Abstract
Introduction
As part of the COVID-19 pandemic response, the Ontario Ministry of Health funded a virtual care pilot program intended to support emergency department (ED) diversion of patients with low acuity complaints and reduce the need for face-to-face contact. The objective was to describe the demographic characteristics, outcomes and experience of patients using the provincial pilot program.
Methods
This was a prospective cohort study of patients using virtual care services provided by 14 ED-led pilot sites from December 2020 to September 2021. Patients who completed a virtual visit were invited by email to complete a standardized, 25-item online survey, which included questions related to satisfaction and patient-reported outcome measures.
Results
There were 22,278 virtual visits. When patients were asked why they contacted virtual urgent care, of the 82.7% patients who had a primary care provider, 31.0% said they could not make a timely appointment with their family physician. Rash, fever, abdominal pain, and COVID-19 vaccine queries represented 30% of the presenting complaints. Of 19,613 patients with a known disposition, 12,910 (65.8%) were discharged home and 3,179 (16.2%) were referred to the ED. Of the 2,177 survey responses, 94% rated their overall experience as 8/10 or greater. More than 80% said they had answers to all the questions they had related to their health concern, believed they were able to manage the issue, had a plan they could follow, and knew what to do if the issue got worse or came back.
Conclusions
Many presenting complaints were low acuity, and most patients had a primary care provider, but timely access was not available. Future work should focus on health equity to ensure virtual care is accessible to underserved populations. We question if virtual urgent care can be safely and more economically provided by non-emergency physicians.
Résumé
Introduction
Dans le cadre de la réponse à la pandémie de COVID-19, le ministère de la Santé de l'Ontario a financé un programme pilote de soins virtuels visant à soutenir la réorientation vers les services d'urgence des patients présentant des problèmes de faible acuité et à réduire le besoin de contact en personne. L'objectif était de décrire les caractéristiques démographiques, les résultats et l'expérience des patients utilisant le programme pilote provincial.
Méthodes
Il s'agissait d'une étude de cohorte prospective de patients utilisant des services de soins virtuels fournis par 14 sites pilotes dirigés par des services d'urgence, de décembre 2020 à septembre 2021. Les patients qui ont effectué une visite virtuelle ont été invités par courriel à répondre à une enquête en ligne standardisée de 25 questions, qui comprenait des questions relatives à la satisfaction et aux résultats rapportés par les patients.
Résultats
Il y a eu 22 278 visites virtuelles. Lorsqu'on a demandé aux patients pourquoi ils avaient contacté les soins urgents virtuels, sur les 82,7 % de patients qui avaient un prestataire de soins primaires, 31,0 % ont répondu qu'ils n'avaient pas pu obtenir un rendez-vous en temps voulu avec leur médecin de famille. Les éruptions cutanées, la fièvre, les douleurs abdominales et les interrogations sur le vaccin COVID-19 représentaient 30 % des plaintes présentées. Sur les 19 613 patients dont la disposition était connue, 12 910 (65,8 %) ont été renvoyés chez eux et 3 179 (16,2 %) ont été orientés vers les urgences. Sur les 2 177 réponses à l'enquête, 94 % ont attribué une note de 8/10 ou plus à leur expérience globale. Plus de 80 % d'entre eux ont déclaré avoir obtenu des réponses à toutes les questions qu'ils se posaient sur leur problème de santé, se croire capables de le gérer, avoir un plan qu'ils pouvaient suivre et savoir quoi faire si le problème s'aggravait ou revenait.
Conclusions
De nombreuses plaintes présentées étaient de faible acuité, et la plupart des patients avaient un fournisseur de soins primaires, mais l'accès en temps opportun n'était pas disponible. Les travaux futurs devraient se concentrer sur l'équité en matière de santé pour s'assurer que les soins virtuels sont accessibles aux populations mal desservies et nous nous demandons si ces services peuvent être fournis en toute sécurité et de manière plus économique par des médecins non urgentistes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known about the topic? |
Virtual visits enable healthcare providers and patients to connect remotely and avoid risk of COVID-19 exposure. |
What did this study ask? |
Why do patients choose virtual urgent care and what are the demographic characteristics, outcomes and experience of patients using these services? |
What did this study find? |
Many presenting complaints were low acuity, and most patients had a primary care provider, but timely access was not available. |
Why does this study matter to clinicians? |
We question if virtual care is a service emergency physicians and nurses should be providing in the context of severe ED workforce shortages. |
Introduction
The COVID-19 pandemic has significantly impacted the way most Canadians live and work, including their interactions with the healthcare system [1, 2]. Early public health measures aimed at preventing and reducing the spread of COVID-19 included the implementation of stay-at-home orders, closures of public venues, and restrictions on social gatherings and travel. Physical distancing regulations made in person, non-urgent, healthcare visits nearly impossible, with in-person primary care declining by nearly 80%, and emergency department (ED) visits decreasing by 50% in the early stages of the pandemic [3,4,5]. To continue to meet the healthcare needs of their patients and prevent the transmission of COVID-19, many clinicians made an early transition to virtual care [6].
Direct-to-patient video and telephone visits enable healthcare providers and patients to connect safely at a distance and avoid potential risk of COVID-19 exposure. While technologies to deliver healthcare through means other than face-to-face contact have been available for decades, there has been incredible growth and rapid adoption of virtual care since the beginning of the COVID-19 pandemic [7, 8]. According to Canada Health Infoway, virtual care use in Canada rose from 15% of all healthcare visits in 2019 to 55% in April 2020 [4].
As part of the COVID-19 pandemic response, in the Fall of 2020 the Ministry of Health approved up to four million dollars to fund a pilot program involving 14 virtual urgent care initiatives across the province of Ontario [9]. This funding was intended to support ED diversion of patients with low acuity complaints and reduce the need for face-to-face contact whenever possible. The objective of this study was to describe the presenting complaints, demographic characteristics and outcomes of patients using virtual services in the provincial pilot program, determine why patients and their families chose virtual urgent care, and describe their experience using these services.
Methods
This was a prospective, multicentered, cohort study of all patients using virtual urgent care provided by 14 ED-led pilot sites in Ontario, Canada from December 2020 to September 2021. The design and implementation of the 14 different ED-led virtual sites has been described elsewhere, but sites had various start dates, operating hours, screening, and staffing models (Appendix 1). Each site posted a list of presenting complaints which would be suitable for virtual urgent care, and those that would not be appropriate for virtual care and should be assessed in person. Most sites allowed patients to self-screen using these lists. Six sites had a triage nurse or nurse practitioner review the presenting complaint and if it was believed the patient required an in-person assessment, they were re-directed to the closest ED. All virtual urgent care patients were assessed by a physician.
Funding allocation, site selection and approval were overseen by an Ontario Health Virtual Care Secretariat, which set program funding criteria and evaluated proposals endorsed by the Ontario Health Regions. The funding agreement ensured the investigators maintained control over the study design, methods and interpretation of the results. The 14 sites approved for virtual urgent care pilot funding represented a mix of pediatric, northern, urban, academic and community sites across the province. As part of the funding agreement, each participating site was required to collect and report a minimum of six months of standardized patient level encounter data which were sent electronically via secure file transfer to Ontario Health. Standardized patient level encounter data included the patient’s health card number, date and time of virtual visit, age, sex, housing status, primary care physician, reason for choosing virtual urgent care, presenting complaint, acuity level, discharge diagnosis and disposition.
Patients who had a virtual urgent care visit and provided their email address were invited by the local site by email to complete a standardized, 25-item online questionnaire. The survey included a series of questions related to satisfaction, experience and patient-reported outcome measures that focused on the outcomes of patient care as perceived by the patients themselves [10, 11]. The survey was developed by researchers based on a review of relevant literature as well as consultation with virtual urgent care providers, qualitative methodologists and a clinical epidemiologist. Prior to distribution, the questionnaire was peer reviewed by five people unrelated to the study and tested for face and construct validity, as well as comprehension. The survey consisted of a variety of multiple choice, Likert, and open-ended questions regarding how the patient heard of the virtual urgent care service, why they chose virtual urgent care, availability of a primary care provider, and their perceived experience and satisfaction with the virtual visit (Appendix 2). Surveys were distributed locally by each of the 14 pilot sites using a standardized link to the questionnaire housed in secure web-based survey software (Qualtrics, Provo, UT). The surveys were completed anonymously and could not be linked back to a specific patient encounter. Descriptive statistics were summarized using means with standard deviations, medians with interquartile range (IQR) or frequencies, where appropriate. All statistical analyses were conducted using SPSS (IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corporation). The study protocol was approved by the Research Ethics Board at each institution, with the main approval from Mount Sinai Hospital in Toronto, Ontario.
Results
Patient level encounter results
From December 2020 to September 2021, there were 22,278 visits across 14 ED-led virtual urgent care sites. Just over 73% of the virtual visits occurred between 12 and 8 pm, with nearly 90% occurring Monday to Friday, which corresponded to the periods the service was available. Median (IQR) wait time from initial patient contact to first contact with a virtual care provider was 171 (67, 276) minutes. The median (IQR) length of the virtual visit was 14 (IQR 11–18) minutes. Just over 85% of the virtual visits were completed using video services. Demographic characteristics and disposition of patients using virtual urgent care services can be viewed in Table 1.
Nearly 80% of patients using virtual urgent care screened themselves using a symptom checklist. A triage nurse screened patients at three pilot sites and reported acuity scores. Of the 4,989 (22%) virtual visits which reported a triage nurse estimated illness severity score using the Canadian Triage and Acuity Scale (CTAS) as a proxy, 2,499 (50%) had a CTAS score of 5; 1,075 (22%) were CTAS 4; 1,109 (22%) had a CTAS score of 3; and 306 (6%) of patients had a CTAS score of 2. Rash, fever, abdominal pain, COVID-19 vaccine query and other minor complaints represented about 30% of the presenting complaints. Concerns were different across the age continuum, with more infectious disease concerns (e.g., fever) in the pediatric population rather than chronic complaints for the adults. In terms of disposition, 65% of patients seen in virtual care were discharged home, 16% were referred to the ED, 6% were referred to their primary care provider, 4% were referred to a specialist, and 5% left without being seen (Table 1).
When patients were asked why they contacted virtual urgent care services, 31% who had a primary care provider said they could not make an appointment with their family physician or they were not available in a timely fashion (Table 2). For patients with no family physician, nearly 50% believed virtual urgent care was the most appropriate health service to use and another 31% said their visit was urgent.
Survey results
Of the 2,177 survey responses, 73% were female, 87% had higher than post-secondary education, 93% were English-speaking at home, 90% had a primary care provider, and 66% said it was their first virtual care visit. Of the 90% of patients who had a primary care provider, 47% said they tried to call their physician and either could not get an appointment or the wait was too long, which was similar to the proportion reported in the patient encounter data. Another 30% of respondents believed virtual urgent care was the most appropriate service, 11% did not try to contact their primary care provider, 5% were referred to virtual care by their family physician and 4% wanted to see a pediatric emergency medicine specialist. When asked if they would have gone to the ED if virtual urgent care was not available, 834/1,218 (69%) patients said they would have gone to the ED.
In terms of overall satisfaction, 94% of respondents rated their overall experience with virtual urgent care as 8/10 or greater, with an average score of 9.2 on a 10-point Likert scale. Patients reported being very satisfied with the ease of registration and scheduling a virtual care consult, with 90% rating their experience as 8/10 or greater. Patients were also satisfied with the software and logging into the virtual service, with 88% rating their experience as 8/10 or greater, and 93% were satisfied with the wait time with an average of 9.4 on a 10-point Likert scale. When patients were asked if they felt comfortable connecting with the health care provider virtually, 96% agreed, and 95% of respondents felt their privacy was respected. When patients were asked if their virtual healthcare provider spent sufficient time with them, 94% agreed, and 91% reported the virtual care visit was thorough. When asked if they would have preferred to meet the healthcare provider in person, half agreed they would want to receive healthcare in person, 35% said they preferred virtual care and 15% were unsure.
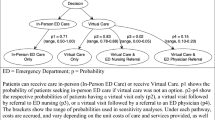
The first patient-reported outcome measure related to the domain of patient understanding. The vast majority (over 80%) of respondents agreed they had answers to all the questions they had related to their health concern, understood their health concern as much as possible, had a clear picture or understanding of their health concern, and had as much information as they currently needed (Fig. 1). For the second patient-reported outcome measure of patient reassurance, over 80% of respondents felt at ease and reassured about their health concern after their virtual visit and had few lingering concerns (Fig. 2). For the third patient-reported outcome measures related to patient’s having a plan, 80% of respondents believed they were able to manage the issue, had a plan they could follow, and knew what to do if the issue got worse or came back (Fig. 3).
Discussion
Interpretation
In this prospective, multicentered, cohort study, we found the majority of virtual urgent care visits were for low acuity presenting complaints by patients who had a primary care provider. Most complaints were managed by the virtual care provider without the need for immediate ED care, suggesting virtual care may be an alternative healthcare resource for patients with minor medical concerns who cannot access their family physician in a timely fashion, or for those trying to avoid a face-to-face healthcare visit during the COVID-19 pandemic. Patients who completed the survey after using virtual urgent care services were extremely satisfied, however, the demographics of those using virtual urgent care suggest these patients may be different from the general population seeking in-person ED care [12].
Previous studies
Recently Ho et al., described the HealthLink BC Emergency iDoctor-in-assistance (HEiDi) program, which is a free virtual healthcare service offered to residents of British Columbia seeking urgent care [13]. Call volumes, median length of the virtual visit and patient demographics were very similar to those seen in our study. Most patients (58%) were in the 20 to 64 age range, 63% were female, and 81% had a primary care physician. Of the patients seeking virtual care from HEiDi providers, 15% were referred to the ED and 7% were referred to their primary care provider.
In 2020, the Canadian Medical Association (CMA) released a poll which found almost half of all Canadians had accessed a physician via virtual care and 91% were highly satisfied with their experience [14]. These results were similar to our study, which found 94% of patients rated their overall experience with virtual care as 8/10 or greater. The same CMA poll reported 46% of Canadians would prefer a virtual method as a first point of contact with their physician moving forward, which was similar to the 35% of patients in our study who said they would prefer virtual care over an in-person visit in the future.
Strengths and limitations
Strengths of this study included standardized provincial data from individual patient encounters, a standardized provincial patient experience survey which included patient-reported outcome measures, and the inclusion of all sites participating in the pilot program, representing a good mix of pediatric, northern, urban, academic and community sites across the province. Our study had several limitations. Not all patients who had a virtual visit completed the patient experience survey. To receive the survey, sites had to obtain the patient’s email address and then patients had to agree to complete the survey. This may have resulted in patient selection and volunteer bias which may have impacted our satisfaction results. Sites did not collect the number of surveys distributed, so we have no way of estimating the survey response rate, but suspect it was very low. Additionally, we had very few patients experiencing homelessness, living in long-term care facilities and patients who did not speak English or French as their primary language. Our results may not be representative of these populations. Also, all the pilot sites were located in Ontario and were led by EDs, so these results may be less generalizable to for-profit and other provider models and provincial health systems.
Clinical implications
Rapid and convenient access to in-person healthcare has always been a challenge for non-emergent medical concerns, and this has only been exacerbated by COVID-19 pandemic [15]. However, our results suggest patients using virtual urgent care often have a primary care provider and seemed to be accessing the service more for “expedited advice” as opposed to “emergency care”, suggesting the current system of virtual urgent care in Ontario may simply be a stop-gap for when primary care is not available [16]. While it seems virtual care will be one of the enduring modernizations that survives the pandemic, it remains unclear which type of healthcare practitioner is best suited to provide this service. Considering the low acuity of presenting complaints, one might question if virtual care is a service emergency physicians and nurses should be providing in the context of severe ED workforce shortages [17,18,19,20]. Future directions in the provision of virtual care should consider if nurse practitioners, physician assistants and primary care physicians could be integrated in virtual urgent care as part of a “primary care first” strategy, with the opportunity to escalate to a virtual ED physician prior to recommending an in-person ED visit. There may also be opportunities to realize economies of scale by amalgamating individual virtual services into one provincial virtual urgent care service (or perhaps a few regional services) to enhance resource sharing and program efficiency.
The use of technology required to access virtual care raises important equity concerns. Previous studies have reported lower rates of technology adoption and increased barriers to virtual care among older patients, racial and ethnic minority groups, and those of lower socioeconomic status [21,22,23,24]. In our study, patients accessing virtual urgent care services were mostly young, well educated, English-speaking females with a primary care provider, suggesting access to virtual care may exacerbate existing health inequities among patients using virtual care compared to the general population. To lessen this disparity, future refinement and implementation of virtual services should engage with community members from vulnerable populations to determine strategies to improve access and uptake of virtual care for equity-deserving and underserved populations. Additionally, future virtual urgent care initiatives may be more beneficial in rural and remote communities where access to healthcare is more challenging.
Conclusions
This prospective, multicentered, cohort study of patients using virtual urgent care services provided by 14 ED-led sites found most patients had a primary care provider, but access to their provider was not available in a timely fashion. Many of the presenting complaints were low acuity and were managed by the virtual care provider without the need for immediate ED care. The overall impact on ED volumes was not significant. Patients were extremely satisfied, however, considering the demographics of those using virtual urgent care, future work should focus on health equity to ensure virtual care is accessible to equity-deserving and vulnerable groups. Given these findings, and the ongoing crisis in ED staffing, we question if virtual urgent care can be safely and more economically provided by non-emergency physicians.
References
Canadian Institute for Health Information. Canadian Health workforce in Canada: Highlights of the impact of COVID-19. Ottawa, ON: CIHI. 2021. https://www.cihi.ca/en/health-workforce-in-canada-highlights-of-the-impact-of-covid-19. Accessed August 4, 2022.
Canada Health Infoway. Canadian Digital Health Survey 2021: What Canadians Think. 2021. https://www.infoway-inforoute.ca/en/component/edocman/4011-canadian-digital-health-survey-2021-what-canadians-think/view-document?Itemid=0. Accessed August 4, 2022.
Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario. Canada CMAJ. 2021;193(6):E200–10.
Canada Health Infoway. Canadians’ Health Care Experiences During COVID-19: Uptake of Virtual Care. https://www.infoway-inforoute.ca/en/component/edocman/3828-canadians-health-care-experiences-during-covid-19/view-document?Itemid=0. Accessed August 4, 2022.
Canadian Institute for Health Information. COVID-19’s impact on emergency departments. Ottawa, ON: CIHI. 2021. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/emergency-departments. Accessed August 4, 2022.
Canadian Institute for Health Information. Virtual care: Impact of COVID-19 on patients receiving physician services. Ottawa, ON: CIHI. 2022. https://www.cihi.ca/en/virtual-care-impact-of-covid-19-on-patients-receiving-physician-services. Accessed August 4, 2022.
Canada Health Infoway. Canadian Digital Health Survey: Virtual Visits. 2021. https://insights.infoway-inforoute.ca/virtual_visits. Accessed August 4, 2022.
Canadian Medical Association. Virtual care in Canada: Progress and potential. Ottawa, ON: CMA. 2022. https://www.cma.ca/sites/default/files/2022-02/Virtual-Care-in-Canada-Progress-and-Potential-EN.pdf. Accessed August 4, 2022.
Ontario Health. Virtual Urgent Care Funding Opportunities. Toronto, ON. 2022. https://www.ontariohealth.ca/sites/ontariohealth/files/2021-08/FundingCriteria-VirtualUrgentCare.pdf. Accessed August 4, 2022.
Vaillancourt S, Seaton MB, Schull MJ, Cheng AHY, Beaton DE, Laupacis A, Dainty KN. Patients’ perspectives on outcomes of care after discharge from the emergency department: a qualitative study. Ann Emerg Med. 2017;70(5):648-658.e2.
Vaillancourt S, Cullen JD, Dainty KN, Inrig T, Laupacis A, Linton D, Malherbe S, Maybee A, Schull MJ, Seaton MB, Beaton DE. PROM-ED: development and testing of a patient-reported outcome measure for emergency department patients who are discharged home. Ann Emerg Med. 2020;76(2):219–29.
Canadian Institute for Health Information. NACRS Emergency Department Visits: Volumes and Median Lengths of Stay, 2003–2004 to 2020–2021: supplementary statistics. https://www.cihi.ca/en/nacrs-emergency-department-visits-and-lengths-of-stay. Accessed August 4, 2022.
Ho K, Lauscher HN, Stewart K, Abu-Laban RB, Scheuermeyer F, Grafstein E, et al. Integration of virtual physician visits into a provincial 8-1-1 health information telephone service during the COVID-19 pandemic: a descriptive study of HealthLink BC Emergency iDoctor-in-assistance (HEiDi). CMAJ Open. 2021;9(2):E635–41.
Canadian Medical Association. What Canadians Think About Virtual Health Care. 2020. https://www.cma.ca/sites/default/files/pdf/virtual-care/cma-virtual-care-public-poll-june-2020-e.pdf. Accessed August 4, 2022.
Environics Research. Dialogue. Canadian Attitudes on Health and Virtual Care 2021 Edition. Toronto, ON. 2021. https://www.dialogue.co/en/canadian-attitudes-on-healthcare-and-virtual-care-202. Accessed August 4, 2022.
Mondoux S, Hall JN, McLeod SL. Virtual emergency care: Decoupling the need for emergency services and expedited care. J Eval Clin Pract. 2022;28(1):10–2.
Atkinson P, McGeorge K, Innes G. Saving emergency medicine: is less more? CJEM. 2022;24(1):9–11.
Dawson T. It's a crisis: Canadian hospitals closing, cancelling surgeries amid COVID-related staff shortages. In: The National Post. 2022. https://nationalpost.com/news/canada/its-a-crisis-canadian-hospitals-closing-cancelling-surgeries-amid-covid-related-staff-shortages. Accessed August 4, 2022.
Dort LA. Nursing shortage cause of emergency department closure. In: The Toronto Star. 2022. https://www.thestar.com/news/canada/2022/04/20/nursing-shortage-cause-of-emergency-department-closure.html. Accessed August 4, 2022.
Grant K. Canadian nurses are leaving in Droves, worn down by 16 merciless months on the front lines of COVID-19. In: The Globe and Mail. 2021. https://www.theglobeandmail.com/canada/article-canadian-nurses-are-leaving-in-droves-worn-down-by-16-merciless-months/. Accessed August 4, 2022.
Li KY, Ng S, Zhu Z, McCullough JS, Kocher KE, Ellimoottil C. Association between primary care practice telehealth use and acute care visits for ambulatory care-sensitive conditions during COVID-19. JAMA Netw Open. 2022;5(3):e225484.
Shaw J, Brewer LC, Veinot T. Recommendations for health equity and virtual care arising from the COVID-19 pandemic: narrative review. JMIR Form Res. 2021;5(4):e23233.
Ganguli I, Orav EJ, Lupo C, Metlay JP, Sequist TD. Patient and visit characteristics associated with use of direct scheduling in primary care practices. JAMA Netw Open. 2020;3(8):e209637.
Budhwani S, Fujioka J, Thomas-Jacques T, De Vera K, Challa P, et al. Challenges and strategies for promoting health equity in virtual care: findings and policy directions from a scoping review of reviews. J Am Med Inform Assoc. 2022;29(5):990–9.
Acknowledgements
The authors wish to thank the members of the Provincial Virtual Urgent Care Evaluation Committee.
Author information
Authors and Affiliations
Contributions
SLM, SM, JNH, KD, JM, JET, LA and HO conceived the study and designed the protocol. SLM and HO secured research resources and support. SLM, SM, JNH and KD derived the survey questions. SM, JNH, ST, RL, MF, RAM, LR, CR, LB, LM, DR, SM and MW were virtual urgent care site leads for their respective institutions. SLM, LA and CT managed the data, including quality control. SLM drafted the manuscript, and all authors contributed substantially to its revision. SLM takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
JM is a paid employee of Ontario Health. HO is a paid advisor to the Ministry of Health and in that capacity has provided executive sponsorship for the virtual urgent care evaluation. Ontario Health provided operational funding to each of the Virtual Urgent Care pilot sites. There was no role of the funding body in the design, analysis, interpretation, writing, or approval of the manuscript. The views expressed in this manuscript are the views of the authors and do not necessarily reflect the views of the province.
Data availability statement
The data pertaining to this study are available in the published article and its online supplementary material.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McLeod, S.L., Mondoux, S., Hall, J.N. et al. Demographic characteristics, outcomes and experience of patients using virtual urgent care services from 14 emergency department led sites in Ontario. Can J Emerg Med 25, 65–73 (2023). https://doi.org/10.1007/s43678-022-00407-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00407-9