Abstract
Background
Leukotriene B4 (LTB4) is a potent inflammatory mediator that also stimulates the immune response. In addition, it promotes polymorphonuclear leukocyte phagocytosis, chemotaxis, chemokinesis and modulates cytokines release. Regarding chemical instability of the leukotriene molecule, in the present study we assessed the immunomodulatory activities conferred by LTB4 released from microspheres (MS). A previous oil-in-water emulsion solvent extraction-evaporation method was chosen to prepare LTB4-loaded MS.
Results
In the mice cremasteric microcirculation, intraescrotal injection of 0.1 ml of LTB4-loaded MS provoked significant increases in leukocyte rolling flux, adhesion and emigration besides significant decreases in the leukocyte rolling velocity. LTB4-loaded MS also increase peroxisome proliferator-activated receptor-α (PPARα) expression by murine peritoneal macrophages and stimulate them to generate nitrite levels. Monocyte chemoattractant protein-1 (MCP-1) and nitric oxide (NO) productions were also increased when human umbilical vein and artery endothelial cells (HUVECs and HUAECs, respectively) were stimulated with LTB4-loaded MS.
Conclusion
LTB4-loaded MS preserve the biological activity of the encapsulated mediator indicating their use as a new strategy to modulate cell activation, especially in the innate immune response.
Similar content being viewed by others
Background
Leukotriene B4 (LTB4), a 5-lipoxygenase (5-LO)-derived eicosanoid acts as a potent chemoattractant for polymorphonuclear neutrophils (PMNs) [1], eosinophils [2] and effector T cells [3]. In addition to its direct impact on leukocyte effector functions, leukotrienes also promote innate immune responses indirectly by stimulating the production of other inflammatory mediators [4, 5], inducing phagocytosis [6] and activating antimicrobial mechanisms [7, 8]. Recent studies in animal models have shown that endogenous leukotrienes display protective effect against infectious diseases, including bacterial peritonitis [9], fungal pneumonia [4] and infections caused by helminths [5]. LTB4 binds to and activates its high-affinity receptor BLT1, which can be localized on neutrophils, eosinophils, monocytes [10] and T cells [11]. Other specific receptors for LTB4 are the so-called peroxisome proliferator-activated receptors (PPARs), which are situated in the cell nucleus. PPARs have been reported to regulate inflammatory responses, both in vivo and in vitro. In this context, PPARα activation by LTB4 binding affects the duration of the inflammatory response induced by this eicosanoid [12].
Regarding leukocyte recruitment, chemoattractants bind to their receptors on leukocytes, thereby converting rolling to firm adhesion via rapid integrin activation and/or up-regulation [13, 14]. Flow cytometry studies have demonstrated that LTB4 triggers the up-regulation of β2-integrins on neutrophil and monocyte surface [15, 16]. Several studies have suggested that lipoxygenase-triggered leukocyte adhesion might actually be due in large part to direct effects on human endothelial cells, although the relevant adhesive mechanisms have yet to be characterized [17–19]. Thus, the mechanisms by which LTB4 contributes to leukocyte activation and recruitment are not clearly defined.
On the other hand, previous studies have reported that LPS, TNF-α, IL-1β and LTB4 itself, differentially increase the expression of BLT1 and/or BLT2 receptors on HUVECs [20]. In addition, in human coronary artery, LTB4 also induces two important physiological responses, chemotaxis and proliferation [21]. Moreover, as demonstrated by intravital microscopy studies, LTB4 was very active in the microcirculation and promoted the adhesion of leukocytes to the endothelium, followed by diapedesis and migration into tissue [3]. Although it has been reported that LTB4 can induce CD54 (ICAM-1) expression in endothelial cells [22, 23], the prevailing notion is that adhesive and migratory effects of this mediator are primarily originated from its action on the leukocyte, where chemoattractants induce up-regulation of cell-adhesion molecules that can interact with their cognate receptors on endothelial cells [24, 25].
The aim of this study was to assess the activity of encapsulated LTB4 during in vitro and in vivo assays. In this regard, different studies have shown that systems that control antigen release can increase specific immunity by selectively driving an antigen or gene vector to immune effectors cells [26]. Based on the successful encapsulation of the LTB4 molecule [27] the proposed formulation can be employed on its own or combined with other therapies for the treatment of inflammatory diseases since LTB4 can act as immunomodulator during the inflammatory response. Other applications for this technology include the use of biodegradable polymer systems, which allow the sustained and controlled release of the encapsulated substances [28, 29]. Therefore, in this study, we have evaluated the effect of LTB4-loaded microspheres (MS) on leukocyte-endothelial cell interactions in the murine cremasteric microcirculation. In addition, we have also investigated the effect of LTB4 released from microspheres in inducing MCP-1 release and nitrites production by mouse peritoneal macrophages, HUVECs and HUAECs. Moreover, in order to elucidate different mechanisms of cell activation after LTB4-loaded MS engulfment we assessed PPARα expression under the effect of the mediator released inside the cell, exclusively.
Methods
Materials
For the purposes of this study, the LTB4 solution, LPS of E. coli (serotype 0127:B8), polyvinyl alcohol, tribromoethanol and Griess reagent mixtures were obtained from Sigma Chemical Co. (St. Louis, MO, USA). Poly-lactic coglycolic acid (PLGA) polymer (50:50) was obtained from Boehringer Ingelheim (Ingelheim, Germany). Methanol, methylene dichloride, acetonitrile and acetic acid (high-performance liquid chromatography grade) were purchased from Merck (Dietikon, Switzerland). Endothelial basal medium (EBM)-2 supplemented with endothelial growth media (EGM)-2 were from Clonetics, Barcelona, Spain. The chemokine and the antibody pair for human human MCP-1 ELISA was from R&D Systems, Madrid, Spain. Neutravidin-horseradish peroxidase was from Perbio Science, Cheshire, UK. K-Blue substrate was from Neogen, Lexington, KY. The specific BLT1 receptor antagonist CP-105,696 was a kind gift from Pfizer, Inc. (Indianapolis, IN, USA).
Ethical approval
Intravital microscopy studies with C57BL/6J mice from Charles River, weighting 23–30 g were approved by the Institutional Animal Care and Use Committee of the Faculty of Medicine, University of Valencia (Spain) and were conducted humanely.
Six- to eight-week old 5-LO-/- (129-Alox5tm1Fun) and strain-matched wild-type (WT) male sv129 mice were obtained from Jackson Laboratories, and were bred in the Faculdade de Ciências Farmacêuticas de Ribeirão Preto, Universidade de São Paulo, Brasil. All experiments were approved and conducted in accordance with the guidelines of the Animal Care Committee of the University of São Paulo, Brazil. Mice were maintained under standard laboratory conditions.
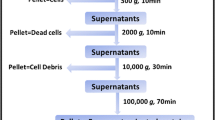
Preparation and characterization of the microspheres
Microspheres (MS) (diameters between 5 and 6 μm) containing LTB4 were prepared using an oil-in-water emulsion solvent extraction-evaporation process [27]. In brief, 0.3 ml internal organic phase (LTB4 3 × 10-5 M, dissolved in ethanol) was added to 10 ml of methylene dichloride containing 30 mg of PLGA 50:50. This phase was poured into an external aqueous phase (40 ml of polyvinyl alcohol solution at 3% w/v) and stirred mechanically (RW20; IKA Labortechnik, Staufen, Germany) at 600 rpm for 4 h to extract the organic solvent. Finally, the microspheres formed were washed three times with doubly distilled water and then freeze-dried. All the assays were conducted with previously characterized microspheres.
Administration of the microspheres in the mouse lungs
5-LO-/- mice were anesthetized with 2.5% tribromoethanol and restrained on a small board. An anterior midline incision was made for trachea exposition. A 30-gauge needle attached to a tuberculin syringe was inserted into the trachea, and intratracheal (i.t.) dispersion was used to introduce 0.1 ml of PBS, LTB4 in solution (3 × 10-8 M), unloaded and LTB4-loaded MS (5 × 10-7 M or 160 ng/ml) into the lungs. PBS was the vehicle for all administrations.
Histology
For representative histological sections that could show leukocyte infiltration in the lung parenchyma, lungs were removed on day 7 after the stimuli administrations. Then, the tissues were fixed in 10% formalin and embedded in paraffin blocks. Lung sections (5 μm) are representative of three experiments with 5-LO-/- mice (5 animals each group) and were stained with hematoxylin and eosin (HE). Analysis of the sections was performed in a "blinded" manner.
Intravital microscopy
The mouse cremaster preparation used in this study was similar to that described previously [30]. Mice were anesthetized by i.p. injection with a mixture of xylazine hydrochloride (10 mg/kg) and ketamine hydrochloride (200 mg/kg). A polyethylene catheter was placed in the jugular vein to permit the intravenous administration of additional anesthetic. The cremaster muscle was dissected free of tissues and exteriorized onto an optical clear viewing pedestal. The muscle was cut longitudinally with a cautery and held flat against the pedestal by attaching silk sutures to the corners of the tissue. The muscle was then perfused continuously at a rate of 1 ml/min with warmed bicarbonate-buffered saline (pH 7.4).
The cremasteric microcirculation was then observed by using an intravital microscope (Nikon Optiphot-2, SMZ1, Badhoevedorp, The Netherlands) equipped with a 20× objective lens (Nikon SLDW, Badhoevedorp, The Netherlands) and a 10× eyepiece. A video camera (Sony SSC-C350P, Koeln, Germany) mounted on the microscope projected the image onto a color monitor and the images were video recorded for playback analysis. Single unbranched cremasteric venules (20–40 μm in diameter) were selected for study and the diameter was measured on-line by using a video caliper (Microcirculation Research Institute, Texas A&M University, College Station, Texas). Centerline red blood cell velocity (Vrbc) was also measured on-line by using an optical Doppler velocimeter (Microcirculation Research Institute, Texas A&M University, College Station, Texas). Venular blood flow was calculated from the product of mean red blood cell velocity (Vmean = Vrbc/1.6) and cross sectional area, assuming cylindrical geometry. Venular wall shear rate (γ) was calculated based on the Newtonian definition: γ = 8 × (Vmean/Dv) s-1, in which Dv is venular diameter [31].
The number of rolling, adherent and emigrated leukocytes was determined off-line during playback of videotaped images. Rolling leukocytes were defined as those white blood cells moving at a velocity less than that of erythrocytes in the same vessel. Leukocyte rolling velocity (Vwbc) was determined from the time required for a leukocyte to move along 100 μm length of the microvessel and is expressed as μm/s. Flux of rolling leukocytes was measured as those cells that could be seen moving past a defined reference point in the vessel. The same reference point was used throughout the experiment because leukocytes may roll for only a section of the vessel before rejoining the blood flow or becoming firmly adherent. A leukocyte was defined as adherent to venular endothelium if it was stationary for at least 30 s. Leukocyte adhesion was expressed as the number per 100 μm length of venule. Leukocyte emigration was expressed as the number of white blood cells per microscopic field surrounding the venule.
Experimental protocol
All preparations were left to stabilize for 30 minutes. Animals were injected locally by s.c. injection beneath the scrotal skin using a 30-gauge needle with 0.1 ml (each testicle) of sterile saline, LPS (0.05 μg/kg), unloaded or LTB4-loaded microspheres (1 mg/ml, containing equivalent to 50 ng/ml of the solution form) and LTB4 in solution (200 ng/ml). Preliminary experiments indicated that local administration of 0.05 μg/kg LPS was optimal for examination of leukocyte-endothelial interaction [32]. Animals were returned to their cages for 3.5 h and the right cremaster muscle was then prepared for intravital microscopy. After 4 h of the intraescrotal injection of the agents under investigation, measurements of leukocyte rolling flux, velocity, adhesion, emigration, Vrbc,, shear rate and diameter were obtained and recorded for 5 min.
Cell isolation and culture
Human umbilical vein and artery endothelial cells (HUVECs and HUAECs, respectively) were isolated by collagenase treatment [33] and maintained in human endothelial cell-specific EBM-2 supplemented with EGM-2 and 10% fetal calf serum (FCS). Cells up to passage 2 were grown to confluence on 24-well culture plates. Before every experiment, cells were incubated for 16 hours in medium containing 1% FCS and then returned to the 10% FCS medium for all experimental incubations. Samples of LTB4 in solution (200 ng/ml) and unloaded or LTB4-loaded microspheres (1 mg/ml, containing equivalent to 50 ng/ml of the solution form) were added to wells. At the end of an incubation time of 4 h, cell-free supernatants were collected and stored at -20°C for MCP-1 ELISA and NO measurement by Griess reaction.
Mice peritoneal macrophages were harvested from killed mice (sv129 mice) by lavage of their peritoneal cavity with 3 ml of RPMI-1640 medium. The isolated cells were centrifuged at 400 g for 10 min and re-suspended to 3 × 106 cells/ml. Aliquots (0.5 ml) of cell suspension were added to the wells of a 24-well plate and placed overnight in a humidified atmosphere (37°C, 5% CO2) for cell adhesion. Non-adherent cells were removed by washing with RPMI-1640 medium with 10% of fetal bovine serum (FBS) and gentamycin (1 μl/ml). Firmly adhering cells (5 × 106 cells/well) were incubated for 4 h with LTB4 in solution (5 × 10-8 M) in the absence or presence of CP 105,696 (5 × 10-8 M), a specific BLT1 receptor antagonist. Similarly, cells were incubated with unloaded or LTB4-loaded MS (1 mg/ml, containing equivalent to 50 ng/ml of the solution form) in the absence or presence of CP 105,696. At the end of the incubation period, cell-free supernatants were collected and stored at -20°C for NO measurement by Griess reaction.
PPAR-alpha expression assay
After 4 h incubation with the stimuli described above, peritoneal macrophages (5 × 106 cells/well) were homogenized in lysis buffer (25 mM TrisHCl pH 7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate, 0.1% SDS), which contained a protease inhibitor cocktail and 100 mM PMSF, (all from Sigma, Heidelberg, Germany). After scrapping the cells they were centrifuged for 5 min, 10000 rpm at 4°C. Protein concentration was determined by using a bicinchoninic acid (BCA) protein assay kit (Pierce). Equal amounts (30 μg/lane) of protein were subjected to SDS-PAGE (10% (w/v)) gel and separated proteins were electroblotted on polyvinylidene difluoride (PVDF) membranes (Bio-Rad Laboratories). Western analysis was performed with antibodies against PPARα (ab8934) (Abcam Cambridge Science Park, Cambridge, UK) and β-actin (Sigma Aldrich).
Densitometry
Densitometric analyses of autoradiograms were performed [34]. For each immunoblot, the pixel density I.O.D. (integrated optical density) was determined by selecting a rectangle of identical surface for all determinations, designed to entirely cover the band of interest. Background, which was subtracted from all values, was obtained using an average value from a clear area of the autoradiogram and all pixels at a black value of 255. Results were expressed as an Index = I.O.D. of stimulated cells/I.O.D. of cells cultured in medium alone.
NO production by HUVECs, HUAECs and murine macrophages
NO production by human endothelial cells and murine macrophages was determined by Griess reaction. HUVECs, HUAECs and peritoneal macrophages were incubated for 4 h with the described stimuli above. Supernatants (0.1 ml) were incubated with an equal volume of Griess reagent mixtures (1% sulfanilamine, 0.1% N-(1-naphtyl)-ethylendiamine dihydrochloride, 2.5% H3PO4) at room temperature for 10 min. The absorbance was measured in a microplate reader at 540 nm and concentrations calculated from a sodium nitrite standard curve. Data are presented as micromoles of NO2- (nitrite) (mean ± the SEM).
MCP-1 release from HUVECs and HUAECs
Human endothelial cells were cultured in 24-well culture plates and stimulated as described. After coating the 96-well plates overnight with the coating anti-MCP-1 mAb, diluted supernatant samples and standards were added in PBS/0.5% BSA/0.05% sodium azide for 2 h. Biotinylated detector antibodies were added for 2 h, followed by neutravidin-horseradish peroxidase for 1 h. All plate washes were of four cycles in freshly made PBS/0.2% Tween 20. Enhanced K-Blue TMB substrate was added for 30 min and the enzyme reaction stopped by addition of 0.19 M sulphuric acid. Absorbance was read at 450 nm and the data processed by GraphPad Prism software. Results are expressed as pM chemokine in the supernatant. The sensitivity of the assay was > 10 pg/ml.
Statistical analysis
The assays were analyzed using One-way analysis of variance (ANOVA) with post test (Tukey's Multiple Comparison Test). Values of P < 0.05 were considered statistically significant.
Results
Effect of the LTB4-loaded MS administration on leukocyte infiltration into the lungs and leukocyte-endothelial cell interactions
To investigate whether microspheres could release the encapsulated LTB4 during days, we assessed the leukocyte infiltration into the lung parenchyma of 5-LO knockout (5-LO-/-) mice submitted to the evaluated administrations. In this context, LTB4-loaded MS provoked a greater leukocyte infiltration into the lung parenchyma when compared to the other groups assayed (Fig. 1D). Intravital microscopy study was chosen to examine leukocyte-endothelial cell interactions in the mice cremasteric microcirculation. Figure 2 shows the effect of LTB4-loaded MS on leukocyte responses. After 4 h intraescrotal injection of 0.1 ml of 0.05 μg/kg LPS (used as control), significant increases in leukocyte rolling flux (91.0 ± 7.8 vs. 46.0 ± 1.7 cells/min), adhesion (14.0 ± 2.8 vs. 1.0 ± 1.4 cells per 100 μm vessel) and emigration (20.5 ± 0.7 vs. 1.3 ± 1.0 cells per field), and significant decreases in leukocyte rolling velocity (8.4 ± 1.9 vs. 25.9 ± 3.3 μm/s) were detected vs. values obtained in the saline treated animals. Injection of LTB4-loaded MS significantly increased leukocyte rolling flux (72.0 ± 5.2 vs. 46.0 ± 1.7 and 45.0 ± 7.07 cells/min), adhesion (4.5 ± 0.7 vs. 1.2 ± 0.5 and 1.5 ± 0.7 cells per 100 μm vessel) and emigration (7.3 ± 0.6 vs. 1.3 ± 1.0 and 2.5 ± 0.7 cells per field), and decreased the leukocyte rolling velocity (14.1 ± 0.9 vs. 25.9 ± 3.3 and 30.4 ± 7.9 μm/s) vs. values obtained in mice injected with saline and unloaded MS, respectively. None of these treatments had significant effects on wall shear rate (Table 1).
LTB 4 -loaded MS provoke leukocyte infiltration in the lung parenchyma. The lungs were removed on day 7 after the administrations, fixed and paraffin-embedded, followed by staining with HE. Lung sections are representative of three experiments with 5-LO-/- mice (5 animals each group) that received (A) PBS; (B) LTB4 in solution (3 × 10-8 M); (C) unloaded MS and (D) LTB4-loaded MS (5 × 10-7 M or 160 ng/ml). Magnifications of each section: ×50 and ×400.
Effect of LTB 4 in solution and released from PLGA microspheres (LTB 4 -loaded MS) on leukocyte rolling flux (A), rolling velocity (B), adhesion (C) and emigration (D) in mice cremaster muscle postcapillary venules. Parameters were measured 4 hours after the intraescrotal administration of saline (negative control), LPS (positive control, 0.05 μg/kg), unloaded and LTB4-loaded MS (1 mg/ml) and LTB4 in solution (200 ng/ml). Results are mean ± SEM (n = 4). *P < 0.05, **P < 0.01, ***P < 0.001, LTB4-loaded MS compared to saline group. # P < 0.05, ## P < 0.01 and &P < 0.05, LTB4-loaded MS compared to unloaded MS and LTB4 solution, respectively.
LTB4-loaded MS increase NO generation in HUVECs and HUAECs
Production of NO by human endothelial cells was quantified as described. In HUVECs, LTB4-loaded MS significantly increased nitrite levels when compared to the other stimuli (Fig. 3A). LTB4 in solution was also able to promote NO release although in moderate amounts. In contrast, the unloaded MS caused no significant increase in NO2- production. On the other hand, the assay performed in HUAECs revealed that only LTB4-loaded MS could significantly increase the levels of nitrite (Fig. 3B).
NO production by HUVECs (A) and HUAECs (B). NO2- levels were quantified by Griess reaction in the supernatants of cells incubated with medium, 1 mg of unloaded and LTB4-loaded MS or LTB4 in solution (200 ng/ml). Results are expressed as mean ± SEM (n = 3); *P < 0.05, ***P < 0.001, LTB4-loaded MS compared to control (medium). ###P < 0.001 and &P < 0.05, &&&P < 0.001, LTB4-loaded MS compared to unloaded MS and LTB4 solution, respectively.
Engulfed LTB4-loaded MS increase NO generation and PPARα expression in murine macrophages
We investigated nitrites levels produced by murine macrophages as a prediction of NO generation. High levels of nitrites were only achieved when the cells were stimulated with LTB4-loaded MS both in the presence or absence of CP 105,696 (Fig. 4A). Moreover, a further increase in nitrites production was detected when the LTB4-loaded MS were co-incubated with the BLT1 antagonist (CP 105,696) (Fig. 4A). Conversely, LTB4 in solution with or without antagonist had no effect on NO release. To assess the expression of the nuclear receptors and their possible activation under the effect of LTB4-loaded MS, we detected PPARα (molecular weight of approximately 52 kDa) in murine macrophages by Western Blot analysis. Treatment with LTB4 in solution increased PPARα expression moderately and this effect was blocked by pre-treatment of the cells with the BLT1 antagonist (CP 105,696) (Fig. 4B). However, when the cells were stimulated with LTB4-loaded MS, a further increase in PPARα expression was noted. Interestingly, a marked and significant increase in PPARα expression was also observed when the cells were stimulated with LTB4-loaded MS in the presence of the antagonist, especially when compared to that observed for the treatments with LTB4 solution + CP and LTB4-loaded MS.
NO production (A) and PPARα expression (B) by peritoneal macrophages after 4 hours incubation in RPMI medium. Peritoneal macrophages were incubated for 4 h with LTB4 in solution (5 × 10-8 M) with or without a specific BLT1 receptor antagonist (CP105,696). Similarly, cells were incubated with unloaded or LTB4-loaded MS (1 mg/ml) in absence or presence of CP105,696. (A) The nitrites levels were quantified by Griess reaction in the supernatants of the cells. The data are expressed as means ± the SEM (n = 3); **P < 0.01, ***P < 0.001, when compared to control (medium). ##P < 0.01, LTB4-loaded MS compared to LTB4-loaded MS + CP. (B) Western blot analysis for PPARα was performed as previously described in the Materials and Methods Section. Densitometric measurements show representative data of three separated experiments (mean ± SEM). **P < 0.01, LTB4-loaded MS + CP compared to LTB4 solution + CP. ##P < 0.01, LTB4-loaded MS + CP compared to LTB4-loaded MS.
LTB4 released from microspheres increases MCP-1 production by human endothelial cells
To evaluate LTB4-induced chemokine release at the cellular level, we used cultures of HUVECs and HUAECs. The amount of the chemokine released in the culture medium was determined by ELISA. In HUVECs, MCP-1 levels were significantly increased after 4 h stimulation with LTB4-loaded MS but not when the cells were stimulated with LTB4 in solution (Fig. 5A). In HUAECs, unloaded, LTB4-loaded MS and LTB4 in solution were able to increase MCP-1 contents in the supernatants investigated (Fig. 5B). Both in HUVECs and HUAECs assay, LTB4-loaded MS were able to increase significantly MCP-1 levels when compared to LTB4 solution stimulus.
MCP-1 levels in the supernatant of HUVECS (A) and HUAECs (B). Cells were incubated with 1 mg of unloaded, LTB4-loaded MS or LTB4 in solution (200 ng/ml). MCP-1 content was determined by ELISA. Results are expressed as mean ± SEM (n = 3); **P < 0.01, ***P < 0.001, LTB4-loaded MS compared to control (medium). ###P < 0.001 and &&&P < 0.001, LTB4-loaded MS compared to unloaded MS and LTB4 solution, respectively.
Discussion
LTB4 is a classical chemoattractant agent that plays a crucial role in multiple inflammatory diseases. It promotes leukocytes adhesion and diapedesis through the endothelial cell barrier. Furthermore, LTB4 also induces chemotaxis and proliferation of human coronary artery [21]. However, the molecular mechanisms by which LTB4 induces transendothelial migration of leukocytes are not completely elucidated although it seems to be involved soluble factors as well as both leukocyte and endothelial cell adhesion molecules [25]. Direct effects of LTB4 on endothelial cells have also been discussed, although these cells have shown a weak reaction to this mediator [35, 36]. First, in this study, we investigated whether the proposed microspheres could release the encapsulated LTB4 during days and stimulate cells recruitment into the lung parenchyma. For this purpose, we performed an assay using 5-LO-/- mice since they do not have endogenous synthesis of leukotrienes and only exogenous LTB4 employed could exert its biological activity. Animals that received LTB4-loaded MS displayed greater leukocyte infiltration in the lung parenchyma compared to PBS, LTB4 in solution or unloaded MS groups, demonstrating that the encapsulation method preserved the biological activity of the mediator. Although LTB4-loaded MS have recruited more leukocytes to the lung parenchyma than the other stimuli, the unloaded MS also provoked a marked cell infiltration. This fact can be due to the particle size (<10 μm) employed in our study since the microspheres will be preferentially engulfed by phagocytes, especially alveolar macrophages present in the lungs. The cell activation provoked by the engulfment of the microspheres suggests that other chemotactic factors or cytokines released during the particles' delivery could increase cell infiltration in the lungs. Regarding the desired pattern of cell activation, the unloaded or LTB4-loaded MS could be useful to stimulate the immune response against intracellular pathogens. Based on these different profiles of leukocyte infiltration provoked by the employment of the microspheres, our histological sections showed marked differences on the cell recruitment to the lungs, especially on day 7 after administrations (Fig. 1). In this regard, we previously demonstrated that the LTB4 released from microspheres recruited high numbers of mononuclear cells and neutrophils to the bronchoalveolar space of 5-LO-/- mice [27]. Also, we conducted lung sections earlier than day 7 (days 1 and 4) but no significant leukocyte infiltration was achieved. Our findings suggest that the extended released of LTB4 from microspheres was able to activate and induce lung cells to generate chemotactic agents, reflected by the greater leukocyte infiltration into the parenchyma lung. These results corroborate the idea that cell migration phenomenon is strongly stimulus-dependent since exogenous LTB4 could prime the cells to chemotactic mediators release and recruit them to the bronchoalveolar space or lung parenchyma.
We have demonstrated that LTB4 released from microspheres but not LTB4 in solution can cause leukocyte-endothelial cell interactions within the mice cremasteric microcirculation, as demonstrated by intravital microscopy studies (Fig. 2). These results confirm that the encapsulation of the lipid mediator is an important strategy to preserve its biological activity, constituting a tool to stimulate cells. We can suggest that the microspheres might protect the LTB4 molecule against degradation and/or even facilitate its interaction with either the endothelium or the leukocytes.
In order to extend these findings to humans, we measured the production of nitrites and MCP-1 in response to LTB4-loaded MS both in HUVECs and HUAECs. In this context, different studies have shown that LTB4 promotes nitrites, presumably reflecting NO generation, and MCP-1 release in HUVECs and this effect is enhanced when the endothelial cells are preincubated with LPS, presumably via a functional up-regulation of BLT1 receptor [20]. In contrast, the amounts of BLT2 mRNA gradually decreased when the cells were incubated with LTB4. In our study, when human endothelial cells were stimulated with LTB4-loaded MS it was detected a massive release of nitrites and MCP-1 compared to those obtained when LTB4 is in solution form. This fact demonstrating the role of LTB4-loaded MS in increasing a chemotactic protein (as detected by MCP-1 levels) corroborates the results obtained from intravital microscopy study where we could observe more leukocytes adhered and emigrated to the cremasteric tissue after the administration of those microspheres. Therefore, our findings add further support to the hypothesis that microspheres protect LTB4 molecule from its metabolism, especially in this protocol in which a 4 h time period was chosen to carry out the different assays. Nevertheless, it is likely that both forms of LTB4 exert similar effects under acute conditions (1 h). Although unloaded MS have induced MCP-1 release by HUAECs (Fig. 5B), this fact can be due to the physical interactions between cell surface and the polymer employed to do the microspheres. Our results suggest that LTB4-loaded MS employed in the assays can stimulate the cells and induce a different pattern of inflammatory response compared to the mediator in solution.
In order to get more conclusive data, we also compared the effect of LTB4 in solution with that released from microspheres on NO production by mice peritoneal macrophages, in the presence of a specific BLT1 receptor antagonist, CP 105,696 (Fig. 4A). In this in vitro system, only LTB4-loaded MS caused a significant nitrites release whereas LTB4 in solution did not display any effect. Interestingly, when BLT1 receptors were blocked with CP 105,696 an enhanced and significant response was observed. This fact can be due to the different mechanisms of cell activation conferred by LTB4 in solution or released from MS. It is also likely that LTB4 released from engulfed MS could exert its activity inside the cell nucleus, where it can bind to specific receptors, whereas exogenous LTB4 in solution binds only to specific BLTs membrane receptors. In this context, it is known that LTB4 is a natural ligand for PPARα, a subtype of a family of PPARs. These transcription factors regulate gene expression of enzymes associated with lipid homeostasis and affect the duration of an inflammatory response induced by LTB4 [12]. Although the majority of studies have indicated an anti-inflammatory role of PPARα ligands, an increase in the neutrophil chemoattractant IL-8 and the MCP-1 levels have also been observed in endothelial cells [37]. In addition, the PPARα ligand fenofibrate was demonstrated to enhance nitric oxide synthase (NOS) expression and activity in isolated endothelial cells [38]. Also, it is important to note that some studies report that PPARγ has no anti-inflammatory activity or might indeed exert a proinflammatory response [39]. With this regard, as proposed in this study, the LTB4 binding to nuclear receptors without previous interaction with its membrane receptors (BLTs) results in an increase of PPARα expression (Fig. 4B) and possibly activates the inflammatory genes to produce NO, MCP-1 and other inflammatory mediators. A recent published work by our group regarding a phagocytosis' assay of LTB4-loaded MS [27] showed that encapsulated LTB4 was able to increase the number of mice peritoneal macrophages that contain microspheres and also the amount of them that were engulfed. These previous findings involving cell activation by the uptake of LTB4-loaded MS support our recent results showing that macrophages activation induced by LTB4-loaded MS can be more persistent than that with the mediator in solution.
Conclusion
As reported in this study, the employment of LTB4-loaded MS seems to preserve the biological activity of the inflammatory lipid mediator as demonstrated by intravital microscopy studies as well as by in vitro assays using murine peritoneal macrophages and human endothelial cells. Therefore, these findings may contribute to the better understanding of the different pattern of cell activation induced by the delivery of the LTB4 to cell cytoplasm or nucleus and maybe these microspheres can constitute an alternative therapy for the control of different infectious diseases.
References
Ford-Hutchinson AW, Bray MA, Doig MV, Shipley ME, Smith MJ: Leukotriene B, a potent chemokinetic and aggregating substance released from polymorphonuclear leukocytes. Nature. 1980, 286: 264-265. 10.1038/286264a0.
Faccioli LH, Nourshargh S, Moqbel R, Williams FM, Sehmi R, Kay AB, Williams TJ: The accumulation of 111In-eosinophils induced by inflammatory mediators, in vivo. Immunology. 1991, 73 (2): 222-227.
Goodarzi KM, Goodarzi AM, Tager AD, Luster , von Andrian UH: Leukotriene B4 and BLT1 control cytotoxic effector T cell recruitment to inflamed tissues. Nat Immunol. 2003, 4: 965-973. 10.1038/ni972.
Medeiros AI, SÁ-Nunes A, Soares EG, Peres CM, Silva CL, Faccioli LH: Blockade of endogenous leukotrienes exacerbates pulmonary histoplasmosis. Infect Immun. 2004, 72: 1637-1644. 10.1128/IAI.72.3.1637-1644.2004.
Machado ER, Ueta MT, Lourenço EV, Anibal FF, Sorgi CA, Soares EG, Roque-Barreira MC, Medeiros AI, Faccioli LH: Leukotrienes play a role in the control of parasite burden in murine strongyloidiasis. J Immunol. 2005, 175: 3892-3899.
Mancuso P, Nana-Sinkam P, Peters-Golden M: Leukotriene B4 augments neutrophil phagocytosis of Klebsiella pneumoniae. Infect Immun. 2001, 69: 2011-10.1128/IAI.69.4.2011-2016.2001.
Serezani CH, Aronoff DM, Jancar S, Mancuso P, Peters-Golden M: Leukotrienes enhance the bactericidal activity of alveolar macrophages against Klebsiella pneumoniae through the activation of NADPH oxidase. Blood. 2005, 106: 1067-1075. 10.1182/blood-2004-08-3323.
Peres CM, Aronoff DM, Serezani CH, Flamand N, Faccioli LH, Peters-Golden M: Specific leukotriene receptors couple to distinct g proteins to effect stimulation of alveolar macrophage host defense functions. J Immunol. 2007, 179: 5454-5461.
Malaviya R, Abraham SN: Role of mast cell leukotrienes in neutrophil recruitment and bacterial clearance in infectious peritonitis. J Leukoc Biol. 2000, 67 (6): 841-6.
Yokomizo T, Izumi T, Chang K, Takuwa Y, Shimizu T: A G-protein coupled receptor for leukotriene B4 that mediates chemotaxis. Nature. 1997, 387: 620-624. 10.1038/42506.
Tager AM, Bromley SK, Medoff BD, Islam SA, Bercury SD, Friedrich EB, Carafone AD, Gerszten RE, Luster AD: Leukotriene B4 receptor BLT1 mediates early effector T cell recruitment. Nat Immunol. 2003, 4: 982-990. 10.1038/ni970.
Devchand PR, Keller H, Peters JM, Vazquez M, Gonzalez FJ, Wahli W: The PPARα-leukotriene B4 pathway to inflammation control. Nature. 1996, 384: 39-43. 10.1038/384039a0.
Springer TA: Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm. Cell. 1994, 76: 301-314. 10.1016/0092-8674(94)90337-9.
Gerszten RE, Garcia-Zepeda EA, Lim YC, Yoshida M, Ding HA, Gimbrone MA, Luster AD, Luscinskas FW, Rosenzweig A: MCP-1 and IL-8 trigger firm adhesion of monocytes to vascular endothelium under flow conditions. Nature. 1999, 398: 718-723. 10.1038/19546.
Vaddi K, Newton RC: Regulation of monocyte integrin expression by β-family chemokines. J Immunol. 1994, 153: 4721-4732.
Showell HJ, Conklyn MJ, Alpert R, Hingorani GP, Wright KF, Smith MA, Stam E, Griffiths RJ: The preclinical pharmacological profile of the potent and selective leukotriene B4 antagonist CP-195543. J Pharmacol Exp Ther. 1998, 285: 946-954.
Patrícia MK, Kim JA, Harper CM, Shih PT, Berliner JA, Natarajan R, Nadler JL, Hedrick CC: Lipoxygenase products increase monocyte adhesion to human aortic endothelial cells. Arterioscler Thromb Vasc Biol. 1999, 19: 2615-2622.
Palmblad J, Lerner R, Larsson SH: Signal transduction mechanisms for leukotriene B4 induced hyperadhesiveness of endothelial cells for neutrophils. J Immunol. 1994, 152: 262-269.
Hoover RL, Karnovsky MJ, Austen KF, Corey EJ, Lewis RA: Leukotriene B4 action on endothelium mediates augmented neutrophil/endothelial adhesion. Proc Natl Acad Sci USA. 1984, 81: 2191-2193. 10.1073/pnas.81.7.2191.
Hong Q, Anne-Sofie J, Mattias S, Min W, Oliver S, Jan P, Jesper ZH: Differential induction of BLT receptor expression on human endothelial cells by lipopolysacharide, cytokines, and leukotriene B4. Proc Natl Acad Sci USA. 2006, 103: 6913-6918. 10.1073/pnas.0602208103.
Back M, Bu DX, Branstrom R, Sheikin Y, Yan ZQ, Hansson GK: Leukotriene B4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia. Proc Natl Acad Sci USA. 2005, 102: 17501-17506. 10.1073/pnas.0505845102.
Palmblad JE, Lerner R: Leukotriene B4-induced hyperadhesiveness of endothelial cells for neutrophils: relation to CD54. Clin Exp Immunol. 1992, 90: 300-304.
Palmblad J, Lerner R, Larsson SH: Signal transduction mechanisms for leukotriene B4 induced hyperadhesiveness of endothelial cells for neutrophils. J Immunol. 1994, 152: 262-269.
Wedmore CV, Williams TJ: Control of vascular permeability by polymorphonuclear leukocytes in inflammation. Nature. 1981, 289: 646-650. 10.1038/289646a0.
Ulbrich H, Eriksson EE, Lindbom L: Leukocyte and endothelial cell adhesion molecules as targets for therapeutic interventions in inflammatory disease. Trends Pharmacol Sci. 2003, 24: 640-647. 10.1016/j.tips.2003.10.004.
Lima KM, Santos SA, Lima VM, Coelho-Castelo AA, Rodrigues JMJR, Silva CL: Single dose of a vaccine based on DNA encoding mycobacterial hsp65 protein plus TDM-loaded PLGA microspheres protects mice against a virulent strain of Mycobacterium tuberculosis. Gene Ther. 2003, 10: 678-685. 10.1038/sj.gt.3301908.
Nicolete R, Lima KM, Rodrigues Júnior JM, Baruffi MD, Medeiros AI, Bentley MVLB, Silva CL, Faccioli LH: In vitro and in vivo activities of leukotriene B4-loaded biodegradable microspheres. Prostaglandins & other Lipid Mediators. 2007, 83: 121-129. 10.1016/j.prostaglandins.2006.10.007.
Eldridge JH, Staas JK, Meulbroek JA, Tice TR, Gilley RM: Biodegradable and biocompatible poly (DL-lactide-co-glycolide) microspheres as an adjuvant for staphylococcal enterotoxin B toxoid which enhances the level of toxin-neutralizing antibodies. Infect Immun. 1991, 59: 2978-2986.
Lima KM, Rodrigues JM: Poly-dl-lactide-co-glycolide microspheres as a controlled release antigen delivery system. Braz J Med Biol Res. 1999, 32: 171-180.
Sanz MJ, Hickey MJ, Johnston B, McCafferty DM, Raharjo E, Huang PL, Kubes P: Neuronal nitric oxide synthase (NOS) regulates leukocyte-endothelial cell interactions in endothelial NOS deficient mice. Br J Pharmacol. 2001, 134: 305-312. 10.1038/sj.bjp.0704234.
House SD, Lipowsky HH: Leukocyte-endothelium adhesion: microhemodynamics in mesentery of the cat. Microvasc Res. 1987, 34: 363-379. 10.1016/0026-2862(87)90068-9.
Andonegui G, Goyert SM, Kubes P: Lipopolysaccharide-induced leukocyte-endothelial cell interactions: a role for CD14 versus toll-like receptor 4 within microvessels. J Immunol. 2002, 169 (4): 2111-2119.
Jaffe EA, Nachman RL, Becker CG, Minick CR: Culture of human endothelial cells derived from umbilical veins. Identification by morphologic and immunologic criteria. J Clin Invest. 1973, 52: 2745-2756. 10.1172/JCI107470.
NIH Image website. [http://rsb.info.nih.gov]
Lerner R: Changes of cytosolic calcium ion concentrations in human endothelial cells in response to thrombin, platelet-activating factor, and leukotriene B4. J Lab Clin Med. 1994, 124: 723-729.
Nohgawa M, Sasada M, Maeda A, Asagoe K, Harakawa N, Takano K, Yamamoto K, Okuma M: Leukotriene B4-activated human endothelial cells promote transendothelial neutrophil migration. J Leukocyte Biol. 1997, 62: 203-209.
Lee H, Shi W, Tontonoz P, Wang S, Subbanagounder G, Hedrick CC: Role for peroxisome proliferator-activated receptor alpha in oxidized phospholipid-induced synthesis of monocyte chemotactic protein-1 and interleukin-8 by endothelial cells. Circ Res. 2000, 87: 516-521.
Goya K, Sumitani S, Xu X, Kitamura T, Yamamoto H, Kurebayashi S, Saito H, Kouhara H, Kasayama S, Kawase I: Peroxisome proliferator-activated receptor alpha agonists increase nitric oxide synthase expression in vascular endothelial cells. Arterioscler Thromb Vasc Biol. 2004, 24: 658-663. 10.1161/01.ATV.0000118682.58708.78.
Tontonoz P, Nagy L, Alvarez JG, Thomazy VA, Evans RM: PPARgamma promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell. 1998, 93: 241-252. 10.1016/S0092-8674(00)81575-5.
Acknowledgements
We are grateful to the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, 02/12856-2 and 05/00110-4), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPp) and grants SAF 2005-01649, CICYT, Spanish Ministerio de Educación y Ciencia; Research Group 03/166 of Conselleria de Cultura y Educación (Generalitat Valenciana). RN was supported by a grant of Programa de Mobilidade Internacional, Banco Santander. CR and LP were supported by a grant from Spanish Ministerio de Educacion y Ciencia. PJJ was supported by a grant from the University of Valencia, Spain.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
RN designed all the experiments, carried out intravital microscopy studies, in vitro cell assays and drafted the manuscript. CR provided help in isolating human endothelial cells. CR and LP carried out the immunoblot assays. PJJ participated in the design of some experiments. CAS provided help in some experimental protocols. EGS carried out the histology sections. MJS and LHF participated in the design and coordination of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nicolete, R., Rius, C., Piqueras, L. et al. Leukotriene B4-loaded microspheres: a new therapeutic strategy to modulate cell activation. BMC Immunol 9, 36 (2008). https://doi.org/10.1186/1471-2172-9-36
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2172-9-36