Abstract
Objectives
This study determined the prevalence and trends in caesarean section (C-section) deliveries and the factors associated with the utilization of C-section deliveries among Indonesian mothers from 2007 to 2017.
Methods
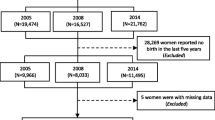
We used Indonesia Demographic and Health Survey data sets (2007, 2012, and 2017) to assess the prevalence, trends, and factors associated with C-section delivery through univariate, bivariate, and multivariate analyses.
Results
A 10% increase in C-section delivery among Indonesian women was observed between the years 2007 and 2017. Mothers from urban areas tended to receive more C-sections than mothers from rural areas (adjusted odds ratio (aOR) = 1.49). More educated mothers were more likely (aOR = 3.373) to receive C-sections than mothers without formal education. Mothers from wealthy family backgrounds were more (aOR = 1.97) likely to receive C-sections than mothers from low-income families. Antenatal care (ANC) visits were significantly positively associated with receiving C-sections; mothers with more than four ANC visits (aOR = 4.54) tended to receive more C-sections than mothers with no ANC visits. For first births, mothers over 25 years of age were more likely (aOR = 2.07) to receive C-sections than mothers less than 18 years of age.
Conclusion
The percentage of C-sections has alarmingly increased. Thus, authorities in Indonesia should consider these findings and take necessary steps to decrease C-sections. The results of this study should help policymakers formulate appropriate policies that will encourage regular delivery where most appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Caesarean section (C-section) has been a major public health concern worldwide in the recent past, because of its overuse and associated complications during and after surgery [1]. C-section was introduced as a clinical practice to save both mothers’ and babies’ lives when critical medical complications arise during pregnancy [2, 3]. However, in the past 2 decades, the rate of childbirth through C-section has increased worldwide [3], to 40.5% in Latin America and the Caribbean, 32.3% in North America, 31.1% in Oceania, 25% in Europe, 19.1% in Asia and 7.3% in Africa [4, 5]. Bangladesh (58.54%), Greece (58%), Cyprus (54.8%), Turkey (51.9%), Brazil (50%), Romania (44.1%), Bulgaria (43.1%), Poland (39.3%), Hungary 37.3%), the USA (32%), and China (27%) are the countries with the highest C-section delivery rates [6,7,8,9]. The World Health Organization has indicated that higher rates of C-sections do not decrease maternal and neonatal deaths, and recommends a C-section rate of 10–15%. However, the rate in Indonesia (18.6%) has exceeded this range [10]. The ever-increasing use of nonemergency C-section is associated with increasing maternal and child mortality and morbidity [11], thus ultimately impeding health sector development in many countries. Indonesia is also facing this global crisis: C-section delivery alternatives to vaginal delivery increased from 12% in 2012 to 17% in 2017, and Jakarta had the highest rate (31.1%) [12]. Inappropriate and unnecessary C-sections pose both immediate and long-lasting mortality and morbidity threats to mothers and babies, thus increasing maternal, neonatal, and child mortality [13]. The immediate negative effects of unnecessary C-sections include miscarriage and stillbirth, placenta previa, post-partum infection, haemorrhage, maternal death, and thromboembolism [14,15,16].
The long-lasting effects of C-section include bleeding, uterine rupture, pelvic organs, fecal incontinence, anaesthetic-associated complications, and increased obstetric risks in subsequent pregnancies [17, 18]. Babies delivered through C-section are more likely to have disorders including asthma, type 1 diabetes, allergies, and obesity, and to have lower general cognitive function and academic achievement [19, 20]. Furthermore, families with low economic status may face financial hardship in paying unnecessary C-section fees and other expenses arising from complications and extended hospital stays [21]. Because of potential maternal and perinatal risks, inequality of access, and costs, this increase in C-sections is becoming a major problem in Indonesia [2, 22]. The crude maternal morbidity in Indonesia between 2002 to 2012 was 38.3% and 53.7%, respectively, whereas the crude pregnancy morbidity in the same period was 7.2% and 13.2%, respectively [23]. Earlier studies [3, 9, 16, 24, 25] have reported various social and economic factors responsible for unnecessary use of C-sections instead of normal vaginal delivery; however, very few studies have addressed the socio-demographic correlations. Settling the debate on the utility of unnecessary C-sections without medical indications requires further research on relevant socio-demographic factors other than socio-cultural and medical conditions. Therefore, the current study attempted to determine the socio-demographic characteristics associated with C-section delivery and related trends in Indonesia by using Indonesia Demographic and Health Survey (IDHS) data from 2007 to 2017.
2 Methods
2.1 Data Source
Pooled data from the IDHS 2007, 2012, and 2017 datasets were used in this study (National Population and Family Planning Board 2018). The IDHS surveys conducted in 2007, 2012, and 2017 were implemented by Badan Pusat Statistik Indonesia in collaboration with the National Population and Family Planning Board and the Ministry of Health. Administratively, Indonesia is divided into 33 (in 2007 and 2012) and 34 (in 2017) provinces. In IDHS, the respondents were all women 15–49 years of age, currently married men 15–54 years of age, and never-married men 15–24 years of age. The 2007, 2012, and 2017 IDHS samples were selected with a stratified two-stage design consisting of 1694, 1840, and 1970 census blocks, the primary units for sampling. The 2017 IDHS sample was selected through two-stage stratified sampling, in which ICF provided technical assistance through the DHS Program, funded by the United States Agency for International Development, which offers technical services for the population and health surveys in many countries worldwide.
2.2 Variables
This study considered C-section delivery as the dependent variable, categorized as yes and no. On the basis of previous literature, we selected a set of socio-economic and demographic factors for determining the utilization of C-section delivery. Before choosing the variables, we conducted a test of association to verify whether they were significantly associated with the dependent variable. Later, we considered only the associated variables in multivariate analysis. The type of residence remained the same as those in the original datasets. For analysis, we categorized the variable antenatal care (ANC) visits as no visit, one to four visits, or more than four visits. The highest education level remained the same as that in the data set, and the categories were as follows: no education, primary education, secondary education, and higher education. For the variable wealth index, poorest and poorer wealth comprised the poor category; moderate wealth comprised the middle category; and the highest wealth comprised the wealthy category. Birth order was categorized as either first order, for one birth only, or as “other” for the rest of the birth orders. Respondents’ current working status category remained the same as that in the data set and was categorized into yes or no. The smallest children comprised the small category, average sized children comprised the average category, and the other children constituted the large categories. The variable of age at first birth was categorized into three levels: less than or equal to 17 years, 18–25 years, and greater than 25 years.
2.3 Statistical Analysis
2.3.1 Binary Logistic Regression
Generally, bivariate analysis (Pearson's χ2) is performed to explore associations between dependent and independent variables. In addition, to determine the significant factors influencing the utilization of C-sections in Indonesia, a logistic regression model was used. Logistic regression is sometimes called a logistic model or logit model. A binary logistic model is suitable for the primary variable of interest in values of two categories [26]. It analyses the associations among multiple independent variables and binary dependent variables, and estimates the probability of an event of interest. The dependent variable was categorized into two categories in this study. With binary logistic regression, highly different factors can be demonstrated to influence outcomes. Logistic regression generates coefficients, odds ratios and 95% CIs to predict a logit transformation of the probability of the presence of the characteristic of interest:
where p is the probability of the presence of the characteristic of interest, and the logit transformation is defined as the log odds:
and
Parameters are usually chosen to minimize the sum of squared errors (as in ordinary regression). Nonetheless, parameters are selected in logistic regression to maximize the likelihood of observing the sample values.
3 Results
Table 1 represents the proportions of sample characteristics among mothers 15–49 years of age with at least one birth throughout each survey year. As shown in the frequency table, use of C-section delivery increased from 6.5 to 16.4% between 2007 and 2017. Moreover, Table 1 illustrates the frequencies of different independent variables and their percentages.
Table 2 demonstrates that the respondents’ place of residence was a significant factor, and urban women were 1.588 (1.355–1.560), 1.472 (1.310–1.653), and 1.354 (1.225–1.498) times more likely than rural women to receive a C-section in 2007, 2012 and 2017, respectively. Crude OR values indicated the same positive relationship between urban women and C-sections. Educated women tended to receive C-sections more frequently than non-educated women. The crude OR indicated that women with jobs were more interested in receiving C-sections than women without jobs. Respondents from affluent families were more likely to receive C-sections than those in low-income families. Women with a wealthy family background were 2.216 (1.810–2.713), 2.084 (1.812–2.397), and 2.236 (1.981–2.523) times more likely to receive C-section delivery in 2007, 2012, and 2017, respectively, than women from poor families. Respondents of all ages using more ANC were more willing to receive C-sections in Indonesia. Women having a first child had a higher probability of receiving a C-section than women having second or other order children. Women with a child of abnormal size (small or large) were more likely to receive C-sections than women with normal size children. Women who had their children at the ages of 18–25 were less likely to receive C-sections than women below 18 years of age. However, women older than 25 years of age were 1.908 (1.637–2.223), 2.345 (2.088–2.634), and 1.930 (1.743–2.137) times more likely to receive C-sections than women younger than 18 years of age.
Table 3 shows the frequency of various selected variables from a merged version of three IDHS data sets from 2007 to 2017. A total of 11.5% of women used C-section delivery over the 10 years. Interestingly, 68.3% of women had their first child before 18 years of age, 75% of women received ANC more than four times, and 51% of the children were normal-sized.
Table 4 indicates that all independent variables were significant in the combined data set. In the combined data set, women from urban areas were 1.491 (1.392–1.596) times more likely to receive C-sections than those from rural areas. Educated women were more likely to receive C-section delivery than uneducated women. Women with higher education levels were 3.373 (2.31–4.92) times more likely to receive C-section delivery than women with no education. Women from wealthier families were 1.970 (1.814–2.139) times more likely to receive C-sections than women from low-income families. The combined data set revealed that the respondents receiving more than four ANC visits were 4.537 (3.06–6.73) times more likely to receive C-section delivery than respondents with no ANC visits. Respondents having a first child were more likely to receive C-sections than those having a second child or other order child. Women with normal-sized children were less likely to receive C-sections. Women older than 25 years of age were at significant risk of receiving C-sections than women younger than 18 years of age.
4 Discussion
The study estimated trends and inequalities in C-section utilization among Indonesian mothers, on the basis of data sampled in 2007, 2012, and 2017. C-section delivery is recommended or performed only when complications exist for the mother or child, and when vaginal delivery is impossible. When complications arise, lifesaving procedures should be accessible to all women worldwide. However, substantial inequalities in C-section utilization exist among different groups of people. This study aimed to identify the critical determinants for decreasing disparities among Indonesia's women. The results showed that place of residence, wealth index, education, and ANC visits influenced this inequality. Between 2007 and 2017, an approximately 10% increase was observed in C-sections utilization in Indonesia. Studies have indicated that the increase from 2004 to 2014 in Bangladesh was 20%, and that in Egypt was 50% [27]. Different studies have widely demonstrated this increasing trend in developing countries [28,29,30]. The results of this study indicated that women with high education levels and women from wealthy family backgrounds were more likely to use C-sections, in agreement with the findings of other studies [31,32,33,34,35,36]. Several studies using recent data have shown that women with high education levels and wealthy family backgrounds might prefer C-section delivery to vaginal delivery because they believe it to be safer [37, 38]. In Indonesia, a lack of expert health staff and health infrastructure, including low socio-economic status and insufficient obstetric care, can increase C-section utilization.[39]. Education may affect C-section utilization because it is interlinked with decision-making power [40, 41]. Sometimes, excessive concern regarding vaginal appearance results in a preference for C-section delivery over normal delivery [37, 42]. An analysis in Indonesia (2013) has indicated that the complications of labour, parity, and health status of the mother and fetus are the variables associated with greater utilization of C-section delivery [43]. Respondents from urban areas were more likely to receive C-section delivery than those from rural areas, thus supporting findings from other studies [44]. Increases in access to internet facilities, maternal age, and access to private insurance have increased the probability of planned C-sections among Indonesian women [45]. The current study revealed that ANC utilization is a crucial factor influencing respondents’ receiving C-section delivery. The reason for this finding may be that mainly women with high socio-demographic status received check-ups, and these women were the primary users of C-section delivery. Another explanation might be physicians’ profit motivations to perform C-sections [46, 47]. This study indicated that women with a first birth at the age of 25 were more likely to receive C-section delivery, because complications during pregnancy and delivery are more likely to occur in older mothers than young mothers [48,49,50]. Sometimes, primigravida mothers are more inclined to have C-section delivery even in the absence of complications [51].
5 Strengths and Limitations
The study used nationally representative data on the utilization of C-sections during delivery. Therefore, the researchers had no scope to be biased during analysis, because the data had been collected with recognized and validated research tools and were quantitative. This study may increase awareness regarding the alarming increasing frequency of C-sections in Indonesia, and highlight its relationship with many factors. However, the study did not address geographic variations during analysis, because country average socio-demographic information was used to analyse the C-sections. Furthermore, this study was based on only quantitative data; therefore, the qualitative context, representing more vivid scenarios, was absent. Because of the unavailability of health-associated variables and the missing information in the DHS data set, many crucial factors could not be studied. Categorizing the severity level of the patients and the importance of C-sections was also not possible because of this limitation.
6 Conclusion
Our results demonstrated that the proportion of women receiving C-sections from 2007 to 2017 in Indonesia increased an alarming level. Simultaneously, inequitable access to facilities performing C-sections exists. This study suggests that place of residence, wealth index, education, and ANC visits play crucial roles in these inequalities. Proper steps must be taken to ensure that the lifesaving procedure of C-section is used when necessary, regardless of patients’ residence, socio-economic status, and education level. Service providers must focus on respondents from rural areas with no education and low-income family backgrounds. Moreover, patients must be more conscious of the utilization of C-section delivery as well as the adverse consequences of unnecessary use.
Data availability
Data can be found from https://dhsprogram.com/. The numerical data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- C-section:
-
C-section
- IDHS:
-
Indonesian Demographic and Health Survey
- DHS:
-
Demographic and Health Survey
- aOR:
-
Adjusted odds ratio
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- Ref.:
-
Reference group
- ANC:
-
Antenatal care
References
Vora KS, Cottagiri SA, Saiyed S, Tailor PJPH. Public Health aspects of Cesarean section including overuse and underuse of the procedure. Int Res J Public Health. 2019;3:30.
Betrán AP, Torloni MR, Zhang JJ, Gülmezoglu A, Aleem HA, Althabe F, Bergholt T, De Bernis L, Carroli G, Deneux‐Tharaux C, Devlieger R, et al. WHO statement on caesarean section rates. Bjog. 2016;123(5):667.
Zahroh RI, Disney G, Betrán AP, Bohren MAJBGH. Trends and sociodemographic inequalities in the use of caesarean section in Indonesia, 1987–2017. BMJ Glob Health. 2020;5(12):844.
Rai SD, Poobalan A, Jan R, Bogren M, Wood J, Dangal G, et al. Caesarean section rates in south asian cities: can midwifery help stem the rise? J Asian Midwives (JAM). 2019;6(2):4–22.
Hoxha I, Braha M, Syrogiannouli L, Goodman DC, Jüni P. Caesarean section in uninsured women in the USA: systematic review and meta-analysis. BMJ Open. 2019;9(3): e025356.
Antoniou E, Orovou E, Iliadou M. Cesarean sections in Greece. How can we stop the vicious cycle? World J Adv Res Rev. 2021;12(1):375–7.
Pratilas GC, Sotiriadis A, Dinas K. Is high use of caesarean section sometimes justified? The Lancet. 2019;394(10192):25–6.
Santas G, Santas F. Trends of caesarean section rates in Turkey. J Obstet Gynaecol. 2018;38(5):658–62.
Verma V, Vishwakarma RK, Nath DC, Khan HT, Prakash R, Abid O. Prevalence and determinants of caesarean section in South and South-East Asian women. PLoS ONE. 2020;15(3): e0229906.
World Health Organization. World health statistics 2015. World Health Organization; 2015.
Villar J, Carroli G, Zavaleta N, Donner A, Wojdyla D, Faundes A, et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ. 2007;335(7628):1025.
Irwinda R, Hiksas R, Lokeswara AW, Wibowo N. Maternal and fetal characteristics to predict c-section delivery: a scoring system for pregnant women. Womens Health. 2021;17:17455065211061968.
Basrowi RW, Sundjaya T, Sitorus NL, Masita BMJWNJ. Perspective of Caesarean section delivery and its health risks on children among Indonesian pediatricians. World Nutr J. 2020;4(1–2):55–61.
Ye J, Betrán AP, Guerrero Vela M, Souza JP, Zhang JJB. Searching for the optimal rate of medically necessary cesarean delivery. Birth. 2014;41(3):237–44.
Sungkar A, Basrowi RW. Rising trends and indication of caesarean section in Indonesia. World Nutr J. 2020;4(1–2):1–7.
Hodgkin K, Joshy G, Browne J, Bartini I, Hull TH, Lokuge K. Outcomes by birth setting and caregiver for low risk women in Indonesia: a systematic literature review. Reprod Health. 2019;16(1):1–12.
Sandall J, Tribe RM, Avery L, Mola G, Visser GH, Homer CS, et al. Short-term and long-term effects of caesarean section on the health of women and children. The Lancet. 2018;392(10155):1349–57.
Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol. 2012;207(1):14–29.
Polidano C, Zhu A, Bornstein JC. The relation between cesarean birth and child cognitive development. Sci Rep. 2017;7(1):1–10.
Shi X-Y, Wang J, Zhang W-N, Zhao M, Ju J, Li X-Y, et al. Cesarean section due to social factors affects children's psychology and behavior: a retrospective cohort study. Front Pediatrics. 2021;8:989.
Cresswell JA, Assarag B, Meski FZ, Filippi V, Ronsmans CJTM, Health I. Trends in health facility deliveries and caesarean sections by wealth quintile in Morocco between 1987 and 2012. Trop Med Int Health. 2015;20(5):607–16.
Abebe FE, Gebeyehu AW, Kidane AN, Eyassu GAJRh. Factors leading to cesarean section delivery at Felegehiwot referral hospital, Northwest Ethiopia: a retrospective record review. Reprod Health. 2015;13(1):1–7.
Widyaningsih V, Khotijah B. Expanding the scope beyond mortality: burden and missed opportunities in maternal morbidity in Indonesia. Glob Health Action. 2017;10(1):1339534.
Pristya TY, Mas’udah AFJKLS. section cesarean in urban areas Indonesia: how the relation with frequencies of antenatal care? 2018:377–82-–82.
Lazasniti S, Machmud PB, Ronoatmodjo SJJBE. Factors that influence cesarean section deliveries in Indonesia. J Berk Epidemiol. 2020;8(2):100–8.
Tranmer M, Elliot M. Binary logistic regression. In: Cathie Marsh for census and survey research, paper. 2008;20.
Khan MN, Islam MM, Rahman M. Inequality in utilization of cesarean delivery in Bangladesh: a decomposition analysis using nationally representative data. Public Health. 2018;157:111–20.
Gebremedhin S. Trend and socio-demographic differentials of Caesarean section rate in Addis Ababa, Ethiopia: analysis based on Ethiopia demographic and health surveys data. Reprod Health. 2014;11(1):1–6.
Sharma G. The changing paradigm of labour and childbirth in Indian cities: an enquiry into increasing rates of caesarean deliveries. Int J Epidemiol. 2016;45(5):1390–3.
Khan MN, Islam MM, Shariff AA, Alam MM, Rahman MM. Socio-demographic predictors and average annual rates of caesarean section in Bangladesh between 2004 and 2014. PLoS ONE. 2017;12(5): e0177579.
Taffel S. Cesarean delivery in the United States, 1990, vol. 51. US Government Printing Office; 1994.
Skalkidis Y, Petridou E, Papathoma E, Revinthi K, Tong D, Trichopoulos D. Are operative delivery procedures in Greece socially conditioned? Int J Qual Health Care. 1996;8(2):159–65.
Tatar M, Günalp S, Somunoğlu S, Demirol A. Women’s perceptions of caesarean section: reflections from a Turkish teaching hospital. Soc Sci Med. 2000;50(9):1227–33.
Huang K, Tao F, Faragher B, Raven J, Tolhurst R, Tang S, et al. A mixed-method study of factors associated with differences in caesarean section rates at community level: the case of rural China. Midwifery. 2013;29(8):911–20.
Janoudi G, Kelly S, Yasseen A, Hamam H, Moretti F, Walker M. Factors associated with increased rates of caesarean section in women of advanced maternal age. J Obstet Gynaecol Can. 2015;37(6):517–26.
Zgheib SM, Kacim M, Kostev K. Prevalence of and risk factors associated with cesarean section in Lebanon—a retrospective study based on a sample of 29,270 women. Women and Birth. 2017;30(6):e265–71.
Feng XL, Xu L, Guo Y, Ronsmans C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ. 2012;90:30–9.
Bhutta ZA, Memon ZA, Soofi S, Salat MS, Cousens S, Martines J. Implementing community-based perinatal care: results from a pilot study in rural Pakistan. Bull World Health Organ. 2008;86:452–9.
Suparmi S, Kusumawardhani N, Susiloretni KA. Sub-national inequality of caesarean section in urban-rural area of Indonesia. In: Proceedings of the international conference on public health, vol. 4, no. 1, 2018. p. 23–32.
Hopkins K. Are Brazilian women really choosing to deliver by cesarean? Soc Sci Med. 2000;51(5):725–40.
Faisal-Cury A, Menezes PR, Quayle J, Santiago K, Matijasevich A. The relationship between indicators of socioeconomic status and cesarean section in public hospitals. Rev Saude Publ. 2017;51:14.
Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86(4):451–6.
Sihombing NM, Saptarini I, Putri DSK. Determinan persalinan sectio caesarea di Indonesia (analisis lanjut data Riskesdas 2013). Indones J Reprod Health. 2017;8(1):63–73.
Stanton CK, Holtz SA. Levels and trends in cesarean birth in the developing world. Stud Fam Plann. 2006;37(1):41–8.
Prasetyoputra P, Sitohang MY, Rahadian AS, Hafsari TA. Too posh to push: determinants of planned c-section delivery among Indonesian Women. In: 4th International Symposium on Health Research (ISHR 2019). Atlantis Press; 2020. p. 604–10.
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5(6): e11190.
Amin R, Shah NM, Becker S. Socio-economic factors differentiating maternal and child health-seeking behaviour in rural Bangladesh: A cross-sectional analysis. International Journal for Equity in Health. 2010;9(9):1.
Padmadas SS, Nair SB, Anitha Kumari KR. Caesarean section delivery in Kerala, India: evidence from a national family health survey. Soc Sci Med. 2000;51(4):511–21.
Bell J, Campbell D, Graham W. Can obstetric complications explain the high levels of caesarean section among older women. BMJ. 2001;322:894–5.
Al Rifai RH. Trend of caesarean deliveries in Egypt and its associated factors: evidence from national surveys, 2005–2014. BMC Pregnancy Childbirth. 2017;17(1):1–14.
Peipert JF, Bracken MB. Maternal age: an independent risk factor for cesarean delivery. Obstet Gynecol. 1993;81(2):200–5.
Acknowledgements
The authors are grateful to the DHS program for providing access to the data set used to complete this study.
Funding
The authors did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
MAI devised the concept and study design, and performed analysis, manuscript writing, primary editing, and supervision of the work. HHS was responsible for data editing, analysis, interpretation, and manuscript writing. AJ and MHH were responsible for manuscript writing and revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Islam, M.A., Shanto, H.H., Jabbar, A. et al. Caesarean Section in Indonesia: Analysis of Trends and Socio-Demographic Correlates in Three Demographic and Health Surveys (2007–2017). Dr. Sulaiman Al Habib Med J 4, 136–144 (2022). https://doi.org/10.1007/s44229-022-00011-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44229-022-00011-0