Abstract
Background
Data describing real-life management and treatment of community-acquired pneumonia (CAP) in Europe are limited. REACH (NCT01293435) was a retrospective, observational study collecting data on the management of EU patients hospitalized with CAP.
The purpose of this study was to understand patient and disease characteristics in patients hospitalized with CAP and to review current clinical practices and outcomes.
Methods
Patients were aged ≥18 years, hospitalized with CAP between March 2010 and February 2011, and requiring in-hospital treatment with intravenous antibiotics. An electronic Case Report Form was used to collect patient, disease and treatment variables, including type of CAP, medical history, treatment setting, antibiotics administered and clinical outcomes.
Results
Patients (N = 2,039) were recruited from 128 centres in ten EU countries (Belgium, France, Germany, Greece, Italy, the Netherlands, Portugal, Spain, Turkey, UK). The majority of patients were aged ≥65 years (56.4%) and had CAP only (78.8%). Initial antibiotic treatment modification occurred in 28.9% of patients and was more likely in certain groups (patients with comorbidities; more severely ill patients; patients with healthcare-associated pneumonia, immunosuppression or recurrent episodes of CAP). Streamlining (de-escalation) of therapy occurred in 5.1% of patients. Mean length of hospital stay was 12.6 days and overall mortality was 7.2%.
Conclusion
These data provide a current overview of clinical practice in patients with CAP in EU hospitals, revealing high rates of initial antibiotic treatment modification. The findings may precipitate reassessment of optimal management regimens for hospitalized CAP patients.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP) has an incidence rate of around 1 case per 1000 population per year in the EU [1] and is associated with considerable morbidity and mortality worldwide, with up to 68.8% of patients requiring hospitalization [1–4]. Previous studies show that patient outcomes are influenced by a number of factors, of which the decision to hospitalize and rapidity of initiation of antibiotic treatment are most important. The decision regarding site of care is critical [5, 6] as low-risk patients may be vulnerable to worsened outcomes when treated in the hospital environment [6], and hospitalization for CAP is responsible for up to 80% of the total costs of this disease [7]. In bacterial pneumonia, rapid selection and initiation of appropriate antibiotic therapy is vital, shortening the illness course and significantly reducing the risk of complications or mortality [8]. Treatment decisions are complicated by the difficulty of obtaining a microbiological diagnosis, and empirical treatment, instead of pathogen-directed therapy, is standard [9]. Further, the ongoing development and shifting global patterns of antibiotic resistance may compromise effectiveness of previously useful antibiotics [10]. Finally, the choices of therapy available, both generic and branded, are numerous.
While the factors driving patient outcomes in CAP are increasingly understood, data on patient morbidity and mortality and associated resource use in Europe are scarce. Information is available mainly from individual countries rather than the whole continent and reports vary widely or are out of date [11]. Furthermore, comprehensive information on CAP management patterns in the real-life setting across Europe and their impact on patient outcomes is not available.
Therefore, we performed a retrospective observational study in ten EU countries (REACH; Retrospective Study to Assess the Clinical Management of Patients With Moderate-to-Severe Complicated Skin and Soft Tissue Infections (cSSTI) or CAP in the Hospital Setting) designed to create a better understanding of clinical management of these infections in response to current, real-world challenges. The study is a collaboration involving independent experts in CAP or cSSTI, a health economist, and clinical investigators across Europe, funded by AstraZeneca. The cSSTI data are reported separately elsewhere (Garau et al. submitted).
The CAP component reported here had two main objectives: to collect detailed background data on patients hospitalized with CAP in Europe, and to provide a summary of clinical practice decisions in these patients and their impact in terms of initial antibiotic treatment modification rates, associated length of hospital stay and mortality.
Methods
Overview
REACH (NCT01293435) was a multinational, multicentre, observational, retrospective cohort study of patients hospitalized with CAP. Patients were enrolled from 128 sites in ten EU countries; Belgium, France, Germany, Greece, Italy, the Netherlands, Portugal, Spain, Turkey and the UK (see Additional file 1: Appendix 2 for full list of investigators). The study was performed according to Good Clinical Practice and the Declaration of Helsinki. All local ethics committees approved the study protocol. Local legislation relating to written informed consent for non-interventional studies was followed in each country; in Germany and Portugal, where this information is mandatory, written informed consent was collected.
Patients
The population comprised patients with CAP requiring hospitalization identified between December 2010 and January 2011. All patients complying with relevant disease codes (Additional file 1: Appendix 1) in the World Health Organization International Classification of Diseases 10th revision (ICD-10; 2007 version) were included [12]. The window for hospitalizations could be extended backward to March 2010 and forward to February 2011 until sufficient patients were identified. Patients to be included were selected from those identified by using an automatic randomization tool, in order to avoid selection bias.
Inclusion criteria
The study included adults (≥18 years of age) requiring treatment with intravenous (IV) antimicrobials. Radiographically confirmed pneumonia and acute illness (≤7 days’ duration) were required, with at least three of: new or increased cough; purulent sputum or change in sputum character; auscultatory findings consistent with pneumonia; dyspnoea, tachypnoea or hypoxaemia (O2 saturation <90% or pO2 <60 mmHg); fever (>38°C [oral]) or hypothermia (<35°C); white blood cell count >10,000 cells/mm3 or <4,500 cells/mm3; >15% band neutrophils irrespective of white blood cell count; requirement for initial hospitalization or treatment in an emergency room or urgent care setting.
Exclusion criteria
Patients already participating in a clinical trial or any other interventional study were not eligible. Patients with CAP deemed suitable for outpatient therapy with an oral antibiotic and patients transferred from another healthcare facility or readmitted with antibiotic use within 2 days were also excluded.
Study variables
Data were collected via an electronic Case Report Form completed by the investigator. The information collected included site characteristics; patient demographics; medical history; disease characteristics, including severity score (Pneumonia Outcomes Research Team/Pneumonia Severity Index [PORT/PSI] [13]; CURB-65 [14]) and microbiological diagnosis; treatment setting; disease course and outcomes; antibacterial and other treatments before and during hospitalization and health resource consumption.
Statistical methods and data interpretation
As the study is descriptive, no formal sample size calculations were performed. The aim was to recruit approximately 200–300 patients per disease per country to achieve a representative spread of patients.
The primary outcome measure was the initial antibiotic treatment modification rate. The initial antibiotic was the first IV antibiotic administered on admission to the hospital. ‘Initial antibiotic treatment modification’ was defined as a change in initial antibiotic treatment due to insufficient response, adverse reaction, interaction with other drugs, non-suitability of the initial antibiotic based on the results of microbiological tests or changes to or additions of new agents in a subsequent line, alone or in combination. Cases of streamlining (also known as de-escalation, defined as change to narrower-spectrum antibiotics upon patient improvement or confirmed microbiological diagnosis) were also recorded, but considered separately. Cases of patient death while on initial antibiotic treatment were also recorded.
Several antibiotic treatment modifications in the same patient were counted as a single case. Changes in dose or frequency of an existing antibiotic (considered as dose escalation or adaptation) and removal of an antibiotic from a combination and adaptation of the dose or frequency of the remaining antibiotic were not considered treatment modification.
For recording time to clinical stability, investigators were asked to report what criteria they had followed: Halm criteria [15], switch from IV to oral therapy or other criteria defined by the investigator.
Results
Patient population
The analysis population included 2,039 patients. Patient disposition is shown in Figure 1. The majority of patients were enrolled between November 2010 and February 2011.
Numbers of sites and numbers of patients per country are shown in Additional file 1: Table S1. Some countries did not achieve the target sample size of 200–300 patients; in Germany, the requirement for signed informed consent in a retrospective study precluded wider patient recruitment, leading to considerably fewer patients than other countries (n = 50), while in Portugal, changes in data protection laws delayed initiation, and in the UK, supply delays for some patient records necessitated their exclusion. Patient demographics and baseline characteristics are shown in Table 1.
Medical history and disease characteristics are shown in Table 2. The mean age of patients differed considerably between patients with and without comorbidities (67.8 years and 52.6 years, respectively). Over half of the patients had received medications in the 3 months prior to admission.
Characteristics of the index CAP infection are shown in Table 3. The majority of patients had no known recent contact with the healthcare system, having been resident in a private house or apartment prior to admission, while 12% of patients had been resident in settings commonly linked with healthcare-associated pneumonia (HCAP), such as in a nursing home. Antibiotic treatment of the index infection prior to hospitalization occurred in 23.5% of patients, the most common antibiotic classes used being penicillins or penicillin–β-lactamase inhibitor combinations (9.3%), fluoroquinolones (4.5%), cephalosporins (4.0%) and macrolides (3.5%).
Diagnostic information
Diagnostic information is shown in Additional file 1: Table S2. Although microbiological testing was conducted in all but one patient (Additional file 1: Table S2a), only 582 (28.5%) patients had a microbiological diagnosis available (Additional file 1: Table S2b). The most commonly isolated organism in the full analysis population was Streptococcus pneumoniae (39.2%). In patients with bacteraemia, this organism accounted for the majority of microbiological diagnoses (63.8%).
Treatment setting and modalities
In total, 128 sites were included. A large number of university (teaching) hospitals were included (n = 54; 42.2%). Almost all sites were publicly funded (n = 124; 96.9%) and the majority were large (>500 beds: n = 91; 71.1%). Participating investigators were most commonly pneumologists (n = 63; 49.2%) or infectious diseases specialists (n = 35; 27.3%). Similar numbers of patients were treated in university and non-university hospitals (958 [47.0%] versus 1,081 [53.0%], respectively) and there were no major differences in patient population between hospital types. Overall use of the PORT/PSI and CURB-65 illness severity scoring systems was low and was more common in university hospitals than in non-university hospitals: PORT/PSI (30.3% versus 5.9%, respectively) and CURB-65 (39.0% versus 14.2%, respectively).
Antibiotics were most frequently administered on the first day of hospitalization (90.0% of patients; n = 1836), with 7.3% of patients (n = 149) receiving antibiotics on the second day. Antibiotics were administered empirically in 1,918 (94.1%) of patients. An analysis of antibiotic therapy administered is presented in Additional file 1: Table S3. Up to 48 different antibiotic agents (alone or in combination) were reported to have been used, the most frequent at initial line being amoxicillin-clavulanate (n = 409; 20.1%). The most common antibiotic families at initial line (whether used as monotherapy or in combinations) were penicillins or penicillin plus β-lactamase inhibitor combinations (54.7%), fluoroquinolones (29.0%), cephalosporins (29.5%) and carbapenems (1.8%). The mean overall treatment duration (calculated as start date of initial-line antibiotic to end date of last-line antibiotic) was 10.0 days (SD: 6.6; median: 9.0).
Clinical outcomes
Clinical outcomes are shown in Table 4. The most common reasons for initial antibiotic treatment modification were insufficient response to treatment (12.0%) and adverse events (2.0%). In some patients, the reason recorded was ‘Other’ or ‘Unknown’, or no reason was reported. On case-by-case review by the investigators, these were found not to be related to clinical improvement, the availability of a microbiological diagnosis or streamlining. For patients in the ‘Other’, ‘Unknown’ and ‘No reason reported’ categories, time to antibiotic treatment modification was <4 days in 37.6% (n = 114) of patients, ≥4 days in 62.0% (n = 188) and unknown in 0.3% (n = 1). The median length of stay in hospital, including all hospitalizations for patients with recurrences, was 10.0 days (mean: 12.6 days; SD: 10.6). If recurrences were excluded, the median length of stay was 9.0 days (mean: 12.1 days; SD: 9.8).
The distribution of time to clinical stability according to any of the criteria is shown in Figure 2. The majority of patients reached clinical stability on days 2–5. Approximately half of the patients with clinical stability data (n = 1,604) achieved clinical stability early in the course of treatment (day ≤4) (51.9%; n = 833), and 97.1% had achieved clinical stability on or before day 15. However, a small percentage (0.7%) of patients had not achieved clinical stability by day 30. Clinical failure (defined as acute haemodynamic deterioration or death, or any other criterion considered by the investigator to be indicative of clinical failure) occurred in 355 patients (17.4%). Of these, the failure was related to CAP in 239 patients (67.3%), unrelated in 85 patients (23.9%) and for unknown reasons in 31 patients (8.7%).
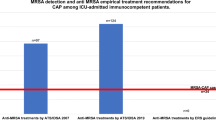
Initial antibiotic treatment modification rates by initial antibiotic agent for the most common antibiotic combinations and monotherapies are shown in Additional file 1: Table S3. Rates differed widely between antibiotics, with no obvious pattern. Clinical outcomes according to disease characteristics are shown in Table 5. Initial antibiotic treatment modification rates were greater in patients with HCAP (31.8%) and immunocompromised/immunosuppressed patients (40.3%) than in patients with CAP (28.4%). Mortality rates were also higher in these subgroups (HCAP: 16.3%; immunocompromised/immunosuppressed: 9.7%) compared with CAP (5.5%). Similarly, high initial antibiotic treatment modification rates were observed in patients with comorbidities versus those without. Worsened clinical outcomes were observed with increased severity of illness as measured by CURB-65 and PORT/PSI scores, albeit with small patient numbers. For patients with vaccine data recorded, neither influenza vaccination nor pneumococcal vaccination had a significant impact on outcomes. Mortality for the full population was 7.2%. Mortality varied across the different countries; Belgium, 12.0% (n = 23/191); France, 5.2% (n = 19/366); Germany 0% (n = 0/50); Greece 2.3% (n = 5/215); Italy, 1% (n = 3/300); the Netherlands, 10.8% (22/203); Portugal, 15.7% (n = 19/121); Spain, 6.8% (n = 19/279); Turkey, 8.5% (n = 17/200) and the UK 17.5% (n = 20/114).
Clinical outcomes in patients attending recurrently with the same infection
In 94 patients (4.6%), the index CAP infection was a recurrence of a previously hospitalized CAP episode. The initial antibiotic treatment modification rate in these patients was 34.0% (n = 32). The median duration of hospital stay was 11.0 days (n = 94) and the median time to clinical stability was 5.0 days (n = 78) (Table 5).
Discussion
CAP-associated morbidity and mortality are considerable and particularly common in patients hospitalized with CAP [16]. The REACH study gathered data on underlying characteristics and treatment patterns in patients hospitalized with CAP in a variety of clinical settings across 128 hospitals in ten EU countries. We found an unexpectedly high overall rate of initial antibiotic treatment modification (28.9%), with the majority of the patients treated empirically. Rates of initial antibiotic treatment modification and associated outcomes, such as overall mortality, were increased in patients with more complicated or more severe illness, such as those patients with a PORT/PSI score of V or ‘severe’ CURB-65 score, immunocompromised/immunosuppressed patients and patients with recurrent infections or comorbidities. Additionally, patients with HCAP had a much higher mortality rate of 16.3% compared with 5.5% in patients with CAP. Total mortality in REACH appears low at 7.2% but is consistent with data published previously for patients with PORT scores [17, 18]. However, it may be that REACH patients without a measure of severity (PORT/PSI or CURB-65) actually had less severe disease globally.
Comparison with previous studies is complicated because different definitions of treatment modification and treatment failure are employed. Indeed, a 2009 review of treatment failure in patients with CAP across Europe found a wide variation (2.4–31%) in reported rates (including both early and late failure) [19]. In studies with treatment failure defined as per the definition of initial antibiotic treatment modification used in REACH, treatment failure rates align closely with the rate of initial antibiotic treatment modification observed [17, 18].
A health economic analysis of our study showed that initial antibiotic treatment modification is associated with higher use of resources compared with no modification of initial antibiotic treatment (Ostermann et al. submitted). Therefore, it is critically important that management decisions for patients with CAP incorporate measures that reduce the likelihood of initial antibiotic treatment modification, including selection and rapid initiation of the most effective antibiotic agent, efficient diagnostic methods and early identification of patients with additional concerns. Initiatives aimed at improving empiric treatment strategies and microbiological stewardship may help in this respect.
The broad range of potential pathogens implicated in CAP and the difficulty in obtaining a precise microbiological diagnosis complicate treatment of CAP. In this study, initial treatment decisions were empiric in 94.1% of patients. A further complication is the wide range of treatment options: 48 different antibiotic regimens were reported in this study.
Although almost every patient underwent a microbiological test, the diagnosis rate was only 28.5%. The most common organism identified was S. pneumoniae, which follows previous studies [8, 20–24]. Interestingly, high percentages of less common pathogens, such as S. aureus (7.2%) and Pseudomonas aeruginosa (7.0%), were observed. A Swedish study found that these pathogens were more common in patients with higher CRB-65 scores [20], and a European review of patients with CAP admitted to intensive care [25] observed S. aureus (7.0%) and Gram-negative enteric bacilli (8.6%) more frequently than in the whole population [8]. In patients with bacteraemia in REACH, the spectrum of pathogens was more homogeneous, being dominated by S. pneumoniae (n = 74; 63.8%). Compared with previous studies [26, 27], a low proportion of resistant pathogens was reported in our study (two patients with penicillin-resistant S. pneumoniae [0.3%] and 12 with methicillin-resistant S. aureus [2.1%]).
Previous studies show that adherence to guidelines for antibiotic therapy for CAP [6, 28] can reduce hospital length of stay [29, 30], costs [30, 31] and mortality [32]. The European Respiratory Society (ERS), in collaboration with The European Society for Clinical Microbiology and Infectious Disease (ESCMID), recommends penicillins, with or without β-lactamase inhibitors, or cephalosporins, administered in combination with newer macrolides for patients hospitalized with CAP [5]. Although there were a large number of different initial antibiotic regimens used in REACH, the majority of treatment decisions were consistent with these guidelines.
Interestingly, several of the most common antibiotic classes (penicillins plus macrolide, 32.3%; cephalosporin [excluding cefuroxime] plus fluoroquinolone, 31.3%) were associated with initial antibiotic treatment modification rates slightly higher than the average for all treatments. This may reflect inappropriate initial treatment choices for the infecting pathogen. A further possible explanation is higher use of certain antibiotics in patients with more severe illness, who may have been predisposed to initial antibiotic treatment modification. It should be noted that the initial antibiotic treatment modification rates reported for antibiotic classes may not generalize to individual agents within that class.
Our study had a number of limitations. The retrospective design may have resulted in inconsistent outcomes assessment between investigators due to differences in interpretation. However, the potential problem of incomplete information in some patient records was not common, generally occurring in ≤7% of patients (although the reason for initial antibiotic treatment modification was ‘Other’, ‘Unknown’ or was not reported in 14.8% of patients). The small patient numbers in some of the subgroups limit the possibility of making firm conclusions. Patient recruitment varied widely between countries owing to differences in ethical requirements. Also, the included countries were mainly western European, and so may not be fully representative of Europe as a whole.
In summary, this large, Europe-wide study provides the most current data to further describe patient characteristics and clinical management of patients hospitalized with CAP in this region. The findings reveal the enormous heterogeneity in clinical management patterns. Initial antibiotic treatment modification occurred in almost one-third of affected patients, and was more common in patients with comorbidities than in those without. Therefore, the authors believe that a reassessment of optimal management regimens should be undertaken and new therapies may be required to address this unmet need.
References
Woodhead M: Community-acquired pneumonia in Europe: causative pathogens and resistance patterns. Eur Respir J Suppl. 2002, 36: 20s-27s.
Welte T: Risk factors and severity scores in hospitalized patients with community-acquired pneumonia: prediction of severity and mortality. Eur J Clin Microbiol Infect Dis. 2012, 31: 33-47. 10.1007/s10096-011-1272-4.
Welte T, Kohnlein T: Global and local epidemiology of community-acquired pneumonia: the experience of the CAPNETZ Network. Semin Respir Crit Care Med. 2009, 30: 127-135. 10.1055/s-0029-1202941.
Capelastegui A, Espana PP, Bilbao A, Gamazo J, Medel F, Salgado J, Gorostiaga I, Esteban C, Altube L, Gorordo I, Quintana JM: Study of community-acquired pneumonia: incidence, patterns of care, and outcomes in primary and hospital care. J Infect. 2010, 61: 364-371. 10.1016/j.jinf.2010.07.015.
Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Read R, Verheij TJ: Guidelines for the management of adult lower respiratory tract infections--full version. Clin Microbiol Infect. 2011, 17 (Suppl 6): E1-E59.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG: Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007, 44 (Suppl 2): S27-S72.
Martinez R, Reyes S, Lorenzo MJ, Menendez R: Impact of guidelines on outcome: the evidence. Semin Respir Crit Care Med. 2009, 30: 172-178. 10.1055/s-0029-1202936.
BTS guidelines for the management of community acquired pneumonia in adults. Thorax. 2001, 56 (Suppl 4): IV1-IV64.
Welte T, Torres A, Nathwani D: Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax. 2010, 67: 71-79.
Aspa J, Rajas O, de Castro FR: Pneumococcal antimicrobial resistance: therapeutic strategy and management in community-acquired pneumonia. Expert Opin Pharmacother. 2008, 9: 229-241. 10.1517/14656566.9.2.229.
Bauer TT, Welte T, Ernen C, Schlosser BM, Thate-Waschke I, de Zeeuw J, Schultze-Werninghaus G: Cost analyses of community-acquired pneumonia from the hospital perspective. Chest. 2005, 128: 2238-2246. 10.1378/chest.128.4.2238.
World Health Organization: International Classification of Diseases (ICD) 10th Revision (2007 version). 2007, Geneva, Switzerland: World Health Organization
Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN: A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997, 336: 243-250. 10.1056/NEJM199701233360402.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, Lewis SA, Macfarlane JT: Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003, 58: 377-382. 10.1136/thorax.58.5.377.
Halm EA, Fine MJ, Marrie TJ, Coley CM, Kapoor WN, Obrosky DS, Singer DE: Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998, 279: 1452-1457. 10.1001/jama.279.18.1452.
Ramirez JA, Anzueto AR: Changing needs of community-acquired pneumonia. J Antimicrob Chemother. 2011, 66 (Suppl 3): iii3-iii9.
Garau J, Baquero F, Perez-Trallero E, Perez JL, Martin-Sanchez AM, Garcia-Rey C, Martin-Herrero JE, Dal-Ré R: Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin Microbiol Infect. 2008, 14: 322-329. 10.1111/j.1469-0691.2007.01915.x.
Blasi F, Iori I, Bulfoni A, Corrao S, Costantino S, Legnani D: Can CAP guideline adherence improve patient outcome in internal medicine departments?. Eur Respir J. 2008, 32: 902-910. 10.1183/09031936.00092607.
Garcia-Vidal C, Carratala J: Early and late treatment failure in community-acquired pneumonia. Semin Respir Crit Care Med. 2009, 30: 154-160. 10.1055/s-0029-1202934.
Stralin K, Olcen P, Tornqvist E, Holmberg H: Definite, probable, and possible bacterial aetiologies of community-acquired pneumonia at different CRB-65 scores. Scand J Infect Dis. 2010, 42: 426-434. 10.3109/00365540903552353.
Garcia-Vidal C, Carratala J, Fernandez-Sabe N, Dorca J, Verdaguer R, Manresa F, Gudiol F: Aetiology of, and risk factors for, recurrent community-acquired pneumonia. Clin Microbiol Infect. 2009, 15: 1033-1038. 10.1111/j.1469-0691.2009.02918.x.
Vila-Corcoles A, Ochoa-Gondar O, Rodriguez-Blanco T, Raga-Luria X, Gomez-Bertomeu F: Epidemiology of community-acquired pneumonia in older adults: a population-based study. Respir Med. 2009, 103: 309-316. 10.1016/j.rmed.2008.08.006.
Gutierrez F, Masia M, Rodriguez JC, Mirete C, Soldan B, Padilla S, Hernandez I, De Ory F, Royo G, Hidalgo AM: Epidemiology of community-acquired pneumonia in adult patients at the dawn of the 21st century: a prospective study on the Mediterranean coast of Spain. Clin Microbiol Infect. 2005, 11: 788-800. 10.1111/j.1469-0691.2005.01226.x.
Hedlund J, Ortqvist A, Ahlqvist T, Augustinsson A, Beckman H, Blanck C, Burman LA, Claesson B, Qvarfordt I, Elbel E, Erntell M, Follin P, Goscinski G, Holmberg H, Hofer M, Jorup C, Lidman C, Lindhusen E, Rensfeldt G, Rosenkvist E, Stenlund G, Stalberg A, Verngren K, Vig I, Wendahl S: Management of patients with community-acquired pneumonia treated in hospital in Sweden. Scand J Infect Dis. 2002, 34: 887-892. 10.1080/0036554021000026965.
Valencia M, Badia JR, Cavalcanti M, Ferrer M, Agusti C, Angrill J, Garcia E, Mensa J, Niederman MS, Torres A: Pneumonia severity index class v patients with community-acquired pneumonia: characteristics, outcomes, and value of severity scores. Chest. 2007, 132: 515-522. 10.1378/chest.07-0306.
Tudose C, Bumbacea D, Bogdan M: Antibiotic resistance of S. pneumoniae and H. influenzae strains isolated from patients with community acquired respiratory tract infections. BACTRO multicenter, multidisciplinary study. Pneumologia. 2011, 60: 30-35.
Valles X, Marcos A, Pinart M, Piner R, Marco F, Mensa JM, Torres A: Hospitalized community-acquired pneumonia due to Streptococcus pneumoniae: Has resistance to antibiotics decreased?. Chest. 2006, 130: 800-806. 10.1378/chest.130.3.800.
Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, Martinez F, Marrie TJ, Plouffe JF, Ramirez J, Sarosi GA, Torres A, Wilson R, Yu VL: Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001, 163: 1730-1754. 10.1164/ajrccm.163.7.at1010.
Dambrava PG, Torres A, Valles X, Mensa J, Marcos MA, Penarroja G, Camps M, Estruch R, Sanchez M, Menendez R, Niederman MS: Adherence to guidelines' empirical antibiotic recommendations and community-acquired pneumonia outcome. Eur Respir J. 2008, 32: 892-901. 10.1183/09031936.00163407.
Orrick JJ, Segal R, Johns TE, Russell W, Wang F, Yin DD: Resource use and cost of care for patients hospitalised with community acquired pneumonia: impact of adherence to infectious diseases society of america guidelines. Pharmacoeconomics. 2004, 22: 751-757. 10.2165/00019053-200422110-00005.
Merchant S, Mullins CD, Shih YC: Factors associated with hospitalization costs for patients with community-acquired pneumonia. Clin Ther. 2003, 25: 593-610. 10.1016/S0149-2918(03)80099-1.
Brown PD: Adherence to guidelines for community-acquired pneumonia: does it decrease cost of care?. Pharmacoeconomics. 2004, 22: 413-420. 10.2165/00019053-200422070-00001.
Acknowledgements
The REACH study was sponsored and funded by AstraZeneca. Editorial assistance was provided by Ben Caldwell of MediTech Media, funded by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
FB has received research grants from Chiesi, GSK, Pfizer and Zambon, has received congress lecture fees from Abbott, Chiesi, GSK and Pfizer and has received consultancy fees from AstraZeneca, GSK and Pfizer. JG has received research grants, speaking invitations and conference invitations from Astellas, AstraZeneca, Bayer, GSK, Novartis, Pfizer and Vifor Pharma, and has recent or ongoing consultancies with Astellas, AstraZeneca, Bayer, Durata, GSK, Janssen Cilag, Novartis, Pfizer, Theravance and Vifor Pharma. HO is a member of an advisory board for AstraZeneca. JM and MA are employees of AstraZeneca. KMB has received consultancy fees from ACT Oncology, AstraZeneca, BioSoteria, Celgene Corporation, Cypress Pharmaceuticals, Integrium LLC, Outcomes Research (now owned by Quintiles), MedImmune, Multiple Myeloma Research Foundation, Sigma-Tau Pharmaceuticals and Worldwide Clinical Trials.
Authors’ contributions
The chief investigators (JG, FB, HO) designed the trial, with input from the sponsor. The chief investigators, together with KM, initiated the analysis presented here, with the other investigators, JM and MA contributing to the analysis and interpretation. The decision to submit the report for publication was made by the lead contributors and chief investigators, who drafted and finalized the report with the help of a medical writer. The sponsor funded editorial assistance and reviewed the draft before submission. All authors have read and approved the final manuscript.
Electronic supplementary material
12931_2012_1359_MOESM1_ESM.pdf
Additional file 1: Table S1: Analysis population by country. Table S2 Microbiological diagnosis. Table S3 Antibiotic therapies. Table S4 Patient demographics in patients with initial antibiotic treatment modification. Table S5 Medical history and disease characteristics. Table S6 Characteristics of index CAP infection. Appendix 1 Pneumonias – ICD-10 coding. Appendix 2 REACH study investigators. (PDF 121 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Blasi, F., Garau, J., Medina, J. et al. Current management of patients hospitalized with community-acquired pneumonia across Europe: outcomes from REACH. Respir Res 14, 44 (2013). https://doi.org/10.1186/1465-9921-14-44
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1465-9921-14-44