antimicrb Agents. 2000, 14: 327-335. 10.1016/S0924-8579(00)00145-X.
Jensen LB, Frimodt-Moller N, Aarestrup FM: Presence of erm gene classes in gram-positive bacteria of animal and human origin in Denmark. FEMS Microbiol Lett. 1999, 170: 151-158. 10.1111/j.1574-6968.1999.tb13368.x.
Teuber M, Meile L, Schwarz F: Acquired antibiotic resistance in lactic acid bacteria from food. Antonie van Leeuwenhoek. 1999, 76: 115-137. 10.1023/A:1002035622988.
Bertram J, Stratz M, Durre P: Natural transfer of conjugative transposon Tn916 between Gram-positive and Gram-negative bacteria. J Bacteriol. 1991, 173: 443-448.
Roberts MC: Resistance to tetracycline, macrolide-lincosamidestreptogramin, trimethoprim and sulfonamide drug classes. Mol Biotechnol. 2002, 20: 261-283. 10.1385/MB:20:3:261.
Roberts MC: Update on acquired tetracycline resistance genes. FEMS Microbiol Lett. 2005, 245: 195-203. 10.1016/j.femsle.2005.02.034.
Nakayama J, Kariyama R, Kumon H: Description of a 23.9-kilobase chromosomal deletion containing a region encoding fsr genes which mainly determines the gelatinase-negative phenotype of clinical isolates of Enterococcus faecalis in urine. Appl Environ Microbiol. 2002, 68: 3152-3155. 10.1128/AEM.68.6.3152-3155.2002.
Roberts JC, Singh KV, Okhuysen PC, Murray BE: Molecular epidemiology of the fsr locus and of gelatinase production among different subsets of Enterococcus faecalis isolates. J Clin Microbiol. 2004, 42: 2317-2320. 10.1128/JCM.42.5.2317-2320.2004.
Licht TR, Laugesen D, Jensen LB, Jacobsen BL: Transfer of the pheromone-inducible plasmid pCF10 among Enterococcus faecalis microorganisms colonizing the intestine of mini-pigs. Appl Environ Microbiol. 2002, 68: 187-193. 10.1128/AEM.68.1.187-193.2002.
Lester CH, Frimodt-Møller N, Sørensen TL, Monnet DL, Hammerum AM: In vivo transfer of the vanA resistance gene from an Enterococcus faecium isolate of animal origin to an E. faecium isolate of human origin in the intestines of human volunteers. Antimicrob Agents Chemother. 2005, 50: 596-599. 10.1128/AAC.50.2.596-599.2006.
Shoemaker NB, Vlamakis H, Hayes K, Salyers AA: Evidence for extensive resistance gene transfer among Bacteroides spp. and among Bacteroides and other genera in the human colon. Appl Environ Microbiol. 2001, 67: 561-568. 10.1128/AEM.67.2.561-568.2001.
Acheson DWK, Linciome LL, Jacewicz MS, Keusch GT: Shiga toxin interaction with intestinal epithelial cells. Escherichia coli 0157: H7 and other shiga-toxin producing E. coli strains. Edited by: Kaper JB, O'Brien AD. 1998, Washington DC, ASM Press, 140-147.
Mater DDG, Langella P, Corthier G, Flores MJ: Evidence of vancomycin resistance gene transfer between enterococci of human origin in the gut of mice harbouring human microbiota. J Antimicrob Chemother. 2005, 56: 975-978. 10.1093/jac/dki336.
Petridis M, Bagdasarian M, Waldor MK, Walker E: Horizontal transfer of shiga toxin and antibiotic resistance genes among Escherichia coli strains on house fly (Diptera; Muscidae) gut. J Med Entomol. 2006, 43: 288-295. 10.1603/0022-2585(2006)043[0288:HTOSTA]2.0.CO;2.
Devriese LA, Van de Kerckhove A, Kilpper-Balz R, Schleifer KH: Characterization and identification of Enterococcus species isolated from the intestines of animals. Int J Syst Bacteriol. 1987, 37: 257-259. 10.1099/00207713-37-3-257.
Dutka-Malen S, Evers S, Courvalin P: Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant enterococci by PCR. J Clin Microbiol. 1995, 33: 24-27.
Kariyama R, Mitsuhata R, Chow JW, Clewell JB, Kumon H: Simple and reliable multiplex PCR assay for surveillance isolates of vancomycin-resistant enterococci. J Clin Microbiol. 2000, 38: 3092-3095.
Arias CA, Robredo B, Singh KV, Torres C, Panesso D, Murray BE: Rapid identification of Enterococcus hirae and Enterococcus durans by PCR and detection of a homologue of the E. hirae muramidase-2 gene in E. durans. J Clin Microbiol. 2006, 44: 1567-1570. 10.1128/JCM.44.4.1567-1570.2006.
National Committee for Clinical Laboratory Standards: Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria. 2002, National Committee for Clinical Laboratory Standards, Wayne,PA
Dunny GM, Craig R, Carron R, Clewell DB: Plasmid transfer in Streptococcus faecalis: production of multiple sex pheromones by recipients. Plasmid. 1978, 2: 454-465. 10.1016/0147-619X(79)90029-5.
Ng LK, Martin I, Alfa M, Mulvey M: Multiplex PCR for the detection of tetracycline resistant genes. Mol Cell Probes. 2001, 15: 209-215. 10.1006/mcpr.2001.0363.
Villedieu A, Diaz-Torres ML, Hunt N, McNab R, Spratt DA, Wilson M, Mullany P: Prevalence of tetracycline resistance genes in oral bacteria. Antimicrob Agents Chemother. 2003, 47: 878-882. 10.1128/AAC.47.3.878-882.2003.
Sutcliffe J, Grebe T, Tait-Kamradt A, Wondrack L: Detection of erythromycin resistant determinants by PCR. Antimicrob Agents Chemother. 1996, 40: 2562-2566.
Vankerckhoven V, Van Autgaerden T, Vael C, Lammens C, Chapelle S, Rossi R, Jabes D, Goossens H: Development of a multiplex PCR for the detection of asa1, gelE, cylA, esp, and hyl genes in enterococci and survey for virulence determinants among European hospital isolates of Enterococcus faecium. J Clin Microbiol. 2004, 42: 4473-4479. 10.1128/JCM.42.10.4473-4479.2004.
Rice LB: Tn916 family conjugative transposons and dissemination of antimicrobial resistance determinants. Antimicrob Agents Chemother. 1998, 42: 1871-1877.
Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ: Basic local alignment search tool. J Mol Biol. 1990, 215: 403-410.
Amachawadi RG, Shelton NW, Jacob ME, Shi X, Narayanan S, Zurek L, Dritz SS, Nelssen JL, Tokach MD, Nagaraja TG: Occurrence of tcrB, a transferable copper resistance gene, in fecal enterococci of swine. Food Path Dis. 2010, 7: 1089-1097. 10.1089/fpd.2010.0540.
Acknowledgements
We thank Rick Santangelo (NCSU) and Jan Metlevski (KSU) for collecting the samples. This project was supported by the USDA-Risk Avoidance and Mitigation Program, #2005-51101-02388 to LZ and CS, and the Blanton J. Whitmire endowment at North Carolina State University (CS). This is contribution no. 11-121-J of the Kansas Agricultural Experiment Station.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
LZ and CS designed the study. AA and AG performed the analysis. AA, CS, AG, and LZ wrote the manuscript. All authors approved the final manuscript.
Electronic supplementary material
12866_2010_1310_MOESM1_ESM.DOCX
Additional file 1: Distribution of tet (M), tet (S), tet (K) and erm (B) determinants in E. hirae isolates from pig feces ( n = 93), German cockroach feces ( n = 30) and house fly digestive tracts ( n = 26). Table describing distribution of tet and erm genes in E. hirae from various sources and their correlation with the phenotype. (DOCX 11 KB)
12866_2010_1310_MOESM2_ESM.DOCX
Additional file 2: Distribution of tet (M), tet (S) and erm (B) determinants in E. casseliflavus isolates from pig feces ( n = 10), German cockroach feces ( n = 14) and house fly digestive tracts ( n =23). Table describing distribution of tet and erm genes in E. casseliflavus from various sources and their correlation with the phenotype. (DOCX 12 KB)
12866_2010_1310_MOESM3_ESM.DOCX
Additional file 3: Distribution [number (%) of isolates] of the tetracycline resistance genes, erm (B) gene, and Tn 916 / 1545 family among isolates from pig feces, cockroach feces and the digestive tract of house flies. Table describing combinations of antibiotic resistance determinants and transposon Tn916/1545 family in four Enterococcus species isolated from various sources. (DOCX 15 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ahmad, A., Ghosh, A., Schal, C. et al. Insects in confined swine operations carry a large antibiotic resistant and potentially virulent enterococcal community. BMC Microbiol 11, 23 (2011). https://doi.org/10.1186/1471-2180-11-23
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2180-11-23