Abstract
Background
Interstitial lung diseases (ILD) are chronic inflammatory disorders leading to pulmonary fibrosis. Monocyte chemotactic protein 1 (MCP-1) promotes collagen synthesis and deletion of the MCP-1 receptor CCR2 protects from pulmonary fibrosis in ILD mouse models. We hypothesized that pulmonary MCP-1 and CCR2+ T cells accumulate in pediatric ILD and are related to disease severity.
Methods
Bronchoalveolar lavage fluid was obtained from 25 children with ILD and 10 healthy children. Levels of pulmonary MCP-1 and Th1/Th2-associated cytokines were quantified at the protein and the mRNA levels. Pulmonary CCR2+, CCR4+, CCR3+, CCR5+ and CXCR3+ T cells were quantified by flow-cytometry.
Results
CCR2+ T cells and MCP-1 levels were significantly elevated in children with ILD and correlated with forced vital capacity, total lung capacity and ILD disease severity scores. Children with lung fibrosis had significantly higher MCP-1 levels and CCR2+ T cells in bronchoalveolar lavage fluid compared to non-fibrotic children.
Conclusion
The results indicate that pulmonary CCR2+ T cells and MCP-1 contribute to the pathogenesis of pediatric ILD and might provide a novel target for therapeutic strategies.
Similar content being viewed by others
Background
Interstitial lung diseases (ILD) are chronic inflammatory disorders characterized by restrictive lung disease and diffuse pulmonary infiltrates. Although the precise incidence is not known, ILD are less frequent in children than adults [1–3]. Lungs of ILD patients show inflammation with alveolar wall thickening by leukocytes and pulmonary fibrosis. Despite immunosuppressive treatment and supportive measures, the progressive course leading to irreversible lung fibrosis sometimes can not be prevented. Therefore, the development of additional therapeutic strategies is of high importance.
Monocyte chemotactic protein 1 (MCP-1, CCL2) is produced in response to inflammatory stimuli by a variety of cells, including monocytes/macrophages, lymphocytes and airway epithelial cells [4–6]. MCP-1 stimulates collagen synthesis and production of the pro-fibrotic factor transforming growth factor β (TGF-β) in fibroblasts, while MCP-1 antisense oligonucleotides reduce TGF-β production[7, 8]. Application of MCP-1 into murine lungs induces an inflammatory cytokine response and pulmonary leukocyte accumulation. In adult patients with ILD, increased levels of MCP-1 were observed in serum[9, 10] and bronchoalveolar lavage fluid (BALF) [11–14]. Although MCP-1 was originally described for its chemotactic activity on monocytes, in vitro studies revealed an even higher activity on T cells[15]. This occurs through MCP-1 binding to its sole receptor CCR2[16]. Deletion of the CCR2-gene or receptor blockade with anti-CCR2 antibodies leads to a dramatic inhibition of leukocyte accumulation in murine lungs[17]. Furthermore, CCR2-/- mice are protected from fluorescein (FITC) or bleomycin induced lung fibrosis[18]. Thus far, CCR2+ T cells in BALF of patients with fibrotic lung diseases have not been determined.
In addition to the MCP-1/CCR2 axis, Th2 cytokines seem to mediate pulmonary fibrosis [19–22]. IL-4 stimulates fibroblast proliferation and collagen synthesis[23, 24], while IFN-γ inhibits this process [25–28]. In a Th2 mouse model fibroblasts expressed more CCR2 protein and higher levels of MCP-1 and TGF-β as compared to fibroblasts from a Th1-mouse model[8]. Furthermore, increased levels of IL-4 were observed in animal models of pulmonary fibrosis[29] and lungs of patients with idiopathic pulmonary fibrosis (IPF)[30] or cryptogenic fibrosing alveolitis[31].
The contribution of MCP-1 to ILD has been investigated exclusively in adults. However, the spectrum of ILD differs considerably between adults and children and some forms are unique to children while others, such as idiopathic pulmonary fibrosis (IPF), are extremely rare in childhood[32].
Therefore, we asked whether levels of MCP-1 and frequencies of CCR2+ T cells are increased in BALF of children with ILD and, if so, how levels of MCP-1 and CCR2+ T cells relate to disease severity in pediatric ILD.
To address these questions levels of MCP-1 and frequencies of CCR2+ T cells in BALF were compared between children with ILD and children without lung disease.
To evaluate the contribution of the pulmonary Th1/Th2 micromilieu to the pathogenesis of pediatric ILD, CCR4+ and CCR3+ (Th2) and CCR5+ and CXCR3+ (Th1) cells were determined in BALF together with an array of pulmonary Th1- and Th2-associated cytokines.
Our results indicate that pulmonary CCR2+ T cells and levels of MCP-1 are characteristic components in BALF of children with ILD. A pathophysiological role in pediatric ILD seems likely as their levels relate to restrictive lung function and ILD disease severity.
Methods
Characterization of the patients
Children attending the Department of Pulmonology and Allergology of the University Children's Hospital of Munich during 1999–2004 were considered for inclusion in this study. Children suspective of ILD underwent a comprehensive clinical evaluation, including patient history, physical examination, routine laboratory tests, lung function testing, chest radiography, high resolution computed tomography (HRCT) and bronchoalveolar lavage (BAL). Children were assigned to the ILD group according to the criteria of Fan[33]: (i) ≥3 months of respiratory symptoms characteristic for ILD, i.e. non-productive cough, dyspnoea, tachypnea, crackles and/or rales, exercise intolerance and/or hypoxemia, (ii) diffuse infiltrates on chest radiographs and HRCT and (iii) restrictive lung function (decreased forced vital capacity (FVC) and total lung capacity (TLC)) according to the ATS criteria[34].
The diagnosis of the specific form of ILD was established by patient history, physical examination, HRCT, BAL and/or lung biopsy according to consensus criteria[33, 35]. Two thoracic radiologists independently evaluated all lobes on HRCT for ground glass opacity and pulmonary fibrosis as described previously[36, 37]. A pathologist specialized on pediatric ILD[38] evaluated the lung sections systematically[39, 40]. Furthermore, the disease severity of each ILD patient was characterized using the clinical ILD score of Fan[41]: 1 = asymptomatic, no desaturation; 2 = symptomatic but normoxic (>90%) under all conditions; 3 = symptomatic with desaturation during sleep or with exercise; 4 = symptomatic with desaturation at rest. None of the included children had familial idiopathic pulmonary fibrosis. Patients with congenital heart disease or suspected or proven bacterial pulmonary infection were excluded from the study.
Twenty-five children with ILD (median age: 7 ± 3.6 years; male/female = 16/9) were included (Table 1).
Ten age-matched children were selected as the control group (median age: 7.5 ± 2.9 years, m/f: 6/4). These children were considered as healthy, i.e. had no systemic disease, had no suspected or proven pulmonary disease and were free of respiratory tract infections. These children underwent elective tonsillectomy under general anaesthesia. BAL was performed prior to the surgical procedure.
Ten age-matched children with chronic severe asthma (median age: 8.7 ± 1.6 years, m/f: 5/5), from a previous study[42], who were comparable to the ILD group in terms of gender and age were included as disease control group. All parents and/or patients gave their informed consent prior to bronchoscopy and the institutional review board approved the study protocol.
Bronchoalveolar lavage
Bronchoscopy with BAL was performed as described previously[43]. Residual BALF cells were used for flow cytometry. The BALF recovery and the viability of cells did not differ significantly between the patient groups. Cellular profiles are shown in Table 2.
Flow cytometry
BALF cells were analyzed by four-colour flow cytometry (FACSCalibur, Becton-Dickinson, Heidelberg, Germany) as described previously[42]. The following antibodies were used: CD4-allophycocyanine (APC) mouse IgG1, CD8-phycocyanine 5 (PC5) mouse IgG1 (Immunotech, Marseille, France), CD69-PE mouse IgG1, CCR5-PE mouse IgG2a, CCR4-PE mouse IgG2a (BD Pharmingen, Heidelberg, Germany), CCR2-PE mouse IgG2b, CXCR3-fluorescein isothiocyanate (FITC) mouse IgG1 and CCR3-FITC rat IgG2a (R&D Systems, Wiesbaden, Germany). Mouse IgG1-FITC, mouse IgG1-PE, mouse IgG2a-PE, mouse IgG2b-PE (Immunotech, Marseille, France) and rat IgG2a-FITC (kindly provided by Dr. E. Kremmer, GSF-Institute of Molecular Immunology, Munich, Germany) were used as isotype controls.
Detection of MCP-1 and cytokines
Levels of MCP-1 and Th1 (IL-2, IFN-γ), Th2 (IL-4, IL-5, IL-10) and pro-inflammatory cytokines (TNF-α, IL-6) were quantified by a multiplex, particle-based assay (Bio-Rad Laboratories, Minneapolis, USA) as described previously[42]. The detection limits for all cytokines were 1.5–2.5 pg/ml (min.) and 1000 pg/ml (max.).
Quantitative RT-PCR
BALF cells were lysed in Trizol LS Reagent (Invitrogen, Life Technologies, Karlsruhe, Germany) and were stored at -20°C until mRNA extraction. Total mRNA was isolated according to the manufacturer's instructions and reverse transcribed into cDNA. Contamination with genomic DNA was excluded by mRNA controls without reverse transcriptase in the cDNA synthesis reaction. The following oligonucleotide primers were used: MCP-1 (5-TGAAGCTCGCACTCTCGCCT-3; 5- GTGGAGTGAGTGTTCAAGTC-3); and GAPDH (5-GAGGTGAAGGTCGGAGTC-3; 5-AAGATGGTGATGGGATTTC-3). Expression levels were determined in duplicates by Real time RT-PCR using SYBR green and the iCycler iQ detection system (Biorad, Hercules, CA, USA) according to the manufacturer's instructions. Threshold cycle (CT) values for genes of interest were normalized to GAPDH and used to calculate the relative mRNA expression.
Statistical analysis
The non-parametric Mann-Whitney U test was applied. Correlations were tested with Spearman's rank correlation test. A probability of p < 0.05 was regarded as significant[44] (SPSS statistical program, version 11.5, SPSS Inc. Chicago, USA).
Results
MCP-1 levels and CCR2+ T cells in BALF
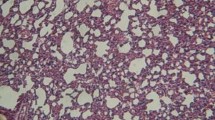
Levels of MCP-1 were significantly higher in children with ILD (n = 25) as compared to the control group at protein and mRNA level (Figure 1A, B). MCP-1 protein and mRNA expression levels correlated positively with each other (r = 0.72, p < 0.01). ILD children with pulmonary fibrosis had significantly higher MCP-1 levels in BALF as compared to children with non-fibrotic ILD (Figure 1C). MCP-1 levels related positively to the stage of disease (Figure 1D). The highest levels of MCP-1 were observed in the three patients who died after respiratory failure (Table 1; P17, P19, P22). Furthermore, MCP-1 levels correlated negatively with restrictive lung function parameters (TLC, FVC) (Figures 2A, B).
MCP-1 levels in children with ILD. MCP-1 levels in bronchoalveolar lavage fluid (BALF) of children with interstitial lung diseases (ILD) and healthy controls are shown at the (A) protein and at the (B) mRNA level. (C) MCP-1 levels in BALF of ILD children with and without pulmonary fibrosis. Pulmonary fibrosis was assessed by computed tomography according to [36,37]. (D) MCP-1 levels in ILD children related to ILD disease severity according to the criteria of Fan [33]. 1 = asymptomatic, no desaturation; 2 = symptomatic but normoxic (> 90%) under all conditions; 3 = symptomatic with desaturation during sleep or exercise; 4 = symptomatic with desaturation at rest; MCP-1 protein levels were quantified in BALF by a multiplex, particle-based assay (Bio-Rad Laboratories, Minneapolis, USA) as described previously [42]. MCP-1 mRNA levels were quantified in BALF cells by Real time RT-PCR using SYBR green and the iCycler iQ detection system (Biorad, Hercules, CA, USA) and were normalized to GAPDH. Median values are shown by horizontal bars. Differences between the patient groups were tested with the Mann-Whitney U test; * p < 0.05, *** p < 0.001; Children with systemic corticosteroid therapy are shown as grey circles. P: Pulmonary alveolar proteinosis; S: Sarcoidosis; † symbolize children who died due to respiratory failure.
Correlation of MCP-1 levels with lung function parameters in children with ILD. MCP-1 levels in bronchoalveolar lavage fluid (BALF) correlated with (A) forced vital capacity (FVC) and (B) total lung capacity (TLC) in children with interstitial lung disease (ILD). FVC and TLC are shown as % of predicted. MCP-1 levels in BALF were quantified by a multiplex, particle-based assay; P: Pulmonary alveolar proteinosis; S: Sarcoidosis;
To test whether increased MCP-1 levels are associated with increased frequencies of CCR2+ T cells, BALF lymphocytes were quantified by flow cytometry. CCR2 was expressed on a higher percentage of CD4+ than CD8+ T cells. The majority of CCR2+ T cells showed an activated phenotype (75% CCR2+CD69+). Children with ILD had significantly higher percentages of CCR2+CD4+and CCR2+CD8+ T cells in BALF as compared to control children (Figure 3A). Similar to MCP-1, percentages of CCR2+CD4+ cells were significantly higher in ILD children with pulmonary fibrosis as compared to children with non-fibrotic ILD (Figure 3B). Again, the highest percentages of CCR2+CD4+ T cells were observed in the three deceased patients and CCR2+CD4+ cells related positively to the stage of ILD (Figure 4). Furthermore, percentages of CCR2+CD4+ T cells correlated negatively with FVC and TLC in ILD patients (Figures 5A, B). Pulmonary levels of MCP-1 correlated positively with CCR2+CD4+ T cells (Figure 5C). No association between MCP-1/CCR2+ cells and immunosuppressive treatment was found in ILD patients.
CCR2+T cells in children with ILD. (A) Percentages of CCR2+CD4+ and CCR2+CD8+ T cells in in bronchoalveolar lavage fluid (BALF) of children with interstitial lung diseases (ILD) and healthy children. (B) Percentages of CCR2+CD4+ and CCR2+CD8+ T cells in BALF of children with and without pulmonary fibrosis. Percentages of CCR2+CD4+ and CCR2+CD8+ T cells were analyzed in BALF by flow cytometry. Pulmonary fibrosis was assessed by computed tomography according to [36,37]. Median values are shown by horizontal bars. Differences between the patient groups were tested with the Mann-Whitney U test; * p < 0.05; *** p < 0.001; Children with systemic corticosteroid therapy are shown as grey circles. P: Pulmonary alveolar proteinosis; S: Sarcoidosis; † symbolize the children who died due to respiratory failure.
CCR2+CD4+T cells and ILD disease severity. Percentages of CCR2+CD4+ T cells in bronchoalveolar lavage fluid (BALF) of children with interstitial lung disease (ILD) related to ILD disease severity. Percentages of CCR2+CD4+ T cells were analyzed in BALF by flow cytometry. ILD disease severity was scored according to the ILD score of Fan(40): 1 = asymptomatic, no desaturation; 2 = symptomatic but normoxic (> 90%) under all conditions; 3 = symptomatic with desaturation during sleep or with exercise; 4 = symptomatic with desaturation at rest; Median values are shown by horizontal bars. Differences between the patient groups were tested with the Mann-Whitney U test; * p < 0.05, ** p < 0.01; Children with systemic corticosteroid therapy are shown as grey circles. P: Pulmonary alveolar proteinosis; S: Sarcoidosis; † symbolize the children who died due to respiratory failure.
CCR2+CD4+T cells and lung function parameters in children with ILD. Correlation of CCR2+CD4+ T cells in bronchoalveolar lavage fluid (BALF) with (A) forced vital capacity (FVC) and (B) total lung capacity (TLC) in children with interstitial lung diseases (ILD). Correlation of percentages of CCR2+CD4+ T cells with levels of MCP-1 in BALF of children with ILD (C). FVC and TLC are shown as % of predicted. Percentages of CCR2+CD4+ T cells were analyzed in BALF by flow cytometry. P: Pulmonary alveolar proteinosis; S: Sarcoidosis
To verify if increased levels of MCP-1 and percentages of CCR2+ T cells are characteristic for pediatric ILD, we analyzed these markers in ten selected age-matched children with well-characterized allergic asthma who are described in detail in a previous study[42]. Levels of MCP-1 and CCR2+ T cells from asthmatic children were in the range of the control group and did not correlate with each other (data not shown).
To assess the value of CCR2+CD4+ T cells and MCP-1 levels in the longitudinal course, three consecutive therapeutical BALs were analyzed in three patients with PAP (P17, P18, P19) and one patient with cholesterol pneumonitis (P22). Two PAP patients (P17, P19) and the patient with cholesterol pneumonitis worsened in the clinical course continuously (increasing oxygen requirement, increasing dyspnoe) and died from respiratory failure, while one PAP patient remained clinically stable (P18). The deceased PAP patients had continuously rising levels of MCP-1 and increasing percentages of CCR2+CD4+ T cells in the three follow-up BALs (Figures 6A, B; black circles) while the clinically stable patient showed steady levels of MCP-1 and percentages of CCR2+CD4+ T cells (Figures 6A, B; white circles).
Longitudinal analysis of MCP-1 levels and CCR2+CD4+T cells. Longitudinal analysis of (A) MCP-1 levels and (B) CCR2+CD4+ T cells in three consecutive bronchoalveolar lavage fluids (BALF) of four children with interstitial lung diseases, including two children with pulmonary alveolar proteinosis (P) and one child with cholesterol pneumonitis (CP). The child with cholesterol pneumonitis and one child with pulmonary alveolar proteinosis died by respiratory failure (†), while one child with pulmonary alveolar proteinosis stayed clinically stable. † symbolize the childen who died. MCP-1 levels were quantified in BALF by a multiplex, particle-based assay. Percentages of CCR2+CD4+ T cells were analyzed in BALF by flow cytometry.
Th1- and Th2-lymphocytes and cytokines in BALF
To test whether increased CCR2+ T cells and levels of MCP-1 were paralleled by a pulmonary Th1/Th2-shift, CCR4+ and CCR3+(Th2) and CCR5+an d CXCR3+ (Th1) cells were determined in BALF together with an array of pulmonary Th1/Th2 cytokines.
Children with ILD had significantly higher percentages of CCR4+CD4+ (Th2) cells as compared to control children (Figure 7A). CCR4 was predominantly expressed on CD4+ cells. The majority of CCR4+CD4+ cells had an activated phenotype (68% CCR4+CD69+). CCR3+ (Th2) cells were not detectable in BALF. Percentages of CCR5+ and CXCR3+ T cells (both Th1) were low and did not differ among the patient groups (Figures 7B, C).
Pulmonary CCR4+, CCR5+, and CXCR3+T cells. Percentages of (A) CCR4+CD4+, CCR4+CD8+, (B) CCR5+CD4+ and CCR5+CD8+ and (C) CXCR3+CD4+ and CXCR3+CD8+ T cells in bronchoalveolar lavage fluid (BALF) are shown in children with interstitial lung diseases (ILD) and healthy controls. Percentages of CCR4+CD4+, CCR4+CD8+, CCR5+CD4+, CCR5+CD8+, CXCR3+CD4+ and CXCR3+CD8+ T cells were analyzed in BALF by flow cytometry. Median values are shown by horizontal bars. Differences between the patient groups were tested with the Mann-Whitney U test; * p < 0.05; ** p < 0.01
Levels of IFN-γ were increased in ILD patients (p < 0.05), whereas the remaining cytokines did not differ among the patient groups (data not shown).
Discussion
The present work demonstrates that BALF levels of MCP-1 are consistently increased in pediatric ILD. This is accompanied by increased frequencies of the corresponding CCR2 + T cells. Levels of MCP-1 and frequencies of CCR2+ T cells were higher in fibrotic than in non-fibrotic forms of ILD and correlated with restrictive lung function parameters and ILD disease severity, indicating a relevance of the MCP-1/CCR2 axis in the pathogenesis of pediatric ILD. Infiltrating T cells are a characteristic feature of pulmonary tissue from ILD patients[45] and T cells in BALF were found to correlate with T cells in pulmonary tissue[46]. In line with previous findings[47, 48], T cells were increased in BALF of our children with ILD as compared to control patients, suggesting a contribution of T cells to the pathogenesis of pediatric ILD. Studies in adult patients indicated that MCP-1 plays a role in the pathogenesis of different forms of ILD, including IPF[9, 12, 13], PAP[11, 14], sarcoidosis[12], scleroderma with lung involvement[49] and granulomatous lung diseases[50]. Serum levels of MCP-1 were significantly elevated in adult patients with ILD[9, 51] and were closely related to the clinical course[9]. However, as outlined above, ILD in children differs noticeably from ILD in adulthood. Pediatric ILD is extremely rare and little data exist with respect to pathoimmunological mechanisms. Thus, it is very hard to study a large patient group and to find enough children for each ILD subtype. We found elevated levels of MCP-1 and CCR2+ T cells in various etiologies of ILD, which suggests a common pulmonary T cell response for various forms of pediatric ILD.
Thus far, frequencies of BALF CCR2+ T cells in human ILD have not been determined. The parallel increase of MCP-1 and CCR2+ T cells in BALF of ILD children further substantiates the importance of this chemokine and its receptor in the pathogenesis of ILD, as suggested by mouse models. In these models, the relevance of the MCP-1/CCR2 interaction was mainly addressed with respect to pulmonary fibrosis. Our children with pulmonary fibrosis had increased levels of MCP-1 and increased percentages of CCR2+ cells compared to children with non-fibrotic ILD. However, MCP-1 levels and percentages of CCR2+ T cells were elevated both in fibrotic and non-fibrotic ILD children as compared to controls. In addition, MCP-1 and CCR2+ T cells were also elevated in pediatric PAP that usually does not progress to pulmonary fibrosis. In fact, one of the three patients with the highest levels of MCP-1 and CCR2+ T cells had PAP without any indication of fibrosis. Similar observations were made recently for MCP-1 in adult PAP patients[11]. A possible biological relevance of MCP-1 levels and CCR2+ T cells in pediatric ILD is further suggested by their correlation with restrictive lung function parameters and the ILD disease severity score and by the finding that the deceased children with the most severe course of disease exhibited the highest BALF levels of these markers. The possibility that MCP-1 and CCR2+ T cells are a general phenomenon of pediatric lung diseases seems very unlikely, since these markers were present only at low levels in BALF of children with severe allergic asthma. This is in line with findings in an Aspergillus-induced allergic mouse model, where a Th2-mediated lung pathology occured in the absence of MCP-1 or CCR2[52].
To assess the value of CCR2+ T cells and MCP-1 levels in the longitudinal course of children with ILD, three consecutive BALs were performed in four children with ILD including three ILD patients who died and one patient who stayed clinically stable. The three deceased children had high and continuously rising levels of MCP-1 and CCR2+CD4+ T cells, while the stable patient had low levels of MCP-1 and percentages of CCR2+CD4+ T cells. Thus, levels of MCP-1 and percentages of CCR2+CD4+ T cells might reflect the disease progression in pediatric ILD.
Interestingly, immunosuppressive treatment was not associated with altered levels of MCP-1 and CCR2+ T cells in BALF (data not shown). This is in contrast to a study of Suga et al.[9] in adult ILD patients where serum levels of MCP-1 were closely related to the effectiveness of corticosteroid therapy. Given the assumption that MCP-1 and CCR2 are important players in the pathophysiology of ILD in children, the lack of association with corticosteroid therapy might explain, at least in part, why corticosteroids are sometimes unable to control the progression of pediatric ILD.
Several studies indicated that MCP-1 and CCR2 are involved in Th1[53, 54] and Th2 immunity [55–58]. Furthermore, it has been suggested that ILD and pulmonary fibrosis are associated with a Th2 immune response[20–22, 59–61]. Experiments in mice showed that a lack of MCP-1[62] leads to decreased Th1 responses while MCP-1 over-expression[58] results in increased levels of Th2 cytokines. Th1/Th2 cytokine levels in BALF were low or undetectable in BALF of our children. However, CCR4+CD4+ T cells were moderately but significantly elevated in ILD patients. On the other hand, CCR4+CD4+ T cells are clearly less frequent in ILD compared to allergic asthma[42]. Thus, a strong Th2 response seems unlikely in our ILD patients. Beneath T-cells, MCP-1 attracts CCR2+ monocytes/macrophages[63]. In mouse models, MCP-1 was found to attract monocytes to the inflamed lung, which was accompanied by a concomitant downregulation of pulmonary MCP-1 levels[64]. We found no difference in the percentage of CCR2+ alveolar macrophages in BALF between children with ILD and control children or between fibrotic and non-fibrotic forms of ILD (data not shown). Instead, we found a strong correlation between percentages of CCR2+ T cells and levels of MCP-1 in BALF of ILD patients. Therefore, we assume that pulmonary MCP-1 acts on CCR2+ T cells, which accumulate in the BALF of children with ILD.
Conclusion
In conclusion, CCR2+ T cells and levels of MCP-1 are characteristic components in BALF of children with ILD. A pathophysiological role in pediatric ILD seems likely as their levels relate to restrictive lung function and ILD disease severity. Therefore, pharmacological targeting of the MCP-1/CCR2 axis might represent an additional option for the treatment of ILD in children.
Abbreviations
- BAL(F):
-
Bronchoalveolar lavage (fluid)
- CC:
-
CC chemokine receptor
- CXC:
-
CXC chemokine receptor
- FVC:
-
Forced vital capacity
- IFN-γ:
-
Interferon-γ
- IL-:
-
Interleukin
- IPF:
-
Idiopathic pulmonary fibrosis
- IPH:
-
Idiopathic pulmonary hemosiderosis
- LIP:
-
Lymphocytic interstitial pneumonia
- MCP-1:
-
Monocyte chemotactic protein 1 (CCL2)
- PAP:
-
Pulmonary alveolar proteinosis
- TGF-β:
-
Transforming growth factor β
- Th1/Th2:
-
T helper cell 1/2
- TLC:
-
Total lung capacity
- TNF-α:
-
Tumor necrosis factor-α
References
Clement A, Allen J, Corrin B, Dinwiddie R, le Pointe HD, Eber E, et al.: Task force on chronic interstitial lung disease in immunocompetent children. European Respiratory Journal 2004, 24:686–697.
Bush A: Diagnosis of interstitial lung disease. Pediatric Pulmonology 1996, 22:81–82.
Hartl D, Griese M: Interstitial lung disease in children – genetic background and associated phenotypes. Respiratory Research 2005., 8:
Yoshimura T, Leonard EJ: Human Monocyte Chemoattractant Protein-1 (MCP-1) – Secretion by Human-Fibroblasts. Journal of Leukocyte Biology 1989, 46:331.
Yoshimura T, Yuhki N, Moore SK, Appella E, Lerman MI, Leonard EJ: Human Monocyte Chemoattractant Protein-1 (MCP-1) – Full-Length Cdna Cloning, Expression in Mitogen-Stimulated Blood Mononuclear Leukocytes, and Sequence Similarity to Mouse Competence Gene Je. FEBS Letters 1989, 244:487–493.
Lundien MC, Mohammed KA, Nasreen N, Tepper RS, Hardwick JA, Sanders KL, et al.: Induction of MCP-1 expression in airway epithelial cells: Role of CCR2 receptor in airway epithelial injury. Journal of Clinical Immunology 2002, 22:144–152.
GharaeeKermani M, Denholm EM, Phan SH: Costimulation of fibroblast collagen and transforming growth factor beta(1) gene expression by monocyte chemoattractant protein-1 via specific receptors. Journal of Biological Chemistry 1996, 271:17779–17784.
Hogaboam GM, Bone-Larson CL, Lipinski S, Lukacs NW, Chensue SW, Strieter RM, et al.: Differential monocyte chemoattractant protein-1 and chemokine receptor 2 expression by murine lung fibroblasts derived from Th1-and Th2-type pulmonary granuloma models. Journal of Immunology 1999, 163:2193–2201.
Suga M, Iyonaga K, Ichiyasu H, Saita N, Yamasaki H, Ando M: Clinical significance of MCP-1 levels in BALF and serum in patients with interstitial lung diseases. European Respiratory Journal 1999, 14:376–382.
Iyonaga K, Suga M, Ichiyasu H, Yamamoto T, Hiraga Y, Ando M: Measurement of serum monocyte chemoattractant protein-1 and its clinical application for estimating the activity of granuloma formation in sarcoidosis. Sarcoidosis Vasculitis and Diffuse Lung Diseases 1998, 15:165–172.
Bonfield TL, John N, Malur A, Barna BP, Culver DA, Kavuru MS, et al.: Elevated monocyte chemotactic proteins 1, 2, and 3 in pulmonary alveolar proteinosis are associated with chemokine receptor suppression. Clinical Immunology 2005, 114:79–85.
Car BD, Meloni F, Luisetti M, Semenzato G, Gialdronigrassi G, Walz A: Elevated Il-8 and Mcp-1 in the Bronchoalveolar Lavage Fluid of Patients with Idiopathic Pulmonary Fibrosis and Pulmonary Sarcoidosis. American Journal of Respiratory and Critical Care Medicine 1994, 149:655–659.
Iyonaga K, Takeya M, Saita N, Sakamoto O, Yoshimura T, Ando M, et al.: Monocyte Chemoattractant Protein-1 in Idiopathic Pulmonary Fibrosis and Other Interstitial Lung-Diseases. Human Pathology 1994, 25:455–463.
Iyonaga K, Suga M, Yamamoto T, Ichiyasu H, Miyakawa H, Ando M: Elevated bronchoalveolar concentrations of MCP-1 in patients with pulmonary alveolar proteinosis. European Respiratory Journal 1999, 14:383–389.
Carr MW, Roth SJ, Luther E, Rose SS, Springer TA: Monocyte Chemoattractant Protein-1 Acts As A T-Lymphocyte Chemoattractant. Proceedings of the National Academy of Sciences of the United States of America 1994, 91:3652–3656.
Murphy PM, Baggiolini M, Charo IF, Hebert CA, Horuk R, Matsushima K, et al.: International union of pharmacology. XXII. Nomenclature for chemokine receptors. Pharmacological Reviews 2000, 52:145–176.
Maus U, von Grote K, Kuziel WA, Mack M, Miller EJ, Cihak J, et al.: The role of CC chemokine receptor 2 in alveolar monocyte and neutrophil immigration in intact mice. American Journal of Respiratory and Critical Care Medicine 2002, 166:268–273.
Moore BB, Paine R, Christensen PJ, Moore TA, Sitterding S, Ngan R, et al.: Protection from pulmonary fibrosis in the absence of CCR2 signaling. Journal of Immunology 2001, 167:4368–4377.
Wynn TA: Fibrotic disease and the Th1/Th2 paradigm. Nature Reviews Immunology 2004, 4:583–594.
Lukacs NW, Hogaboam C, Chensue SW, Blease K, Kunkel SL: Type 1/type 2 cytokine paradigm and the progression of pulmonary fibrosis. Chest 2001, 120:5S-8S.
Jakubzick C, Choi ES, Carpenter KJ, Kunkel SL, Evanoff H, Martinez FJ, et al.: Human pulmonary fibroblasts exhibit altered interleukin-4 and interleukin-13 receptor subunit expression in idiopathic interstitial pneumonia. American Journal of Pathology 2004, 164:1989–2001.
Jakubzick C, Choi ES, Kunkel SL, Evanoff H, Martinez FJ, Puri RK, et al.: Augmented pulmonary IL-4 and IL-13 receptor subunit expression in idiopathic interstitial pneumonia. Journal of Clinical Pathology 2004, 57:477–486.
Monroe JG, Haldar S, Prystowsky MB, Lammie P: Lymphokine Regulation of Inflammatory Processes – Interleukin-4 Stimulates Fibroblast Proliferation. Clinical Immunology and Immunopathology 1988, 49:292–298.
Postlethwaite AE, Holness MA, Katai H, Raghow R: Human Fibroblasts Synthesize Elevated Levels of Extracellular-Matrix Proteins in Response to Interleukin-4. Journal of Clinical Investigation 1992, 90:1479–1485.
Duncan MR, Berman B: Gamma-Interferon Is the Lymphokine and Beta-Interferon the Monokine Responsible for Inhibition of Fibroblast Collagen Production and Late But Not Early Fibroblast Proliferation. Journal of Experimental Medicine 1985, 162:516–527.
Serpier H, Gillery P, SalmonEhr V, Garnotel R, Georges N, Kalis B, et al.: Antagonistic effects of interferon-gamma and interleukin-4 on fibroblast cultures. Journal of Investigative Dermatology 1997, 109:158–162.
Yuan WH, Yufit T, Li LY, Mori Y, Chen SJ, Varga J: Negative modulation of (alpha 1(I) procollagen gene expression in human skin fibroblasts: Transcriptional inhibition by interferon-gamma. Journal of Cellular Physiology 1999, 179:97–108.
Oldroyd SD, Thomas GL, Gabbiani G, El Nahas AM: Interferon-gamma inhibits experimental renal fibrosis. Kidney International 1999, 56:2116–2127.
Buttner C, Skupin A, Reimann T, Rieber EP, Unteregger G, Geyer P, et al.: Local production of interleukin-4 during radiation-induced pneumonitis and pulmonary fibrosis in rats: Macrophages as a prominent source of interleukin-4. American Journal of Respiratory Cell and Molecular Biology 1997, 17:315–325.
Emura M, Nagai S, Takeuchi M, Kitaichi M, Izumi T: In vitro Production of B-Cell Growth-Factor and B-Cell Differentiation Factor by Peripheral-Blood Mononuclear-Cells and Bronchoalveolar Lavage Lymphocytes-T from Patients with Idiopathic Pulmonary Fibrosis. Clinical and Experimental Immunology 1990, 82:133–139.
Wallace WAH, Ramage EA, Lamb D, Howie SEM: A Type-2 (Th2-Like) Pattern of Immune-Response Predominates in the Pulmonary Interstitium of Patients with Cryptogenic Fibrosing Alveolitis (CFA). Clinical and Experimental Immunology 1995, 101:436–441.
Fan LL, Langston C: Pediatric interstitial lung disease – Children are not small adults. American Journal of Respiratory and Critical Care Medicine 2002, 165:1466–1467.
Fan LL, Kozinetz CA, Deterding RR, Brugman SM: Evaluation of a diagnostic approach to pediatric interstitial lung disease. Pediatrics 1998, 101:82–85.
[Anon]: Standardization of Spirometry – 1994 Update. American Journal of Respiratory and Critical Care Medicine 1995, 152:1107–1136.
Agusti C: American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. American Journal of Respiratory and Critical Care Medicine 2002., 165:
Kazerooni EA, Martinez FJ, Flint A, Jamadar DA, Gross BH, Spizarny DL, et al.: Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: Correlation with pathologic scoring. American Journal of Roentgenology 1997, 169:977–983.
Copley SJ, Coren M, Nicholson AG, Rubens MB, Bush A, Hansell DM: Diagnostic accuracy of thin-section CT and chest radiography of pediatric interstitial lung disease. American Journal of Roentgenology 2000, 174:549–554.
Brasch F, Muller KM: Classification of pulmonary alveolar proteinosis in newborns, infants, and children. Pathologe 2004, 25:299–309.
[Anon]: Idiopathic pulmonary fibrosis: Diagnosis and treatment – International consensus statement. American Journal of Respiratory and Critical Care Medicine 2000, 161:646–664.
Coren ME, Nicholson AG, Goldstraw P, Bush A: Open lung biopsy in the investigation of diffuse lung disease in children. American Journal of Respiratory and Critical Care Medicine 1999, 159:A779.
Fan LL, Langston C: Chronic Interstitial Lung-Disease in Children. Pediatric Pulmonology 1993, 16:184–196.
Hartl D, Griese M, Nicolai T, Zissel G, Prell C, Konstantopoulos N, et al.: Pulmonary chemokines and their receptors differentiate children with asthma and chronic cough. Journal of Allergy and Clinical Immunology 2005, 115:728–736.
Griese M, Felber J, Reiter K, Strong P, Reid K, Belohradsky BH, et al.: Airway inflammation in children with tracheostomy. Pediatric Pulmonology 2004, 37:356–361.
Motulsky H: Intuitive biostatistics. New York: Oxford University Press; 1995.
Katzenstein ALA, Myers JL: Idiopathic pulmonary fibrosis – Clinical relevance of pathologic classification. American Journal of Respiratory and Critical Care Medicine 1998, 157:1301–1315.
Semenzato G, Bortolin M, Facco M, Tassinari C, Sancetta R, Agostini C: Lung lymphocytes: Origin, biological functions, and laboratory techniques for their study in immune-mediated pulmonary disorders. Critical Reviews in Clinical Laboratory Sciences 1996, 33:423–455.
Ronchetti R, Midulla F, Sandstrom T, Bjermer L, Zebrak J, Pawlik J, et al.: Bronchoalveolar lavage in children with chronic diffuse parenchymal lung disease. Pediatric Pulmonology 1999, 27:395–402.
Tessier V, Chadelat K, Baculard A, Housset B, Clement A: BAL in children – A controlled study of differential cytology and cytokine expression profiles by alveolar cells in pediatric sarcoidosis. Chest 1996, 109:1430–1438.
Luzina IG, Atamas SP, Wise R, Wigley FM, Xiao HQ, White B: Gene expression in bronchoalveolar lavage cells from scleroderma patients. American Journal of Respiratory Cell and Molecular Biology 2002, 26:549–557.
Oshima M, Maeda A, Ishioka S, Hiyama K, Yamakido M: Expression of C-C chemokines in bronchoalveolar lavage cells from patients with granulomatous lung diseases. Lung 1999, 177:229–240.
Ohnishi H, Yokoyama A, Kondo K, Hamada H, Abe M, Nishimura K, et al.: Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. American Journal of Respiratory and Critical Care Medicine 2002, 165:378–381.
Koth LL, Rodriguez MW, Bernstein XL, Chan S, Huang XZ, Charo IF, et al.: Aspergillus antigen induces robust Th2 cytokine production, inflammation, airway hyperreactivity and fibrosis in the absence of MCP-1 or CCR2. Respiratory Research 2004., 5:
Traynor TR, Herring AC, Dorf ME, Kuziel WA, Toews GB, Huffnagle GB: Differential roles of CC chemokine ligand 2/monocyte chemotactic protein-1 and CCR2 in the development of T1 immunity. Journal of Immunology 2002, 168:4659–4666.
Boring L, Gosling J, Chensue SW, Kunkel SL, Farese RV, Broxmeyer HE, et al.: Impaired monocyte migration and reduced type 1 (Th1) cytokine responses in C-C chemokine receptor 2 knockout mice. Journal of Clinical Investigation 1997, 100:2552–2561.
Chonsue SW, Boring L, Warmington KS, Ruth JR, Charo IF, Kunkel SL: Effect of C-C chemokine receptor 2 (CCR2) knockout on Schistosomal egg antigen-elicited granuloma formation and the regional lymphoid response. Faseb Journal 1998, 12:A646.
Gu L, Tseng S, Horner RM, Tam C, Loda M, Rollins BJ: Control of Th2 polarization by the chemokine monocyte chemoattractant protein-1. Nature 2000, 404:407–411.
Kim Y, Sung SSJ, Kuziel WA, Feldman S, Fu SM, Rose CE: Enhanced airway Th2 response after allergen challenge in mice deficient in CC chemokine receptor-2 (CCR2). Journal of Immunology 2001, 166:5183–5192.
Matsukawa A, Lukacs NW, Standiford TJ, Chensue SW, Kunkel SL: Adenoviral-mediated overexpression of monocyte chemoattractant protein-1 differentially alters the development of Th1 and Th2 type responses in vivo. Journal of Immunology 2000, 164:1699–1704.
Belperio JA, Dy M, Murray L, Burdick MD, Xue YY, Strieter RM, et al.: The role of the Th2CC chemokine ligand CCL17 in pulmonary fibrosis. Journal of Immunology 2004, 173:4692–4698.
Kunkel SL, Strieter RM: Cytokine Networking in Lung Inflammation. Hospital Practice 1990, 25:63.
Selman M: Plunging into the chaos of the cytokine/chemokine cocktail in pulmonary fibrosis – How many and how important are they? American Journal of Respiratory and Critical Care Medicine 2003, 168:730–731.
Lu B, Rutledge BJ, Gu L, Fiorillo J, Lukacs NW, Kunkel SL, et al.: Abnormalities in monocyte recruitment and cytokine expression in monocyte chemoattractant protein 1-deficient mice. Journal of Experimental Medicine 1998, 187:601–608.
Maus U, von Grote K, Kuziel WA, Mack M, Miller EJ, Cihak J, et al.: The role of CC chemokine receptor 2 in alveolar monocyte and neutrophil immigration in intact mice. American Journal of Respiratory and Critical Care Medicine 2002, 166:268–273.
Maus UA, Wellmann S, Hampl C, Kuziel WA, Srivastava M, Mack M, et al.: CCR2-positive monocytes recruited to inflamed lungs downregulate local CCL2 chemokine levels. American Journal of Physiology-Lung Cellular and Molecular Physiology 2005, 288:L350-L358.
Acknowledgements
This work was supported by grants from the Else-Kröner-Fresenius Stiftung, the Friedrich-Baur-Stiftung, by a grant of the University and Science Program of the Ludwig-Maximilians-University (HWP) and by the Clinical Cooperation Groups "Pediatric Immune Regulation" and "Immune Monitoring". We thank Cory M. Hogaboam, Department of Pathology, University of Michigan Medical School, Ann Arbor, for helpful discussions and critical revision of the mansucript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
DH carried out the experimental analyses and wrote the manuscript. MG characterized the study population, performed bronchoalveolar lavage and participated in the study design. TN performed bronchoalveolar lavage and patient characterization. GZ and CP participated in the experimental analyses. DR and DJS participated in the study design and reviewed the manuscript. SKE designed the study, supervised the experimental analyses and wrote the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hartl, D., Griese, M., Nicolai, T. et al. A role for MCP-1/CCR2 in interstitial lung disease in children. Respir Res 6, 93 (2005). https://doi.org/10.1186/1465-9921-6-93
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1465-9921-6-93