Abstract
Background
An imbalance in the generation of pro-inflammatory leukotrienes, and counter-regulatory lipoxins is present in severe asthma. We measured leukotriene B4 (LTB4), and lipoxin A4 (LXA4) production by alveolar macrophages (AMs) and studied the impact of corticosteroids.
Methods
AMs obtained by fiberoptic bronchoscopy from 14 non-asthmatics, 12 non-severe and 11 severe asthmatics were stimulated with lipopolysaccharide (LPS,10 μg/ml) with or without dexamethasone (10-6M). LTB4 and LXA4 were measured by enzyme immunoassay.
Results
LXA4 biosynthesis was decreased from severe asthma AMs compared to non-severe (p < 0.05) and normal subjects (p < 0.001). LXA4 induced by LPS was highest in normal subjects and lowest in severe asthmatics (p < 0.01). Basal levels of LTB4 were decreased in severe asthmatics compared to normal subjects (p < 0.05), but not to non-severe asthma. LPS-induced LTB4 was increased in severe asthma compared to non-severe asthma (p < 0.05). Dexamethasone inhibited LPS-induced LTB4 and LXA4, with lesser suppression of LTB4 in severe asthma patients (p < 0.05). There was a significant correlation between LPS-induced LXA4 and FEV1 (% predicted) (rs = 0.60; p < 0.01).
Conclusions
Decreased LXA4 and increased LTB4 generation plus impaired corticosteroid sensitivity of LPS-induced LTB4 but not of LXA4 support a role for AMs in establishing a pro-inflammatory balance in severe asthma.
Similar content being viewed by others
Introduction
Patients with asthma are usually well-controlled with inhaled corticosteroids (CS) and long-acting β2-agonists, but a minority of patients described as severe asthma continues to experience uncontrolled asthma in spite of these treatments. Patients with severe asthma suffer greater morbidity, face a higher risk of asthma death, and consume a greater proportion of health resources than other non-severe asthma patients [1, 2]. One feature of severe asthma is the presence of airway inflammation despite corticosteroid therapy, often characterised by the persistence of eosinophilic inflammation and the presence of neutrophils[3, 4]. Persistent symptoms with frequent exacerbations of asthma despite corticosteroid therapy also indicate the possibility that CS may not be as effective in patients with severe asthma. The presence of reduced CS sensitivity in severe asthma is supported by the finding that release of cytokines from peripheral blood mononuclear cells and alveolar macrophages is less suppressible by dexamethasone than those from non-severe asthma patients[5, 6].
Lipid mediators of the 5-lipoxygenase pathway such as cysteinyl-leukotrienes are implicated as mediators of airway bronchoconstriction and eosinophilic inflammation in asthma; another product, leukotriene B4 (LTB4), has also been implicated, particularly in view of its chemoattractant and activating properties for neutrophils [7]. Similar to LTs, lipoxins (LXs) are products of arachidonic acid metabolism, yet LXs are generated via interactions between 5- and 15-lipoxygenases or 5- and 12-lipoxygenases to form structurally distinct compounds that promote the resolution of inflammation. Thus, LXs are counter-regulatory to the cysteinyl-leukotrienes and LTB4 [8]. The possibility that dysregulation of the balance among these arachidonic acid products might contribute to the persistent inflammation in severe asthma has been supported by the demonstration of an increased generation of cysteinyl-leukotrienes with impaired biosynthesis of lipoxin A4 (LXA4) from whole blood of patients with severe asthma compared to non-severe asthma patients[9]. In addition, LXA4 levels in bronchoalveolar lavage fluid of patients with severe asthma from the NHLBI Severe Asthma Research Program were decreased when compared to non-severe asthma patients [10].
We determined whether an imbalance in pro-inflammatory LTB4 and anti-inflammatory LXA4 in the lungs of patients with severe asthma could be reflected in the formation of these products from alveolar macrophages (AMs). We also determined whether there would also be a differential suppressibility of these mediators that reflect different effects in asthma.
Methods
Patients
Patients with asthma were recruited from the Asthma Clinic of the Royal Brompton Hospital, London. Severe asthma patients underwent the Royal Brompton severe asthma protocol, in order to confirm the diagnosis and to maximise treatments[11]. All patients showed either an improvement in baseline FEV1 of ≥12% over baseline values after inhalation of 400 μg of salbutamol aerosol, or the presence of bronchial hyperresponsiveness defined by methacholine PC20 of < 4 mg/ml. Current and ex-smokers of >5 pack-years were excluded. Severe asthmatics were defined according to the American Thoracic Society major criteria of needing either continuous or near-continuous oral corticosteroids or high dose inhaled corticosteroids (2,000 μg beclomethasone-equivalent per day or more) or both in order to achieve a level of mild-moderate persistent asthma, and by 2 or more minor criteria of asthma control[12]. Patients who had well-controlled asthma defined by the lack of day-time or nocturnal symptoms and no need for reliever medications while using ≤ 800 μg of inhaled beclomethasone-equivalent per day were enrolled into the non-severe asthma group. Healthy volunteers with no diagnosis of asthma and with a negative PC20 (>16 mg/ml), using no medications and never-smokers, were also recruited. All participants gave informed consent to a protocol approved by the Ethics Committee of Royal Brompton & Harefield NHS Trust/National Heart & Lung Institute.
Fiberoptic bronchoscopy
All asthmatic subjects received 5 mg of nebulised salbutamol before the procedure. Fibreoptic bronchoscopy was performed using topical anesthesia with lignocaine and intravenous sedation with midazolam. Warmed 0.9% NaCl solution (50 ml × 4) was instilled into the right middle lobe and recovery of broncho-alveolar lavage (BAL) fluid was carried out by gentle hand suction.
Alveolar macrophage isolation
BAL cells were centrifuged (500 × g for 10 minutes) and washed with Hanks' balanced salt solution (HBSS). They were resuspended in culture media (RPMI with 0.5% fetal calf serum, antibiotics and L-glutamine) and counted using Kimura dye. Cytospins were prepared and stained with Diff Quick (Harleco, Gibbstown, NJ) stain for differential cell count. 5×105 macrophages were isolated by plastic adhesion and stimulated for 18 hours with lipopolysaccaride (LPS, 10 μg/ml) in the presence or absence of dexamethasone (Dex, 10-6 M). Supernatants were aliquoted and coded. These de-identified materials were analysed in a separate laboratory for LTB4 and LXA4 by enzyme immunoassay (Cayman Chemical, Ann Arbor, Mich; Neogen, Lexington, KY). The stimulated formation of LTB4 and LXA4 was calculated as the difference between the total amount present with LPS and the basal amounts without LPS.
Validation of Immunoreactive LXA4 by Addition of Authentic LXA4
As the absolute amounts of LXA4 in the macrophage supernatant samples were too low for detection by physical methods, we validated our immunoassay measurements by purposefully adding 20-30 pg of authentic LXA4 to selected sample aliquots and then measuring immunoreactive LXA4 levels in both neat and spiked samples. Addition of authentic LXA4 increased the total amount of LXA4 (endogenous plus exogenous) above the lower limits of detection for the ELISA. Neat and spiked samples displayed only minor variance in the amount of endogenous LXA4.
Data analysis
Results are expressed as means ± SEM. The differences in LTB4 and LXA4 generated at baseline were compared using one-way analysis of variance with Dunn's multiple comparison test. Differences between LPS and LPS plus dexamethasone treatment were analysed using Wilcoxon paired t-tests and in this case differences between groups were compared using Mann-Whitney t-test. Correlations were performed using Spearman's rank tests. p < 0.05 was taken as significant.
Results
Severe asthmatics had more severe airflow obstruction (p < 0.05) and bronchial hyperresponsiveness (p < 0.05) compared to non-severe asthmatics (Table 1). They were also on higher doses of inhaled corticosteroids (p < 0.05). BAL yielded fewer cells from severe asthmatics compared to non-severe asthmatics (p = 0.06), but there were proportionately more eosinophils (p < 0.05) and neutrophils (p < 0.05) with fewer macrophages (p < 0.01) in severe asthma compared to non-severe asthma.
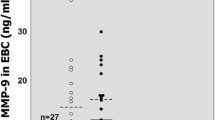
Baseline and LPS-stimulated generation of LXA4
Low levels of LXA4 were generated by AMs in culture. The baseline LXA4 from AMs obtained from normal subjects was higher than that from both non-severe (p < 0.05) and severe asthmatics (p < 0.01; Figure 1A). There was a significant difference between non-severe and severe asthmatics (p < 0.05) with a three-fold higher baseline level in non-severe asthmatics. The LXA4 production induced by LPS is shown as the increment in LXA4 above baseline (Figure 1B). There was a small but significant increase in LPS-induced LXA4 levels in all three groups (Figure 1B), with the lowest amounts in severe compared to non-severe asthma (p < 0.01) and to normal subjects (p < 0.001).
Panel A: Individual levels of LXA 4 in supernatants of alveolar macrophages before and after lipopolysaccharide (LPS) from normal subjects (n = 14), non-severe asthmatics (n = 12) and severe asthmatics (n = 11). In the asthmatic groups, closed symbols indicate those on regular treatment with inhaled and/or oral corticosteroids. Panel B: Mean levels of LXA4 induced by LPS (level after LPS minus basal level) in the 3 groups. Data shown as mean ± SEM.
There was a negative correlation between baseline LXA4 levels in asthmatic patients and the percentage of neutrophils in the BAL (rs = - 0.42, p < 0.05), and a positive correlation between LPS-induced LXA4 levels from asthmatic patients and FEV1 (% predicted; r = 0.60, p < 0.01). In addition, there was a negative correlation between percentage neutrophils in the BAL and FEV1 (rs = -0.65, p < 0.001).
Basal and LPS-stimulated generation of LTB4
The basal level of LTB4 from AMs obtained from normal subjects was higher than that from both non-severe (p < 0.05) and severe asthmatics (p < 0.05; Figure 2A), with no significant differences between non-severe and severe asthmatics. The LTB4 production induced by LPS is shown as increments in LTB4 above baseline (Figure 2B). LPS induced LTB4 generation in all three groups (p < 0.05), but the increase in LTB4 in severe asthma patients was 5-fold greater than in non-severe asthmatics (p < 0.05; Figure 2B).
Panel A: Individual levels of LTB 4 in supernatants of alveolar macrophages before and after lipopolysaccharide (LPS) from normal subjects (n = 9), non-severe asthmatics (n = 9) and severe asthmatics (n = 8). In the asthmatic groups, closed symbols indicate those on regular treatment with inhaled and/or oral corticosteroids. Panel B: Mean levels of LPS-stimulated LTB4 represented by the difference between LTB4 levels with LPS and the basal level of LTB4 in the 3 groups. Data shown as mean ± SEM.
Corticosteroid suppression of LXA4. and LTB4
Dexamethasone suppression of LPS-initiated LXA4 was significant in all three groups (p < 0.05), with no significant differences between the groups (Figure 3). Dexamethasone suppression of LTB4 was observed in all three groups: normal subjects (LPS: 102 ± 23 versus LPS and dexamethasone: 11.6 ± 7.7 pg/ml, p < 0.05); non-severe asthmatics (183 ± 122 versus 21.4 ± 22 pg/ml, p < 0.05) and severe asthmatics (230 ± 102 versus 60 ± 32 pg/ml, p < 0.01). When the suppression was expressed as a percentage of LPS-induced eicosanoid production, there was no significant differences observed between normal and non-severe asthmatics with ~90% suppression. However, there was a lesser degree of suppression in severe asthmatics (Figure 4).
Individual levels of LXA 4 measured after LPS in the absence or presence of dexamethasone (10 -6 M) from alveolar macrophages stimulated by LPS from normal subjects (n = 14), non-severe asthmatics (n = 12) and severe asthmatics (n = 11). In the asthmatic groups, closed symbols indicate those on regular treatment with inhaled and/or oral corticosteroids. Data shown as mean ± SEM.
Individual levels of LTB 4 measured after LPS in the absence or presence of dexamethasone (10 -6 M) from alveolar macrophages stimulated by LPS in normal subjects (n = 9), non-severe asthmatics (n = 9) and severe asthmatics (n = 8). In the asthmatic groups, closed symbols indicate those on regular treatment with inhaled and/or oral corticosteroids. Data shown as mean ± SEM. Panel C. Mean degree of suppressibility of LXA4 and LTB4 release by dexamethasone. Data is expressed as % of LXA4 or LTB4 release after exposure to LPS (level after LPS minus basal level) and shown as mean ± SEM.
In macrophages from normal subjects, the ratio of LTB4 to LXA4 (using pg/ml) was unchanged after exposure to LPS or to LPS plus dexamethasone. In non-severe asthmatics, both LPS and LPS plus dexamethasone gave an increased LTB4/LXA4 ratio, but only in severe asthmatics was the increase induced by LPS and dexamethasone significantly greater than that induced by LPS alone (p < 0.05) (Figure 5). In addition, LTB4/LXA4 ratios after LPS and dexamethasone were significantly greater in severe asthmatics compared to non-severe asthmatics (p < 0.05) as a result of both an increase in LTB4 and a decrease in LXA4 compared to normal subjects.
Effect of LPS (Stim) and LPS plus dexamethasone (LPS/Dex) on the ratio of LTB 4 to LXA 4 from alveolar macrophages. In both asthmatic groups, the ratio of released LTB4 to released LXA4 is increased after LPS and this is not reversed in the presence of dexamethasone. *p < 0.05 compared to baseline (base) within each group; +p < 0.01 compared to LPS/Dex of normal subjects. Data shown as shown as mean ± SEM.
Discussion
We have shown that the basal generation of the proinflammatory LTB4 and the anti-inflammatory LXA4 were both lower in cultured AMs from severe asthmatics compared to those from non-asthmatics, while only LXA4 was lower in severe asthmatics compared to non-severe asthmatics. The LPS induced formation of LTB4 was higher in severe asthma compared to non-severe asthma and normal subjects, while the LPS induced production of LXA4 was significantly impaired in severe asthmatics compared to normal subjects, but to a similar extent as in non-severe asthma patients. The overall effect of LPS stimulation was a net pro-inflammatory balance in terms of enhanced generation of LTB4, and a decrease in LXA4 compared to AMs from normal subjects. In addition, while the LPS-induced LTB4 was largely suppressed by dexamethasone, it was only partly suppressed in AMs from severe asthma patients; by contrast, induced generation of LXA4 was suppressed in all three groups. Therefore, the overall balance of these 2 lipid mediators in severe asthma was in favour of an overall pro-inflammatory response through both increased production and relative corticosteroid insensitivity of LTB4 and decreased levels of LXA4 in severe asthmatics, as illustrated by the LTB4 to LXA4 ratios.
Human AMs can generate both 5-lipoxygenase and 15-lipoxygenase derived eicosanoids, including LTB4 and LXA4, from endogenous sources of arachidonic acid[13]. LXA4 generation from endogenous stores is low, but LX biosynthesis can be amplified by select TH2 cytokines, namely interleukin-4 and interleukin-13 [14, 15]. In addition, exogenous LTA4 can be converted by AMs to more substantial amounts of LXs [16], as would occur during transcellular biosynthesis with LTA4 donation from one cell to a second cell for enzymatic conversion by either 12- or 15-lipoxygenase to LXs. Our studies are the first to document both LTB4 and LXA4 generation from human AMs from asthmatic subjects. Although the levels of LXA4 are low, they were detected reproducibly, validated with authentic material and picogram quantities of LXs are biologically active in resolving inflammation (reviewed in reference [17]). Interestingly, when the data was expressed as a ratio of pro-inflammatory LTB4 to anti-inflammatory LXA4, there was an increased pro-inflammatory imbalance when the macrophages from both asthmatic groups were exposed to LPS, and this was not reversed by corticosteroids. Indeed, in macrophages from severe asthma, this pro-inflammatory ratio favouring LTB4 over LXA4 was further unbalanced by dexamethasone.
Our results indicate that the pulmonary macrophage can be an important source of lipid mediators, and that differences in LTB4 and LXA4 between the asthmatic groups are in general agreement with recent studies that have examined levels in whole blood[9, 18] and BAL fluids [10]. In the study of Wenzel et al, levels of LTB4 in BAL fluid from severe asthma were the highest compared to levels from moderate symptomatic asthma patients and normals [19]. This indicates that the baseline contribution of LTB4 from macrophages is unlikely to explain this increased levels found in BAL of severe asthma patients; however, following ex vivo stimulation of macrophages from severe asthma patients, greater levels of LTB4 were released compared to non-severe asthma patients. Using a similar method as our study to distinguish severe from non-severe asthma, a deficiency in both baseline and divalent cation ionophore-stimulated production of LXA4 in whole blood of patients with severe asthma compared to moderate asthma was established, while the production of cysteinyl-leukotrienes and LTB4 were increased[9]. In addition, similar findings have been reported in airway fluids for the levels of these lipid mediators; thus, an increase in LTB4 levels was found in the supernatant of induced sputum of severe asthma patients compared to non-severe asthma. In these same samples, LXA4 levels were highest in the mild asthma group[20, 21]. Moreover, LXA4 levels in BAL fluids from patients with severe asthma recruited in the NHLBI Severe Asthma Research Program are decreased compared to non-severe asthma patients, and BAL cells from severe asthma patients had increased 5-LO and decreased 15-LO expression [10]. These results are in line with the current observation of reduced basal and LPS-stimulated production of LXA4 from alveolar macrophages of patients with severe asthma. In conjunction with the large number of alveolar macrophages in healthy and asthmatic lung, these observations provide support to the idea that the alveolar macrophage is a likely important source of LXA4 in human airways.
There have been very few studies of the effect of LPS on human macrophages in terms of LT and LX generation. Brief exposure of murine macrophages to LPS can prime them to increase LT synthesis in response to an activating stimulus such as immune complexes or divalent cation ionophore A23187[22], an observation that has been subsequently shown in human AMs [23]. On the other hand, prolonged exposure to LPS impaired the capacity of rat macrophages to produce LTs in response to stimulating agents, a process that was due to the production of inhibitory substances such as nitric oxide [24, 25]. LPS can induce human AM phagocytosis of apoptotic cells, but AMs from subjects with severe asthma display defective clearance mechanisms and lower levels of PGE2 and 15-hydroxyeicosatetraenoic acid formation in response to LPS[26]. Both PGE2 and 15-HETE can play pivotal roles in establishing LX biosynthesis [27, 28].
Differences in basal LTB4 from AMs have not been previously observed between asthma and normal atopic or non-atopic control subjects[29], or those with nocturnal asthma [30]. However, asthmatic subjects in these studies would not have met the NHLBI Severe Asthma Research Program's criteria for severe asthma [2]. Regarding calcium ionophore-induced LTB4 biosynthesis by AMs, one study reported increased LTB4 generation by cells in asthma compared to non-asthmatics [31], while another study did not report any significant differences[29]. Our study shows reduced baseline LTB4 in non-severe asthma and no significant differences in stimulated production by LPS compared to non-asthmatics. Because LTB4 biosynthesis by AMs in vitro can be modulated by environmental factors in vivo, such as cigarette smoking [32], smokers were excluded from the study.
Glucocorticoids have been shown to inhibit LT generation through inhibition of phospholipase A2 activity [33, 34]. Chronic oral corticosteroid therapy may lead to a suppression of eicosanoid biosynthesis and could underlie the baseline reduction in LXA4 and LTB4 observed in the macrophages from patients with severe asthma. Both LTB4 and LXA4 stimulated by calcium ionophore in the circulating neutrophil was reduced in corticosteroid-dependent asthmatics who were on oral prednisolone [35]. However, as far as the AM is concerned, there was no significant inhibition of LTB4 from AMs of normal subjects treated with oral prednisolone despite the fact that direct incubation of these cells with dexamethasone leads to an inhibition of basal and calcium ionophore triggered formation of LTB4 [36]. Other work also indicate that oral short-term treatment with prednisone does not inhibit the levels of the eicosanoids, PGD2, 5-HETE and LTE4, in BAL from asthmatic subjects at baseline or after allergen challenge [37]. However, ex-vivo treatment of BAL cells with prednislone did cause inhibition of LTB4 and thromboxane generation. Similarly, in the work of Wenzel et al, a single dose of oral prednisone inhibited LTB4 release from alveolar macrophages from patients with nocturnal asthma but not from those without nocturnal asthma [30]. Only half of the patients with severe asthma in this study were on oral corticosteroid therapy and there was no significant differences in terms of LPS-induced LTB4 or LXA4 or of dexamethasone-induced suppression between macrophages of severe asthma patients who were on prednisolone versus those not on prednisolone. Similarly, in the non-severe asthma group, there was no difference in terms of LPS-induced LTB4 or LXA4 or of dexamethasone-induced suppression between macrophages of non-severe asthma patients who were on daily inhaled corticosteroids versus those not on inhaled corticosteroids. However, the influence of long-term oral or inhaled corticosteroid therapy, as contrasted to short-term, on this ex-vivo production of arachidonic acid-derived mediators cannot be entirely excluded.
We have elected to group our asthmatic patients as non-severe and severe asthma patients on the basis of the definition of severe asthma proposed by the ATS [12]. This definition of severe asthma is based on the lack of control of asthma despite taking maximal anti-inflammatory treatments with corticosteroids, while the non-severe asthma patients were those on no or only low-dose inhaled corticosteroids. We observed that there was relative CS insensitivity of LTB4 generation but not of LXA4 from AMs of patients with severe asthma. Previously, no differences in CS sensitivity of AMs in terms of calcium ionophore induced LTB4 from asthmatics as compared to non-asthmatic macrophages have been reported[29]. In a previous study, we have shown that AMs from patients with severe asthma demonstrate a reduced sensitivity to dexamethasone in terms of LPS-induced release of pro-inflammatory cytokines [5].
Our data on LXA4 is one of the first regarding its stimulated production by LPS, and its suppression by dexamethasone. Levels of anti-inflammatory LXs were low in severe asthmatics, and did not increase in response to LPS stimulation, further increasing the disparity between severe asthmatics and non-severe asthmatics in the levels of these mediators. Moreover, dexamethasone suppressed LPS-induced increases in LXA4 in all groups. This differential response of AMs from severe asthmatics vis-a-vis LTB4 and LXA4 and the effect of corticosteroids (increased LTB4 in response to LPS and impaired CS suppression of the rise in LTB4 vs. little change in LXA4 in response to LPS and unimpaired CS suppression of LXA4 levels) may contribute to persistent airway neutrophilic inflammation since LXA4 can inhibit LTB4-induced chemotaxis, adhesion and transmigration[17]. This potential role of LXA4 in regulating neutrophil chemotaxis is supported by the inverse relationship between baseline LXA4 and the percentage of neutrophils in bronchoalveolar lavage fluid.
Lipoxins are a distinct class of eicosanoids with anti-inflammatory properties at subnanomolar concentrations. Thus, although the basal and stimulated levels of LXA4 from alveolar macrophages are in low picogram amounts, these levels would be predicted to have pro-resolving actions for airway inflammation (reviewed in [17]. In support of the protective effect of LXA4, we found a positive correlation between LPS-induced LXA4 and lung function as represented by FEV1. Indirectly, this protection in lung function may occur through an effect on neutrophilic inflammation, since there was an inverse correlation between BAL neutrophilia and FEV1. LXA4 can inhibit LTB4-initiated chemotaxis, adhesion and transmigration. In addition, LXA4 inhibits eosinophilic allergic inflammation [38]. Thus, a possible imbalance in LTB4 and LXA4 in the airways would serve to increase airway neutrophil and eosinophil accumulation and activation. Interestingly, a similar imbalance between LT and LX generation is present in scleroderma lung disease [39] and decreased lipoxin production has also been reported in inflammatory bowel disease [40].
One of the potential limitations of our work regards the relative age of the healthy control group that were younger than the asthma groups. Generation of LXA4 can decrease and LTB4 increase with age [41, 42], but there is no information available at present on the influence of age on the release of these eicosanoids from human alveolar macrophages. While there may be uncertainty about the effect of age, we are able to compare the non-severe with the severe group of asthmatic subjects as they were of comparable age group.
In summary, we demonstrate impaired corticosteroid modulation of the pro-inflammatory lipid mediator LTB4 but not of the anti-inflammatory lipoxin, LXA4, in AMs of severe asthma. Together with the augmented LPS induced formation of LTB4 and decreased generation of LXA4 in severe asthma, our observations indicate a net pro-inflammatory imbalance in severe asthma.
Abbreviations
- AM :
-
alveolar macrophage
- BAL:
-
bronchoalveolar lavage
- BALF:
-
bronchoalveolar lavage fluid
- CS:
-
corticosteroid
- Dex:
-
dexamethasone
- FEV1 :
-
forced expiratory volume in one second
- LT:
-
leukotriene
- LTB4 :
-
leukotriene B4
- LPS:
-
lipopolysaccaride
- LX:
-
liopoxin
- LXA4 :
-
lipoxin A4
- PC20 :
-
provocative concentration of metacholine causing a 20% fall in FEV1
- SEM:
-
standard error of the mean.
References
Stirling RG, Chung KF: Severeasthma: definition and mechanisms. Allergy 2001, 56:825–840.
Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, Calhoun WJ, Castro M, Chung KF, Clark MP, Dweik RA, Fitzpatrick AM, Gaston B, Hew M, Hussain I, Jarjour NN, Israel E, Levy BD, Murphy JR, Peters SP, Teague WG, Meyers DA, Busse WW, Wenzel SE: Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol 2007, 119:405–413.
Jatakanon A, Uasuf C, Maziak W, Lim S, Chung KF, Barnes PJ: Neutrophilic inflammation in severe persistent asthma. Am J Respir Crit Care Med 1999, 160:1532–1539.
Wenzel SE, Schwartz LB, Langmack EL, Halliday JL, Trudeau JB, Gibbs RL, Chu HW: Evidence That Severe Asthma Can Be Divided Pathologically into Two Inflammatory Subtypes with Distinct Physiologic and Clinical Characteristics. Am J Respir Crit Care Med 1999, 160:1001–1008.
Bhavsar P, Hew M, Khorasani N, Torrego A, Barnes PJ, Adcock I, Chung KF: Relative corticosteroid insensitivity of alveolar macrophages in severe asthma compared with non-severe asthma. Thorax 2008, 63:784–790.
Hew M, Bhavsar P, Torrego A, Meah S, Khorasani N, Barnes PJ, Adcock I, Fan Chung K, National Heart Lung and Blood Institute's Severe Asthma Research Program: Relative Corticosteroid Insensitivity of Peripheral Blood Mononuclear Cells in Severe Asthma. Am J Respir Crit Care Med 2006, 174:134–141.
Chung KFBP: Cytokines in asthma. Thorax 1999, 54:825–857.
Levy BD, De Sanctis GT, Devchand PR, Kim E, Ackerman K, Schmidt BA, Szczeklik W, Drazen JM, Serhan CN: Multi-pronged inhibition of airway hyper-responsiveness and inflammation by lipoxin A(4). Nat Med 2002, 8:1018–1023.
Levy BD, Bonnans C, Silverman ES, Palmer LJ, Marigowda G, Israel E, Severe Asthma Research Program NHLaBI: Diminished Lipoxin Biosynthesis in Severe Asthma. Am J Respir Crit Care Med 2005, 172:824–830.
Planaguma A, Kazani S, Marigowda G, Haworth O, Mariani TJ, Israel E, Bleecker ER, Curran-Everett D, Erzurum SC, Calhoun WJ, Castro M, Chung KF, Gaston B, Jarjour NN, BUSSE WW, Wenzel SE, Levy BD, NHLBI Severe Asthma Research Program (SARP): Airway Lipoxin A4 Generation and Lipoxin A4 Receptor Expression Are Decreased in Severe Asthma. Am J Respir Crit Care Med 2008, 178:574–582.
Robinson DS, Campbell DA, Durham SR, Pfeffer J, Barnes PJ, Chung KF: Systematic assessment of difficult-to-treat asthma. Eur Respir J 2003, 22:478–483.
Proceedings of the ATS Workshop on Refractory Asthma. Current Understanding, Recommendations, and Unanswered Questions Am J Respir Crit Care Med 2000, 162:2341–2351.
Levy BD, Romano M, Chapman HA, Reilly JJ, Drazen J, Serhan CN: Human alveolar macrophages have 15-lipoxygenase and generate 15(S)-hydroxy-5,8,11-cis-13-trans-eicosatetraenoic acid and lipoxins. J Clin Invest 1993, 92:1572–1579.
Nassar GM, Morrow JD, Roberts LJ, Lakkis FG, Badr KF: Induction of 15-lipoxygenase by interleukin-13 in human blood monocytes. J Biol Chem 1994, 269:27631–27634.
Profita M, Sala A, Siena L, Henson PM, Murphy RC, Paterno A, Bonanno A, Riccobono L, Mirabella A, Bonsignore G, Vignola AM: Leukotriene B4 Production in Human Mononuclear Phagocytes Is Modulated by Interleukin-4-Induced 15-Lipoxygenase. J Pharmacol Exp Ther 2002, 300:868–875.
Chavis C, Godard P, de Crastes Paulet A, Damon M: Formation of lipoxins and leukotrienes by human alveolar macrophages incubated with 15(S)-HETE: a model for cellular cooperation between macrophages and airway epithelial cells. Eicosanoids 1992, 5:203–211.
Serhan CN: Resolution Phase of Inflammation: Novel Endogenous Anti-Inflammatory and Proresolving Lipid Mediators and Pathways. Annual Review of Immunology 2007, 25:101–137.
Çelik GE, Erkekol FO, Misirligil Z, Melli M: Lipoxin A 4 levels in asthma: relation with disease severity and aspirin sensitivity. Clin Exp Allergy 2007, 37:1494–1501.
Wenzel S, Szefler S, Leung D, Sloan S, Rex M, Martin R: Bronchoscopic Evaluation of Severe Asthma. Persistent Inflammation Associated with High Dose Glucocorticoids. Am J Respir Crit Care Med 1997, 156:737–743.
Vachier I, Bonnans C, Chavis C, Farce M, Godard P, Bousquet J, Chanez P: Severe asthma is associated with a loss of LX4, an endogenous anti-inflammatory compound. J Allergy Clin Immunol 2005, 115:55–60.
Bonnans C, Vachier I, Chavis C, Godard P, Bousquet J, Chanez P: Lipoxins Are Potential Endogenous Antiinflammatory Mediators in Asthma. Am J Respir Crit Care Med 2002, 165:1531–1535.
Aderem AACDWSCZ: Bacterial lipopolysaccharides prime macrophages for enhanced release of arachidonic acid metabolites. J Exp Med 1986, 164:179.
Suzuki K, Yamamoto T, Sato A, Murayama T, Amitani R, Yamamoto K, Kuze F: Lipopolysaccharide primes human alveolar macrophages for enhanced release of superoxide anion and leukotriene B4: self-limitations of the priming response with protein synthesis. Am J Respir Cell Mol Biol 1993, 8:500–508.
Coffey MJ, Phare SM, Peters-Golden M: Prolonged Exposure to Lipopolysaccharide Inhibits Macrophage 5-Lipoxygenase Metabolism Via Induction of Nitric Oxide Synthesis. J Immunol 2000, 165:3592–3598.
Brock TG, McNish RW, Mancuso P, Coffey MJ, Peters-Golden M: Prolonged lipopolysaccharide inhibits leukotriene synthesis in peritoneal macrophages: mediation by nitric oxide and prostaglandins. Prostaglandins Other Lipid Mediat 2003, 71:131–145.
Huynh ML, Malcolm KC, Kotaru C, Tilstra JA, Westcott JY, Fadok VA, Wenzel SE: Defective Apoptotic Cell Phagocytosis Attenuates Prostaglandin E2 and 15-Hydroxyeicosatetraenoic Acid in Severe Asthma Alveolar Macrophages. Am J Respir Crit Care Med 2005, 172:972–979.
Levy BD, Clish CB, Schmidt B, Gronert K, Serhan CN: Lipid mediator class switching during acute inflammation: signals in resolution. Nat Immunol 2001, 2:612–619.
Brezinski ME, Serhan CN: Selective incorporation of (15S)-hydroxyeicosatetraenoic acid in phosphatidylinositol of human neutrophils: agonist-induced deacylation and transformation of stored hydroxyeicosanoids. Proc Natl Acad Sci USA 1990, 87:6248–6252.
Balter MS, Eschenbacher WL, Peters-Golden M: Arachidonic acid metabolism in cultured alveolar macrophages from normal, atopic, and asthmatic subjects. Am Rev Respir Dis 1988, 138:1134–1142.
Wenzel SE, Trudeau JB, Westcott JY, Beam WR, Martin RJ: Single oral dose of prednisone decreases leukotriene B4 production by alveolar macrophages from patients with nocturnal asthma but not control subjects: relationship to changes in cellular influx and FEV1. J Allergy Clin Immunol 1994, 94:870–881.
Damon M, Chavis C, Daures JP, Crastes dP, Michel FB, Godard P: Increased generation of the arachidonic metabolites LTB4 and 5-HETE by human alveolar macrophages in patients with asthma: effect in vitro of nedocromil sodium. Eur Respir J 1989, 2:202–209.
Laviolette M, Coulombe R, Picard S, Braquet P, Borgeat P: Decreased leukotriene B4 synthesis in smokers' alveolar macrophages in vitro. J Clin Invest 1986, 77:54–60.
Sorensen D, Kelly T, Murray D, Nelson D: Corticosteroids stimulate an increase in phospholipase A2 inhibitor in human serum. J Steroid Biochem 1988, 29:271–273.
Sano A, Munoz N, Sano H, Choi J, Zhu X, Jacobs B, Leff A: Inhibition of cPLA2 Translocation and Leukotriene C4 Secretion by Fluticasone Propionate in Exogenously Activated Human Eosinophils. Am J Respir Crit Care Med 1999, 159:1903–1909.
Vachier I, Chavis C, Majori M, Farce M, Bousquet J, Godard P, Chanez P: Effects of glucocorticoids on endogenous and transcellular metabolism of eicosanoids in asthma. Journal of Allergy and Clinical Immunology 2001, 107:824–831.
Yoss EB, Spannhake EW, Flynn JT, Fish JE, Peters SP: Arachidonic acid metabolism in normal human alveolar macrophages: stimulus specificity for mediator release and phospholipid metabolism, and pharmacologic modulation in vitro and in vivo. Am J Respir Cell Mol Biol 1990, 2:69–80.
Dworski R, Fitzgerald GA, Oates JA, Sheller JR: Effect of oral prednisone on airway inflammatory mediators in atopic asthma. Am J Respir Crit Care Med 1994, 149:953–959.
Levy BD, Lukacs NW, Berlin AA, Schmidt B, Guilford WJ, Serhan CN, Parkinson JF: Lipoxin A4 stable analogs reduce allergic airway responses via mechanisms distinct from CysLT1 receptor antagonism. FASEB J 2007, 21:3877–3884.
Kowal-Bielecka O, Kowal K, Distler O, Rojewska J, Bodzenta-Lukaszyk A, Michel BA, Gay RE, Gay S, Sierakowski S: Cyclooxygenase-lipoxygenase-derived eicosanoids in bronchoalveolar lavage fluid from patients with scleroderma lung disease: An imbalance between proinflammatory and antiinflammatory lipid mediators. Arthritis and rheumatism 2005, 52:3783–3791.
Mangino MJ, Brounts L, Harms B, Heise C: Lipoxin biosynthesis in inflammatory bowel disease. Prostaglandins & Other Lipid Mediators 2006, 79:84–92.
Lu MC, Peters-Golden M, Hostetler DE, Robinson NE, Derksen FJ: Age-related enhancement of 5-lipoxygenase metabolic capacity in cattle alveolar macrophages. Am J Physiol Lung Cell Mol Physiol 1996, 271:L547-L554.
Gangemi S, Pescara L, D'Urbano E, Basile G, Nicita-Mauro V, Dav¥ G, Romano M: Aging is characterized by a profound reduction in anti-inflammatory lipoxin A4 levels. Experimental Gerontology 2005, 40:612–614.
Acknowledgements
Supported by NIH-RO1 grants, HL-69155, HL69349 and AI068084. Conducted in collaboration with the Severe Asthma Research Program (SARP) funded by the NHLBI and consisting of: Brigham and Women's Hospital--Elliot Israel; Cleveland Clinic Foundation--Serpil C. Erzurum; Emory University--W. Gerald Teague; Imperial College London--Kian Fan Chung; National Jewish Medical and Research Center--Sally E. Wenzel; University of Pittsburgh & University of Texas Medical Branch--William J. Calhoun; University of Virginia--Benjamin Gaston; University of Wisconsin--William W. Busse; Wake Forest University--Eugene R. Bleecker; Washington University in St. Louis--Mario Castro; Data Coordinating Center--James R. Murphy; NHLBI--Patricia Noel.
The Authors declare that the Funding Bodies had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
PB has no conflicts of interest to disclose. BBL is a co-inventor on patents on lipoxins that are owned by Brigham and Women's Hospital that have been licensed for clinical development and are the subject of consultancies. MH has no conflicts of interest to disclose. MP has no conflicts of interest to disclose. SK has no conflicts of interest to disclose. EI has no conflicts of interest to disclose. KFC has participated on Advisory Boards of several pharmaceutical companies to discuss treatments used for asthma and COPD. He has received unrestricted grant money from one pharmaceutical company, and other grant money to participate in clinical trials.
Authors' contributions
KFC and BDL conceived the study, PB and MH collected the samples, MP, SK and BDL did the measurements of lipoxins, PB, BDL, EI and KFC wrote the manuscript. All the authors have read the and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bhavsar, P.K., Levy, B.D., Hew, M.J. et al. Corticosteroid suppression of lipoxin A4 and leukotriene B4from alveolar macrophages in severe asthma. Respir Res 11, 71 (2010). https://doi.org/10.1186/1465-9921-11-71
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1465-9921-11-71