Abstract
Idiopathic pulmonary fibrosis (IPF) is a chronic, fibrosing interstitial lung disease that primarily affects older adults. Median survival after diagnosis is 2–3 years. The clinical course of IPF may include periods of acute deterioration in respiratory function, which are termed acute exacerbations of IPF (AEx-IPF) when a cause cannot be identified. AEx-IPF may represent a sudden acceleration of the underlying disease process of IPF, or a biologically distinct pathological process that is clinically undiagnosed. An AEx-IPF can occur at any time during the course of IPF and may be the presenting manifestation. The incidence of AEx-IPF is hard to establish due to variation in the methodology used to assess AEx-IPF in different studies, but AEx-IPF are believed to occur in between 5 and 10% of patients with IPF every year. Risk factors for AEx-IPF are unclear, but there is evidence that poorer lung function increases the risk of an AEx-IPF and reduces the chances of a patient surviving an AEx-IPF. The presence of comorbidities such as gastroesophageal reflux disease (GERD) and pulmonary hypertension may also increase the risk of an AEx-IPF. AEx-IPF are associated with high morbidity and mortality. Patients who experience an AEx-IPF show a worsened prognosis and AEx-IPF are believed to reflect disease progression in IPF. Current treatments for AEx-IPF have only limited data to support their effectiveness. The latest international treatment guidelines state that supportive care remains the mainstay of treatment for AEx-IPF, but also give a weak recommendation for the treatment of the majority of patients with AEx-IPF with corticosteroids. There is emerging evidence from clinical trials of investigational therapies that chronic treatment of IPF may reduce the incidence of AEx-IPF. Additional clinical trials investigating this are underway.
Similar content being viewed by others
Introduction
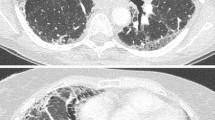
Idiopathic pulmonary fibrosis (IPF) is a chronic, fibrosing interstitial pneumonia of unknown cause that occurs primarily in older adults [1]. In the United States, the incidence of IPF has been estimated to be between 6.8 and 8.8 cases per 100,000 person years using narrow case definitions, and between 16.3 and 17.4 cases per 100,000 person years using broad case definitions [2]. IPF is rare in patients under 50 years, with patients typically presenting in their fifties or sixties [1]. The prognosis of IPF is poor, with a median survival time after diagnosis of 2 to 3 years [3]; death generally occurs as a result of progressive respiratory failure [1, 4]. However, the course of IPF is highly variable. Some patients progress rapidly, others much more slowly, while some patients experience periods of relative stability punctuated by acute deteriorations in respiratory function (Figure 1) [1, 4, 5]. If a cause of this deterioration cannot be identified (e.g. infection, pulmonary embolism), this deterioration is termed an acute exacerbation of IPF (AEx-IPF) [1, 6]. This review focuses on the evidence on the impact, management and possible prevention of AEx-IPF.
Schematic representation of clinical disease courses in patients with IPF. There are several possible disease courses in patients with IPF. Patients may experience rapid disease progression (line A) or a much more gradual progression of disease (line C), while some patients exhibit periods of relative stability punctuated by periods of acute worsening (stars) (line B). Where the cause of the acute deterioration cannot be identified, the deterioration is termed an acute exacerbation of IPF. Reproduced from Ley B, Collard HR, King TE Jr: Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011, 183:431–440. Reprinted with permission of the American Thoracic Society. Copyright © 2013 American Thoracic Society.
Definition of AEx-IPF
A universally agreed definition of an AEx-IPF has not been established. Clinical studies have used a variety of criteria to define AEx-IPF, which differ in factors such as whether chest X-ray, or high-resolution computed tomography (HRCT) is required, how hypoxemia is defined, and the conditions that must be ruled out [7–14]. Variation in the definitions and methodology used to assess AEx-IPF has complicated researchers’ and physicians’ understanding of AEx-IPF and their impact.
In 2007, a consensus definition for AEx-IPF was proposed by an expert committee sponsored by the IPF Clinical Research Network and the National Heart Lung and Blood Institute (NHLBI), in an attempt to standardize the diagnostic criteria used across studies [6]. This committee defined AEx-IPF as an acute, clinically significant deterioration of unidentifiable cause and proposed five diagnostic criteria (Table 1) [6]. This definition has become the most widely used definition of AEx-IPF and has been used in several clinical studies [13, 15–19].
Incidence of AEx-IPF
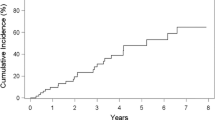
The true incidence of AEx-IPF remains unclear. Reported incidences vary widely across studies, due to the lack of a consistent definition and differences in study methodology and patient selection [20, 21]. The most recent international guidelines, issued jointly by the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS) and Latin American Thoracic Association (ALAT) on the diagnosis and treatment of IPF state that AEx-IPF occurs in approximately 5–10% of patients with diagnosed IPF annually [1]. A recent retrospective study of data collected from 461 patients with diagnosed IPF found 1-year and 3-year incidences of AEx-IPF of 14.2% and 20.7%, respectively [19]. However, the incidence rates of AEx-IPF reported in clinical trials have tended to be lower than this.
Pathophysiology of AEx-IPF
A variety of patterns of acute lung injury have been observed in AEx-IPF [22]. The most common histopathological finding is diffuse alveolar damage superimposed on the underlying usual interstitial pneumonia (UIP) pattern [6, 8, 9, 11, 12, 23, 24], but organizing pneumonia and extensive fibroblastic foci have also been reported [22].
Several hypotheses for the etiology of AEx-IPF have been proposed. AEx-IPF may represent a sudden acceleration of the underlying disease process due to unknown acute injury to the lung, or a biologically distinct pathological process due to a clinically occult condition, such as infection or gastroesophageal reflux disease (GERD) [6]. As AEx-IPF have a clinical presentation that shares a number of features with viral respiratory infections (e.g. fever, cough, myalgia), it has been suggested that occult viral infection may contribute to the pathophysiology of AEx-IPF [20, 25, 26]. However, the evidence supporting the involvement of viral infections in AEx-IPF is mixed [1, 20, 25]. The most recent and extensive study, which used genomic-based technologies to investigate the role of viruses in the etiology of AEx-IPF, suggested that viral infection is not a common cause of AEx-IPF [27].
Although research is ongoing into gene expression patterns and the identification of biomarkers, the molecular mechanisms underlying AEx-IPF remain poorly understood. Activation of the immune system, disordered coagulation/fibrinolysis, and oxidative stress may all contribute to the pathophysiology of AEx-IPF. Immune cells (e.g. neutrophils, macrophages) [12, 28, 29], inflammatory mediators (e.g. interleukin 6, high mobility group protein B1) [30, 31], markers of coagulation/fibrinolysis (e.g. protein C, thrombomodulin, and plasma activator inhibitor-1) [30], and markers of oxidative stress (thioredoxin 1) [32] are all elevated in patients with AEx-IPF.
Epithelial cell damage in patients with IPF is demonstrated by over-expression of matrix metalloproteinase (MMP)-7 [33], MMP-9 [34], and Krebs von den Lungen-6 (KL-6) [30]. Accelerated epithelial cell proliferation, with increases in the proliferation markers CCNA2 and Ki-67, in patients with AEx-IPF may be a compensatory response to injury, and is associated with epithelial cell death [33]. Transforming growth factor (TGF)-beta, a fibrogenic cytokine, is upregulated in IPF [35], and galectin-3, a mediator of fibrosis induced by TGF-beta, is elevated in the lungs and serum of patients with stable IPF and AEx-IPF [36]. Circulating bone marrow-derived fibrocytes may also provide a source of lung fibroblasts and myofibroblasts, as the number of circulating fibrocytes has been shown to be higher in patients with IPF and AEx-IPF, compared with healthy subjects [37, 38].
Risk factors and precipitating factors for AEx-IPF
An AEx-IPF can occur at any time during the course of IPF and, for some patients, may be the presenting manifestation [1, 11, 23, 39]. Risk factors for AEx-IPF are unclear, but there is evidence that a number of factors may increase risk. Lower total lung capacity, lower forced vital capacity (FVC) and/or lower diffusing capacity of the lung for carbon monoxide (DLco) have been shown to increase the risk of AEx-IPF [3, 19], as has a greater decline in FVC over time [40, 41].
A higher degree of dyspnea (score ≥2 on the modified Medical Research Council dyspnea scale) [40] or of fibrosis on HRCT [42] has been shown to increase the risk of AEx-IPF, as has the presence of concomitant conditions such as emphysema [3] or pulmonary hypertension [43]. However, age does not appear to be an independent predictor of the risk of an AEx-IPF [6]. Invasive examinations such as bronchoscopy [18], bronchoalveolar lavage (BAL) [11, 44, 45], and pulmonary resection for lung cancer [42] can precipitate AEx-IPF, although these exacerbations may be regarded as complications of these procedures rather than true exacerbations. There is some evidence from a number of small, retrospective studies that surgical lung biopsy is a precipitating factor for AEx-IPF; however, the risk of AEx-IPF from video-assisted thoracoscopic operation appears to be elevated only in patients with severe physiologic impairment or substantial comorbidity [46].
GERD, a common comorbidity in patients with IPF, may contribute to the pathogenesis of IPF through introduction of gastric acid into the respiratory tree [16, 47, 48]. In some patients with AEx-IPF, pepsin levels were found to be elevated in BAL fluid, suggesting a possible role for GERD in the pathogenesis of AEx-IPF [47]. There is some evidence to suggest that the treatment of GERD in patients with IPF reduces mortality rates [49, 50].
Impact of AEx-IPF on patients
The latest international guidelines for the management of IPF state that the occurrence of AEx-IPF is consistent with disease progression [1]. The precise impact of AEx-IPF on IPF, such as which and to what extent disease processes are accelerated following an AEx-IPF, and how AEx-IPF affect the lives of patients with IPF who survive them, is difficult to determine. However, AEx-IPF are certainly a leading cause of hospitalization [51] and death [40, 51, 52] among patients with IPF. Median survival after an AEx-IPF has been reported to be between 22 days and 4.2 months [18, 19, 40]. Reported in-hospital mortality rates vary widely, between 27% and 96% [18, 19, 23, 53]. In a retrospective review of 461 patients with IPF, 96 (21%) patients were hospitalized for AEx-IPF over a median follow-up period of 22.9 months [19]. Patients with an AEx-IPF had a lower median survival time than those who had not suffered an AEx-IPF (15.5 months vs. 60.6 months from the diagnosis of IPF) and lower 5-year survival rates (18.4% vs. 50.0%). There is some evidence that patients with better lung function (FVC, PaO2, DLCO) prior to AEx-IPF are more likely to survive an AEx-IPF [18, 54], suggesting that preservation of lung function may be an important way of reducing the impact of AEx-IPF in patients with IPF.
Management of AEx-IPF
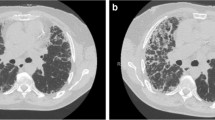
The latest international treatment guidelines state that supportive care remains the mainstay of treatment for AEx-IPF, but also give a weak recommendation for the treatment of the majority of patients with AEx-IPF with corticosteroids, based on anecdotal reports of benefit and the high mortality associated with AEx-IPF [1]. In clinical practice, the treatment of AEx-IPF is variable. Corticosteroids (e.g. prednisone, methylprednisolone) are used in the majority of patients who suffer an AEx-IPF, usually in pulse doses [9, 12, 18, 28, 53]. Preliminary data suggest that response to high-dose corticosteroid treatment may depend on the type of HRCT lesion, with better responses achieved in those with a peripheral pattern [8]. Broad-spectrum antibiotics and immunosuppressants (cyclosporin or cyclophosphamide) are sometimes used in addition to corticosteroids [28]. However, the efficacy of immunosuppressants in the treatment of AEx-IPF is based on a few small retrospective studies that do not provide conclusive evidence for benefit [54–56].
A small prospective clinical trial of anticoagulation in IPF published in 2005 reported improved survival in the anticoagulation group, mostly due to reduced mortality associated with AEx-IPF suggesting the efficacy of anticoagulation in the treatment of AEx-IPF; however, debate remained about the benefits of anticoagulation therapy in patients with IPF due to the small size and methodological limitations of this study [51]. The ACE-IPF trial, a randomized, double-blind, placebo-controlled study of warfarin as a treatment for IPF, was terminated early on the recommendation of the Data and Safety Monitoring Board due to higher mortality in the warfarin arm and a low likelihood of benefit [57] and the use of anticoagulants in patients with IPF is now discouraged.
Mechanical ventilation is often used in patients with AEx-IPF, but the data on its effects on outcomes are mixed [11, 28, 30, 53, 58]. Other treatments for AEx-IPF that have been investigated in small studies include polymyxin B-immobilized fiber column (PMX) hemoperfusion [7, 59] and tacrolimus, a cytokine transcription inhibitor [60], usually administered in addition to corticosteroids.
There is some evidence that delaying the initiation of treatment following AEx-IPF is associated with worse mortality rates. In a retrospective review of 37 AEx-IPF experienced by 27 patients, patients who were discharged had a significantly shorter delay between admission and initiation of treatment than those who died in hospital (mean 3.1 days vs. 6.0 days) [18]. In this study, all of the patients received oxygen therapy, most received methylprednisolone and antibiotics and some received cyclophosphamide [18].
Reducing the risk of exacerbations
Clinical trials of several investigational treatments for IPF have evaluated whether chronic treatment of IPF reduces the incidence of AEx-IPF. A trial of sildenafil, a phosphodiesterase-5 inhibitor, showed a numerical reduction in AEx-IPF in patients given sildenafil versus placebo (3 [3.4%] vs. 7 [7.6%]), but the number of events was small and the difference was not statistically significant [61]. In trials of imatinib, a tyrosine kinase inhibitor [62], bosentan, an endothelin receptor antagonist [63], the anticoagulant warfarin [57], and inhaled N-acetylcysteine [15], numerically higher rates of AEx-IPF were found in the active treatment arms compared with the placebo arms. Further, in the PANTHER-IPF trial, which investigated triple therapy with prednisone, azathioprine, and N-acetylcysteine in patients with IPF, a significantly higher rate of AEx-IPF was observed in patients receiving triple therapy versus placebo [17]. Indeed this arm of the study was terminated prematurely after a mean follow-up of 32 weeks due to a significantly higher mortality and hospitalization rates in patients receiving triple therapy versus placebo [17]. Interferon gamma-1b showed similar rates of AEx-IPF compared with placebo in the INSPIRE study, which was prematurely terminated due to the absence of a benefit on mortality [64].
Pirfenidone, an anti-fibrotic molecule that has been licensed for the treatment of IPF in Japan, India, China, Europe, and Canada, but was not approved in the United States, has shown inconsistent effects on AEx-IPF. A Phase II study in Japanese patients with IPF was terminated after 9 months of a planned 1-year follow-up based on a higher frequency of AEx-IPF in the placebo group than in the pirfenidone 1800 mg/day group [10]. However, in a Phase III trial in Japanese patients, no significant differences were observed in the incidence of AEx-IPF between patients treated with pirfenidone (1800 or 1200 mg/day) or placebo for 52 weeks [41]. Pirfenidone was investigated in two 72-week Phase III randomized, placebo-controlled trials conducted in thirteen countries: CAPACITY 1 and CAPACITY 2 [13]. Neither of these studies showed a significant difference between groups in time to worsening of IPF, the definition of which included the time to an AEx-IPF, death, lung transplantation, or admission to hospital for respiratory problems. An additional Phase III trial of pirfenidone is ongoing (ASCEND; NCT01366209).
Nintedanib (formerly known as BIBF 1120) is a tyrosine kinase inhibitor in clinical development for the treatment of IPF. In the Phase II, 12-month, randomized, placebo-controlled TOMORROW trial, a lower incidence of AEx-IPF was observed in patients treated with nintedanib 300 mg/day than placebo (2.4 vs. 15.7 AEx-IPF per 100 patient years) [14]. However, these results should be interpreted with a degree of caution, as the incidence of AEx-IPF was a secondary endpoint, with no adjustment for multiple comparisons, and the discontinuation rate in the nintedanib 300 mg/day group was higher than in the placebo group (37.6% vs. 28.2%) [14]. It is interesting that nintedanib may have an effect on AEx-IPF whereas the tyrosine kinase inhibitor imatinib, which inhibits the platelet-derived growth factor receptor (PDGFR), did not [62]. Nintedanib is an inhibitor of PDGFR, vascular endothelial growth factor receptor (VEGFR), and fibroblast growth factor receptor (FGFR) [65] and this specificity of inhibition may be key to its effects on AEx-IPF. In pre-clinical studies, nintedanib has demonstrated anti-fibrotic and anti-inflammatory effects that may influence the course of IPF [66, 67]. The effect of nintedanib on the progression of IPF and on AEx-IPF remains to be established and is being investigated in two ongoing 52-week Phase III trials (INPULSIS-1 and INPULSIS-2; NCT01335464 and NCT01335477). In these trials, the criteria used to diagnose AEx-IPF are similar to those defined by the IPF Clinical Research Network [6] and cases of suspected AEx-IPF will be adjudicated by an independent committee.
Finally, a recent study using prospective data from 242 patients in the placebo groups of three randomized clinical trials showed that patients who used anti-acid treatments (proton-pump inhibitors or histamine-receptor-2 blockers) at baseline had fewer AEx-IPF than those not taking such treatments at baseline (zero vs. nine events after a mean follow-up of 30 weeks) [68]. The authors hypothesized that anti-acid treatment might decrease the frequency of AEx-IPF by reducing the acidity of the microaspirate and suggested that controlled clinical trials of anti-acid treatments are needed.
Conclusions
IPF is a progressive disease and all patients will deteriorate over time. However, IPF has a highly variable disease course. Some patients with IPF suffer AEx-IPF, which are associated with high morbidity and mortality and a worsened prognosis. The methodology used to define AEx-IPF has varied across studies, making it difficult to form an accurate understanding of the incidence and clinical implications of AEx-IPF. More data are needed on the impact of AEx-IPF on patients with IPF. Current treatments for AEx-IPF have only limited data to support their effectiveness and supportive therapy remains the mainstay of care. There is emerging evidence that chronic treatment of IPF may reduce the risk of AEx-IPF and clinical trials investigating this are underway.
Author’s contributions
The author was fully responsible the content of this review article.
Abbreviations
- AEx-IPF:
-
Acute exacerbation(s) of idiopathic pulmonary fibrosis
- ALAT:
-
Latin American Thoracic Association
- ATS:
-
American Thoracic Society
- BAL:
-
Bronchoalveolar lavage
- DLco:
-
Diffusing capacity of the lung for carbon monoxide
- ERS:
-
European Respiratory Society
- FGFR:
-
Fibroblast growth factor receptor
- FVC:
-
Forced vital capacity
- GERD:
-
Gastroesophageal reflux disease
- HRCT:
-
High-resolution computed tomography
- IPF:
-
Idiopathic pulmonary fibrosis
- JRS:
-
Japanese Respiratory Society
- KL-6:
-
Krebs von den Lungen-6
- MMP:
-
Matrix metalloproteinase
- NHLBI:
-
National Heart Lung and Blood Institute
- PaO2:
-
Arterial oxygen tension
- PDGFR:
-
Platelet-derived growth factor receptor
- PMX:
-
Polymyxin B-immobilized fiber column
- TGF:
-
Transforming growth factor
- UIP:
-
Usual interstitial pneumonia
- VEGFR:
-
Vascular endothelial growth factor receptor.
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ, ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis: An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011, 183: 788-824. 10.1164/rccm.2009-040GL.
Nalysnyk L, Cid-Ruzafa J, Rotella P, Esser D: Incidence and prevalence of idiopathic pulmonary fibrosis: review of the literature. Eur Respir Rev. 2012, 21: 355-361. 10.1183/09059180.00002512.
Mura M, Porretta MA, Bargagli E, Sergiacomi G, Zompatori M, Sverzellati N, Taglieri A, Mezzasalma F, Rottoli P, Saltini C, Rogliani P: Predicting survival in newly diagnosed idiopathic pulmonary fibrosis: a 3-year prospective study. Eur Respir J. 2012, 40: 101-109. 10.1183/09031936.00106011.
Martinez FJ, Safrin S, Weycker D, Starko KM, Bradford WZ, King TE, Flaherty KR, Schwartz DA, Noble PW, Raghu G, Brown KK, IPF Study Group: The clinical course of patients with idiopathic pulmonary fibrosis. Ann Intern Med. 2005, 142: 963-967. 10.7326/0003-4819-142-12_Part_1-200506210-00005.
Kim DS, Collard HR, King TE: Classification and natural history of the idiopathic interstitial pneumonias. Proc Am Thorac Soc. 2006, 3: 285-292. 10.1513/pats.200601-005TK.
Collard HR, Moore BB, Flaherty KR, Brown KK, Kaner RJ, King TE, Lasky JA, Loyd JE, Noth I, Olman MA, Raghu G, Roman J, Ryu JH, Zisman DA, Hunninghake GW, Colby TV, Egan JJ, Hansell DM, Johkoh T, Kaminski N, Kim DS, Kondoh Y, Lynch DA, Müller-Quernheim J, Myers JL, Nicholson AG, Selman M, Toews GB, Wells AU, Martinez FJ, Idiopathic Pulmonary Fibrosis Clinical Research Network Investigators: Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007, 176: 636-643. 10.1164/rccm.200703-463PP.
Abe S, Azuma A, Mukae H, Ogura T, Taniguchi H, Bando M, Sugiyama Y: Polymyxin B-immobilized fiber column (PMX) treatment for idiopathic pulmonary fibrosis with acute exacerbation: a multicenter retrospective analysis. Intern Med. 2012, 51: 1487-1491. 10.2169/internalmedicine.51.6965.
Akira M, Hamada H, Sakatani M, Kobayashi C, Nishioka M, Yamamoto S: CT findings during phase of accelerated deterioration in patients with idiopathic pulmonary fibrosis. AJR Am J Roentgenol. 1997, 168: 79-83. 10.2214/ajr.168.1.8976924.
Ambrosini V, Cancellieri A, Chilosi M, Zompatori M, Trisolini R, Saragoni L, Poletti V: Acute exacerbation of idiopathic pulmonary fibrosis: report of a series. Eur Respir J. 2003, 22: 821-826. 10.1183/09031936.03.00022703.
Azuma A, Nukiwa T, Tsuboi E, Suga M, Abe S, Nakata K, Taguchi Y, Nagai S, Itoh H, Ohi M, Sato A, Kudoh S: Double-blind, placebo-controlled trial of pirfenidone in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2005, 171: 1040-1047. 10.1164/rccm.200404-571OC.
Kim DS, Park JH, Park BK, Lee JS, Nicholson AG, Colby T: Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J. 2006, 27: 143-150. 10.1183/09031936.06.00114004.
Kondoh Y, Taniguchi H, Kawabata Y, Yokoi T, Suzuki K, Takagi K: Acute exacerbation in idiopathic pulmonary fibrosis. Analysis of clinical and pathologic findings in three cases. Chest. 1993, 103: 1808-1812. 10.1378/chest.103.6.1808.
Noble PW, Albera C, Bradford WZ, Costabel U, Glassberg MK, Kardatzke D, King TE, Lancaster L, Sahn SA, Szwarcberg J, Valeyre D, Du Bois RM, CAPACITY Study Group: Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011, 377: 1760-1769. 10.1016/S0140-6736(11)60405-4.
Richeldi L, Costabel U, Selman M, Kim DS, Hansell DM, Nicholson AG, Brown KK, Flaherty KR, Noble PW, Raghu G, Brun M, Gupta A, Juhel N, Klueglich M, Du Bois RM: Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med. 2011, 365: 1079-1087. 10.1056/NEJMoa1103690.
Bando M, Hosono T, Mato N, Nakaya T, Yamasawa H, Ohno S, Sugiyama Y: Long-term efficacy of inhaled N-acetylcysteine in patients with idiopathic pulmonary fibrosis. Intern Med. 2010, 49: 2289-2296. 10.2169/internalmedicine.49.4011.
Lee JS, Collard HR, Raghu G, Sweet MP, Hays SR, Campos GM, Golden JA, King TE: Does chronic microaspiration cause idiopathic pulmonary fibrosis?. Am J Med. 2010, 123: 304-311. 10.1016/j.amjmed.2009.07.033.
Raghu G, Anstrom KJ, King TE, Lasky JA, Martinez FJ: Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012, 366: 1968-1977.
Simon-Blancal V, Freynet O, Nunes H, Bouvry D, Naggara N, Brillet PY, Denis D, Cohen Y, Vincent F, Valeyre D, Naccache JM: Acute exacerbation of idiopathic pulmonary fibrosis: outcome and prognostic factors. Respiration. 2012, 83: 28-35. 10.1159/000329891.
Song JW, Hong SB, Lim CM, Koh Y, Kim DS: Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J. 2011, 37: 356-363. 10.1183/09031936.00159709.
Hyzy R, Huang S, Myers J, Flaherty K, Martinez F: Acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2007, 132: 1652-1658. 10.1378/chest.07-0299.
Kim DS: Acute exacerbation of idiopathic pulmonary fibrosis. Clin Chest Med. 2012, 33: 59-68. 10.1016/j.ccm.2012.01.001.
Churg A, Muller NL, Silva CI, Wright JL: Acute exacerbation (acute lung injury of unknown cause) in UIP and other forms of fibrotic interstitial pneumonias. Am J Surg Pathol. 2007, 31: 277-284. 10.1097/01.pas.0000213341.70852.9d.
Parambil JG, Myers JL, Ryu JH: Histopathologic features and outcome of patients with acute exacerbation of idiopathic pulmonary fibrosis undergoing surgical lung biopsy. Chest. 2005, 128: 3310-3315. 10.1378/chest.128.5.3310.
Rice AJ, Wells AU, Bouros D, Du Bois RM, Hansell DM, Polychronopoulos V, Vassilakis D, Kerr JR, Evans TW, Nicholson AG: Terminal diffuse alveolar damage in relation to interstitial pneumonias. An autopsy study. Am J Clin Pathol. 2003, 119: 709-714. 10.1309/UVARMDY8FE9FJDKU.
Vannella KM, Moore BB: Viruses as co-factors for the initiation or exacerbation of lung fibrosis. Fibrogenesis Tissue Repair. 2008, 1: 2-10.1186/1755-1536-1-2.
Yoshizawa Y: Idiopathic pulmonary fibrosis: acute exacerbation and lung cancer associated with pulmonary fibrosis. Jpn Med Assoc J. 2003, 46: 490-496.
Wootton SC, Kim DS, Kondoh Y, Chen E, Lee JS, Song JW, Huh JW, Taniguchi H, Chiu C, Boushey H, Lancaster LH, Wolters PJ, DeRisi J, Ganem D, Collard HR: Viral infection in acute exacerbation of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011, 183: 1698-1702. 10.1164/rccm.201010-1752OC.
Agarwal R, Jindal SK: Acute exacerbation of idiopathic pulmonary fibrosis: a systematic review. Eur J Intern Med. 2008, 19: 227-235. 10.1016/j.ejim.2007.04.024.
Mukae H, Liboshi H, Nakazato M, Hiratsuka T, Tokojima M, Abe K, Ashitani J, Kadota J, Matsukura S, Kohno S: Raised plasma concentrations of alpha-defensins in patients with idiopathic pulmonary fibrosis. Thorax. 2002, 57: 623-628. 10.1136/thorax.57.7.623.
Collard HR, Calfee CS, Wolters PJ, Song JW, Hong SB, Brady S, Ishizaka A, Jones KD, King TE, Matthay MA, Kim DS: Plasma biomarker profiles in acute exacerbation of idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2010, 299: L3-L7. 10.1152/ajplung.90637.2008.
Ebina M, Taniguchi H, Miyasho T, Yamada S, Shibata N, Ohta H, Hisata S, Ohkouchi S, Tamada T, Nishimura H, Ishizaka A, Maruyama I, Okada Y, Takashi K, Nukiwa T: Gradual increase of high mobility group protein b1 in the lungs after the onset of acute exacerbation of idiopathic pulmonary fibrosis. Pulm Med. 2011, 2011: 916486-
Iwata Y, Okamoto M, Hoshino T, Kitasato Y, Sakazaki Y, Tajiri M, Matsunaga K, Azuma K, Kawayama T, Kinoshita T, Imaoka H, Fujimoto K, Kato S, Yano H, Aizawa H: Elevated levels of thioredoxin 1 in the lungs and sera of idiopathic pulmonary fibrosis, non-specific interstitial pneumonia and cryptogenic organizing pneumonia. Intern Med. 2010, 49: 2393-2400. 10.2169/internalmedicine.49.4049.
Konishi K, Gibson KF, Lindell KO, Richards TJ, Zhang Y, Dhir R, Bisceglia M, Gilbert S, Yousem SA, Song JW, Kim DS, Kaminski N: Gene expression profiles of acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2009, 180: 167-175. 10.1164/rccm.200810-1596OC.
Suga M, Iyonaga K, Okamoto T, Gushima Y, Miyakawa H, Akaike T, Ando M: Characteristic elevation of matrix metalloproteinase activity in idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2000, 162: 1949-1956. 10.1164/ajrccm.162.5.9906096.
Willis BC, Borok Z: TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007, 293: L525-L534. 10.1152/ajplung.00163.2007.
Mackinnon AC, Gibbons MA, Farnworth SL, Leffler H, Nilsson UJ, Delaine T, Simpson AJ, Forbes SJ, Hirani N, Gauldie J, Sethi T: Regulation of transforming growth factor-β1-driven lung fibrosis by galectin-3. Am J Respir Crit Care Med. 2012, 185: 537-546. 10.1164/rccm.201106-0965OC.
Mehrad B, Burdick MD, Zisman DA, Keane MP, Belperio JA, Strieter RM: Circulating peripheral blood fibrocytes in human fibrotic interstitial lung disease. Biochem Biophys Res Commun. 2007, 353: 104-108. 10.1016/j.bbrc.2006.11.149.
Moeller A, Gilpin SE, Ask K, Cox G, Cook D, Gauldie J, Margetts PJ, Farkas L, Dobranowski J, Boylan C, O’Byrne PM, Strieter RM, Kolb M: Circulating fibrocytes are an indicator of poor prognosis in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2009, 179: 588-594. 10.1164/rccm.200810-1534OC.
Sakamoto K, Taniguchi H, Kondoh Y, Ono K, Hasegawa Y, Kitaichi M: Acute exacerbation of idiopathic pulmonary fibrosis as the initial presentation of the disease. Eur Respir Rev. 2009, 18: 129-132. 10.1183/09059180.00000409.
Kondoh Y, Taniguchi H, Katsuta T, Kataoka K, Kimura T, Nishiyama O, Sakamoto K, Johkoh T, Nishimura M, Ono K, Kitaichi M: Risk factors of acute exacerbation of idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2010, 27: 103-110.
Taniguchi H, Ebina M, Kondoh Y, Ogura T, Azuma A, Suga M, Taguchi Y, Takahashi H, Nakata K, Sato A, Takeuchi M, Raghu G, Kudoh S, Nukiwa T: Pirfenidone Clinical Study Group in Japan: Pirfenidone in idiopathic pulmonary fibrosis. Eur Respir J. 2010, 35: 821-829. 10.1183/09031936.00005209.
Suzuki H, Sekine Y, Yoshida S, Suzuki M, Shibuya K, Yonemori Y, Hiroshima K, Nakatani Y, Mizuno S, Takiguchi Y, Yoshino I: Risk of acute exacerbation of interstitial pneumonia after pulmonary resection for lung cancer in patients with idiopathic pulmonary fibrosis based on preoperative high-resolution computed tomography. Surg Today. 2011, 41: 914-921. 10.1007/s00595-010-4384-z.
Judge EP, Fabre A, Adamali HI, Egan JJ: Acute exacerbations and pulmonary hypertension in advanced idiopathic pulmonary fibrosis. Eur Respir J. 2012, 40: 93-100. 10.1183/09031936.00115511.
Hiwatari N, Shimura S, Takishima T, Shirato K: Bronchoalveolar lavage as a possible cause of acute exacerbation in idiopathic pulmonary fibrosis patients. Tohoku J Exp Med. 1994, 174: 379-386. 10.1620/tjem.174.379.
Sakamoto K, Taniguchi H, Kondoh Y, Wakai K, Kimura T, Kataoka K, Hashimoto N, Nishiyama O, Hasegawa Y: Acute exacerbation of IPF following diagnostic bronchoalveolar lavage procedures. Respir Med. 2012, 106: 436-442. 10.1016/j.rmed.2011.11.006.
Kaarteenaho R: The current position of surgical lung biopsy in the diagnosis of idiopathic pulmonary fibrosis. Respir Res. 2013, 14: 43-10.1186/1465-9921-14-43.
Lee JS, Song JW, Wolters PJ, Elicker BM, King TE, Kim DS, Collard HR: Bronchoalveolar lavage pepsin in acute exacerbation of idiopathic pulmonary fibrosis. Eur Respir J. 2012, 39: 352-358. 10.1183/09031936.00050911.
Tobin RW, Pope CE, Pellegrini CA, Emond MJ, Sillery J, Raghu G: Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998, 158: 1804-1808. 10.1164/ajrccm.158.6.9804105.
Lee JS, Ryu JH, Elicker BM, Lydell CP, Jones KD, Wolters PJ, King TE, Collard HR: Gastroesophageal reflux therapy is associated with longer survival in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011, 184: 1390-1394. 10.1164/rccm.201101-0138OC.
Raghu G, Yang ST, Spada C, Hayes J, Pellegrini CA: Sole treatment of acid gastroesophageal reflux in idiopathic pulmonary fibrosis: a case series. Chest. 2006, 129: 794-800. 10.1378/chest.129.3.794.
Kubo H, Nakayama K, Yanai M, Suzuki T, Yamaya M, Watanabe M, Sasaki H: Anticoagulant therapy for idiopathic pulmonary fibrosis. Chest. 2005, 128: 1475-1482. 10.1378/chest.128.3.1475.
Daniels CE, Yi ES, Ryu JH: Autopsy findings in 42 consecutive patients with idiopathic pulmonary fibrosis. Eur Respir J. 2008, 32: 170-174. 10.1183/09031936.00176307.
Al-Hameed FM, Sharma S: Outcome of patients admitted to the intensive care unit for acute exacerbation of idiopathic pulmonary fibrosis. Can Respir J. 2004, 11: 117-122.
Morawiec E, Tillie-Leblond I, Pansini V, Salleron J, Remy-Jardin M, Wallaert B: Exacerbations of idiopathic pulmonary fibrosis treated with corticosteroids and cyclophosphamide pulses. Eur Respir J. 2011, 38: 1487-1489. 10.1183/09031936.00127311.
Inase N, Sawada M, Ohtani Y, Miyake S, Isogai S, Sakashita H, Miyazaki Y, Yoshizawa Y: Cyclosporin A followed by the treatment of acute exacerbation of idiopathic pulmonary fibrosis with corticosteroid. Intern Med. 2003, 42: 565-570. 10.2169/internalmedicine.42.565.
Sakamoto S, Homma S, Miyamoto A, Kurosaki A, Fujii T, Yoshimura K: Cyclosporin A in the treatment of acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2010, 49: 109-115. 10.2169/internalmedicine.49.2359.
Noth I, Anstrom KJ, Calvert SB, De Andrade J, Flaherty KR, Glazer C, Kaner RJ, Olman MA, Idiopathic Pulmonary Fibrosis Clinical Research Network (IPFnet): A placebo-controlled randomized trial of warfarin in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2012, 186: 88-95. 10.1164/rccm.201202-0314OC.
Yokoyama T, Kondoh Y, Taniguchi H, Kataoka K, Kato K, Nishiyama O, Kimura T, Hasegawa R, Kubo K: Noninvasive ventilation in acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2010, 49: 1509-1514. 10.2169/internalmedicine.49.3222.
Seo Y, Abe S, Kurahara M, Okada D, Saito Y, Usuki J, Azuma A, Koizumi K, Kudoh S: Beneficial effect of polymyxin B-immobilized fiber column (PMX) hemoperfusion treatment on acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2006, 45: 1033-1038. 10.2169/internalmedicine.45.6018.
Horita N, Akahane M, Okada Y, Kobayashi Y, Arai T, Amano I, Takezawa T, To M, To Y: Tacrolimus and steroid treatment for acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2011, 50: 189-195. 10.2169/internalmedicine.50.4327.
Zisman DA, Schwarz M, Anstrom KJ, Collard HR, Flaherty KR, Hunninghake GW: A controlled trial of sildenafil in advanced idiopathic pulmonary fibrosis. N Engl J Med. 2010, 363: 620-628.
Daniels CE, Lasky JA, Limper AH, Mieras K, Gabor E, Schroeder DR: Imatinib treatment for idiopathic pulmonary fibrosis: randomized placebo-controlled trial results. Am J Respir Crit Care Med. 2010, 181: 604-610. 10.1164/rccm.200906-0964OC.
King TE, Brown KK, Raghu G, Du Bois RM, Lynch DA, Martinez F, Valeyre D, Leconte I, Morganti A, Roux S, Behr J: BUILD-3: a randomized, controlled trial of bosentan in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011, 184: 92-99. 10.1164/rccm.201011-1874OC.
King TE, Albera C, Bradford WZ, Costabel U, Hormel P, Lancaster L, Noble PW, Sahn SA, Szwarcberg J, Thomeer M, Valeyre D, Du Bois RM, INSPIRE Study Group: Effect of interferon gamma-1b on survival in patients with idiopathic pulmonary fibrosis (INSPIRE): a multicentre, randomised, placebo-controlled trial. Lancet. 2009, 374: 222-228. 10.1016/S0140-6736(09)60551-1.
Hilberg F, Roth GJ, Krssak M, Kautschitsch S, Sommergruber W, Tontsch-Grunt U, Garin-Chesa P, Bader G, Zoephel A, Quant J, Heckel A, Rettig WJ: BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008, 68: 4774-4782. 10.1158/0008-5472.CAN-07-6307.
Hostettler KE, Papakonstantinou E, Klagas I, Karakiulakis G, Zhong J, Tamm M, Lardinois D, Roth M: Anti-fibrotic effects of nintedanib (BIBF 1120) in primary human lung fibroblasts derived from patients with idiopathic pulmonary fibrosis and from non-fibrotic controls. Am J Respir Crit Care Med. 2013, 187: A3374-
Wollin L, Neugebauer J, Ostermann A, Holweg A, Wex E, Ehinger K, Maertens M, Gantner F: Sustained inactivation of human lung fibroblasts by nintedanib. Am J Respir Crit Care Med. 2013, 187: A3378-
Lee JS, Collard HR, Anstrom KJ, Martinez FJ, Noth I, Roberts RS, Yow E, Raghu G: Anti-acid treatment and disease progression in idiopathic pulmonary fibrosis: an analysis of data from three randomised controlled trials. Lancet Respir Med. 2013, 1: 369-376. 10.1016/S2213-2600(13)70105-X.
Acknowledgments
Medical writing assistance, supported financially by Boehringer Ingelheim Pharmaceuticals, Inc, was provided by Clare Ryles and Wendy Morris of Fleishman-Hillard Group, Ltd during the preparation of this manuscript. The author was fully responsible for all content and editorial decisions, was involved at all stages of manuscript development, and has approved the final version of the review, which reflects the author’s interpretation and conclusions. Boehringer Ingelheim was given the opportunity to check the data used in the review article for factual accuracy only.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
DSK has acted as a consultant, steering committee member, and advisory board member for Boehringer Ingelheim, which is developing nintedanib as a treatment for IPF. The article processing charge for this article has been covered by Boehringer Ingelheim.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kim, D.S. Acute exacerbations in patients with idiopathic pulmonary fibrosis. Respir Res 14, 86 (2013). https://doi.org/10.1186/1465-9921-14-86
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1465-9921-14-86