Abstract
Background
Patient safety culture, an important aspect in the field of patient safety, plays an important role in the promotion of healthcare quality. Improved patient safety culture decreases patient readmission rates, lengths of hospital stay, and patient safety issues. Patient safety culture includes a set of dimensions. This review focuses on the differing perceptions of these dimensions among healthcare providers in hospitals.
Aims
This study aimed to identify studies examining healthcare providers’ perceptions of patient safety culture in hospitals and to summarize the data from these studies.
Method
Electronic database searching was based on the research question. Two electronic databases were used: CINHAL and Scopus. The search was limited to the period 2005–2012, and studies examining healthcare providers’ perceptions of patient safety culture were identified. Key terms were used to search the articles that were selected on the basis of inclusion and exclusion criteria. Articles examining healthcare providers’ perceptions of patient safety culture in hospitals without comparison between nurses and other healthcare professionals were selected.
Results
Eight articles were reviewed. Several questionnaires were used to assess healthcare providers’ perceptions of patient safety culture in these articles. Our review indicated differences in healthcare providers’ perceptions. In two articles, participants reported a high positive response to teamwork. In addition, participants in the other two articles reported a high positive response to job satisfaction.
Conclusion
The results of the current review reveal healthcare providers’ perceptions of patient safety culture. The results highlight that careful recognition and committed work on various scales/dimensions of patient safety culture can improve healthcare quality and consequently decrease patient safety issues associated with nursing care. Our findings also encourage hospital management and decision-makers to focus on and establish improvements in areas that will positively affect the quality of healthcare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Patient safety culture is an integral part of healthcare services. Healthcare has become complex, with the development of therapeutic interventions and new technologies. Such factors may negatively affect the level of healthcare provided and patient safety, according to the World Health Organization [1]. The Agency for healthcare Research and Quality (AHRQ) [2] has defined patient safety as “freedom from accidental or preventable injuries produced by medical care” and patient safety culture as “the extent to which an organization's culture supports and promotes patient safety” [3]. Patients are admitted to hospitals to be treated for health problems, but in some cases, patients are exposed to adverse events, such as medication errors, incorrect surgeries, nosocomial infections, falls in hospitals, and pressure ulcers. These events may injure patients and even lead to death, according to the World Health Organization [1]. Consequently, patient safety has become an important concern, owing to the prevalence of such adverse events, which have negatively affected patients and healthcare organizations.
The Harvard Medical Practice study has found that 4% of patients are exposed to adverse events. Of these adverse events, 70% of cause disability, and 14% lead to death, as reported by the World Health Organization [1]. The Department of Health and Children [4] of the Institute of Medicine has released a report called “To Err is Human: Building a Safer Health System,” which states that “there are between 44,000 and 98,000 preventable deaths annually due to medical error in hospitals.” Such adverse events not only affect patients (primary victims) but also have been reported to have psychological and psychosomatic effects, such as distress, anxiety, anger, and emotional stress, on healthcare providers as secondary victims [5]. Positive patient safety culture can reduce the occurrence of adverse effects [6].
Patient safety culture is one of several important aspects of patient safety. According to AHRQ, patient safety culture refers to the beliefs, values, and norms shared by healthcare and other staff in an organization that influence their conduct related to patient safety. Patient safety culture is measured by the values, beliefs, norms, and behaviors that are recognized, rewarded, expected, and accepted in an organization [3]. Additionally, AHRQ underscores the presence of patient safety culture at multiple levels, from the unit, department, and organization levels to the system level [3]. Hammer et al. [7] have stated that, because of the importance of patient safety culture, healthcare institutions perform improvement activities that create a positive culture. Patient safety culture assessment and interventions can improve the overall perceptions of patient safety [8]. Improvements in patient safety culture positively influence healthcare services. Positive patient safety culture decreases the readmission rate for patients and the length of hospital stay. Hospitals with a positive safety culture have reported low rates of adverse events [9, 10]. Patient safety culture is measured by several tools. According to The Health Foundation [9, 10], three main tools are used to assess patient safety culture. The first tool is the Hospital Surveys On Patient Safety Culture (HSOPSC), developed by the AHRQ in the United States. Its validity and reliability have been examined in several studies. The survey includes 12 dimensions for patient safety culture, measured by 42 items [11]. The dimensions are communication openness, feedback and communication about errors, handoffs and transitions, management support for patient safety, nonpunitive response to errors, organizational learning, overall perceptions of patient safety, staffing, supervisor/manager expectations, and actions promoting safety, teamwork across units, teamwork within units, and frequency of events reported [12]. The second tool is the Manchester patient safety culture assessment tool developed by the National Patient Safety Agency in the United Kingdom. It was developed to enable the National Health Service to assess patient safety culture improvement within healthcare organizations. The tool includes ten dimensions [13]: continual improvement, priority given to safety, system errors and individual responsibility, recording incidents, evaluating incidents, learning and effecting change, communication, personnel management, staff education, and teamwork [14]. The validity and reliability of this tool were tested in several studies on patient safety culture [9, 10]. The third tool is the Safety Attitudes Questionnaire (SAQ), which originated from the Flight Management Attitude Questionnaire used to assess safety culture in cockpits in airplanes [15]. This tool includes six domains focusing on the safety climate: safety climate, teamwork climate, stress recognition, perceptions of management, working conditions, and job satisfaction [14]. This questionnaire is valid and reliable according to previous studies [9, 10].
To gauge patient safety culture, it is crucial to consider nurses. Nurses make up the majority of healthcare professionals [16]. In addition, nurses play a pivotal role in healthcare settings, such as through ensuring steady bedside care and communicating with other healthcare providers, such as physicians and the pharmacists [17]. Nurse staffing and empowerment have been significantly associated with patient safety and patient safety culture, respectively [17, 18]. Consequently, the issues affecting nursing care should be examined and addressed in the assessment of patient safety culture in healthcare organizations.
Interest in patient safety culture assessment among nurses has become important [19]. Amiri et al. [18] have described patient safety culture as a culture in which nurses are cognizant of errors and are supported to discuss them. Several articles have assessed nurses’ perceptions of dimensions of patient safety culture in hospitals [16, 19,20,21,22,23,24,25]. However, no published reviews have systematically analyzed and summarized nurses’ perceptions of various patient safety culture dimensions and the differences in their perceptions across several descriptive socio-demographic variables. Such a comprehensive systematic review is essential to estimating and improving patient safety culture in healthcare settings. Therefore, in this study, articles associated with nurses’ perceptions of patient safety culture were systematically reviewed and summarized. This review also aims to present the differences in perceptions across various respondent characteristics, such as age, education, experience, hospital unit, and position at work.
2 Materials and Methods
2.1 Formulation of the Research Question
The research question was formulated on the basis of the following process. The area of interest was nurses’ perceptions of patient safety culture dimensions in hospitals. This area was selected because of its effects on healthcare services. The Patient/Population, Intervention, Comparison, and Outcomes (PICO) method was not appropriate for the formulation of the research question, because it is suitable for clinical research using interventions. Sample, Phenomenon of Interest, Design, Evaluation, Research type (SPIDER) is another method for research question formulation. The research question was formulated by using the items in the SPIDER framework, as shown in Table 1.
The research question was formulated as follows: What are nurses’ perceptions of patient safety culture in hospitals, according to questionnaires?
2.2 Inclusion Criteria
The specific inclusion criteria were as follows:
-
1.
Type of studies studies focusing on nurses’ perceptions of patient safety culture in hospitals, studies based on a descriptive design, studies using questionnaires to measure patient safety culture among nurses, regardless of questionnaire type.
-
2.
Country of studies studies focusing on measuring healthcare nurses’ perceptions of patient safety culture in any country worldwide.
-
3.
Place of studies studies measuring nurses’ perceptions of patient safety culture in one hospital, more than one hospital, all departments of a hospital, specific departments of a hospital, or one unit in a hospital, regardless of hospital type.
-
4.
Type of participants studies whose participants are nurses occupying various positions throughout a hospital.
-
5.
Qualification of participants studies in which participants are healthcare providers with qualifications such as a diploma, bachelor's degree, master’s degree or PhD.
-
6.
Experience of participants in work studies in which participants have different experiences, included without limitation.
-
7.
Nationality of participants studies on participants of all nationalities, included without limitation.
-
8.
Gender studies focusing on one gender or men and women, included without limitation.
-
9.
Age studies in all age groups, included without limitation.
-
10.
Outcome studies examining some or all dimensions of patient safety culture, for example, manager expectations, frequency of event reporting, rating overall perceptions of safety, number of events reported, patient safety grade, organizational learning, communication openness, communication, nonpunitive response to error, teamwork, hospital handoffs, and transitions, and staffing and hospital management support for patient safety.
2.3 Search Strategies
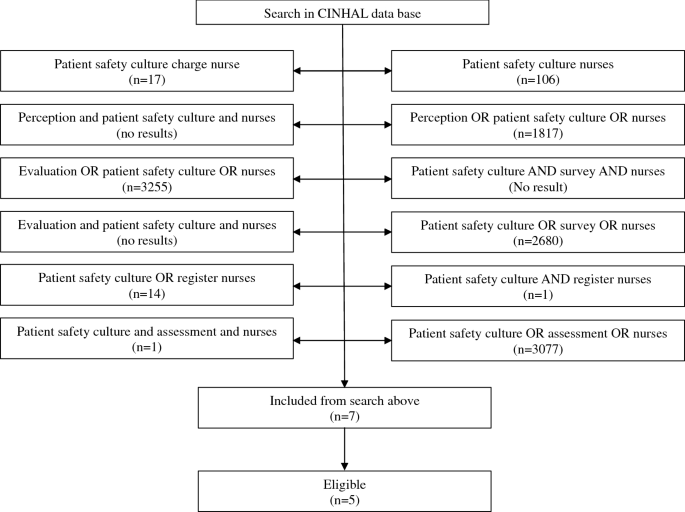
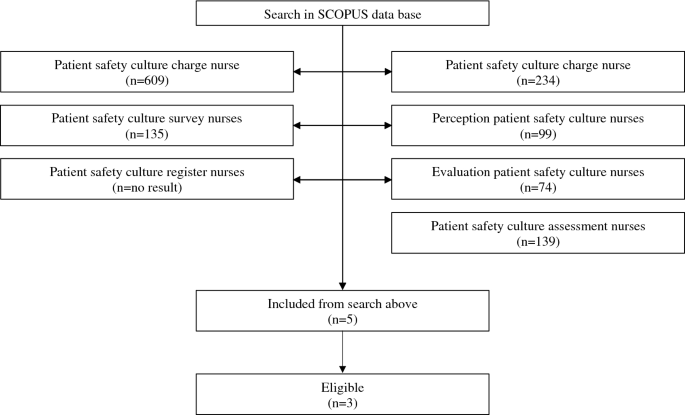
The search in the electronic database was based on the research question. Two electronic databases were used: Cumulative Index of Nursing and Allied Health Literature (CINHAL) and Scopus. Key terms and synonyms in the questions were used in the electronic search. Searching by using statements (patient safety culture nurses) provided 106 results in the CINHAL database and 609 results in the Scopus database. Another statement was used in searching, “patient safety culture charge nurses,” which yielded 17 results in the CINHAL database and 234 results in the Scopus Database. The advanced search in CINHAL using the terms “perception AND patient safety culture AND nurses” yielded zero results, whereas searching “perception OR patient safety culture OR nurses” yielded 1817 results. Using “perception patient safety culture nurses” and “patient safety culture survey nurses” in the Scopus database provided 99 and 135 results, respectively. An advanced search in the CINHAL database with “evaluation AND patient safety culture AND nurses” yielded zero results, whereas “evaluation OR patient safety culture OR nurses” provided 3255 results. The combined words “evaluation patient safety culture healthcare providers” in the Scopus database yielded 74 results. An advanced search in the CINHAL database by using “patient safety culture AND survey AND healthcare providers” yielded zero results, whereas “patient safety culture OR survey OR healthcare providers” gave 2680 results. A search in the Scopus database by using the combined words “patient safety culture survey nurses” provided 135 results. Using “patient safety culture AND registered nurses” gave 1 result, and using “patient safety culture OR registered nurses” gave 14 results. Scopus database searching using the combined words “patient safety culture registered nurses” yielded zero results, whereas using “evaluation patient safety culture” gave 74 results. An advanced search in the CINHAL database for “patient safety culture AND assessment AND nurses” provided 1 result. Using “patient safety culture OR assessment OR nurses” gave 3077 results. In the Scopus database, using “patient safety culture assessment nurses” provided 139 results (see Figs. 1 and 2).
No restriction was applied to search for articles according to the country of study, whereas restrictions were applied to the language of articles and period of publication. The language of the articles was limited to English, and the period of publication was limited to 2005–2012. In addition, the search was limited to studies with full text and abstract availability.
2.4 Study Selection Procedures
Studies were selected according to the following procedures. The title and abstract in each article were scanned, and articles were assessed according to the inclusion criteria. Articles measuring nurses’ perceptions of patient safety culture in hospitals, in specific departments, or in one department in a hospital, were included. Articles not associated with the review topic, such as those examining the relationship between patient safety culture and the level of healthcare, articles measuring the effects of patient safety culture improvement programs, and articles in which the full text or abstract was not available were excluded from this systematic review.
2.5 Data Extraction and Synthesis
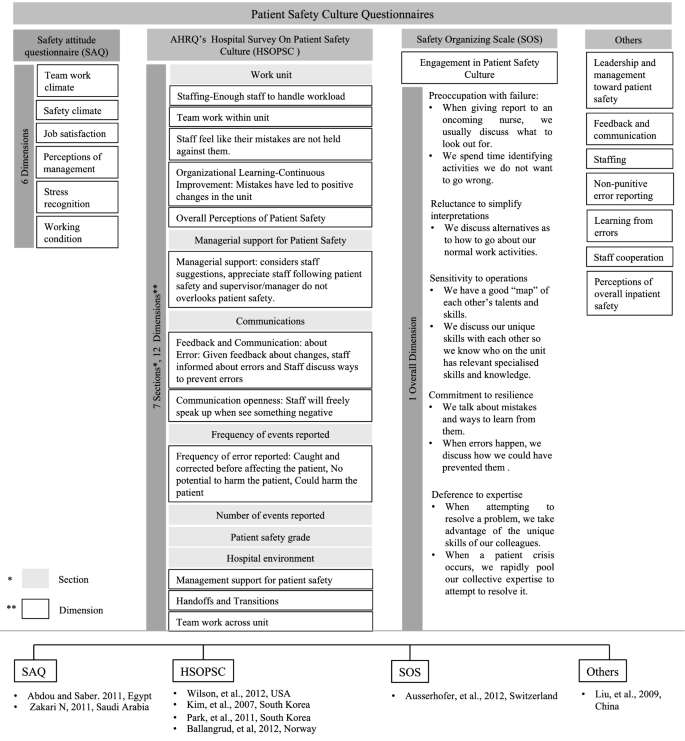
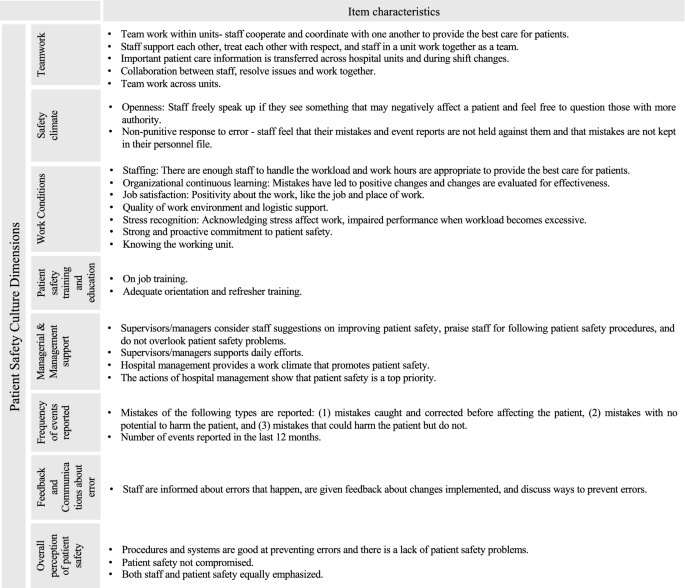
Data were extracted from each eligible article. The key aspects of each article were extracted, including the location of the study, sample size, response rate, healthcare providers' work experience, healthcare providers' age, nurses’ qualification, study design, type of questionnaire, method of data analysis, patient safety culture dimensions, and duration of data collection. In addition, data associated with the results were extracted, which included healthcare providers’ perceptions of patient safety culture. Because the articles included in this review presented the perceptions of nurses according to multiple questionnaires (Fig. 3), data comparability was important for identifying the direction and the gaps of the patient safety culture perception. On the basis of the commonalities among surveys, we grouped the results from these studies into seven patient safety culture dimensions, as shown in Fig. 4 [26].
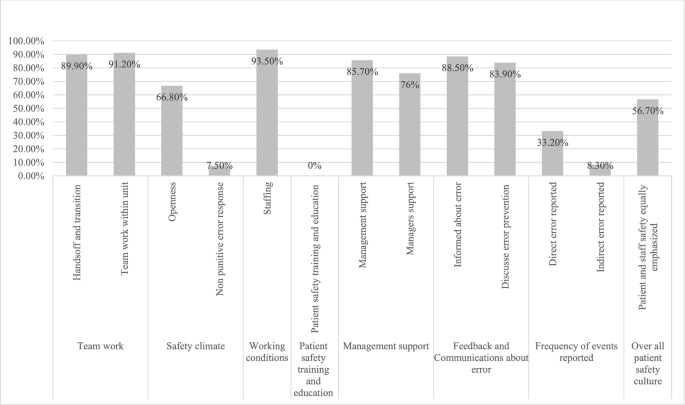
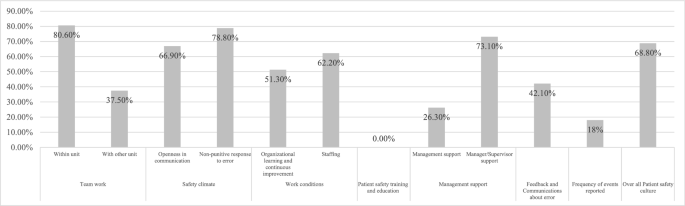
Nurses’ perceptions of patient safety culture by Liu et al. [16]: the percentage of nurses (y-axis) agreeing to various items across each patient safety culture dimension (x-axis)
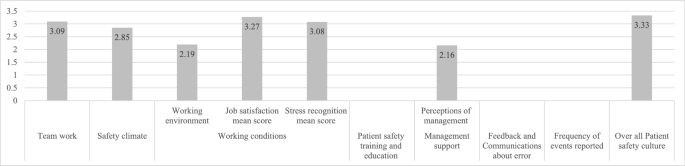
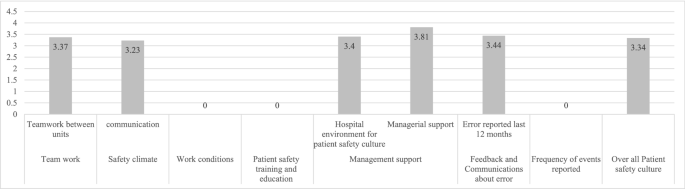
Nurses’ perceptions of patient safety culture by Abdou and Saber [19]: the mean scores (y-axis) of the patient safety culture dimensions (x-axis)
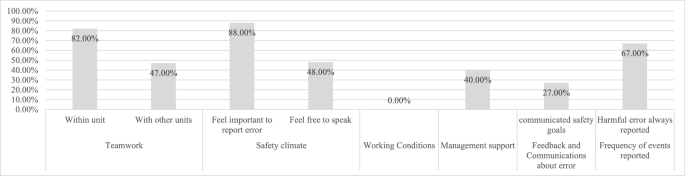
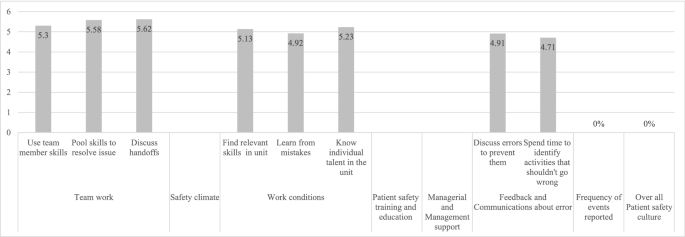
Nurses’ perceptions of patient safety culture by Kim et al. [21]: the percentage of nurses (y-axis) strongly agreeing with various items across each patient safety culture dimension (x-axis)
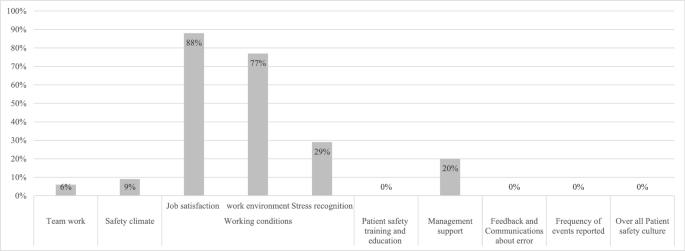
Nurses’ perceptions of patient safety culture by Zakari [22]: the percentage of nurses with a positive patient safety attitude (y-axis) toward the various patient safety dimensions (x-axis)
Nurses’ perceptions of patient safety culture by Park et al. [23]: the mean scores of some items (y-axis) of the patient safety culture dimensions (x-axis)
Nurses’ perceptions of patient safety culture by Ausserhofer et al. [12]: the mean scores of various items (y-axis) of the patient safety culture dimensions (x-axis)
Nurses’ perceptions of patient safety culture by Ballangrud et al. [25]: the registered nurses' positive scores (y-axis) for various items of the patient safety culture dimensions (x-axis)
The extracted data were synthesized in a simple manner. Attitude was considered highly positive if the article reported the score as positive or having a scale score > 75; attitude was considered positive/desirable if an item had a mean score > 3 on a 5-point Likert scale or > 4 on a 7-point Likert scale, i.e., “strongly agree,” “agree,” or “somewhat agree” [22, 26].
Quality assessment strategy The quality of selected articles was assessed on the basis of questions in the critical appraisal tool for cross-sectional designs (Joanna Briggs Institute’s critical appraisal tool available on the website of the University of Adelaide) [27]. This tool provides a checklist for assessing the quality, relevance, and reliability of analytical cross-sectional studies. Questions in the checklist focus on the inclusion relevance, appropriateness of study design, appropriateness of the population in the study, response rate, validity of questionnaires, and statistical methods used for analysis of results. The assessment of the quality of selected articles indicated that all eight articles [16, 19,20,21,22,23,24,25] were relevant to this project. In the selected articles, researchers provided background and overviews of previous articles associated with the area of research. Moreover, the aim of the study was stated in each article; this aspect was important to ensure that the findings were relevant to the aim of this study and that no bias was present. No systematic bias was present in the selected articles, because of their appropriate study design. All eight articles used a cross-sectional design, which was suitable for the aim of each study. In addition, articles were assessed on the basis of other criteria. Samples in eight articles were considered representative, because the target population in each article was hospital nurses. Seven articles measured nurses’ perceptions of patient safety culture in a hospital [16, 19,20,21,22,23,24]; one study targeted the population of nurses in an intensive care unit (ICU) in a hospital [25]. The participant selection procedure in each article was explained. In some articles, researchers randomly selected the place of the study and targeted the entire population. All healthcare providers in selected departments were included, thus ensuring no bias in the participant selection procedure [9]. Confounding factors were not identified during bias assessment, because the studies included measured behavioral and attitudinal factors [27]. The appraisal was scored as “yes,” “no,” “unclear,” and “not applicable,” and was later converted to a percentage. For measuring the risk of bias, a score above 70 indicated low bias, a score of 50–69 indicated moderate bias, and a score < 49 indicated high bias [6]. A summary is presented in Table 2.
3 Results
3.1 Characteristics of the Included Studies
The selected studies showed marked diversity with respect to study location, encompassing four continents: Asia [16, 21,22,23], Europe [24, 25], North America [20], and Africa [19]. These studies also varied in hospital number and size. The included studies presented the perceptions of respondents from a single hospital [19, 20, 22, 23] to as many as 35 hospitals [24]. Respondent nurses with roles as diverse as clinical or ambulatory nurses, and nurse managers were included in these studies (Table 3). Differences in sample size, response rate, and participants’ characteristics were observed among the selected articles. Ausserhofer et al. [24] had the largest study sample size among the selected articles (n = 1633), with a response rate of 72%. The second highest sample size was n = 886, with a response rate of 92.3%, in a study by Kim et al. [21]. The lowest sample size was n = 126, but the study had a response rate of 100% [23]. Data are provided in Table 2.
Participants in these eight articles had different characteristics with respect to age, working experience, hospital unit, and qualifications. In some articles, the researchers did not report some of the participants’ characteristics, for example, the age of participants [20]. Data are shown in Table 3.
3.2 Assessment of Patient Safety Culture
The studies included in this review assessed the nurses’ overall perceptions of patient safety culture through surveys. The most common survey questionnaire used was the HSOPSC [20, 25]. The survey measured patient safety culture under 12 dimensions, as described above. Two studies used the Korean translated version of the same survey [21, 23]. The SAQ, typically measuring six domains (as listed above) of patient safety culture, was also used by some included studies [19, 22]. The Safety Organizing Scale (SOS) questionnaire, which assesses engagement in patient safety culture through nine items under the single domain of engagement in patient safety culture was also used in one of the studies [24]. Liu et al. [16] used a custom two-part survey constructed from existing surveys, which was tested before being administered to the respondents. That study assessed patient safety culture under the following domains: leadership and management regarding patient safety, feedback and communication about errors, staffing, nonpunitive error reporting, learning from errors, staff cooperation, and perceptions of overall inpatient safety. Although different questionnaires were used, and some were translated into the respondents’ language [19, 21, 23,24,25], all were verified for reliability/validity. Most of the studies scored the items of patient safety culture dimensions on a 5-point Likert scale [19,20,21,22,23, 25], with reverse scoring for negative questions. One study used a 7-point Likert scale [24], and one study used a yes/no format [16]. Data are shown in Table 4. The results of nurses’ perceptions of patient safety culture dimensions, as reported by the authors, are represented herein through bar graphs in Figs. 5, 6, 7, 8, 9, 10 and 11 in which the x-axis represents assessed dimensions of patient safety culture and the y-axis represents the percentage of positive responses [16, 21, 22, 25] or the mean score of a dimension [19, 23, 24].
Because different patient safety culture assessment questionnaires were used in the reviewed articles, for ease of understanding and discussion, the observations are discussed under the following dimensions: teamwork, safety climate, working conditions, management support, frequency of errors reported, feedback and communication, and overall patient safety culture [26]. The characteristic items of these dimensions that were considered in reviewing the articles are shown in Fig. 4.
3.3 Teamwork
On the basis of the HSOPSC survey, between 80.6% [25] and 82.6% [21] of nurses strongly agreed that staff were supported within the working unit, and 30% of nurses strongly agreed that physicians and nurses worked well as a team, whereas only 39.3% strongly agreed about teamwork between units [21]. Additionally, the perceptions of handling handoff and transition during shift changes were considered positive by only 57.3% [25] of nurses, whereas approximately 56.8% considered the shift change problematic [21]. A total of 58% of nurses expressed that important patient care information is often lost during shift changes, and 56% found difficulty in approaching physicians [21]; 47.1% indicated that hospital units do not coordinate, and 49.5% indicated unpleasant feelings in working with other units [21]. In a study from South Korea, collaboration between units received a mean score of 3.37 ± 0.40 [23], thus suggesting fairly good and positive cooperation between units. Similarly, the teamwork perceptions inferred through the SAQ received a mean score of 3.09 ± 0.78 [19], whereas the perspective of ambulatory nurses’ regarding teamwork was lowest, with only 6% positive perception [22]. The SOS questionnaire revealed that discussion during handoffs received a mean score of 5.62 ± 1.074, with nurses agreeing to a good extent [24]. Considerable agreement, with mean scores of 5.34 ± 1.154 and 5.58 ± 1.060, was observed for using one another’s skills to resolve an issue and teams acting collectively during crises, respectively [24]. According to other questionnaires, teamwork within a unit was perceived to be positive by 91.2% of the nurses [16]. The shift change procedure was considered to promote patient safety by 89.9% [16].
3.4 Safety Climate
According to the HSOPSC survey, only 15% of nurses perceived feeling free to reporting an error [21]; 66.9% expressed a positive attitude to openness to communication [25], whereas communication among clinicians was fair, with a mean score of 3.23 ± 0.40 [23]. A total of 78.8% felt positive about the nonpunitive response to error reporting [25], 88% believed in the importance of reporting errors, and 77.3% felt that errors must be reported even if they cause no harm [21]. A total of 48% felt free to speak regarding errors, 27% felt free to question authority, and 38% felt free to voice opinions different from those in authority [21]. By contrast, with the SAQ, safety climate received a mean score of 2.85 ± 0.97 [19], which translated to a neutral positive attitude, and organizational commitment toward patient safety was expressed positively by only 9% [23]. Through the other questionnaire, 66.8% of staff reported feeling free to report errors [16], 92.2% believed that the person committing the error would be punished, and 90.3% believed that the person making the error was responsible for the consequences [16]. Here, making an error was also considered shameful by 69.11% [16]. The SOS questionnaire did not assess the safety climate dimension.
3.5 Working Conditions
Through the SAQ, perceptions of job satisfaction and stress recognition were reported positively by 88% and 29% of nurses, respectively [22]. In another study using the SAQ, job satisfaction received a mean score of 3.27 ± 0.61 [19], reflecting a neutral attitude among nurses. Similarly, stress recognition received a mean score of 3.08 ± 1.02 [19]. The working conditions were perceived positively by 77% of nurses [22] and received a mean score of 2.19 ± 0.79 in another study [19]. According to the HSOPSC questionnaire, organizational learning and continual improvement were positively perceived by 51.3% [25], whereas 62% considered that the working unit had sufficient staff for the given workload [25]. Through the other questionnaire, the number of staff present to handle the workload was considered sufficient by 93.5% of nurses [16]. Some characteristic perceptions emerged through the SOS questionnaire. A discussion to identify the suitable skills among the working unit staff was agreed upon to a considerable extent by responding nurses, with a mean score of 5.13 ± 1.237. Similarly, having a map of the abilities of the staff in the working unit received a mean score of 5.23 ± 1.073 [24], and learning from mistakes received a mean score of 4.92 ± 1.25.
3.6 Management Support
According to the HSOPSC questionnaire, six Norwegian hospitals reported a low rate of 26.3% positivity regarding management support [25], whereas 40% indicated that management cared more about cutting costs than patient safety culture [21]. The mean score for hospital work environment promoting patient safety was 3.4 ± 0.62, whereas that for managerial support was 3.81 ± 0.54, inclining toward “agree” [23]. Managerial support for patient safety was perceived positively by 73.1% [25]. The perception of management support for patient safety culture according to the SAQ questionnaire revealed that 9% of nurses had a positive attitude [22]; another article reported a mean of 2.16 ± 0.59 for perceptions regarding management [19], thus indicating agreement to a very limited extent. In the article using the other questionnaire, 85.7% considered hospital administrators to have patient safety as a priority, and 76% indicated managerial support for patient support [16]. The SOS questionnaire did not address the dimension of management support for establishing patient safety culture.
3.7 Frequency of Errors Reported
Results obtained with the HSOPSC questionnaire indicated that 18% of nurses had a positive attitude toward reporting an error [25]; 67% [21] of nurses considered reporting errors that harmed patients, whereas 66% [21] always reported mistakes that resulted in patient harm. For the number of errors reported in the previous 12 months, the mean was 3.44 for one or two events being reported [23]. However, 50% were unclear on what type of errors to report [21]. The other questionnaire highlighted direct and indirect patient safety error reporting systems [16], wherein 33.3% agreed that direct errors were always reported, and 8.3% agreed that indirect errors were always reported. With the SAQ and the SOS questionnaires, the perceptions of nurses regarding the frequency of error reporting were not documented.
3.8 Feedback and Communication
According to the HSOPSC questionnaire, 52% reported receiving feedback on errors committed, whereas 66% of respondents felt that their suggestions to improve patient safety were ignored [21]. A total of 42.1% indicated a positive attitude toward feedback and communication [25]. A total of 27% reported that hospital leaders successfully communicated patient safety goals [21]. Other questionnaires revealed that 88.5% of respondents agreed that they were informed when an error occurred in their unit [16]. The SOS and another questionnaire shed light on openness toward discussing error causes and prevention, which was affirmed by 70.1% [24] and 83.9% [16] of respondents, respectively, whereas 67.3% [24] affirmed discussions on identifying activities that should never occur through the SOS questionnaire. The SAQ questionnaire did not elaborate on the feedback and communication dimension of patient safety culture.
3.9 Overall Patient Safety Culture
According to the HSOPSC questionnaire, 68.8% [25] indicated that nurses showed a positive attitude toward overall patient safety culture. However, 83% strongly agreed or agreed that more serious errors did not occur only because of chance, expressed negative perceptions of overall patient safety [21], and had negative perceptions of overall patient safety culture. The SAQ questionnaire results indicated that the mean for overall perceptions of safety culture was 3.33 ± 0.58, indicating near neutral opinions toward patient safety culture [19]. The other questionnaire revealed that 56.7% agreed to equal emphasis on patient and staff safety [16] and 67% expressed that no safety committee (system) is present in the hospital [16].
3.10 Differences in Perceptions Across Descriptive Variables
Differences in respondents’ perceptions of patient safety culture dimensions were reported across descriptive variables, such as the hospital unit or hospital, position at work, age, experience, education level, marital status, working hours, and language region of the respondents. All the reported differences in perceptions are presented in Table 5. The perceptions of overall patient safety culture dimensions among healthcare providers in the ICU were reported to be higher (3.38 ± 0.51) than those among coronary care unit (CCU) nurses (3.34 ± 0.46) followed by general unit nurses (3.32 ± 0.60) [19]. CCU unit nurses were more perceptive to stress recognition [19]. Technical healthcare providers showed higher positivity for overall patient safety culture dimensions (mean score of 3.41 ± 0.54) than professional nurses (3.23 ± 0.61) [19]. Similarly, regarding job satisfaction, the mean scores among technical nurses were higher (3.07 ± 0.0.91) than those among professional nurses (2.56 ± 0.98) [19]. Registered nurses had more positive attitudes toward stress recognition and acknowledgment of the effects of stress on patient safety than nurse managers [22]. In addition, perceptions of management were higher among nurse managers than registered nurses [22]. A significant difference (P < 0.05) was found between work position and job satisfaction dimension. The nurse managers had greater positive attitudes than registered nurses [19]. In addition, significant differences (P < 0.05) were observed among head nurses, staff nurses, and charge nurses. Head nurses reported higher positive perceptions of patient safety culture in their units [21]. They also reported more errors [21]. Respondent age significantly influenced perceptions [19, 21]. Nurses above 40 years of age responded more positively toward patient safety culture dimensions than younger nurses [19, 21]. Respondent experience also influenced overall patient safety culture perceptions [20, 21], job satisfaction [19], communication [23], and the frequency of error reporting [21]. Education level and marital status have been reported to affect respondents’ job satisfaction [19]. Moreover, working hours influenced the perceptions of job satisfaction, teamwork, safety climate, and overall patient safety [19]. Notably, an influence of language region on the perceptions of the respondents was observed [24]. Data are shown in Table 5.
4 Discussion
In this systematic review, eight articles were selected, on the basis of specific criteria of showing different healthcare providers’ perceptions of patient safety culture. The participants in the selected articles reported high perceptions regarding several characteristic items of patient safety culture dimensions, such as teamwork within a unit, discussing handoff during shift change, discussing and preventing errors, job satisfaction, and having sufficient staff for the workload in a unit and managerial support. Similarities were observed among several selected articles concerning several findings. The respondents’ perceptions of teamwork within the unit were reported to be highly positive across all studies except those using the SAQ [19, 22]. Moreover, a positive attitude toward teamwork within the unit was reported to be highest in one study using the HSOPSC questionnaire [25]. However, teamwork across units was perceived comparatively less positively [21, 25]. Ineffective teamwork in hospitals negatively affects healthcare, and this aspect was one cause of adverse events in the ICU, as reported by Ballangrud et al. [25]. Nurses reported the highest positive perceptions of effective teamwork at the unit level and not across units because they might experience feelings of being part of a team, which seldom occur with other teams, which are often viewed critically [24]. The finding was in agreement with those of a study reported by Georgiou et al. [28], wherein teamwork within a unit was perceived more positively than safety climate, because of the implementation of quality systems at the unit level. In a study involving multicultural nurses, negative perceptions of nurses toward teamwork have been reported to be due to language and cultural differences [22]. Job satisfaction, an item in the work condition dimension, has been perceived positively by nurses [19]. Glendon and Mckenna, in 1995, expressed that the characteristics of an organization with high patient safety culture are high positive job satisfaction and effective communication [19]. This aspect has also emerged in studies conducted through the SAQ questionnaire, wherein the perceptions of job satisfaction ranked first [22] and second [19] among other dimensions of patient safety culture. In the dimension of managerial and management support, the analyzed results indicated positive managerial perceptions but low perceptions of management regarding patient safety culture, according to the SAQ questionnaire [19, 22], and of management support, according to the HSOPSC questionnaire [21, 23, 25]. The not very positive attitude toward management support for patient safety culture might be attributable to management decisions not to form patient safety committees [16]. Among these articles, a study conducted in Norway [25] has shown low positive attitudes toward management support, because the health personnel had undergone considerable reorganization and efficiency improvement in the past few years [29], and the management was more focused on production than communication [30]. By contrast, a study on Chinese hospitals has reported high positive perceptions among nurses regarding hospital management support [16]. Huang et al. [31] have also recognized the importance of management and organizational commitment in improving patient safety culture. The Department of Health and Children (Dublin, Ireland) [4] has noted a strong association between the management of healthcare institutions and positive patient safety culture. However, the SOS questionnaire does not cover the perceptions of management while assessing the dimensions of patient safety culture. In addition, it does not address several aspects of the safety climate dimension. Findings for other dimensions indicated the close link between the dimensions of safety climate and frequency of errors reported: the results showed low positive perceptions of the frequency of error reporting along with negative perceptions toward nonpunitive responses to errors (an item of the safety climate dimension). Although the importance of reporting errors was perceived positively by 88% of the respondents, as expressed through the HSOPSC questionnaire [21], the frequency of error reporting was low among the nurses [25], and negative perceptions of nonpunitive response to error were observed [16]. The reason for this behavior might be a fear of repercussions from colleagues and punishment from management [19]. Making errors was considered shameful by 69.11% of the respondents [16]. A closely related factor involves feedback and communication regarding errors. That dimension also received a low positive response [21, 25], as expressed through the HSOPSC questionnaire. However, negligence in patient safety and risks to critically ill patients can be effectively diminished through fostering communication and the flow of information [32]. The low error reporting frequency was also associated with low feedback and communication about errors [25]. Discussing the possible causes of error and establishing an effective feedback system are essential for patient safety [16]. Positive attitudes toward feedback and communication, and reporting of errors can be increased if a working unit’s reporting system is blame-free and considers errors as system failures [30]. Finally, this review highlights variations in perceptions of patient safety culture dimensions across multiple descriptive variables, such as the hospital unit or hospital, position at work, experience, age, education, marital status, working hours, and language region. The differences in perceptions of patient safety across working units in a hospital are attributable to variations in culture across units [31]. The variations in perceptions due to differences in position may be explained by their direct effects on patients. Technical nurses did not directly affect patients, unlike professional nurses; thus, they felt more positive toward patient safety culture [19]. Nurses who had less experience and were young perceived patient safety culture negatively, because of high perceptions of stress and low job satisfaction [21]. Finally, the effects of the language region on positive perceptions were considered to be due to more patient safety programs being introduced in certain regions [25].
Interestingly, although prominent safety culture assessment questionnaires were used, some important patient safety culture dimensions were not measured. The SAQ [19, 22] and SOS [24] questionnaires do not report the frequency of error reporting—an important dimension to assess overall patient safety. Moreover, the SOS questionnaire does not report management support and items of safety climate, and the SAQ does not cover feedback and communication aspects of patient safety culture. However, a customized questionnaire used by Liu et al. [16] has been used to investigate all dimensions of patient safety culture missed by the other questionnaires. In addition, the SOS survey includes questions not covered by other surveys. In the future, a notable practice to enhance patient safety culture will be encouraging and fostering on-job training and educational programs. The studies included in this review unexpectedly did not analyze the importance of on-job training and education while assessing various patient safety culture dimensions. The importance of on job training programs has effectively been documented by Ginsburg et al. [30], and an interventional training program has been found to enhance the perceptions of patient safety culture among nurse leaders [33]. Similarly, Al Mutair et al. have reported a decrease in hospital-acquired pressure ulcers through the implementation of an educational program. The educational program significantly decreased the number of hospital-acquired pressure ulcers, even though the number of inpatients tripled in 2018 [34]. Morello et al. [35] have stated that educational activities in hospitals positively affect patient safety culture. Involving staff in the implementation of updated policy and procedures and setting documentation requirements in addition to key performance indicator tracking will reinforce new behaviors in a strong care culture [36]. A lack of knowledge and information among healthcare workers can also weaken healthcare delivery [37]. Results from the reviewed studies by AlJohani et al. have shown that high-level knowledge of precautionary measures affects compliance with needle safety precautions. Thus, updating knowledge and information greatly affects patient safety in several ways. On-job training, appropriate programs, and an effective feedback system are critical to incident reporting and overall patient safety [38]. In addition, health organizations must use an effective reporting environment for the process of medication use to ensure sounder practice [39].
4.1 Limitations
This review has several limitations. One is the limited number of articles in the electronic database associated with nurses’ perceptions of patient safety culture in hospitals, given that the field of patient safety culture is considerably new, and researchers have only recently begun conducting studies in this area, in the past few years. Another limitation is the unavailability of published reviews on nurses’ perceptions of patient safety culture in hospitals. Therefore, we were unable to compare the results of this review. In addition, the association between descriptive variables and patient safety culture dimensions was not calculated in some selected articles. The included studies were also characterized by specific limitations, such as limited sample sizes and nurses belonging to a single hospital, thus making the overall results difficult to generalize [19, 20, 22, 23]. Similarly, a limitation was also observed for a study based in a single city [16]. The self-reporting survey design is also considered a limitation, because of potential doubts regarding the trustworthiness of the respondents’ answers [22]. The risk of bias is also a limitation, owing to the lack of random sampling [24]. The SOS provides information on patient safety behavior but not other patient safety culture dimensions, such as a blame-free environment or management support for patient safety [24]. Despite these limitations, including the small sample sizes, the results provided information regarding the level of patient safety culture in hospitals. These findings may be considered by decision-makers in other small hospitals.
5 Conclusion
Patient safety culture is an important component of patient safety. Improvement in patient safety culture positively affects the quality of healthcare. The perceptions of patient safety culture dimensions among nurses are dissimilar; however, promoting patient safety culture can minimize issues that affect patient safety and consequently errors in patient safety. Through this systematic review, we presented substantial observations that may help foster patient safety culture in healthcare organizations. First, a comprehensive assessment of patient safety culture requires rigorous considerations while selecting an assessment tool that encompasses most, if not all, patient safety culture dimensions. In the future, although teamwork within a unit is generally perceived positively, improvement in teamwork across units in a healthcare organization can additionally contribute to the building of patient safety culture. Furthermore, management support is another key contributor to patient safety culture and must be improved. In addition, to ameliorate error reporting, a nonpunitive attitude toward error reporting must be fostered simultaneously with strengthened communication. Ultimately, substantial improvements in the availability and accessibility of on-job training and continuing education are necessary to achieve and sustain a robust patient safety culture. In conclusion, careful recognition and committed work on various scales/dimensions of patient safety culture can lead to improvements in the quality of healthcare and consequently decrease patient safety issues associated with nursing care. These results may provide direction and guidance for healthcare management and decision-makers in focusing and establishing improvement in areas that will positively affect the quality of healthcare.
Data availability
Data used and analyzed in this study are available on request.
Abbreviations
- CINHAL:
-
Cumulative Index of Nursing and Allied Health Literature
- SAQ:
-
Safety Attitudes Questionnaire
- SPIDER:
-
Sample, Phenomenon of Interest, Design, Evaluation, Research type
- HSOPSC:
-
Hospital Survey on Patient Safety Culture survey
- SOS:
-
Safety Organizing Scale
- ICU:
-
Intensive care unit
- CCU:
-
Coronary care unit
References
World Health Organization. World alliance for patient safety: WHO draft guidelines for adverse event reporting and learning systems: from information to action. 2005. https://apps.who.int/iris/handle/10665/69797. Accessed 2 Mar 2022.
Zrelak PA, Utter GH, Sadeghi B, Cuny J, Baron R, Romano PS. Using the Agency for Healthcare Research and Quality patient safety indicators for targeting nursing quality improvement. J Nurs Care Qual. 2012;27(2):99–108.
Agency for Healthcare Research and Quality. What Is Patient Safety Culture? [Internet]. [cited 2022 May 23]. https://www.ahrq.gov/sops/about/patient-safety-culture.html. Accessed 23 May 2022.
Building a Culture of Patient Safety: Report of the Commission on Patient Safety and Quality Assurance [Internet]. 2008 [cited 2022 Feb 22]. https://www.gov.ie/en/publication/5d9570-building-a-culture-of-patient-safety-report-of-the-commission-on-pat/. Accessed 22 Feb 2022.
Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and psychosomatic symptoms of second victims of adverse events: a systematic review and meta-analysis. J Patient Saf [Internet]. 2020 Jun [cited 2022 Feb 22];16(2):61–74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386870/. Accessed 22 Feb 2022.
Alanazi FK, Sim J, Lapkin S. Systematic review: Nurses’ safety attitudes and their impact on patient outcomes in acute-care hospitals. Nurs Open. 2022;9(1):30–43.
Hammer A, Ernstmann N, Ommen O, Wirtz M, Manser T, Pfeiffer Y, et al. Psychometric properties of the Hospital Survey on Patient Safety Culture for hospital management (HSOPS_M). BMC Health Serv Res [Internet]. 2011;11(1):165. https://doi.org/10.1186/1472-6963-11-165.
Adams-Pizarro I, Walker Z, Robinson J, Kelly S, Toth M. Using the AHRQ Hospital Survey on Patient Safety Culture as an Intervention Tool for Regional Clinical Improvement Collaboratives. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 2: Culture and Redesign) [Internet]. 2008 [cited 2022 Feb 22]; http://www.ncbi.nlm.nih.gov/books/NBK43728/. Accessed 22 Feb 2022.
Lachman P, Linkson L, Evans T, Clausen H, Hothi D. Developing person-centred analysis of harm in a paediatric hospital: a quality improvement report. BMJ Qual Saf. 2015;24(5):337–44.
Pittet D, Donaldson L. Challenging the world: patient safety and health care-associated infection. Int J Qual Health Care. 2006;18(1):4–8.
Sorra J, Gray L, Streagle S, Famolaro T, Yount N, Behm J. AHRQ Hospital Survey on Patient Safety Culture: User’s Guide [Internet]. AHRQ Publication; 2016 [cited 2022 Feb 22]. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospcult.pdf. Accessed 22 Feb 2022.
Hao HS, Gao H, Li T, Zhang D. Assessment and Comparison of Patient Safety Culture Among Health-Care Providers in Shenzhen Hospitals. RMHP [Internet]. 2020 Sep 11 [cited 2022 May 23];13:1543–52. https://www.dovepress.com/assessment-and-comparison-of-patient-safety-culture-among-health-care--peer-reviewed-fulltext-article-RMHP. Accessed 23 May 2022.
NPSA: Manchester Patient Safety Framework (2006) [Internet]. Patient Safety Learning - the hub. [cited 2022 Mar 2]. https://www.pslhub.org/learn/culture/safety-culture-programmes/incentives-and-techniques/npsa-manchester-patient-safety-framework-2006-r753/. Accessed 02 Mar 2022.
Measuring safety culture-The Health Foundation [Internet]. 2011 [cited 2022 May 23]. https://www.health.org.uk/publications/measuring-safety-culture. Accessed 23 May 2022.
Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res [Internet]. 2006;6(1):44. https://doi.org/10.1186/1472-6963-6-44.
Liu Y, Kalisch BJ, Zhang L, Xu J. Perception of safety culture by nurses in hospitals in china. J Nurs Care Qual. 2009;24(1):63–8.
Malliaris AP, Phillips J, Bakerjian D. Nursing and Patient Safety [Internet]. Patient Safety Network. 2021 [cited 2022 Feb 22]. https://psnet.ahrq.gov/primer/nursing-and-patient-safety. Accessed 22 Feb 2022.
Amiri M, Khademian Z, Nikandish R. The effect of nurse empowerment educational program on patient safety culture: a randomized controlled trial. BMC Medical Educ [Internet]. 2018. https://doi.org/10.1186/s12909-018-1255-6.
Abdou H, Saber K. A baseline assessment of patient safety culture among nurses at Student University Hospital. World J Med Sci. 2011;1(6):17–26.
Wilson D, Redman RW, Talsma A, Aebersold M. Differences in perceptions of patient safety culture between charge and noncharge nurses: implications for effectiveness outcomes research. Nurs Res Pract. 2012;2012:847626. https://doi.org/10.1155/2012/847626
Kim J, An K, Kim MK, Yoon SH. Nurses’ perception of error reporting and patient safety culture in Korea. West J Nurs Res. 2007;29(7):827–44.
Zakari N. Attitude of Academic Ambulatory Nurses toward Patient Safety Culture in Saudi Arabia. undefined [Internet]. 2011 [cited 2022 Feb 20]; https://www.semanticscholar.org/paper/Attitude-of-Academic-Ambulatory-Nurses-toward-in-Zakari/fd932a8b140f31f8742d99a4b9dc125fec837962. Accessed 20 Feb 2022.
Park SA, Lee SJ, Choi GU. Survey of factors associated with nurses’ perception of patient safety. Asian Pac J Cancer Prev. 2011;12(8):2129–32.
Ausserhofer D, Schubert M, Engberg S, Blegen M, De G, Schwendimann R. Nurse-reported patient safety climate in Swiss hospitals: a descriptive-explorative substudy of the Swiss RN4CAST study. Swiss Med Wkly. 2012;142: w13501.
Ballangrud R, Hedelin B, Hall-Lord ML. Nurses’ perceptions of patient safety climate in intensive care units: a cross-sectional study. Intensive Crit Care Nurs. 2012;28(6):344–54.
Tocco Tussardi I, Benoni R, Moretti F, Tardivo S, Poli A, Wu AW, et al. Patient safety in the eyes of aspiring healthcare professionals: a systematic review of their attitudes. Int J Environ Res Public Health. 2021;18(14):7524.
Joanna Briggs Institute. Critical Appraisal Tools [Internet]. [cited 2022 Mar 2]. https://jbi.global/critical-appraisal-tools. Accessed 02 Mar 2022.
Kyriacou Georgiou M, Merkouris A, Hadjibalassi M, Sarafis P, Kyprianou T. Correlation Between Teamwork and Patient Safety in a Tertiary Hospital in Cyprus. Cureus [Internet]. 2021 [cited 2022 Mar 1];13(11):e19244. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8642670/. Accessed 01 Mar 2022.
Lægreid P, Opedal S, Stigen IM. The Norwegian Hospital reform: balancing political control and enterprise autonomy. J Health Polit Policy Law. 2005;30:1027–64.
McFadden KL, Stock GN, Gowen CR. Implementation of patient safety initiatives in US hospitals. Int J Oper Prod Manag [Internet]. 2006;26(3):326–47. https://doi.org/10.1108/01443570610651052.
Huang DT, Clermont G, Sexton JB, Karlo CA, Miller RG, Weissfeld LA, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med. 2007;35(1):165–76.
Valentin A, Capuzzo M, Guidet B, Moreno R, Metnitz B, Bauer P, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ [Internet]. 2009;338(mar12 1):b814–b814. https://doi.org/10.1136/bmj.b814.
Ginsburg L, Norton PG, Casebeer A, Lewis S. An educational intervention to enhance nurse leaders’ perceptions of patient safety culture. Health Serv Res [Internet]. 2005 Aug [cited 2022 Mar 1];40(4):997–1020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361187/. Accessed 01 Mar 2022.
Al Mutairi A, Schwebius D, Al MA. Hospital-acquired pressure ulcer incident rates among hospitals that implement an education program for staff, patients, and family caregivers inclusive of an after discharge follow-up program in Saudi Arabia. Int Wound J [Internet]. 2020;17(5):1135–41. https://doi.org/10.1111/iwj.13459.
Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf. 2013;22(1):11–8.
Al Mutair A, Al Mutairi A, Schwebius D. The retention effect of staff education program: sustaining a decrease in hospital-acquired pressure ulcers via culture of care integration. Int Wound J. 2021;18(6):843–9.
AlJohani A, Karuppiah K, Al Mutairi A, Al Mutair A. Narrative Review of Infection Control Knowledge and Attitude among Healthcare Workers. J Epidemiol Glob Health [Internet]. 2021 Mar [cited 2022 Feb 22];11(1):20–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7958281/. Accessed 22 Feb 2022.
Cullen DJ, Bates DW, Small SD, Cooper JB, Nemeskal AR, Leape LL. The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv. 1995;21(10):541–8.
Mutair AA, Alhumaid S, Shamsan A, Zaidi ARZ, Mohaini MA, Al Mutairi A, et al. The effective strategies to avoid medication errors and improving reporting systems. Medicines [Internet]. 2021 Sep [cited 2022 Feb 22];8(9):46. https://www.mdpi.com/2305-6320/8/9/46. Accessed 22 Feb 2022.
Acknowledgements
The research team and the authors extend sincere thanks and appreciation to all respondents for their patience in cooperation.
Funding
None.
Author information
Authors and Affiliations
Contributions
SA, MA, AA: methodology; CS; validation and formal analysis; SA, MA, AA, CS: data curation; SA, ABA, MA, CS, HA, AAL, AA: original draft preparation, writing, review and editing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the institutional review board.
Consent for publication
All authors have read and approved the manuscript for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Almutairi, S., Aljohani, A., Awad, M. et al. Perceptions of Patient Safety Culture Dimensions among Hospital Nurses: A Systematic Review. Dr. Sulaiman Al Habib Med J 4, 103–125 (2022). https://doi.org/10.1007/s44229-022-00012-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44229-022-00012-z