Abstract
Background
Selenoprotein S (SelS) protects the functional integrity of the endoplasmic reticulum against the deleterious effects of metabolic stress. SEPS1/SelS polymorphisms have been involved in the increased release of pro-inflammatory cytokines interleukin (IL)-1β, tumor necrosis factor (TNF)-α and IL-6 in macrophages. We aimed at investigating the role of the SEPS1 variants previously associated with higher plasma levels of these cytokines and of the SEPS1 haplotypes in the susceptibility to develop immune-mediated diseases characterized by an inflammatory component.
Results
Six polymorphisms distributed through the SEPS1 gene (rs11327127, rs28665122, rs4965814, rs12917258, rs4965373 and rs2101171) were genotyped in more than two thousand patients suffering from type 1 diabetes, rheumatoid arthritis or inflammatory bowel diseases and 550 healthy controls included in the case-control study.
Conclusion
Lack of association of SEPS1 polymorphisms or haplotypes precludes a major role of this gene increasing predisposition to these inflammatory diseases.
Similar content being viewed by others
Background
The human gene SEPS1, located on chromosome 15q26.3, encodes selenoprotein S which participates in the retro-translocation of misfolded proteins from the endoplasmic reticulum (ER) to the cytosol for their degradation [1]. This ER membrane protein functions in stress responses to prevent the deleterious consequences of accumulation of misfolded proteins, accumulation that has been linked to immune and inflammatory processes [2]. A study identified the strong association of the proximal promoter SEPS1 polymorphism at -105G/A with circulating levels of three pro-inflammatory cytokines, interleukin (IL)-6, IL-1β and TNF-α [3]. Moreover, these authors reported that the mutant variant significantly reduced the promoter activity of the SEPS1 gene in stressed HepG2 cells and that the suppression of this gene by short interfering RNA increased the release of pro-inflammatory cytokines in a macrophage cell line. A regulatory loop has been recently proposed whereby cytokines stimulate the expression of SEPS1, which in turn diminishes cytokine production [4].
The murine homolog gene of the human SEPS1 is the Tanis gene, which encodes a serum amyloid A receptor [5]. Acute phase serum amyloid A proteins (SAAs) are multifunctional apolipoproteins produced in large amounts during the acute phase of inflammation and also during the development of chronic inflammatory diseases. SAAs are involved in the pathogenesis of several chronic inflammatory diseases, such as rheumatoid arthritis (RA) [6–9], multiple sclerosis (MS)[10] and inflammatory bowel diseases (IBD) [11–13]. It is believed that locally synthesized SAA by synovial cells in the inflamed joints acts as an autocrine inducer of matrix metalloproteinase-1 and causes extensive joint erosion [14].
Altogether these data point to the important role of selenoprotein S mediating inflammation, and we aimed at testing whether the SEPS1 gene was involved in the development of inflammatory autoimmune complex diseases. These are multifactorial traits influenced by both genetic predisposing factors and environmental triggers. The activation of SEPS1 expression by fasting in vivo and by glucose-deprivation in vitro allowed its assignation to the glucose-regulated protein family [5, 15]. Furthermore, a locus on 15q26, IDDM3, was described to increase susceptibility to type 1 diabetes, T1D [16, 17]. Therefore, we decide to test the SEPS1 polymorphisms for association with diabetes risk in a cohort of Spanish T1D patients. Additionally, we pursued to study two other autoimmune diseases with an important inflammatory component, rheumatoid arthritis and the inflammatory bowel diseases, Crohn's disease (CD) and ulcerative colitis (UC). Provided this candidate gene previously related with the inflammatory response shows any influence on the pathogenesis of these diseases, a new mechanistic tool for treatment would be available.
Methods
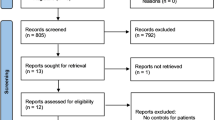
Patients and controls
The study group consisted of 592 RA, 674 IBD and 311 T1D unrelated patients, consecutively recruited from one centre, either Hospital Clínico San Carlos or Hospital Ramón y Cajal (Madrid, Spain).
T1D patients (median age at onset 15 years) diagnosed according to the criteria of the American Diabetes Association (ADA), were insulin-dependent at the time to study.
RA diagnosis was established based on the American College of Rheumatology (ACR) criteria [18] and samples were previously genotyped for HLA-DRB1. Mean age at onset was 54 ± 14 years; 61% of the patients carried the shared epitope; 66% and 50% of the patients were positive for rheumatoid factor and for anti-cyclic citrullinated peptide, respectively, and 32% of the patients presented nodular disease.
Diagnosis of IBD patients was based on standard clinical, radiologic, endoscopic and histologic criteria [19]. The mean age at onset for UC patients was 38 years; 41% of the patients presented pancolitis; 47% and 13% of the patients suffered extraintestinal manifestations and colectomy, respectively. CD patients were classified according to the location of the lesions in ileal (L1, 48%), colonic (L2, 16%), ileocolonic (L3, 32%) and upper gastrointestinal tract (L4, 3%) and according to the disease behavior in inflammatory (B1, 43%), stricturing (B2, 15%) and perforating (B3, 42%). Only 20% of the CD patients debuted after the age of 40.
A group of 550 healthy unrelated subjects from Madrid (mainly hospital employees and blood donors) were selected as controls. Cases and controls were all white Spanish subjects and were included in this study after written informed consent. The Ethics Committee of Hospital Clínico (Madrid) approved the study.
SEPS1 polymorphisms
The SEPS1 polymorphisms (rs11327127, rs28665122, rs4965814, rs12917258, rs4965373 and rs2101171) were genotyped using TaqMan assays from Applied Biosystems following manufacturer's suggestions and analyzed in an ABI 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA). Their location is indicated by the distance from the transcription start site: two of them are in the promoter region; another two in intron 5; rs4965373 depending of alternative splicing is either in intron 6 or in the 3'UTR region; and the last one is downstream at 9707 (see Table 1).
Statistical Analysis
Allele and genotype frequencies in patients and controls were compared by χ2 test or Fisher exact test when necessary; p values were considered significant at a level of <0.05. Odds ratio (OR) and p values were calculated using a standard package (Epi Info v. 6.02, CDC, Atlanta, USA). For an OR = 1.5, the statistical power of our cohorts ranged from 80 – 95% depending on the specific polymorphism analyzed.
Haplotypic frequencies were estimated using the Expectation-Maximization algorithm implemented in the Arlequin v2.000 software [20] with number of iterations set at 5000 and initial conditions at 50, with an epsilon value of 10-7.
Results and discussion
The present study investigates the influence of all SEPS1 variants previously correlated with increased pro-inflammatory cytokines levels (polymorphisms at -105G/A, 3705G/A and 5227C/T) and of the SEPS1 haplotypes on predisposition to inflammatory complex diseases.
We first analyzed the functional SEPS1 promoter polymorphism at -105G/A and no significant differences in genotypic frequencies were observed when healthy controls were compared with patients suffering from T1D, RA or IBD (Table 1). As two other variants (rs4965814 and rs4965373) have been associated with high plasma cytokine levels [3], we studied them in our cohorts, and the distribution of genotypes followed the same pattern in patients and in controls (Table 1).
We selected three additional polymorphisms along the gene from those described by Curran et al [3] in order to analyze the haplotypes inferred by applying the Expectation-Maximization algorithm implemented in the Arlequin software. No significant difference in haplotype frequencies was observed after appropriate correction for multiple testing in any diseased cohort (Table 2).
A direct functionality has been attributed to the SEPS1 promoter polymorphism at -105G/A, increasing plasma levels of the aforementioned cytokines presumably due to the disruption of an ER stress element (ERSE). Two other tested variants have also been strongly related with the circulating levels of the inflammatory cytokines [3]. In contrast, a recent report did not find consistent association of this polymorphism with circulating levels of either IL-6 or TNF-α [21]. We did not observe differences in the genotypic distribution of the SEPS1 polymorphisms analyzed in Spanish cohorts between patients suffering from autoimmune diseases with a clear inflammatory component, like T1D, RA or IBD, and controls. The analysis of SEPS1 haplotypic frequencies did not differ between patients and healthy individuals either.
Given that evidences exist for the affected expression and activity of some selenoproteins depending on sexual dimorphism in mouse [22] and human [23], we decided to check for a gender specific association of -105G/A SEPS1 polymorphism with the autoimmune disorders under study; however, we did not detect a gender-bias in our results. No significant difference between sex-stratified cohorts was found for any of the polymorphisms studied (Table 3).
SEPS1 expression was not significantly altered in intestinal epithelial cells of IBD murine models or in intestinal biopsies from IBD patients when compared with that present in controls [24]. Concordantly, a study testing the association of the promoter variant at -105 with cerebrovascular disease found no influence on stroke risk [25]. Both studies are in agreement with our results that showed lack of association between SEPS1 polymorphisms and susceptibility to chronic inflammatory diseases. Moreover, a Finnish study of five variants in the SEPS1 gene locus showed no significant difference between carriers/non-carriers when cardiovascular cases and healthy individuals were compared. The authors suggested that two polymorphisms contribute to the risk for coronary heart disease and for ischemic stroke in females; interestingly, the associated polymorphisms do not correspond with the one at -105G/A [21]. Therefore, evidences are mounting against the role of the SEPS1 gene in all these conditions, with the only exception to this point of one report defining the minor allele at -105G/A SEPS1 as a risk factor for preeclampsia in a large Norwegian cohort [26].
Conclusion
The Wellcome Trust Case Control Consortium published recently a genome wide association study for several inflammatory conditions, such as RA, T1D or CD [27] Although the chromosomal region where the gene maps did not show association for any of the mentioned diseases, the SEPS1 polymorphisms were not analyzed and therefore their involvement in susceptibility could not be formally excluded. Ours is a thorough study analyzing the influence of six polymorphisms along the SEPS1 gene on susceptibility to common diseases, unravelling lack of association. Our data allow discardind a major individual role of this gene in the aetiology of the studied polygenic diseases.
Abbreviations
- SelS(SEPS1) :
-
Selenoprotein S gene
- (IL)-1β :
-
Interleukin 1 beta
- TNF-α :
-
Tumor necrosis factor alpha
- IL-6 :
-
Interleukin 6
- ER :
-
Endoplasmic reticulum
- HepG2 :
-
Human hepatocellular liver carcinoma cell line
- RNA :
-
Ribonucleic acid
- SAAs :
-
Acute phase serum amyloid A proteins
- RA :
-
Rheumatoid arthritis
- MS :
-
Multiple sclerosis
- IBD :
-
Inflammatory bowel diseases
- IDDM3 :
-
Insulin-dependent diabetes mellitus 3
- T1D :
-
Type 1 diabetes
- CD :
-
Crohn's disease
- UC :
-
Ulcerative colitis
- ERSE :
-
ER stress element
- ADA :
-
American Diabetes Association
- ACR :
-
American College of Rheumatology
- L1 :
-
Ileal lesions
- L2 :
-
Colonic lesions
- L3 :
-
Ileocolonic lesions
- L4 :
-
Upper gastrointestinal tract lesions
- B1 :
-
Inflammatory disease behavior
- B2 :
-
Structuring disease behavior
- B3 :
-
Perforating disease behavior
- OR :
-
Odds ratio
- FIS :
-
Fondo de Investigaciones Sanitarias.
References
Ye Y, Shibata Y, Yun C, Ron D, Rapoport TA: A membrane protein complex mediates retro-translocation from the ER lumen into the cytosol. Nature. 2004, 429: 841-847. 10.1038/nature02656.
Pahl HL, Baeuerle PA: Endoplasmicreticulum-induced signal transduction and gene expression. Trends Cell Biol. 1997, 7: 50-55. 10.1016/S0962-8924(96)10050-7.
Curran JE, Jowett JB, Elliott KS, Gao Y, Gluschenko K, Wang J, Abel Azim DM, Cai G, Mahaney MC, Comuzzie AG, Dyer TD, Walder KR, Zimmet P, MacCluer JW, Collier GR, Kissebah AH, Blangero J: Genetic variation in selenoprotein S influences inflammatory response. Nat Genet. 2005, 37: 1234-1241. 10.1038/ng1655.
Gao Y, Hannan NR, Wanyonyi S, Konstantopolous N, Pagnon J, Feng HC, Jowett JB, Kim KH, Walder K, Collier GR: Activation of the selenoprotein SEPS1 gene expression by pro-inflammatory cytokines in HepG2 cells. Cytokine. 2006, 33: 246-251. 10.1016/j.cyto.2006.02.005.
Walder K, Kantham L, McMillan JS, Trevaskis J, Kerr L, De Silva A, Sunderland T, Godde N, Gao Y, Bishara N, Windmill K, Tenne-Brown J, Augert G, Zimmet PZ, Collier GR: Tanis: a link between type 2 diabetes and inflammation?. Diabetes. 2002, 51: 1859-1866. 10.2337/diabetes.51.6.1859.
O'Hara R, Murphy EP, Whitehead AS, FitzGerald O, Bresnihan B: Local expression of the serum amyloid A and formyl peptide receptor-like 1 genes in synovial tissue is associated with matrix metalloproteinase production in patients with inflammatory arthritis. Arthritis Rheum. 2004, 50: 1788-1799. 10.1002/art.20301.
Kokubun M, Imafuku Y, Okada M, Ohguchi Y, Ashikawa T, Yamada T, Yoshida H: Serum amyloid A (SAA) concentration varies among rheumatoid arthritis patients estimated by SAA/CRP ratio. Clin Chim Acta. 2005, 360: 97-102. 10.1016/j.cccn.2005.04.006.
Zhang N, Ahsan MH, Purchio AF, West DB: Serum amyloid A-luciferase transgenic mice: response to sepsis, acute arthritis, and contact hypersensitivity and the effects of proteasome inhibition. J Immunol. 2005, 174: 8125-8134.
Mullan RH, Bresnihan B, Golden-Mason L, Markham T, O'Hara R, FitzGerald O, Veale DJ, Fearon U: Acute-phase serum amyloid A stimulation of angiogenesis, leukocyte recruitment, and matrix degradation in rheumatoid arthritis through an NF-kappaB-dependent signal transduction pathway. Arthritis Rheum. 2006, 54: 105-114. 10.1002/art.21518.
Ristori G, Laurenti F, Stacchini P, Gasperini C, Buttinelli C, Pozzilli C, Salvetti M: Serum amyloid A protein is elevated in relapsing-remitting multiple sclerosis. J Neuroimmunol. 1998, 88: 9-12. 10.1016/S0165-5728(98)00037-X.
Chambers RE, Stross P, Barry RE, Whicher JT: Serum amyloid A protein compared with C-reactive protein, alpha 1-antichymotrypsin and alpha 1-acid glycoprotein as a monitor of inflammatory bowel disease. Eur J Clin Invest. 1987, 17: 460-467. 10.1111/j.1365-2362.1987.tb01143.x.
De Beer FC, Mallya RK, Fagan EA, Lanham JG, Hughes GR, Pepys MB: Serum amyloid-A protein concentration in inflammatory diseases and its relationship to the incidence of reactive systemic amyloidosis. Lancet. 1982, 2: 231-234. 10.1016/S0140-6736(82)90321-X.
Niederau C, Backmerhoff F, Schumacher B: Inflammatory mediators and acute phase proteins in patients with Crohn's disease and ulcerative colitis. Hepatogastroenterology. 1997, 44: 90-107.
Vallon R, Freuler F, Desta-Tsedu N, Robeva A, Dawson J, Wenner P, Engelhardt P, Boes L, Schnyder J, Tschopp C, Urfer R, Baumann G: Serum amyloid A (apoSAA) expression is up-regulated in rheumatoid arthritis and induces transcription of matrix metalloproteinases. J Immunol. 2001, 166: 2801-2807.
Gao Y, Feng HC, Walder K, Bolton K, Sunderland T, Bishara N, Quick M, Kantham L, Collier GR: Regulation of the selenoprotein SelS by glucose deprivation and endoplasmic reticulum stress - SelS is a novel glucose-regulated protein. FEBS Lett. 2004, 563: 185-190. 10.1016/S0014-5793(04)00296-0.
Field LL, Tobias R, Magnus T: A locus on chromosome 15q26 (IDDM3) produces susceptibility to insulin-dependent diabetes mellitus. Nat Genet. 1994, 8: 189-194. 10.1038/ng1094-189.
Zamani M, Pociot F, Raeymaekers P, Nerup J, Cassiman JJ: Linkage of type I diabetes to 15q26 (IDDM3) in the Danish population. Hum Genet. 1996, 98: 491-496. 10.1007/s004390050245.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324. 10.1002/art.1780310302.
Lennard-Jones JE: Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989, 170: 2-6; discussion 16-9. 10.3109/00365528909091339.
Excoffier L, Slatkin M: Maximum-likelihood estimation of molecular haplotype frequencies in a diploid population. Mol Biol Evol. 1995, 12: 921-927.
Alanne M, Kristiansson K, Auro K, Silander K, Kuulasmaa K, Peltonen L, Salomaa V, Perola M: Variation in the selenoprotein S gene locus is associated with coronary heart disease and ischemic stroke in two independent Finnish cohorts. Hum Genet. 2007, 122: 355-365. 10.1007/s00439-007-0402-7.
Riese C, Michaelis M, Mentrup B, Gotz F, Kohrle J, Schweizer U, Schomburg L: Selenium-dependent pre- and posttranscriptional mechanisms are responsible for sexual dimorphic expression of selenoproteins in murine tissues. Endocrinology. 2006, 147: 5883-5892. 10.1210/en.2006-0689.
Meplan C, Crosley LK, Nicol F, Beckett GJ, Howie AF, Hill KE, Horgan G, Mathers JC, Arthur JR, Hesketh JE: Genetic polymorphisms in the human selenoprotein P gene determine the response of selenoprotein markers to selenium supplementation in a gender-specific manner (the SELGEN study). Faseb J. 2007, 21: 3063-3074. 10.1096/fj.07-8166com.
Seiderer J, Dambacher J, Kuhnlein B, Pfennig S, Konrad A, Torok HP, Haller D, Goke B, Ochsenkuhn T, Lohse P, Brand S: The role of the selenoprotein S (SELS) gene -105G>A promoter polymorphism in inflammatory bowel disease and regulation of SELS gene expression in intestinal inflammation. Tissue Antigens. 2007, 70: 238-246. 10.1111/j.1399-0039.2007.00888.x.
Hyrenbach S, Pezzini A, del Zotto E, Giossi A, Lichy C, Kloss M, Werner I, Padovani A, Brandt T, Grond-Ginsbach C: No association of the -105 promoter polymorphism of the selenoprotein S encoding gene SEPS1 with cerebrovascular disease. Eur J Neurol. 2007, 14: 1173-1175. 10.1111/j.1468-1331.2007.01898.x.
Moses EK, Johnson MP, Tommerdal L, Forsmo S, Curran JE, Abraham LJ, Charlesworth JC, Brennecke SP, Blangero J, Austgulen R: Genetic association of preeclampsia to the inflammatory response gene SEPS1. Am J Obstet Gynecol. 2008, 198: e1-5.
Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007, 447: 661-678. 10.1038/nature05911.
Acknowledgements
The authors thank Carmen Martínez for her skilful technical assistance. Alfonso Martínez and Jose Luis Santiago hold research FIS contracts (CP04/00175 and CM05/00216, respectively). Jezabel Varadé is a fellow and Elena Urcelay works for the "Fundación para la Investigación Biomédica-Hospital Clínico San Carlos". This work was supported by grants from: Fundación Mutua Madrileña and Fundación Ramón Areces.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
JLS, JV and AnM, carried out the genotyping of the patients and a great part of the controls, participated in the statistical analysis and drafted the manuscript. JLM, HdlC, MDR, JRL and BFG made the diagnosis and collaborated in collection of samples. AM participated in the coordination of the study and participated in the statistical analysis. EGdlC coordinated the study and critically revised the manuscript. EU conceived of the study, participated in the statistical analysis and completed the writing of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Martínez, A., Santiago, J.L., Varadé, J. et al. Polymorphisms in the selenoprotein S gene: lack of association with autoimmune inflammatory diseases. BMC Genomics 9, 329 (2008). https://doi.org/10.1186/1471-2164-9-329
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2164-9-329